Abstract
OBJECTIVES:
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) is a newly defined disease in neuropsychiatry and occurs with an autoimmune mechanism after Group A Beta Hemolytic Streptococcus (GABHS) infection. Tumor necrosis factor (TNF), encoded by TNF-α gene has an important role in the apoptotic mechanisms of autoimmune diseases. Recently, TNF-α polymorphisms and autoimmune/psychiatric disorders have been reported to be related. In this regard, we focused on to investigate a possible relation between the TNF-α gene promoter region−308 G/A and − 850 C/T polymorphisms and PANDAS.
MATERIALS AND METHODS:
In this study, ages of PANDAS patient and control groups were ranging from 4 years to 12-year-old. Patient group includes childhood onset PANDAS patients (n = 42) and control group includes healthy children (n = 58). Diagnoses have been carried out according to Diagnostic and Statistical Manual of Mental Disorder (DSM-IV) criteria with Affective Disorders and Schizophrenia-Present and Lifetime (KSAD-S-PL) and Children Yale-Brown Obsessive Compulsive Scale Moreover, PANDAS criteria established by the American National Psychiatry Institute have been employed for diagnoses. For identifying polymorphisms; Polymerase Chain Reaction, Restriction Fragment Length Polymorphism and Polyacrylamid Gel Electrophoresis were used.
RESULTS AND DISCUSSION:
For −308 polymorphism, 37 of 42 PANDAS patients’ results and for −850 C/T polymorphism, 38 of 42 PANDAS patients’ results were obtained. According to our statistical analysis there is a positive relationship between PANDAS patients for −308 G/A polymorphism but not for −850 C/T polymorphism. There is no positive relationship between −308 G/A polymorphism and antistrep-tolysin O (ASO) titers and no relationship between −850 C/T polymorphism and ASO titers. We found, however, positive relationship between genders of patients (boys) and the disease. According to our results, we propose that the AA polymorphism of −308 G/A polymorphism can be used as a molecular indicator for PANDAS.
Keywords: Autoimmune, pediatric autoimmune neuropsychiatric disorders associated with streptococcal, polymorphism, streptococcus, tumor necrosis factor-α gene
Introduction
Obsessive-compulsive disorder (OCD), tic disorders, a subgroup of childhood-onset OCDs called Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal (PANDAS) are pre-pubertal onset autoimmune neuropsychiatric disorders associated with the basal ganglia abnormalities in which antibodies produced against Group A Beta Hemolytic Streptococcus (GABHS) infections cross react with neuron epitopes.[1] Therefore, these disorders are referred as post-streptococcal movement disorders.[2–7] OCD and tic disorders may be triggered by stress, anxiety, and illnesses (for example; GABHS infections).[8] GABHS infections, comorbidities, and tics are characteristic features in the etiology of OCD, PANDAS, and Sydenham’s chorea.[9,10] Due to the damage of basal ganglia in a period of days to weeks following a GABHS infection, tics, and obsessive compulsive symptoms occur in patients.[9] The association between Sydenham’s chorea and streptococcus was first stated by Taranta and Stollerman in 1956 however, association between OCD and Sydenham’s chorea was discovered by some workers.[11,12] In the following decades, clinicians, and researchers continued to perform studies for neuropsychiatric disorders.[12,13] Recent studies suggest that 50-80% of OCD cases have a childhood onset.[9,14–21] Childhood onset OCD patients usually have a positive history of childhood tonsillitis, tic disorders and more antistrep-tolysin O (ASO) titers than adult onset OCD patients.[22,23] In addition, obsessions and compulsions are the common symptoms for both of them.[24] Prevalence of OCD among adolescents is 0.4%.[6] Gender of patients can be effective or non-effective factors for PANDAS. It is proposed that mostly boys are affected compared to girls (3:2, boys:girls ratio) and age of onset for boys is generally earlier.[14] Immune system of patient is affected as the disease progress. In the patient’s immune system, first B lymphocytes which are susceptible to M group of antigens neutralize streptococcus via macrophages. Following this activation some B lymphocytes pass over blood-brain barrier and associate with the cell membrane of neurons due to epitope similarity.[18,25–28] Outcome of this association is the neuronal destruction of the patient’s apoptosis mechanisms. Therefore, the loss of neurons in the brain part which is supposed to coordinate the movement and active memory cannot function properly thereby neuropshychiatric signs like tics would be unavoidable.
Tumor necrosis factor (TNF)-α gene was selected because it is an important cytokine secreted by monocyte, phagocyte T-and B-lymphocytes, and natural killer cells and it is association with autoimmune-based neuropsychiatric disorders has been proposed previously. Moreover, primary incentive for us to research on this topic is that there has not been any research performed on TNF-α, which is a part of Major Histocompatibility (MHC) complex and autoimmune-based PANDAS disorder. Secondly, TNF-α-308 G/A and − 850 C/T polymorphisms have been shown to be related with autoimmune-based disorders which makes it plausible to think that these polymorphisms could also be related to PANDAS. Despite other researches on this issue, the relationship between neuropsychiatric disorders specifically PANDAS and GABHS infections are not completely understood yet. One reason for this uncertainty is the triggering of other existing factors.[29]
Materials and Methods
In this study, 42 children with PANDAS from Cukurova University Medical Faculty Child and Adolescent Psychiatry Department and 58 healthy children from Cukurova University Medical Faculty Social Pediatrics Department were included. Ages of patient and control groups’ ages were ranging from 4-year to 12-year-old. Patients were diagnosed by Cukurova University Medical Faculty Child and Adolescent Psychiatry Department according to Diagnostic and Statistical Manuel of Mental Disorder (DSM-IV) criteria with Kiddie Shedule for Affective Disorders and Shizophrenia-Present and Lifetime Version (KSAD-S-PL). Children’s Yale-Brown Obsessive Compulsive Scale was used to evaluate the severity of PANDAS symptoms. Demographic data and previous infection histories of patients and their families including tonsillitis infection history (more than 6 tonsillitis attacks/year), prophylactic antibiotic/penicillin use, tonsillectomy, ASO titers, symptom aggravation associated with infections were obtained. The Ethics Committee of the Cukurova University Medical Faculty approved this study. Informed consent obtained from the patient and control groups’ parents before collecting blood samples. To identify TNF-α gene polymorphisms; first we performed deoxyribonucleic acid (DNA) isolation from the blood; DNA of the patients was isolated by using the Miller’s salting out method.[30]−308 G/A and − 850 C/T regions were amplified with Polymerase Chain Reaction. Polymorphisms were genotyped by using restriction enzymes with Restriction Fragment Length Polymorphism (RFLP) and Polyacrylamid Gel Electrophoresis (PAGE) methods.[13] Cycle conditions of the reaction mixture were carried out in a thermal cycler using the thermal profile given below for identifying −308 G/A polymorphism; initial denaturation at 94°C for 1 min, denaturation at 94°C for 15 s, annealing at 62°C for 30 s, primer extension at 72°C for 15 s for 40 cycles and a final extension at 72°C for 1 h. For −308 G/A polymorphism, the 142 bp product was amplified with following primers; F-5’- GGGACACACAAG CATCAAGG-3’ and R-5’-AATAGGTTTTGAGGGCCATG-3’. 126 bp digested product was referred as polymorphic AA genotype. The non-digested 142 bp product was referred as wild-type GG genotype. An allele generates a restriction site for Nco I restriction enzyme. This polymorphism includes only one base variation (G → A) distinguished by Nco I on 8% polyacrylamide gel. Thermal profile for identifying −850 C/T polymorphism; initial denaturation at 94°C for 3 min, denaturation at 94°C for 20 s, annealing at 68°C for 30 s, primer extension at 72°C for 1 min for 40 cycles and final extension at 72°C for 1 h. For −850 C/T polymorphism, the 131 bp product was amplified with following primers; F-5’AAGTCGAGTATGGGGACCCCCCGTTAA-3’ and R-5’- CCCCAGTGTGTGGCCATATCTTCTT-3’. 106 bp digested product was referred as wild-type CC poymorphism. The non-digested 131 bp product was referred as polymorphic TT poymorphism. This polymorphism includes only one base variation (C → T) distinguished by Hind II enzyme on 8% polyacrylamide gel. Polymorphisms were genotyped using available restriction enzymes with RFLP and PAGE methods.[31–33] ASO is considered in Streptolysin O enzyme units (TODD). Values above 200 are accepted as significant and referred as a new indicator of infection.[34] Actually, normal value of ASO is 200 but in our study, cut-off value was taken as 400 because children in the patient group had already consulted to out-patient clinic during active infection period. Serum ASO titers of patients were determined using the Beckman Delta Nephelometor in Cukurova University Medical Faculty Balcali Hospital Central Laboratory Biochemistry Department. This laboratory is accredited by Joint Commission International.
Statistical analysis for comparing the prevalence of polymorphic genotypes between PANDAS patient and control groups were carried out using the Chi-square Test. In PANDAS patients, to evaluate the effect of ASO titer values on the polymorphic genotypes Kruskal-Wallis Test and for multiple comparisons Bonferroni adjusted Mann Whitney U Test was employed. Statistical analysis was performed using SPSS 15.0 software and the level of statistical significance was accepted as P < 0.05.
Results
The current study was carried out to investigate the effect of polymorphic genotypes in the progress of PANDAS. For −308 G/A polymorphism, 37 of 42 PANDAS patients’ results were obtained [Table 1]. In the patient group, for −308 G/A polymorphism, we detected 5 polymorphic GA (13.5%) and 32 polymorphic AA genotypes (86.5%) but no normal GG polymorphism. In the control group, however, five polymorphic GA (8.6%) and 53 normal (91.4%) GG genotypes were detected [Table 1].
Table 1.
Comparison of PANDAS patient and control groups according to polymorphisms and gender
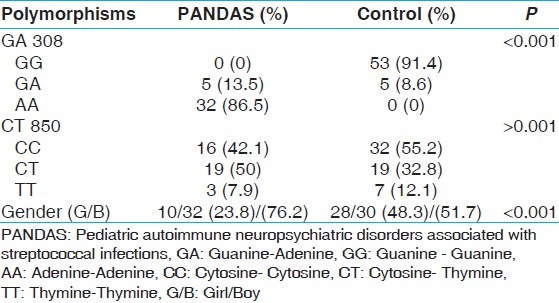
For −850 C/T polymorphism, 38 of 42 PANDAS patients’ results were obtained [Table 1]. In the PANDAS patients group, 16 normal CCpolymorphism (42.1%), 19 polymorphic CT polymorphism (50%), and 3 TT (7.9%) genotypes were detected. In the control group, 19 polymorphic CT genotype (32.8%) and 7 polymorphic TT genotype (12.1%) were detected. However, the majority of genotypes consist of 32 normal CC genotypes (55.2%). Thirty two of the PANDAS patients (76%) and 30 of the control group (51.7%) were boys [Table 1].
According to our statistical results, there is a positive association between the PANDAS patients and − 308 G/A polymorphism (Chi-square value = 84.486, P < 0.001) but no association for −850 C/T polymorphism was observed (Chi-square value = 2.892, P = 0.235). In addition, we evaluated ASO titers of the patients to see if high levels of ASO titers affect the disease prognosis. We also compared the PANDAS patients’ ASO titers; however, we could not compare them with ASO titers of the control group since we had only ASO titer values of the patient group. There was no positive association between −308 G/A polymorphism-ASO titers (Mann Whitney = Z= −0.489, P = 0.651) and −850 C/T polymorphism-ASO titers (Kruskal-Wallis Chi-square value = 0.496, P = 0.780). We, however, found a positive relationship between disease and gender of the PANDAS patients (boys) (Chi-square value = 13.027, P = 0.001). We know that boys are generally affected more than girls with PANDAS8 but we could not find a positive relationship between gender of the patients and ASO titers (Mann-Whitney = Z = −0. 753, P = 0.457). In addition to these factors, frequent infections are very strong determinants and typical features of PANDAS.
Discussion
In our country, GABHS infections occurring in childhood period are much more common than other countries.[34–36] Some of the patients delay treatment because of not going to the doctor in time or don’t take enough care for their disease. Because of unconscious use of antibiotics, suppression of immune system, we took into consideration these conditions and decided to study. We know GABHS infections are associated with OCD/PANDAS symptoms.[35–38] We studied two polymorphisms of TNF-α gene and ASO titers of patients. According to our statistical results, we have demonstrated a positive association between TNF-α −308 G/A and the PANDAS susceptibility but there is no association for − 850 C/T polymorphism with the PANDAS. In different parts of the world, studies conducted for different OCD patients have variable results. Hounie’s et al. results are in consistent with our results.[37] According to their report, −308 G/A polymorphism is strongly associated with OCD.[20] Rheumatic fever (RF) is a disease that occurs after GABHS infections. RF/rheumatic heart disease is an inflammatory disease that occurs after GABHS infections. It is believed to be caused by similar mechanism of PANDAS. Another study supporting our study is made by Rajendranath et al. with RF patients. They found that − 308 G/A polymorphism is associated with RF.[38] In contrast to, Zai’s et al. who stated that TNF-α gene − 308 G/A polymorphism is not associated with OCD in Canadian patients.[38] Especially, we can see the remarkable effects of − 308 G/A polymorphism on phenotype-genotype relations because of the increased frequency of polymorphic genotypes in the PANDAS patients. If the PANDAS patients are not treated for longer periods, schizophrenic symptoms may be unavoidable because of the damage in particular parts of the brain. Boin et al. found significant association between − 308 G/A polymorphism and schizophrenia.[39] We didn’t find statistically significant difference among ASO titers, −308 G/A and − 850 C/T polymorphism. In other words, ASO is not a determinant for both polymorphisms. According to some investigators; there hasn’t been any relationship between ASO titers among children with OCD only, OCD + PANDAS, OCD + Chronic Tic Disorder (CTD) patients and the control group.[9,10] In contrast, the results of another study revealed positive relationship between ASO titer and severity of tic disorder for 150 consecutive children presenting with tics.[23,40–42] In another study of 105 patients diagnosed with CTD, OCD or attention-deficit hyperactivity disorder (ADHD), ASO titers were definitive. They found that ASO titers of ADHD patients were significantly increased.[24,25] Furthermore, we found that boys are affected more compared to girls and gender of a patient was a significant factor for the disease. However, if we consider gender frequency for boys and girls who were not equal to each other, it seems like boys has more tendency for PANDAS genotypically. We think that it will be more appropriate to reach this conclusion when the number of boys and girls are equal to each other with broader sampling groups. As a secondary reason, for this difference could be the fact that the 6p21 chromosomal region where MHC locus resides along with TNF-α is a fragile site which support the findings that this syndrome is autoimmune-based.[43,44] Moreover, considering the fact that FRAXE-associated mental retardation protein (FMR 2) and FAM IIA genes located on fragile X E site ((folic acid sensitive site of Xq28, FRAXE) and FRAXF loci on X chromosome, respectively, are fragile sites associated with mental retardation, we could say that chromosomes other than X chromosome are also important on the higher tendency of boys to have PANDAS.[43,44] Through the new comprehension of the diseases, we can say epigenetic mechanism plays role for inactivation of some genes therefore, we have to look in a larger perspective for the disease. In many multifactorial and single gene neurodegenerative disorders, the symptoms are similar, but also these are the common characteristics of polygenic traits.[45] In addition, there are symptoms which differ from patient-to-patient. For that reason, simultaneous expression profiles of immune system genes should be investigated as well. The most compelling aspect of our research is the finding that TNF-α −308 promoter region AA polymorphism was detected in 86.5% of patients but not in controls which makes it a possible indicator to be evaluated in pre-disposition to PANDAS, however, due to the low sampling number our work should be supported with further research employing higher sampling numbers. In conclusion, we propose that TNF-α −308 AA polymorphism can be regarded as a definitive and molecular indicator of PANDAS which should be supported by further research on this issue.
Conclusion
We propose that TNF-α −308 AA polymorphism can be regarded as a definitive and molecular indicator of PANDAS, however, our findings should be supported by further research on this issue.
Footnotes
Source of Support: Scientific research foundation of Cukurova University
Conflict of Interest: None declared.
References
- 1.Dale RC, Heyman I. Post-streptococcal autoimmune psychiatric and movement disorders in children. Br J Psychiatry. 2002;181:188–90. doi: 10.1192/bjp.181.3.188. [DOI] [PubMed] [Google Scholar]
- 2.Hirschtritt ME, Hammond CJ, Luckenbaugh D, Buhle J, Thurm AE, Casey BJ, et al. Executive and attention functioning among children in the PANDAS subgroup. Child Neuropsychol. 2009;15:179–94. doi: 10.1080/09297040802186899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morris CM, Pardo-Villamizar C, Gause CD, Singer HS. Serum autoantibodies measured by immunofluorescence confirm a failure to differentiate PANDAS and Tourette syndrome from controls. J Neurol Sci. 2009;276:45–8. doi: 10.1016/j.jns.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 4.Murphy TK, Storch EA, Turner A, Reid JM, Tan J, Lewin AB. Maternal history of autoimmune disease in children presenting with tics and/or obsessive-compulsive disorder. J Neuroimmunol. 2010;229:243–7. doi: 10.1016/j.jneuroim.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marconi D, Limpido L, Bersani I, Giordano A, Bersani G. PANDAS: A possible model for adult OCD pathogenesis. Riv Psichiatr. 2009;44:285–98. [PubMed] [Google Scholar]
- 6.Martino D, Defazio G, Giovannoni G. The PANDAS subgroup of tic disorders and childhood-onset obsessive-compulsive disorder. J Psychosom Res. 2009;67:547–57. doi: 10.1016/j.jpsychores.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Yaddanapudi K, Hornig M, Serge R, De Miranda J, Baghban A, Villar G, et al. Passive transfer of streptococcus-induced antibodies reproduces behavioral disturbances in a mouse model of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection. Mol Psychiatry. 2010;15:712–26. doi: 10.1038/mp.2009.77. [DOI] [PubMed] [Google Scholar]
- 8.Derenne JL. Abrupt-onset obsessive-compulsive disorder (OCD) in a child with Crohn’s disease. Psychosomatics. 2009;50:425–6. doi: 10.1176/appi.psy.50.4.425. [DOI] [PubMed] [Google Scholar]
- 9.Snider LA, Swedo SE. Childhood-onset obsessive-compulsive disorder and tic disorders: Case report and literature review. J Child Adolesc Psychopharmacol. 2003;13:S81–8. doi: 10.1089/104454603322126377. [DOI] [PubMed] [Google Scholar]
- 10.Gause C, Morris C, Vernekar S, Pardo-Villamizar C, Grados MA, Singer HS. Antineuronal antibodies in OCD: Comparisons in children with OCD-only, OCD+chronic tics and OCD+PANDAS. J Neuroimmunol. 2009;214:118–24. doi: 10.1016/j.jneuroim.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Chapman AH, Pilkey L, Gibbons MJ. A psychosomatic study of eight children with Sydenham’s chorea. Pediatrics. 1958;21:582–95. [PubMed] [Google Scholar]
- 12.Swedo SE, Rapoport JL, Cheslow DL, Leonard HL, Ayoub EM, Hosier DM, et al. High prevalence of obsessive-compulsive symptoms in patients with Sydenham’s chorea. Am J Psychiatry. 1989;146:246–9. doi: 10.1176/ajp.146.2.246. [DOI] [PubMed] [Google Scholar]
- 13.Arnold PD, Richter MA. Is obsessive-compulsive disorder an autoimmune disease. CMAJ. 2001;165:1353–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Swedo SE, Leonard HL, Rapoport JL. The pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS) subgroup: Separating fact from fiction. Pediatrics. 2004;113:907–11. doi: 10.1542/peds.113.4.907. [DOI] [PubMed] [Google Scholar]
- 15.Fernández Ibieta M, Ramos Amador JT, Auñón Martínc I, Marín MA, González Tomé MI, Simón de Las Heras R. Neuropsychiatric disorders associated with streptococci: A case report. An Pediatr (Barc) 2005;62:475–8. doi: 10.1157/13074623. [DOI] [PubMed] [Google Scholar]
- 16.Hoekstra PJ, Minderaa RB. Tic disorders and obsessive-compulsive disorder: Is autoimmunity involved. Int Rev Psychiatry. 2005;17:497–502. doi: 10.1080/02646830500382003. [DOI] [PubMed] [Google Scholar]
- 17.Swedo SE, Grant PJ. Annotation: PANDAS: A model for human autoimmune disease. J Child Psychol Psychiatry. 2005;46:227–34. doi: 10.1111/j.1469-7610.2004.00386.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim SW, Grant JE, Kim SI, Swanson TA, Bernstein GA, Jaszcz WB, et al. A possible association of recurrent streptococcal infections and acute onset of obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci. 2004;16:252–60. doi: 10.1176/jnp.16.3.252. [DOI] [PubMed] [Google Scholar]
- 19.Singer HS, Loiselle C. PANDAS: A commentary. J Psychosom Res. 2003;55:31–9. doi: 10.1016/s0022-3999(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu E, Hashimoto K, Iyo M. The neurobiological approaches to obsessive-compulsive disorder. Nihon Shinkei Seishin Yakurigaku Zasshi. 2002;22:111–9. [PubMed] [Google Scholar]
- 21.Swedo SE. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) Mol Psychiatry. 2002;7:S24–5. doi: 10.1038/sj.mp.4001170. [DOI] [PubMed] [Google Scholar]
- 22.Lewin AB, Storch EA, Geffken GR, Goodman WK, Murphy TK. A neuropsychiatric review of pediatric obsessive-compulsive disorder: Etiology and efficacious treatments. Neuropsychiatr Dis Treat. 2006;2:21–31. [PMC free article] [PubMed] [Google Scholar]
- 23.Church AJ, Dale RC. Antistreptolysin-O titers: Implications for adult PANDAS. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. Am J Psychiatry. 2002;159:320. doi: 10.1176/appi.ajp.159.2.320. [DOI] [PubMed] [Google Scholar]
- 24.Morer A, Viñas O, Lázaro L, Calvo R, Andrés S, Bosch J, et al. Subtyping obsessive-compulsive disorder: Clinical and immunological findings in child and adult onset. J Psychiatr Res. 2006;40:207–13. doi: 10.1016/j.jpsychires.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Irak M, Flament MF. Neuropsychological profile of childhood-onset obsessive-compulsive disorder. Turk Psikiyatri Derg. 2007;18:293–301. [PubMed] [Google Scholar]
- 26.Moretti G, Pasquini M, Mandarelli G, Tarsitani L, Biondi M. What every psychiatrist should know about PANDAS: A review. Clin Pract Epidemiol Ment Health. 2008;4:13. doi: 10.1186/1745-0179-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dale RC. Autoimmunity and the basal ganglia: New insights into old diseases. QJM. 2003;96:183–91. doi: 10.1093/qjmed/hcg026. [DOI] [PubMed] [Google Scholar]
- 28.Shulman ST. Pediatric autoimmune neuropsychiatric disorders associated with streptococci: Update. Curr Opin Pediatr. 2009;21:127–30. doi: 10.1097/MOP.0b013e32831db2c4. [DOI] [PubMed] [Google Scholar]
- 29.Walker KG, Lawrenson J, Wilmshurst JM. Neuropsychiatric movement disorders following streptococcal infection. Dev Med Child Neurol. 2005;47:771–5. doi: 10.1017/S0012162205001611. [DOI] [PubMed] [Google Scholar]
- 30.Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramasawmy R, Faé KC, Spina G, Victora GD, Tanaka AC, Palácios SA, et al. Association of polymorphisms within the promoter region of the tumor necrosis factor-alpha with clinical outcomes of rheumatic fever. Mol Immunol. 2007;44:1873–8. doi: 10.1016/j.molimm.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Kato T, Honda M, Kuwata S, Juji T, Kunugi H, Nanko S, et al. Novel polymorphism in the promoter region of the tumor necrosis factor alpha gene: No association with narcolepsy. Am J Med Genet. 1999;88:301–4. doi: 10.1002/(sici)1096-8628(19990820)88:4<301::aid-ajmg4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 33.Pazarbaþi A, Kasap M, Güzel AI, Kasap H, Onbaþioðlu M, Ozbakir B, et al. Polymorphisms in the tumor necrosis factor-alpha gene in Turkish women with pre-eclampsia and eclampsia. Acta Med Okayama. 2007;61:153–60. doi: 10.18926/AMO/32904. [DOI] [PubMed] [Google Scholar]
- 34.Kara A. Tonsillopharyngitis. J Pediatr Infect. 2009;3:25–34. [Google Scholar]
- 35.Giulino L, Gammon P, Sullivan K, Franklin M, Foa E, Maid R, et al. Is parental report of upper respiratory infection at the onset of obsessive-compulsive disorder suggestive of pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection. J Child Adolesc Psychopharmacol. 2002;12:157–64. doi: 10.1089/104454602760219199. [DOI] [PubMed] [Google Scholar]
- 36.Swedo SE, Leonard HL, Garvey M, Mittleman B, Allen AJ, Perlmutter S, et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: Clinical description of the first 50 cases. Am J Psychiatry. 1998;155:264–71. doi: 10.1176/ajp.155.2.264. [DOI] [PubMed] [Google Scholar]
- 37.Hounie AG, Cappi C, Cordeiro Q, Sampaio AS, Moraes I, Rosário MC, et al. TNF-alpha polymorphisms are associated with obsessive-compulsive disorder. Neurosci Lett. 2008;442:86–90. doi: 10.1016/j.neulet.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 38.Zai G, Arnold PD, Burroughs E, Richter MA, Kennedy JL. Tumor necrosis factor-alpha gene is not associated with obsessive-compulsive disorder. Psychiatr Genet. 2006;16:43–5. doi: 10.1097/01.ypg.0000185026.12687.92. [DOI] [PubMed] [Google Scholar]
- 39.Boin F, Zanardini R, Pioli R, Altamura CA, Maes M, Gennarelli M. Association between-G308A tumor necrosis factor alpha gene polymorphism and schizophrenia. Mol Psychiatry. 2001;6:79–82. doi: 10.1038/sj.mp.4000815. [DOI] [PubMed] [Google Scholar]
- 40.Cardona F, Orefici G. Group A streptococcal infections and tic disorders in an Italian pediatric population. J Pediatr. 2001;138:71–5. doi: 10.1067/mpd.2001.110325. [DOI] [PubMed] [Google Scholar]
- 41.Leonard HL, Swedo SE. Paediatric autoimmune neuropsychiatric disorders associated with streptococcal infection. Int J Neuropsychopharmacol. 2001;4:191–8. doi: 10.1017/S1461145701002371. [DOI] [PubMed] [Google Scholar]
- 42.Bektaº D, Çaylan R, Çaylan R. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. Tur Clin. 2004;4:120–4. [Google Scholar]
- 43.Demirhan O, Tastemir D, Sertdemir Y. Chromosomal fragile sites in schizophrenic patients. Genetika. 2006;42:985–92. [PubMed] [Google Scholar]
- 44.Gu Y, Shen Y, Gibbs RA, Nelson DL. Identification of FMR2, a novel gene associated with the FRAXE CCG repeat and CpG island. Nat Genet. 1996;13:109–13. doi: 10.1038/ng0596-109. [DOI] [PubMed] [Google Scholar]
- 45.Luleyap HU, Onatoglu D, Tahiroglu AY, Alptekin D, Yilmaz MB, Cetiner S, Pazarbasi A, Unal I, Avcý A. Association between obsessive compulsive disorder and tumor necrosis factor-α gene -308 (G>A) and -850 (C>T) polymorphisms in Turkish children. BJMG. 2012;15:61–66. doi: 10.2478/bjmg-2013-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]