Abstract
OBJECTIVE:
Proteus syndrome (PS) is characterized by patchy or segmental overgrowth and hyperplasia of multiple tissues and organs, along with susceptibility to development of tumors. Very few cases are reported in literature from developing countries. Due to certain overlapping features with other overgrowth syndromes, diagnosis is usually delayed. Our aim was to describe clinical profile of this rare condition in six patients.
MATERIALS AND METHODS:
Retrospective case sheet review of patients followed in a Pediatric Genetic and Metabolic clinic at a tertiary care institute of North India with a diagnosis of hemihypertrophy/overgrowth syndrome.
RESULTS:
Six cases presented with asymmetric overgrowth and peculiar features suggestive of PS were included in this study. Age at presentation was 2 months to 10 years; two were males and four were females. Hemihypertrophy was noticed in only one case at birth, and focal overgrowths in rest of other patients were seen later during childhood.
CONCLUSION:
Due to certain overlapping features with other overgrowth syndromes, diagnosis of PS is usually delayed. Pediatricians are the first persons who come across such patients and they should be aware about this rare condition.
Keywords: Hamartoma, hemihypertrophy, lipoma, localized overgrowth, macrodactyly
Introduction
Proteus syndrome (PS) is a rare postnatal overgrowth disorder affecting multiple tissue including bone, soft-tissue, and skin. First described by Cohen and Heyden in 1979,[1,2] Wiedemann et al. in 1983 given the name of "PS" to this distinct entity.[3] It is a complex hamartomatous condition characterized by partial gigantism of hands, feet or both, plantar hyperplasia, hemangiomas, lipomas, lymphangiomas, varicosities, verrucous epidermal nevi, macrocephaly; cranial exostosis, and asymmetry of the limbs because of long bone overgrowth.[4] Until recently approximately 200 cases of PS has been reported in literature. Only a few isolated cases have been reported from India.[5,6] So we thought it would be relevant to report this case series as several aspects of this condition are important for pediatricians, as pediatricians are the first person to encounter such cases. Over a period of 3 years, six patients with Proteus and Proteus like syndromes were seen. Their clinical profile and disease characteristics are described.
Materials and Methods
Between January 2008 and December 2010, we retrospectively reviewed the case profile of nine patients who presented with localized over-growth and/or hemihypertrophy in the out-patient clinic of Genetic and Metabolic unit of Department of Pediatrics. Six patients were included in this analysis. Three cases were excluded from the study because their clinical features were consistent with other diagnosis. The clinical evaluation was done by expert clinical geneticist. Information about demographic profile and presenting complaints were obtained. Detailed clinical examination was done for extent of overgrowth, other associated manifestations, anthropometric profile, and complications. The diagnosis of PS was kept on the basis of clinical features, and radiological findings as per the criteria recommended by Biesecker et al.[7]
Results
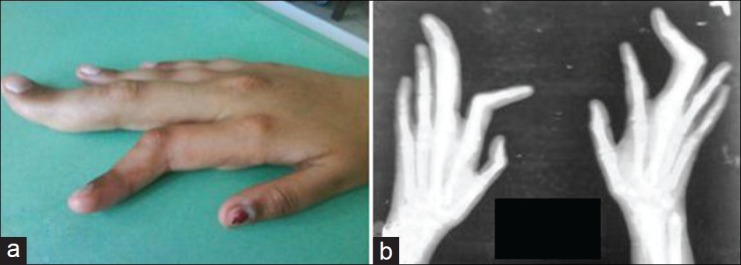
Among the nine short-listed cases, one patient had hemi-hypertrophy and he had history of hypoglycemia and omphalocele at birth, so he was diagnosed as a case of "Beckwith Weidemann syndrome" (BWS) and excluded from analysis. Two cases were diagnosed as "Macrocephaly-capillary malformation syndrome" (M-CM) as per diagnostic criteria described by Martínez-Glez et al.[8] Of the six patients included in final analysis; two patients were male and four were female. Age range of the patients at presentation was between 2 months and 10 years. Most common presenting features which brought them to notice of the clinician were focal over-growth and asymmetry. Hemihypertrophy was noticed in one patient at birth, and focal over-growths in rest of other patients were noticed later in life. The clinical profiles of each of these cases are presented in [Table 1]. Three patients had dysmorphic facies, one patient had strawberry hemangioma on face and one patient had lipoma over scapular area. Cerebriform connective tissue nevi (CCTN) were seen in two patients at palmar aspect. Two patients had developmental delay; and among them magnetic resonance imaging (MRI) was suggestive of megalencephaly in one and lissencephaly in other (case 2 and 5, respectively) [Table 1]. Sonography of abdomen for internal organ visceromegaly was done in all patients but visceromegaly or internal hemangiomas were not detected. A 10-year-old girl presented with facial deformity, swelling over forehead, hemihypertrophy involving lower limbs, macrodactyly [Figure 1a] and pigmentation anomalies and her X-ray showed macrodactyly [Figure 1b], tibial bowing, and hyperostosis in skull [Figure 2].
Table 1.
Clinical and demographic profile of six patients with proteus and proteus like syndromes
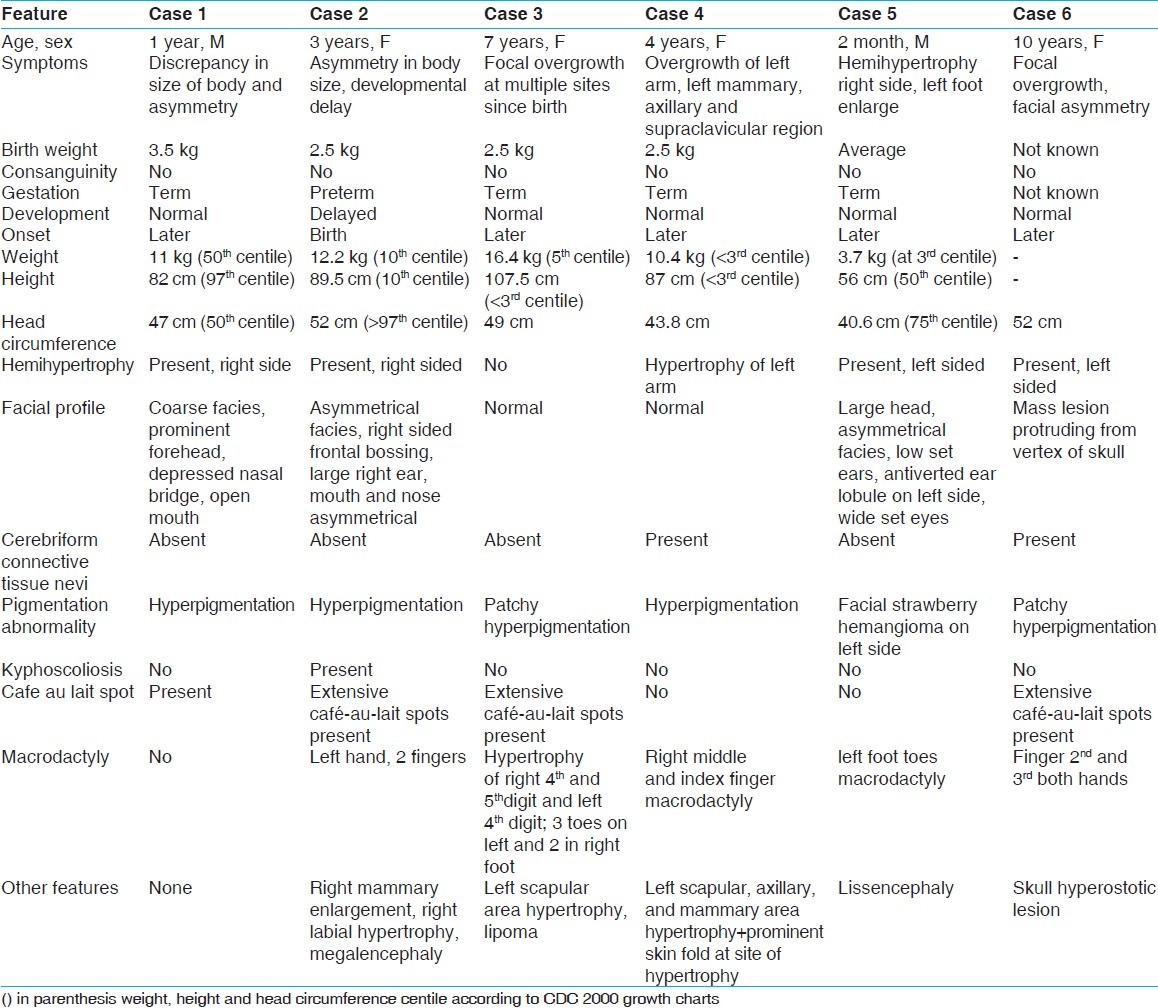
Figure 1.
(a) Asymmetric and disproportionate over growth of right hand fingers with macrodactyly in a patient with Proteus syndrome; (b) X - ray of both the hands showing bony over growth in the same patient
Figure 2.

X - ray skull showing Hyperostotic lesion over vertex (arrow) in a girl with Proteus syndrome
Discussion
PS is a rare congenital disorder that produces multifocal over-growth of tissue. It may affect tissues derived from any of the three germinal layers.[1,9] Hallmark of this disorder is the random or mosaic distribution of its manifestations throughout the body. Klippel-Trénaunay syndrome and Hemi hyperplasia-multiple lipomatosis syndromes are the entities most commonly confused with PS.[10] Other disorders like BWS, Banayan-Zonana, Neurofibromatosis type 1, encephalocraniocutaneous lipomatosis and M-CM syndrome also have similarities to PS.[11] During analysis of present series we also excluded three cases with alternate diagnoses.
Signs of this sporadic syndrome may include over-growth of the long bones, asymmetric macrocephaly, asymmetric over-growth, vertebral anomalies, hyperostosis, partial gigantism of hands or feet, limb asymmetry, connective-tissue nevi, lipomas, and vascular malformations.[2,3,10] Visceral anomalies such as splenomegaly, asymmetric megalencephaly, white-matter abnormalities, and nephromegaly, as well as malformations involving fatty, muscular, and vascular tissue are seen.[1,4,12]
Diagnosis of PS was based on criteria provided by Biesecker et al.[1] General criteria were fulfilled by all cases in present series. Category A criteria was fulfilled by only two patients who had CCTN at palmar aspect. CCTN is hall-mark of the disease, and it can occur on plantar surface of foot, palmar aspect of hand, or rarely on chest, abdomen, back, lateral and dorsal aspect of fingers, and on nose.[13,14] Presence of single CCTN is sufficient for making diagnosis of PS. CCTN is never reported at birth, usually appears later in life and it is progressive throughout childhood.
Dermatological manifestations of PS as reported by Beachkofsky et al., CCTN was present among 94% of their 36 patients.[14] Among category B, although epidermal nevus was not seen in any of our patients, pigmentation abnormality was present in all: Café-au-lait spots and areas of patchy hyperpigmentation with hypopigmentation. Strawberry hemangioma was present on face in one patient. Other dermatological manifestation reported are epidermal nevi, cutaneous vascular malformations including capillary, venous, lymphatic or combined malformation, lipoma, partial lipohypoplasia and patchy dermal hyperplasia.[14]
Extracutaneous manifestations include skeletal and visceral over-growth, tumors, cyst, vascular abnormality, deformity, and hypoplasia or maldevelopment. All patients usually have disproportionate overgrowth of hands and feet and it may involve fingers and toes in the form of macrodactyly. Overgrowth in PS is not only disproportionate and asymmetric, but also progressive and distorting.[4,14,15] Four patients had hemihypertrophy and four had macrodactyly involving fingers as well as toes. In two patients, underlying bony overgrowths was also noticed in X-ray of the hand [Figure 1b]. Disproportionate overgrowth was present at birth in one patient and among rest it was observed in later life. Abnormalities of bony cortex with deficiency of overlying soft tissue can be seen in radiograph. One girl in present series had hyperostosis on vertex of skull [Figure 2].
Lipomas are the most common tumor type in PS. Other tumors which are specific of PS like bilateral ovarian cystadenoma and parotid monomorphic adenoma usually seen in second decade of life. Other tumors reported are meningioma, testicular tumor, astrocytoma, optic nerve tumor, breast intraductal papilloma and they also can have simultaneously multiple tumors.[9,16] One patient had lipoma over scapular area. None had any other tumor during follow-up. Facial dysmorphism was present in three patients. One had coarse facies, prominent forehead, widely spaced eyes, depressed nasal bridge, and open mouth. Two other patients had asymmetrical facies with large head, large ears and low set ear on the side of hemimhypertophy. Developmental delay was present in one patient and his MRI showed megalencephaly. She also had kyphoscoliosis, right sided mammary hyperplasia as well as enlargement of right sided labia (case 2). One more patient who presented at 2 month of age had MRI changes suggestive of lissencephaly. Up to 40% of patients can have central nervous system (CNS) manifestations including mental retardation and 71% can have kyphoscoliosis and chest wall asymmetry.[4,14] When the features of PS are fully established, the diagnosis is not difficult, however, in early childhood, tissue over-growth, epidermal nevi or vascular malformation may not be evident. Characteristic lesions may not be seen at birth, only they can have subtle facial asymmetry or mild hemihyperplasia. The characteristic asymmetrical disproportionate over-growth is seen in 17% patients and 43% have epidermal nevi or vascular malformation at birth.[4,7] Therefore, diagnosis is usually delayed until the lesions are fully expressed in later childhood or adolescence.
PS has been reported in discordant monozygotic twins.[15] Pathogenesis behind PS is a somatic mutation that is lethal when constitutively expressed.[4] A somatic mutation arises in a somatic cell and is thus present only in that cell and the lineages to which it gives rise, rather than being present in the conceptus and thus constitutively present in every cell of the body.[15] Management should be directed towards functional improvement. Patients with limb length discrepancy, joint immobility and macrodactyly are best managed by team consisting of pediatrician, orthopedic surgeon, plastic surgeon and occupational therapist.
Conclusion
PS is characterized by progressive mosaic over-growth of skin, bone, muscle, and fatty tissue. The variable signs of PS makes the diagnosis challenging. A multidisciplinary approach is needed with follow-up for detection and management of complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Biesecker L. The challenges of proteus syndrome: Diagnosis and management. Eur J Hum Genet. 2006;14:1151–7. doi: 10.1038/sj.ejhg.5201638. [DOI] [PubMed] [Google Scholar]
- 2.Cohen MM, Jr, Hayden PW. A newly recognized hamartomatous syndrome. Birth Defects Orig Artic Ser. 1979;15:291–6. [PubMed] [Google Scholar]
- 3.Wiedemann HR, Burgio GR, Aldenhoff P, Kunze J, Kaufmann HJ, Schirg E. The proteus syndrome. Partial gigantism of the hands and/or feet, nevi, hemihypertrophy, subcutaneous tumors, macrocephaly or other skull anomalies and possible accelerated growth and visceral affections. Eur J Pediatr. 1983;140:5–12. doi: 10.1007/BF00661895. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MM., Jr Proteus syndrome: An update. Am J Med Genet C Semin Med Genet. 2005;137C:38–52. doi: 10.1002/ajmg.c.30063. [DOI] [PubMed] [Google Scholar]
- 5.Sinha C, Gupta B, Kaur M, Kumar A, Dey CK. Proteus syndrome: A medical rarity. Saudi J Anaesth. 2011;5:233–4. doi: 10.4103/1658-354X.82818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dalal AB, Phadke SR, Pradhan M, Sharda S. Hemihyperplasia syndromes. Indian J Pediatr. 2006;73:609–15. doi: 10.1007/BF02759927. [DOI] [PubMed] [Google Scholar]
- 7.Turner JT, Cohen MM, Jr, Biesecker LG. Reassessment of the Proteus syndrome literature: Application of diagnostic criteria to published cases. Am J Med Genet A. 2004;130A:111–22. doi: 10.1002/ajmg.a.30327. [DOI] [PubMed] [Google Scholar]
- 8.Martínez-Glez V, Romanelli V, Mori MA, Gracia R, Segovia M, González-Meneses A, et al. Macrocephaly-capillary malformation: Analysis of 13 patients and review of the diagnostic criteria. Am J Med Genet A. 2010;152A:3101–6. doi: 10.1002/ajmg.a.33514. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MM., Jr Proteus syndrome: Clinical evidence for somatic mosaicism and selective review. Am J Med Genet. 1993;47:645–52. doi: 10.1002/ajmg.1320470514. [DOI] [PubMed] [Google Scholar]
- 10.Biesecker LG, Happle R, Mulliken JB, Weksberg R, Graham JM, Jr, Viljoen DL, et al. Proteus syndrome: Diagnostic criteria, differential diagnosis, and patient evaluation. Am J Med Genet. 1999;84:389–95. doi: 10.1002/(sici)1096-8628(19990611)84:5<389::aid-ajmg1>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 11.Satter E. Proteus syndrome: 2 case reports and a review of the literature. Cutis. 2007;80:297–302. [PubMed] [Google Scholar]
- 12.Türk CY, Güney A, Oner M, Halýcý M. An unusual initial presentation of Proteus syndrome: Macrosyndactyly. Eklem Hastalik Cerrahisi. 2011;22:56–9. [PubMed] [Google Scholar]
- 13.Beachkofsky TM, Sapp JC, Biesecker LG, Darling TN. Progressive overgrowth of the cerebriform connective tissue nevus in patients with Proteus syndrome. J Am Acad Dermatol. 2010;63:799–804. doi: 10.1016/j.jaad.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen D, Turner JT, Olsen C, Biesecker LG, Darling TN. Cutaneous manifestations of proteus syndrome: Correlations with general clinical severity. Arch Dermatol. 2004;140:947–53. doi: 10.1001/archderm.140.8.947. [DOI] [PubMed] [Google Scholar]
- 15.Lindhurst MJ, Sapp JC, Teer JK, Johnston JJ, Finn EM, Peters K, et al. A mosaic activating mutation in AKT1 associated with the Proteus syndrome. N Engl J Med. 2011;365:611–9. doi: 10.1056/NEJMoa1104017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gordon PL, Wilroy RS, Lasater OE, Cohen MM., Jr Neoplasms in Proteus syndrome. Am J Med Genet. 1995;57:74–8. doi: 10.1002/ajmg.1320570117. [DOI] [PubMed] [Google Scholar]


