Abstract
Purpose
This paper seeks to describe how novel technologies such as the computer-assisted research environment (CAREN) may improve physical and cognitive rehabilitation for wounded warfighters.
Design/methodology/approach
The CAREN system is a dynamic platform which may assist service members who have sustained improvised explosive device injuries during Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn. The complex nature of warfighter injuries present unique rehabilitation challenges that demand new tools for quick return to active duty or the civilian community.
Findings
Virtual reality-based gait training programs may directly influence physiological and biomechanical performance for those who have endured combat injuries. The CAREN system provides a safe, interactive environment for the user while capturing kinematic and kinetic data capture to improve rehabilitation regimens.
Conclusions
This paper provides an overview of the CAREN system and describes how this dynamic rehabilitation aid may be a translational tool for collecting biomechanical and physiological data during prosthetic training. The CAREN platform allows users to be fully immersed in a virtual environment while healthcare providers use these simulations to improve gait and stability, obstacle avoidance, or improved weight shifting. As such, rehabilitation regimens may be patient specific.
Keywords: Rehabilitation, CAREN, Service members, Wounded warriors
Narrative
The use of improvised explosive devices during Operation Iraqi Freedom (OIF), Operation New Dawn (OND), and Operation Enduring Freedom (OEF) often results in complex orthopedic/neurological trauma which may include limb loss, spinal cord injury, and traumatic brain injury1. While advancements in military medicine during OIF/OEF has resulted in 92% of wounded warriors surviving blast-related injuries,2 musculoskeletal extremity trauma has been estimated to occur in 50% of all injuries in theatre1 – with 2% of warfighters incurring limb loss.3 Military databases have indicated that as of May 2012, returning US military combatants have sustained 1356 major limb amputations (775 from OIF/OND and 581 from OEF) and 243 minor amputations (213 from OIF/OND and 30 from OEF) (Fischer, 2012). The primary rehabilitation goal for these individuals is to provide them an expedited recovery and progressive reintroduction in the civilian or active duty populations.
The relative youth and high fitness level of injured service members with amputations make them an ideal population for new challenging rehabilitation methods which may require more physical/cardiac output than the civilian community.4,5 Novel technologies such as the computer-assisted research environment (CAREN) provide virtual simulations as a means to improve physical and cognitive skills for wounded warfighters while promoting resilience and recovery. The CAREN system, developed by MOTEK Medical (Amsterdam, Netherlands) consists of a motion capture system and a base driven by hydraulic and mechanical actuators. The base where the user stands is retrofit with force plates and a treadmill, with up to 6 degrees of freedom.6 This allows the operator to generate visual and physical perturbations that require the user to make dynamic responses during their gait patterns. The CAREN system may also be equipped with varying degrees of virtual reality immersion ranging from a flat video, dual-channel audio, theater in its “base” model to a 360°, surround sound dome enclosure in its “high end” version. Real-time motion tracking technology enables the CAREN system to follow patient movements frame-by-frame for detailed kinematic and biomechanical analysis using up to 24 mounting locations. Numerous studies have also been conducted assessing over ground walking vs. virtual reality treadmill-based rehabilitation indicating that the CAREN system is an effective rehabilitation aid for patient assessment.7 As demonstrated in Fig. 1, the CAREN system is equipped with a harness to ensure patient safety while simulations are being conducted.
Figure 1.

Photograph of a wounded warrior with a lower limb prosthetic using the CAREN system. (Image courtesy of Erik Wolf, Ph.D., Director of the Center for Performance and Clinical Research, WRNMMC).
The CAREN system is unique in that it allows a wounded warrior to be immersed in a realistic clinical environment, while therapist and physicians collect kinematic and kinetic data in order to plan future rehabilitation regimens. In everyday life, warfighters with lower extremity trauma may experience uneven terrain, cracks in pavements, slippery conditions, etc. – all potential scenarios that would may increase fall risk or injury.8 However, when using the CAREN system, specific physical perturbations may simulate these environmental conditions in a more safe and controlled setting. New rehabilitation methods and gait/prosthetic limb training may be developed for these individuals to mitigate falling risks outside of the clinic.8,9
Depending on the warfighters’ rehabilitation goals, simulations in the CAREN system may challenge reactive balance, reaction time, and muscle activation in order to improve gait and stability, obstacle avoidance or improved weight shifting (Fig. 2).10 The D-flow control software suite that the CAREN is equipped with allows for personalized monitoring modalities to be integrated during real-time during data collection. Owing to the modular and customizable nature of the software suite, D-flow can be easily programmed to accept a variety of complementary software packages that may run simultaneously using real-time feedback. Supplementing the CAREN system with complementary diagnostic tools enables clinicians and researchers to investigate a range of concurrent clinically relevant health markers during virtual simulations (Geijetbeek et al., 2011).
Figure 2.
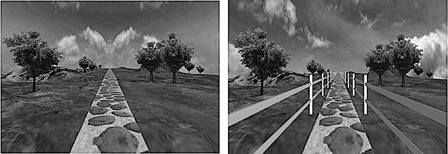
Side-by-side images of the two CAREN programs developed for wounded warrior rehabilitation. Note that the image on the left uses a basic path to encourage the individual to walk straight, while the image to the right has additional visual obstructions for those who are more experienced with their prosthetic device. (Image courtesy of Erik Wolf, Ph.D., Director of the Center for Performance and Clinical Research, WRNMMC).
Drawing on the customizable nature of the CAREN system, electro-myographic, and other physiological measures such as heart rate, VO2, VCO2, and ventilation data may be integrated directly into the feedback stream. Data gloves may be fitted to the patient during virtual reality immersion to track upper extremity limb, hand, and digit macro-movements when investigating grasping, reaching, and vestibular perturbation response (Subramanian et al., 2007). In addition, in-shoe pressure measurement and haptic/resistance may also be integrated into the system software (Mert et al., 2010). These supplementary systems significantly enhance the diagnostic power of the CAREN system and may enable a higher degree of patient-specific treatment and enhance rehabilitation regimens (Mert et al., 2010).
As a result of the rehabilitation benefits of the CAREN system, many of the United States military treatment facilities have been equipped with these platforms. Researchers at Walter Reed National Military Medical Center (WRNMMC) and the Center for the Intrepid (CFI) at Brooke Army Medical Center have used the CAREN to better understand gait patterns of warfighters who have sustained lower extremity trauma. One specific study by Werner et al.12 demonstrated that when eight transfemoral amputees were subjected to lateral perturbations on the CAREN platform, these wounded warriors avoided falling by using their uninjured limb and that there was little change in prosthetic ankle or knee kinematics on the affected side. This finding has important rehabilitation implications and may require improved prosthetic training – since overuse of an intact limb may lead to future complications (osteoarthritis and lower back pain),11 factors which may be correctable, if discovered early in the therapy process.
Another distinct advantage of the CAREN system is that testing may be conducted in a controlled environment in order to regulate mechanical and visual cues. As such, rehabilitation outcomes may be specifically investigated without the risk of confounding variables. Once such example is from a study by Nottingham et al.13 in which this team compared temporospatial parameters while using several prosthetic limb options: the conventional single axis hydraulic (SAH) knee, a microprocessor-controlled (MP) prosthetic knee and the X2 microprocessor knee (Otto Bock Healthcare, GmbH, Duderstadt, Germany) during slope ambulation. Twenty unilateral transfermoral amputees demonstrated that when descending a 10° slope that X2 users self-selected a faster walking speed, took longer steps than those using either the SAH or MP knee, and also did not require ambulatory aids; thereby demonstrating how MP knees may be beneficial for wounded warriors in slope descent. Data from this study may impact which prosthetic limb service members with lower limb amputations are fitted with, since the ultimate goal is to return these individuals to the active life they had prior to injury.
The applications for the CAREN system have continued to demonstrate how this rehabilitation tool is an important element in wounded warrior care. One distinct advantage of this system is that it provides physical and cognitive aid for those with multi-trauma and traumatic brain injury. Gait training has, and will always remain, an important therapy element for individuals with lower extremity amputations.14 While traditional therapy methods will always have a place in the clinic, virtual reality-based gait training programs have demonstrated the ability to directly influence physiological and biomechanical performance.11,15 However, it is worth noting that while the CAREN system has numerous clinical advantages, the financial and spatial requirements for the platform may preclude this from being a rehabilitation aid for individuals in the general public.
Acknowledgment
This material is based upon work supported by the Department of the US Army under Award Numbers W81XWH-12-2-0017 to the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (Fort Detrick, MD) and the Center for Rehabilitation Science Research USU Award NF90UG, (Bethesda, MD).
Disclaimer: The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army, the Department of Defense, or the United States government.
References
- 1.Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv 2010;19(1):2–7 [PubMed] [Google Scholar]
- 2.Gajewski D, Granville R. The United States Armed Forces Amputee Patient Care Program. J Am Acad Orthop Surg 2006;14(10 Spec No.):S183–7 [DOI] [PubMed] [Google Scholar]
- 3.Potter BK, Scoville CR. Amputation is not isolated: an overview of the US Army Amputee Patient Care Program and associated amputee injuries. J Am Acad Orthop Surg 2006;14(10 Spec No.):S188–90 [DOI] [PubMed] [Google Scholar]
- 4.Isaacson BM, Weeks SR, Pasquina PF, Webster JB, Beck JP, Bloebaum RD. The road to recovery and rehabilitation for injured service members with limb loss: a focus on Iraq and Afghanistan. US Army Med Dep J 2010;31–36 [PubMed] [Google Scholar]
- 5.Pasquina PF, Tsao JW, Collins DM, Chan BL, Charrow A, Karmarkar AM, Cooper RA. Quality of medical care provided to service members with combat-related limb amputations: report of patient satisfaction. J Rehabil Res Dev 2008;45(7):953–60 [DOI] [PubMed] [Google Scholar]
- 6.De Groot IJM, Zohar E, Haspels R, Van Keeken HG, Otten E. Case study: CAREN (computer assisted rehabiliation environment): a novel way to improve shoe efficacy. J Prosthet Orthot Int 2003;27:158–62 [DOI] [PubMed] [Google Scholar]
- 7.McAndrew PM, Dingwell JB, Wilken JM. Walking variability during continuous pseudo-random oscillations of the support surface and visual field. J Biomech 2010;43(8):1470–5 doi:10.1016/j.jbiomech.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gates DH, Darter BJ, Dingwell JB, Wilken JM. Comparison of walking overground and in a Computer Assisted Rehabilitation Environment (CAREN) in individuals with and without transtibial amputation. J Neuroeng Rehabil 2012;9(1):81 doi:10.1186/1743-0003-9-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vrieling AH, van Keeken HG, Schoppen T, Otten E, Hof AL, Halbertsma JP, et al. Balance control on a moving platform in unilateral lower limb amputees. Gait Posture 2008;28(2):222–8 doi:10.1016/j.gaitpost.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 10.Lees A, Vanrenterghem J, Barton G, Lake M. Kinematic response characteristics of the CAREN moving platform system for use in posture and balance research. Med Eng Phys 2007;29(5):629–35 doi:10.1016/j.medengphy.2006.06.004 [DOI] [PubMed] [Google Scholar]
- 11.Darter BJ, Wilken JM. Gait training with virtual reality-based real-time feedback: improving gait performance following transfemoral amputation. Phys Ther 2011;91(9):1385–94 doi:10.2522/ptj.20100360 [DOI] [PubMed] [Google Scholar]
- 12.Werner KM, Linberg A, Wolf EJ. Balance recovery kinematics after a lateral perturbation in patients with transfemoral amputations. Paper presented at the American Society of Biomechanics, 2012
- 13.Nottingham E, Aldridge J, Linberg A, Wolf EJ, Wilken JM, Scoville CR. Temporospatial outcomes during slope ascent and descent while using a novel microporcessor knee. Paper presented at the Gait and Clinical Movement Analysis Society, 2012
- 14.Kruger S. A virtual reality approach to gait training in service members with lower extremity amputations. Int J Disabil Human Dev 2011;10(4):313–6 [Google Scholar]
- 15.Everding VQ, Kruger S. Virtual reality enhanced balance training for service members with amputations. Paper presented at the 2011 Internation Conference on Virtual Rehabiliation (ICVR), Walter Reed Army Medical Center, Washington, DC, USA.
- 16.Subramanian S, Knaut LA, Beaudoin C, McFadyen BJ, Feldman AG, Levin MF. Virtual reality environments for post-stroke arm rehabilitation. J Neuroeng Rehabil 2007;4:20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fischer H. US military casualty statistics: Operation new dawn, operation iraqi freedom, and operation enduring freedom. Congressional Research Service 2012;7-5700:RS22452 [Google Scholar]
- 18.Geijetbeek T, Steenbrink F, Otten B, Even-Zohar O. D-flow: immersive virtual reality and real-time feedback for rehabilitation. Proceedings of the 10th International Conference on Virtual Reality Continuum and Its Applications in Industry, 2011;201–208 doi:10.1145/2087756.2087785 [Google Scholar]
- 19.Mert A, Frunt T, van der Lint R, Uittewaal KJM, Wurff vd P. The CAREN system is useful in the rehabilitation process: user survey of 50 patients. Dutch Society for Rehabilitation Physicians (VRA) annual congress, 2010. [Google Scholar]


