Abstract
Aim:
This work was carried out to study the hematologic profile of human immunodeficiency virus (HIV)-positive patients and its association with the clinicoimmunologic stage of the disease.
Materials and Methods:
A total of 187 patients with HIV, whether symptomatic or asymptomatic, diagnosed by enzyme-linked immunosorbent assay (ELISA) method according to the National AIDS Control Organization (NACO) guidelines were included in this study. Patients in the study population were divided into two groups: (1) Group A (antiretroviral therapy (ART) included patients receiving ART [ART-Y]) and (2) Group B included treatment naïve patients (ART-N). The patients were tested for hemoglobin (Hb), total red blood cells (RBC) count, RBC indices, reticulocyte count, packed cell volume (PCV), total lymphocyte counts(TLC), differential leukocyte counts (DLC), platelet count, and erythrocyte sedimentation rate (ESR). Cut-off values were determined as Hb < 10 g/dl, platelet count < 1.5 lakh/cumm, and TLC < 4,000/cumm. The group or categorical data were tested for statistical significance using Chi-square test and Z-test. The difference was reported as significant if P < 0.05.
Results:
(1) Anemia (predominantly normocytic normochromic) was prevalent in 40.1%, with slightly higher prevalence in those not receiving ART. It occurred with high frequency in patients with immunological (42.05%) and clinical acquired immunodeficiency disease syndrome (AIDS) (70.58%) compared with those who had an asymptomatic HIV infection with CD4 > 200/μl (28.57%). Patients on zidovudine (AZT) therapy had 34.6% anemia with increased mean corpuscular volume (MCV). (2) Thrombocytopenia was seen in 3.74% patients (higher percentage in untreated patients). (3) Leucopenia was observed in 5.88% in ART-Y (Group A) and 8.14% in ART-N (Group B) patients. (4) Pancytopenia was found in 1.6% patients.
Keywords: Anemia, art, clinicoimmunologic stage, human immunodeficiency virus
INTRODUCTION
Human immunodeficiency virus (HIV) infection is a state of profound immunodeficiency, encompassing a spectrum of disease ranging from acute syndrome seen with primary infection, prolonged asymptomatic state, to an advanced disease or full-blown acquired immunodeficiency disease syndrome (AIDS). Disorders of hematopoietic system are common but often overlooked complications of HIV infection which manifest at any stage of the disease and include anemia, leukopenia, thrombocytopenia, hemophagocytic syndrome, AIDS-related lymphoma, and rarely thromboembolism.
Due to the lack of laboratory technologies in resource-limited countries, WHO guidelines suggest the use of simple tests such as hemoglobin (Hb) <12 g/dl and total lymphocyte counts (TLC) <1,200/cumm as indicators for initiation of antiretroviral therapy (ART).[1] Thus the objective of this study was to study the hematologic profile of HIV-positive patients and its association with the clinicoimmunologic stage of the disease.
MATERIALS AND METHODS
The study population included 187 consecutive HIV-positive patients attending the ART clinic at Dr. Ram Manohar Lohia Hospital, New Delhi. The inclusion criteria included HIV-positive patients, symptomatic as well as asymptomatic, diagnosed by enzyme-linked immunosorbent assay (ELISA) method according to the National AIDS Control Organization (NACO) guidelines. Exclusion criteria included any primary hematologic disorder (such as thalassemia, leukemia, etc.), chronic renal/liver disease, receiving cytotoxic/immune modulating chemotherapy, pregnant and lactating women.
The study population was divided into three categories based on the clinicoimmunologic status of the patients:
HIV infection: No symptoms/signs of clinical AIDS, CD4 count > 200/μl.
Immunological AIDS: With CD4 < 200/μl, no symptoms/signs of clinical AIDS but CD4 count < 200/μl.
Clinical AIDS: Patients with any AIDS defining illness.
The patients in the study group were divided into two groups:
Group A (ART-Y): Patients receiving ART.
Group B (ART-N): Treatment naïve patients not on ART.
Cut-off values were defined to calculate the prevalence of different hematologic values. Anemia (Hb < 10 g%), thrombocytopenia (platelets < 1.5 lakh/mm3), leucopenia (white blood cells (WBC) <4,000/mm3). The hematologic profile was then statistically analyzed for prevalence of abnormalities and their association with the clinicoimmunologic stage of the disease, as well as between treated and nontreated groups (group A and group B). The group or categorical data were tested for statistical significance using the Chi-square test and Z-test. The difference was reported as significant if P < 0.05.
OBSERVATIONS AND RESULTS
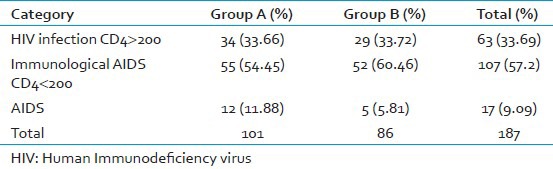
A total of 187 patients were included in the study population. There were 134 male and 53 female patients at a male–female ratio of 2.53:1. Age of the patients ranged from 18 to 66 years. The study population was divided into two groups. The distribution of patients in group A and group B in different categories is shown in Table 1.
Table 1.
The distribution of patients in group A and group B in different categories were as follows
Anemia
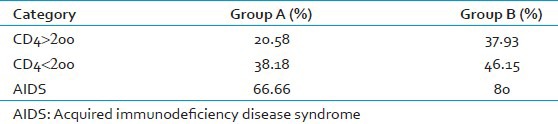
Anemia was observed in 40.10% of the total population, with higher prevalence of anemia in group A (35.64%) than in group B (45.34%). The difference in prevalence of anemia between the three categories was statistically significant (P = 0.005), the highest percentage seen in patients with full-blown AIDS (70.58%) compared to those without AIDS (28.57%). The difference in prevalence between the three categories was statistically significant (P = 0.005). In each clinical category, the percentage of patients with anemia was higher in group B compared with that in group A. The prevalence of anemia in group A was 35.64% (36 of 101). In group B, a higher proportion of patients, i.e. 45.34% (39 of 86), had anemia [Table 2]. Normocytic, normochromic anemia was the most common type of anemia accounting for 63.88% in group A and 69.23% in group B. Microcytic, hypochromic anemia was found in 19.44% and 25.64% in group A and B, respectively. Macrocytic anemia was the least common type. Dimorphic anemia was seen in 13.88% of patients in group A, probably due to degree of macrocytosis induced by anemia in patients with zidovudine (AZT) in this group (average MCV − 95.4 fl).
Table 2.
In each clinical category, the percentage of patients with anemia in two different groups of patients
Anemia in patients with zidovudine therapy
Anemia was seen in 9 of 26 patients on AZT therapy, i.e., 34.62%. The average MCV of anemic patients on AZT therapy was 95.4 fl. Thus the anemia in these patients was normocytic to macrocytic. However, macrocytosis was also present in patients on AZT therapy who did not have anemia.
Platelet count
Platelet counts were normal in 96.03% of patients in group A and 94.18% of patients in group B. Thrombocytosis was seen in 0.99% and 1.16% in group A and group B, respectively. The overall prevalence of thrombocytopenia was 3.74%. There was a slightly greater prevalence in early HIV infection (CD4 > 200), i.e., 4.76%, as well as in patients with clinical AIDS, i.e., 5.88%.
Leukocyte counts
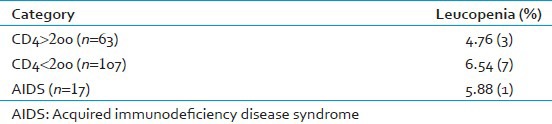
Leukocyte counts were mostly normal in group A (89.91%) and group B (79.07%) patients, respectively. Leukocytosis was found in 6.93% of patients in group A, with a higher prevalence of 12.79% in group B. The total prevalence of leukopenia in the study population was 5.88%:3.96% patients in group A and 8.14% in group B had leukopenia. The difference was statistically insignificant (P = 0.24). The prevalence of leukopenia in different clinical categories is as shown in Table 3. Thus leukopenia was found in all stages of disease. Associated anemia was observed in 75% of patients with leukopenia in group A and 100% of patients with leucopenia in group B. Pancytopenia was found in 1.60%, with 0.99% and 2.32% patients in group A and group B, respectively (P > 0.05). Eosinophilia was a striking feature found in a total of 22.99%, with the prevalence of 24.75% in group A and 20.93% in group B (P = 0.62). Venous thrombosis was found in one patient of group A, with the prevalence of 0.53%. Hemophagocytic syndrome is a rare entity, found in one patient (0.53%) of group B who presented with fever, hepatosplenomegaly, and pancytopenia.
Table 3.
The prevalence of leucopenia in different clinical categories was as follows
DISCUSSION
Disorders of the hematologic system are common in HIV-infected patients. The hematologic manifestations of HIV are varied and prevalent throughout the course of the disease. Anemia is a frequent complication of HIV infection. In a study by Patwardhan et al.,[2] who investigated the hematologic profile of 500 HIV patients, anemia was found in 30.8% of individuals. Our analysis showed a 40.1% prevalence of anemia, with a higher prevalence in patients not receiving ART compared to that in those receiving highly active antiretroviral therapy (HAART). Thus, the use of HAART results in decrease in the prevalence of anemia. In our study, the proportion of patients having a normal Hb (>12 g%) was significantly different in treatment and nontreatment groups. Only 20.93% patients who were not receiving any ART (group B) had Hb > 12 g%. However, this percentage was significantly higher, i.e. 42.57%, in group A, who were receiving HAART. This observation was also found in a previous study which included patients recruited to the EuroSIDA cohort.[3]
However, in this study, the prevalence of anemia was still high (35.64%) in the treated group. This could be because of various drugs used for treatment of HIV and prophylaxis/treatment of opportunistic infections causing bone marrow suppression and anemia. This study also revealed an increase in the prevalence of anemia with progression of clinicoimmunologic stage of the disease, which is in accordance with previous studies.[4,5]
Various studies have shown that anemia is an important factor in understanding the clinical course of HIV-infected patients.[6] Sullivan et al., in their study reported that the incidence of anemia was strongly and consistently associated with progression of HIV disease as measured by diagnosis of AIDS defining opportunistic illness and measurement of CD4 count < 200 cells/μl. This association is most likely explained by the increasing viral burden as HIV disease progresses, which leads to cytokine-mediated myelosuppression and anemia.[4] The results of a study by Mocroft et al.,[3] showed that hemoglobin levels provided prognostic information independent of that provided by CD4 count.
In this study, normocytic normochromic anemia was the most common morphologic type of anemia, followed by microcytic hypochromic and the macrocytic, the rarest of all. A dimorphic picture was found in 13.88% of anemic patients in group A probably due to AZT-induced macrocytosis. These results are similar to those reported by other workers.[2,5]
In our study, anemic patients on AZT therapy had mostly a macrocytic type of anemia. However, macrocytosis was also seen in patients who did not have anemia and who were on AZT therapy. Thus AZT-induced macrocytosis is not necessarily associated with anemia. More recent studies of combination ART have confirmed the relatively low incidence of severe anemia at low doses of AZT.[7] In our study, most of the patients had normal platelet counts. Thrombocytopenia was seen in 3.74%, i.e. 2.95% in group A and 4.65% in group B. This was similar to the finding of Tripathi et al., and Patwardhan et al.,[2,5] Thrombocytopenia occurred in all stages of the disease, with preponderance in early stages as well as in late stages of full-blown AIDS.
In this study, normal leukocyte count was most commonly seen in both the groups. Leukocytosis was seen in 6.93% of patients in group A and 12.79% in group B. This is similar to that observed in Patwardhan's study.[2] The higher prevalence in group B, i.e., untreated patients, probably reflects an increase in leukocyte count secondary to various opportunistic infections that are more common in patients not receiving any antiretroviral or chemoprophylactic therapy. Patwardhan reported leukopenia in 15.47% of cases.[2] Leukopenia was seen in a total of 5.88% of patients in this study with no significant difference with respect to clinical stage of the disease. It was, however, more common in group B, ART-N (8.14%) compared with those in the group A, ART-Y (3.96%). In total, 75% and 100% of leukopenic patients in group A and group B, respectively, had associated anemia. This observation is in accordance with that reported by Zon et al.,[8] who described a considerable overlap in hematologic abnormalities, wherein 88% of granulocytopenic patients were found to be anemic.
Our study reported pancytopenia in 1.6% of patients. Eosinophilia is probably due to reaction to various parasitic infestations that are common in patients with HIV infection. Venous thrombosis was found in 0.53% of patients, i.e., one out of 187 patients. A center for disease control (CDC) study found the incidence of thrombosis to be 2.6 per 1,000 person years, which is significantly higher than expected in the general population.[9] The hemophagocytic syndrome, a rare complication of HIV, was found in one patient in our study, thus giving a prevalence of 0.53%. This complication was associated with a CD4 of less than 200/μl.
CONCLUSION
This study of the hematologic profile of HIV patients reiterated the fact that affection of the hematopoietic system by HIV is common. The hematologic abnormalities are prevalent through all stages of the disease, and some of these may serve as indicators of clinical progression.
Limitations of the study
There is one limitation that needs to be acknowledged and addressed regarding this study. Although routine hematologic investigations and relevant clinical history (e.g., history of repeated blood transfusions or positive family history in thalassemics) were taken into consideration, further specific investigations (e.g., iron studies, high-performance liquid chromatography, and Hb electrophoresis) should be carried out in such studies to rule out other causes of anemia (e.g., iron deficiency anemia and thalassemia).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Badri M, Wood R. Usefulness of total lymphocyte count in monitoring highly active antiretroviral therapy in resource-limited settings. AIDS. 2003;17:541–5. doi: 10.1097/00002030-200303070-00009. [DOI] [PubMed] [Google Scholar]
- 2.Patwardhan MS, Golwilkar AS, Abhyankar JR, Atre MC. Hematological profile of HIV positive patients. Indian J Pathol Microbiol. 2002;45:147–50. [PubMed] [Google Scholar]
- 3.Mocroft A, Kirk O, Barton SE, Dietrich M, Proenca R, Colebunders R, et al. Anaemia is an independent predictive marker for clinical prognosis in HIV-infected patients from across Europe. EuroSIDA study group. AIDS. 1999;13:943–50. doi: 10.1097/00002030-199905280-00010. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: Results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91:301–8. [PubMed] [Google Scholar]
- 5.Tripathi AK, Kalra P, Misra R, Kumar A, Gupta N. Study of bone marrow abnormalities in patients with HIV disease. J Assoc Physicians India. 2005;53:105–10. [PubMed] [Google Scholar]
- 6.Sullivan P. Associations of anemia, treatments for anemia, and survival in patients with human immunodeficiency virus infection. J Infect Dis. 2002;185:S138–42. doi: 10.1086/340203. [DOI] [PubMed] [Google Scholar]
- 7.Eron JJ, Benoit SL, Jemsek J, MacArthur RD, Santana J, Quinn JB, et al. Treatment with lamivudine, zidovudine, or both in HIV-positive patients with 200 to 500 CD4+cells per cubic millimeter. North American HIV Working Party. N Engl J Med. 1995;333:1662–9. doi: 10.1056/NEJM199512213332502. [DOI] [PubMed] [Google Scholar]
- 8.Zon LI, Arkin C, Groopman JE. Haematologic manifestations of the human immune deficiency virus (HIV) Br J Haematol. 1987;66:251–6. doi: 10.1111/j.1365-2141.1987.tb01307.x. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan PS, Dworkin MS, Jones JL, Hooper WC. Epidemiology of thrombosis in HIV-infected individuals. The Adult/Adolescent Spectrum of HIV Disease Project. AIDS. 2000;14:321–4. doi: 10.1097/00002030-200002180-00015. [DOI] [PubMed] [Google Scholar]


