Abstract
Background:
Researchers have reported association of plasma/serum lipids and lipoproteins with different cancers. Increase levels of circulating lipids and lipoproteins have been associated with breast cancer risk.
Aim:
The aim of this study is to compare serum lipid profiles: total-cholesterol (T-CHOL), triglyceride (TG), high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-cholesterol (LDL-C) and very low density lipoprotein-cholesterol (VLDL-C) between breast cancer patients and normal participants.
Materials and Methods:
A total of 403 women in this study were divided into two groups in the period during May 2006-April 2007. Blood samples were collected from 249 patients with early stage breast cancer and 154 normal controls for serum lipid profiles (T-CHOL, TG, HDL-C, LDL-C and VLDL-C) analysis using Hitachi 717 Autoanalyzer (Roche Diagnostic GmbH, Germany). TG, LDL-C and VLDL-C levels in breast cancer group were significantly increased as compared with normal controls group (P < 0.001), whereas HDL-C and T-CHOL levels were not.
Results:
The results of this study suggest that increased serum lipid profiles may associate with breast cancer risk in Thai women. Further studies to group important factors including, cancer stages, types of cancer, parity, and menopausal status that may affect to lipid profiles in breast cancer patients along with an investigation of new lipid profiles to clarify most lipid factors that may involve in breast cancer development are needed.
Keywords: Breast cancer, lipid profiles, lipoprotein, serum lipids
INTRODUCTION
Lipids are the major cell membrane components essential for various biological functions including cell growth and division of normal and malignant tissues. Usefulness of variations in tissue/blood cholesterol levels in diagnosis and treatment of various diseases has been studied by several workers. Although, its prime role in the pathogenesis of coronary heart disease has been consistently found, researchers have reported association of plasma/serum lipids and lipoproteins with different cancers.[1,2,3,4] Alterations in the circulatory cholesterol levels have been found to be associated with etiology of breast cancer and colorectal cancer. However, only a few reports are available on plasma lipid profile in the head and neck cancer.[5]
Plasma lipids level reflects dietary lipid intake in individuals. There are several reports of elevated plasma lipid level such as total lipids, phospholipids, triglycerides (TG), total-cholesterol (T-CHOL), low density lipoprotein-cholesterol (LDL-C) and free fatty acids in pre and post-menopausal breast cancer patients.[6] It has been postulated that changes in the concentration of serum lipids in the breast cancer patients could result in an increase production of tumor necrosis factor and inhibit adipose lipoprotein lipase activity by the action of insulin.[7] These changes impair the catabolism of very low density lipoprotein (VLDL), leading to an increase in high density lipoprotein-cholesterol (HDL-C). Epidemiology studies reveal that HDL-C and breast cancer are influenced by variables such as dietary fat intake, alcohol consumption, body weight, country of residence, pregnancy, endogenous hormones, smoking, exercise, and socioeconomic status.[8] HDL-C level has been shown to be higher in the subject with extensive mammographic dysphasia, which was defined as sheet-like areas of radiological density that were distinguished from the linear densities that characterize prominent ducts and breast occupied by radiological changes at least 75% family history of breast cancer.[9] However, it has been reported that HDL-C level was either elevated or depressed in women with the breast cancer.[10]
Breast cancer is the most common type of cancer in women; about 80-90% of all breast cancers are infiltrating ductal carcinoma. The precise cause of breast cancer is unknown; however, the female sex hormone, estrogen, is reported carcinogenic promoter for cellular growth in breast tissues and reproductive organs. In addition, environmental factors such as exposure to radiation and chemicals may trigger the onset of breast cancer.[11] The risk for breast cancer increases with a high fat diet, obesity,[1,2] use of contraceptives, lack or short duration of breast feeding and family history of breast cancer. The discovery of the tumor suppressor genes BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 and BRCA2 genes. In normal cells, these genes help prevent cancer by making proteins that keep the cells from growing abnormally. If you have inherited a mutated copy of either gene from a parent, you have a high risk of developing breast cancer during your lifetime. The risk may be as high as 80% for members of some families with BRCA mutations.[12,13]
Increase levels of circulating lipids and lipoproteins have been associated with breast cancer risk. The aim of this study is to compare serum lipid profiles: (i) T-CHOL, (ii) LDL-C, (iii) HDL-C, (iv) VLDL-C and (v) TG between normal control and breast cancer patients in Thai women.
MATERIALS AND METHODS
Subjects
The women in our study participated as two populations during the period of May 2006-April 2007. A total of 403 subjects were studied. First group or breast cancer including 249 patients had early stage of malignant tumors limited to the breast and regional lymph nodes and tissue was diagnosed by histopathological examination, which was removed at surgery and diagnosed at the Division of Pathology, National Cancer Institute, Thailand and 154 controls group, who had no any illness, were included in the study control and were selected randomly from an annual health check-up women at National Cancer Institute, Thailand. Ethnic of this research was approved by the Ethnic Committee of the National Cancer Institute, Thailand.
Blood sample collection and preparation
Five milliliters of fasting blood was collected into Vacutainer® plain tube from each of the subjects. The blood was allowed to clot and then centrifuged at 3,000 rpm for 15 min within 30 min of sample collection and analyzed within 6 h after it's the separation.
Laboratory assay
The following parameters were analyzed with each sample. (i) T-CHOL (ii) TG (iii) HDL-C (iv) LDL-C and (v) VLDL-C. Serum lipid profile was performed with the Hitachi 717 Autoanalyzer (Roche Diagnostic GmbH, Mannheim, Bad Nauheim, Germany) using commercial kits from Roche Diagnostic Products.
Two levels of control material and analyses were performed by at the Clinical Chemistry Laboratory Section, Division of Pathology, National Cancer Institute, Bangkok, Thailand according to the manufacturer.
Statistical analysis
All data was analyzed using the Statistical Package for Social Sciences (SPSS) software computer program version 11.0 (SPSS, Chicago, IL). Data were expressed as mean (x̄) and standard deviation (SD) following analyzes using student t-test, which was performed for comparison between control and patient groups. A value of P < 0.05 was considered significant, and P < 0.01 was considered as statistical significant.
RESULTS
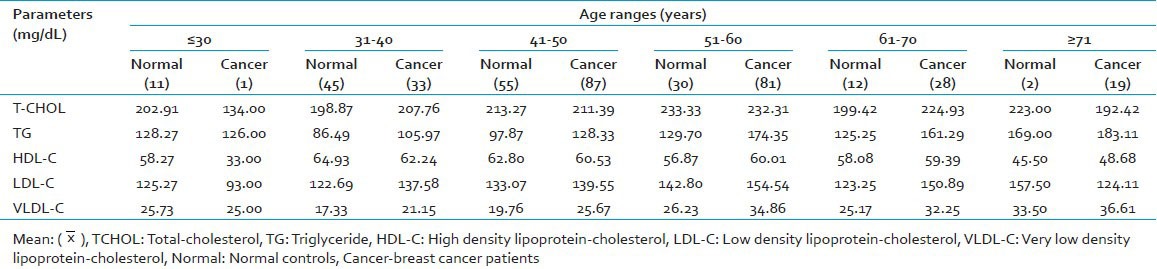
The level of T-CHOL was lower in cancer group at ≤30, 41-50 and ≥71 age ranges. Except for the ≤30 age range, TG level in cancer group was higher than normal control group [Table 1]. The HDL-C level was lower in cancer group at ≤50 year old and higher when it was at ≥50 year old. LDL-C level in cancer group at ≤30 and ≥71 year old was lower than controls, therefore, cancer group between 31 and 70 years old had higher LDL-C concentration than control and also higher than normal range (0-130 mg/dl). VLDL-C level in cancer group was also higher than control at 31-70 and ≥71 age ranges, however, not over the normal range (0-40 mg/dl).
Table 1.
Mean (x̄) of lipid profile in normal control and breast cancer patients with age ranges (years)
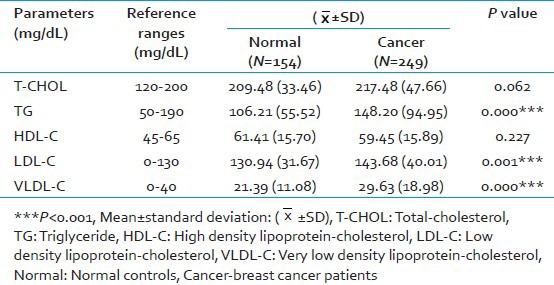
The comparison of lipid profiles between normal controls and breast cancer patients are shown in Table 2. The levels of TG, LDL-C and VLDL-C (mean ± SD) in breast cancer group were 148.20 + 94.95, 143.68 + 40.01 and 29.63 + 18.98 while in controls group were 217.48 + 47.66 and 59.45 + 15.89, respectively. We found that TG, LDL-C and VLDL-C levels in breast cancer group were significantly higher than controls group (P < 0.001). However, T-CHOL level in breast cancer group was not significantly higher than the control group. HDL-C level in breast cancer group was lower than controls group, but it was not statically significant.
Table 2.
Comparison of lipid profile between normal controls and breast cancer patients
DISCUSSION
Human mammary tissue metabolizes lipids from plasma affected by female gonadal hormones. Malignant proliferation of breast tissue in women has been associated with changes in plasma lipid and lipoproteins levels.[14] HDL-C level have been shown to be higher in the subject with extensive mammographic dysplasia and family history of breast cancer.[9,15] Contrary, HDL-C level was lower in cancer group at ≤50 year old and was not significant different in our study. Few studies have however directly shown the relationship of HDL-C to breast cancer.[16]
The relationship between lipid profiles in breast cancer patients was observed during the present study and corresponded to the previous study, which reported by Hoyer and Engholon 1992.[17] Our study was indicated significant higher in TG, LDL-C and VLDL-C levels of breast cancer group [Table 2]. However, HDL-C and T-CHOL levels were not significant different between breast cancer group and control group. The increased TG, LDL-C and VLDL-C and decreased HDL-C value increases the risk of coronary heart disease,[18] and high body fat with increased serum lipid profiles were important risks for breast cancer. Researchers have reported association of plasma/serum lipids and lipoproteins with different cancers.[1,2,3,4]
This finding was corresponded to Elkhadrawy, et al. 1998[19] that LDL-C level was increased in breast cancer patients and T-CHOL level was not significant increased. Whereas, our results were not in agreement with the previous study reported by Hasija and Bagga 2005,[10] that T-CHOL level was highly significant to breast cancer. Thus, we suggest that further study need to group important factors including cancer stages, types of cancer, parity and menopausal status may affect to lipid profiles in breast cancer patients along with lipid profiles to clarify most lipid factors, which is alter in breast cancer patients.
ACKNOWLEDGMENTS
We are grateful to the National Cancer Institute, Bangkok, Thailand for a research facility and grant support. We would like to sincerely thank all staffs of Clinical Chemistry Laboratory Section, Division of Pathology and all participants (normal controls and breast cancer patients) for providing useful data and helping on this research.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schatzkin A, Hoover RN, Taylor PR, Ziegler RG, Carter CL, Albanes D, et al. Site-specific analysis of total serum cholesterol and incident cancer in the national health and nutrition examination survey I epidemiologic follow-up study. Cancer Res. 1988;48:452–8. [PubMed] [Google Scholar]
- 2.Gerber M, Richardson S, Crastes de Paulet P, Pujol H, Crastes de Paulet A. Relationship between vitamin E and polyunsaturated fatty acids in breast cancer. Nutritional and metabolic aspects. Cancer. 1989;64:2347–53. doi: 10.1002/1097-0142(19891201)64:11<2347::aid-cncr2820641126>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 3.Forones NM, Falcao JB, Mattos D, Barone B. Cholesterolemia in colorectal cancer. Hepatogastroenterology. 1998;45:1531–4. [PubMed] [Google Scholar]
- 4.Chyou PH, Nomura AM, Stemmermann GN, Kato I. Prospective study of serum cholesterol and site-specific cancers. J Clin Epidemiol. 1992;45:287–92. doi: 10.1016/0895-4356(92)90089-6. [DOI] [PubMed] [Google Scholar]
- 5.Patel PS, Shah MH, Jha FP, Raval GN, Rawal RM, Patel MM, et al. Alterations in plasma lipid profile patterns in head and neck cancer and oral precancerous conditions. Indian J Cancer. 2004;41:25–31. [PubMed] [Google Scholar]
- 6.Bani IA, Williams CM, Boulter PS, Dickerson JW. Plasma lipids and prolactin in patients with breast cancer. Br J Cancer. 1986;54:439–46. doi: 10.1038/bjc.1986.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knapp ML, al-Sheibani S, Riches PG. Alterations of serum lipids in breast cancer: Effects of disease activity, treatment, and hormonal factors. Clin Chem. 1991;37:2093–101. [PubMed] [Google Scholar]
- 8.Boyd NF, McGuire V. Evidence of association between plasma high-density lipoprotein cholesterol and risk factors for breast cancer. J Natl Cancer Inst. 1990;82:460–8. doi: 10.1093/jnci/82.6.460. [DOI] [PubMed] [Google Scholar]
- 9.Boyd NF, McGuire V, Fishell E, Kuriov V, Lockwood G, Tritchler D. Plasma lipids in premenopausal women with mammographic dysplasia. Br J Cancer. 1989;59:766–71. doi: 10.1038/bjc.1989.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hasija K, Bagga HK. Alterations of serum cholesterol and serum lipoprotein in breast cancer of women. Indian J Clin Biochem. 2005;20:61–6. doi: 10.1007/BF02893044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paley PJ. Screening for the major malignancies affecting women: Current guidelines. Am J Obstet Gynecol. 2001;184:1021–30. doi: 10.1067/mob.2001.111714. [DOI] [PubMed] [Google Scholar]
- 12.Davis DL, Bradlow HL. Can environmental estrogens cause breast cancer? Sci Am. 1995;273:167–72. [PubMed] [Google Scholar]
- 13.Jamall S, Ishaq M, Mahmood AJ, Khadim M. CA-15-3 and lipid profile in breast cancer patients. Pak J Biochem Mol Biol. 2010;43:114–8. [Google Scholar]
- 14.Lane DM, Boatman KK, McConathy WJ. Serum lipids and apolipoproteins in women with breast masses. Breast Cancer Res Treat. 1995;34:161–9. doi: 10.1007/BF00665788. [DOI] [PubMed] [Google Scholar]
- 15.Ray G, Husain SA. Role of lipids, lipoproteins and vitamins in women with breast cancer. Clin Biochem. 2001;34:71–6. doi: 10.1016/s0009-9120(00)00200-9. [DOI] [PubMed] [Google Scholar]
- 16.Agheli N, Therwath A. Nutrition, dietary fat and breast cancer: A review. Indian J Cancer. 1994;31:218–25. [PubMed] [Google Scholar]
- 17.Høyer AP, Engholm G. Serum lipids and breast cancer risk: A cohort study of 5,207 Danish women. Cancer Causes Control. 1992;3:403–8. doi: 10.1007/BF00051352. [DOI] [PubMed] [Google Scholar]
- 18.Kannel WB. Status of risk factors and their consideration in antihypertensive therapy. Am J Cardiol. 1987;59:80A–90. doi: 10.1016/0002-9149(87)90182-2. [DOI] [PubMed] [Google Scholar]
- 19.Elkhadrawy TM, Ahsan H, Neugut AI. Serum cholesterol and the risk of ductal carcinoma in situ: A case-control study. Eur J Cancer Prev. 1998;7:393–6. doi: 10.1097/00008469-199810000-00004. [DOI] [PubMed] [Google Scholar]


