Abstract
Background
The behavioral and psychological symptoms associated with dementia (BPSD) can be burdensome to informal/family caregivers, negatively affecting mental health and expediting the institutionalization of patients. Because the dementia patient–caregiver relationship extends over long periods of time, it is useful to examine how BPSD impact caregiver depressive symptoms at varied stages of illness. The goal of this study was to assess the association of BPSD that occur during early stage dementia with subsequent caregiver depressive symptoms.
Methods
Patients were followed from the early stages of dementia every six months for up to 12 years or until death (n = 160). Caregiver symptoms were assessed on average 4.5 years following patient’s early dementia behaviors. A generalized estimating equation (GEE) extension of the logistic regression model was used to determine the association between informal caregiver depressive symptoms and BPSD symptoms that occurred at the earliest stages dementia, including those persistent during the first year of dementia diagnosis.
Results
BPSD were common in early dementia. None of the individual symptoms observed during the first year of early stage dementia significantly impacted subsequent caregiver depressive symptoms. Only patient agitation/aggression was associated with subsequent caregiver depressive symptoms (OR = 1.76; 95% CI = 1.04–2.97) after controlling for concurrent BPSD, although not in fully adjusted models.
Conclusions
Persistent agitation/aggression early in dementia diagnosis may be associated with subsequent depressive symptoms in caregivers. Future longitudinal analyses of the dementia caregiving relationship should continue to examine the negative impact of persistent agitation/aggression in the diagnosis of early stage dementia on caregivers.
Keywords: dementia caregiving, BPSD, behavioral symptoms
Introduction
The number of family members providing informal unpaid (i.e., non-professional or family) caregiving to individuals with dementia continues to increase (National Alliance for Caregiving and AARP, 2004). While these informal (unpaid) caregivers provide a critical service to family members in lieu of formal sources of long-term care, they often suffer from chronic stress which results in negative consequences for the caregiver’s mental and physical health (Aneshensel et al., 1995; Pinquart and Sorensen, 2003). The behavioral and psychological symptoms associated with dementia (BPSD), which consist of a wide variety of patient behaviors, including depression, physical aggression, and paranoid delusions, are highly prevalent in patients with dementia over the course of their illness (Lyketsos et al., 2002; Steinberg et al., 2003). Although cognitive decline is considered the clinical hallmark of dementia, an extensive body of literature suggests that BPSD are particularly burdensome to caregivers and may eventually lead to decisions to institutionalize patients (Black and Almeida, 2004).
The length of time an informal caregiver spends caring for the patient is significant. According to the National Alliance for Caregiving and AARP (2004), the average caregiver serves in their caregiving capacity for 4.3 years. Caregivers of people with Alzheimer’s disease (AD) and other dementias provide more hours of help, on average, than caregivers of other older people and serve in their caregiving role for longer periods of time. Thirty-two percent of caregivers serve in their role for five or more years (Alzheimer’s Association, 2012). Yet relatively few caregiving studies to date (e.g., Aneshensel et al., 1995) adopt longitudinal designs to determine potential predictors of caregiver psychosocial adaptation over time (Pinquart and Sorensen, 2003). Among studies that have examined BPSD and its impact on caregiving, the vast majority have been cross-sectional studies (Black and Almeida, 2004; Ornstein and Gaugler, 2012).
This paper examines the association between BPSD and caregiver depressive symptoms using the stress process model as a conceptual framework and a life course epidemiological approach. According to the stress process model (Pearlin et al., 1990; Aneshensel et al., 1995), caregiving is a chronic stressor that gives rise to strains from multiple domains and ultimately leads to increased risk for psychiatric distress and diagnosable disorder, including depression. The model differentiates between objective stressors (e.g., BPSD), the caregiver’s subjective experience of those stressors, and background and contextual factors that impact the stressor and caregiver outcomes. Within life course epidemiology, the concept of a sensitive time period refers to a time period during which an exposure has a greater effect than outside the period (Ben-Shlomo and Kuh, 2002). While an exposure is always harmful, during the sensitive time period there is an increased risk. The beginning of the relationship may be a sensitive time period relative to negative caregiving outcomes within the patient–caregiver relationship. Unexpected entry into roles is known to be disruptive for individuals (Cottrell, 1942); this finding may be especially salient for those individuals who enter the official “unexpected career” of caregiving. Research suggests that among caregivers, those who have a more unexpected transition into their role have increased risk of depression and are more likely to institutionalize patients (Gaugler, et al., 2003).
Existing dementia caregiving research points to the critical role of timing in understanding the stress process and informal caregiver outcomes. For example, age of onset of dementia is inversely associated with time to nursing home placement (Stern et al., 1997). In addition, Gaugler et al. (2007) found that low resilience early in the caregiving career was associated with relinquishing the caregiver role at three years follow-up, suggesting that the caregiver’s experience earlier in the patient’s illness may be predictive of later outcomes. Together, these findings suggest that challenges that occur early in the caregiving career when signs of illness first appear may have lasting impact for the caregivers over the course of the patient’s illness. The unpredictable nature of BPSD, for example, may severely tax resources of caregivers new to their role such that features that occur early in the disease process may impact caregivers’ depressive symptoms independent of subsequent changes in disease course.
One study that specifically examined the impact of BPSD early in the caregiver–patient relationship (Gaugler et al., 2005) reported that severe behavioral symptoms early in caregiving were independent predictors of increased burden and depression over three years regardless of later BPSD development. This study, however, did not follow patients from disease onset prospectively, but instead relied on caregiver reports of care duration. We therefore do not fully know how symptoms that occur early in the disease course impact subsequent caregiver outcomes. Further research is warranted which follows patients when they are at the earliest stages of their illness to assess how the timing of BPSD impact depressive symptoms for the caregiver. By studying the impact of timing of behaviors, we may be able to focus on specific stages of the patient–caregiver relationship in which intervention for caregivers would be most beneficial. In addition, given concerns about lack of safe long-term pharmacotherapy to treat BPSD (Ballard et al., 2009), knowledge of whether individual behaviors that occur early in the dementia process independently impact subsequent caregiver outcomes may better direct current treatment protocols.
Study aims
This study aims to assess the association between BPSD symptoms that occur early in dementia patients and subsequent depressive symptoms among informal caregivers. Based on life course frameworks of epidemiology and prior empirical research, we hypothesize that BPSD symptoms that occur early and are persistent during the course of dementia will be independently associated with subsequent caregiver depressive symptoms.
Methods
Sample
The Predictors 2 cohort consists of patients with probable AD and dementia with Lewy Bodies (DLB) who were followed prospectively from the earliest stages of dementia. Patients were recruited from memory disorder centers or private physician offices in three sites between 1997 and 2007: Columbia University College of Physicians and Surgeons; Johns Hopkins University School of Medicine; and Massachusetts General Hospital. All patients were diagnosed in a consensus conference with at least two faculty physicians specializing in dementia and one faculty neuropsychologist. All AD patients met the National Institute of Neurological and Communicative Disorders and Stroke (NINCDS)–Alzheimer’s Disease and Related Disorders Association (ADRDA) criteria for probable AD (McKhann et al., 1984), and intellectual impairment was documented with neuropsychological testing. At entry into the study, each AD participant was required to have relatively mild dementia operationalized as a modified Mini-Mental State Examination (MMSE) (Stern et al., 1987; Soto et al., 2006), or an MMSE score of ≥30, equivalent to a score of ≥16 on the Folstein Mini-Mental State Examination. Patients with DLB were diagnosed according to the 1996 consensus guidelines for probable disease (McKeith et al., 1996). Participants were required to have at least one informant available to assist with answering questions (informal or paid caregiver). Exclusion criteria were stroke, alcoholism, schizophrenia, schizoaffective disorder, and electroconvulsive treatments.
During an initial visit, the following data were collected about the patient via clinical assessment: medical history, neurological evaluation, presenting features of cognitive impairment, functional status, family history of dementia, onset dating and features, and BPSD. Follow-up data were collected at six-month intervals via outpatient visit thereafter until dropout or death, including: neurological evaluation, functional and cognitive status, medical and psychiatric history, and quality of life. If patients were unable to travel to the outpatient clinic for evaluation, they were visited at their homes, nursing homes, or healthcare facilities. There is 94% follow up of patients. Patients who did not respond at a particular visit could respond at a subsequent visit.
Beginning in 2004, we initiated the collection of detailed data on the demographics, mental health, and care activities provided by one informal caregiver of each patient in the Predictors 2 cohort, regardless of patient’s date of entry into Predictors study. This cohort of caregivers was called the “Caregiver Study.” Follow-up data on caregiver mental health status, level of care, and living situation were collected at six-month intervals up to six years simultaneous to the collection of data on patient cognitive, functional, and BPSD symptoms on the entire Predictors 2 cohort. A total of 169 patients were active in the Predictors 2 cohort at the time of, or subsequent to, the onset of the Caregiver Study. Of these patients, six did not have an eligible informal caregiver to complete the study (3.6%). Of the 163 eligible patient–caregiver dyads, 98.2% have caregiver data available for at least one assessment, and three caregivers refused to participate. We combined the following data for this study analysis: (1) early dementia behaviors measured during patient’s first year in the Predictors 2 study (baseline, six-month, and one-year assessments), and (2) all caregiver data collected during the Caregiver Study (baseline and all follow-up assessments). On average, early dementia patient behavioral symptoms were measured 4.5 years prior to follow-up caregiver symptom assessments (range = six months to 12 years). Multiple assessments per individual caregiver were included (range = 1 to 12; mean = 4). Figure 1 provides a diagram of the study timeline and the construction of our analytic cohorts.
Figure 1.
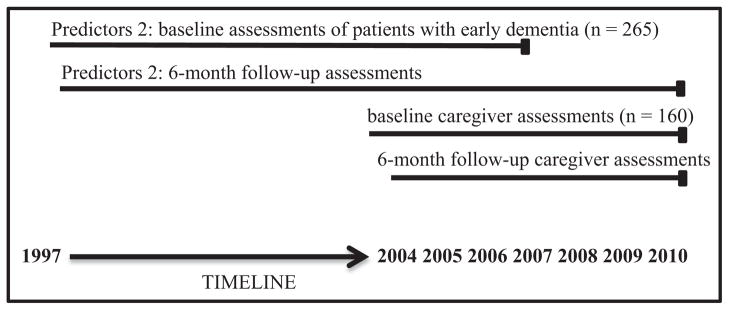
Predictors 2 cohort and caregiver study timeline.
Measures
Caregiver depressive symptoms were measured at six-month intervals by the six-item depression subsection of the Brief Symptom Inventory (BSI; Derogatis, 1993). Caregivers were asked how much during the past week they were bothered by the following: feeling lonely, feeling blue, feeling no interest in things, feeling hopeless about the future, feelings of worthlessness, and thoughts of ending your life using a five-point Likert scale response for each item ranging from “not at all” to “extremely.” A higher score indicates higher depressive symptoms. The mean score across six symptoms was calculated (mean = 1.4, standard deviation (SD) = 0.6). The standardized Cronbach’s coefficient α was >0.8, indicating acceptable reliability. Because data were highly skewed, BSI scores were dichotomized as few to no depressive symptoms (<2) and depressive symptoms (≥2). Although there is no standard clinical cut point for depressive symptomatology for this scale, previously published mean BSI depression scores for female elderly caregivers is <1 (Anthony-Bergstone and Zarit, 1988). Based on a previous work (Ornstein et al., 2013), we chose to use a more conservative higher cut point to discern meaningful differences in depressive symptoms among our sample of dementia caregivers. Using this method, caregivers categorized as having depressive symptoms indicated that on average each of the six symptoms bothered or impacted them from a minimal to extreme level. Symptom scores categorized as depressive were one SD above the mean depressive symptom score.
At entry to Predictors Study, the Columbia University Scale for Psychopathology in Alzheimer’s Disease (CUSPAD; Devanand et al., 1992) was used to measure patient BPSD. The CUSPAD is a semi-structured rating scale that a clinician or research assistant administers to the informant regarding the presence of 26 patient symptoms during the last month before each interview. Inter-rater reliabilities for individual symptoms range from κ coefficients of 0.6–0.7 (Devanand et al., 1992). We examined the following four symptom clusters and used a dichotomous variable to characterize the presence or absence of each symptom cluster as follows: (1) Patient depressive symptoms were defined as having (a) depressed mood and (b) either difficulty in sleeping or change in appetite. (2) Agitation/ aggression, included showing agitation or restlessness, making verbal outbursts, and being physically aggressive. (3) Psychotic symptoms consisted of hallucinations, illusions, and delusions. Finally, based on previous research that hypothesized aggressive and accusatory behavior cannot be easily dismissed by caregivers and may make the caregiver fearful of the patient (Ornstein et al., 2013), we also examined the impact of any aggressive or accusatory symptoms (e.g., physical violence or beliefs that people are stealing things and accusing caregiver of plotting to leave him/her). Given that these behaviors may be directed at the caregivers and are unlikely to be easily ignored, they may be particularly disturbing to the caregivers over time. Finally, we created a dichotomous variable (present/absent) to indicate the presence of any of the above four individual symptom behaviors presenting at patient cohort inception.
Each symptom cluster was examined (1) at study baseline only, and (2) over the course of the first year of the study. All symptoms documented as present at least two times over the course of the first year were considered as “persistent early symptoms.”
The following patient and caregiver characteristics are objective stressors and contextual factors that were examined as potential confounding variables and as sources of variation among groups of patient–caregiver dyads:
Patient cognitive status was assessed at study baseline and each subsequent visit using the MMSE in which higher score indicates better cognitive status. Patient functional status was assessed at each visit using parts I and II of the Blessed Dementia Rating Scale (BDRS; Blessed et al., 1968). Patients’ medical histories were used to construct a modified version of the Charlson Index of Comorbidity (Charlson et al., 1987). A modified Unified Parkinson’s Disease Rating Scale (UPDRS; Marcus et al., 1991) was administered at each visit to measure the presence or absence of extrapyramidal signs (EPS; e.g., tremors, rigidity). A dichotomous indicator was constructed for the use of EPS if any of the items were rated 2 or higher (0 being normal and 4 indicating maximum impairment). Patient’s age, ethnicity, sex, and the highest level of education were recorded at the inception of the Predictors cohort; and marital status was recorded at each visit. Duration of illness in years was estimated by a neurologist based on baseline interviews with the patient and the caregiver.
Caregiver’s age, gender, and relationship with patient were recorded when caregivers were initially assessed in the Predictors 2 study (i.e., “Caregiver study baseline”). Whether the caregiver lived with the patient and the frequency of contact with the patient were recorded at each visit. Whether the caregiver assisted with basic and instrumental activities of daily living (IADLs), the amount of hours the patient spent per day with the caregiver, whether a home health aide/home attendant assisted with care, and caregiver’s employment status were reported annually.
Statistical analysis
We tested the relationship between individual early dementia behaviors and caregiver depressive symptoms (1) unadjusted, (2) controlling for behavioral symptoms concurrent to caregiver depressive symptoms, and (3) controlling for potential confounding variables and concurrent patient behavioral symptoms at every assessment following the initiation of the caregiver study (see Figure 1). For 160 patient caregiver dyads n = 637 time points were examined ranging from 1 to 12 assessments per dyad. To account for repeated measures per dyad, we used a logistic model with a generalized estimating equation (GEE) extension. To determine which variables would be included in the final model, bivariate associations between (1) caregiver depressive symptoms and potential confounders and (2) individual early dementia BPSD and potential confounders were assessed. Variables that showed an effect approaching statistical significance with the outcome at the p < 0.1 level were associated with at least one symptom cluster, and were not highly correlated with other variables (correlation > 0.5) in the bivariate analysis were included in the final adjusted model.
Results
Baseline descriptive and clinical characteristics of the patient sample and their caregivers are depicted in Table 1. Mean patient age was 75.4 years, slightly more than half patients were females, and most were white. The vast majority (91.9%) had at least a High School education and almost two-thirds were married. Consistent with study enrollment criteria, patients were at early stages of illness with relatively mild levels of dementia. Average dependence score was 5.0 and functional status score was 3.7, indicating a mild level of dependence and high physical function. Accordingly, very few patients lived in a nursing home (3.8%) and only 11.9% required any home healthcare assistance.
Table 1.
Patient and caregiver characteristics at baseline for Predictors 2 cohort and caregiver study (n = 160)
| PATIENT
|
CAREGIVER
|
||||
|---|---|---|---|---|---|
| CHARACTERISTICS | CATEGORIES | PERCENTAGE / MEAN ± SD | PERCENTAGE / MEAN ± SD | ||
| Age | 75.4 ± 7.4 | 65.3 ± 14.4 | |||
| Gender | Female | 54.4% | 76.3% | ||
| Ethnicity | White | 90% | 91% | ||
| Other | 10% | 9% | |||
| Years of schooling | Mean ± SD | 14.7 ± 3.1% | 15.8 ± 3.3 | ||
| Less than HS | 8.1% | 5.0% | |||
| HS | 26.3% | 18.4% | |||
| Above HS | 65.6% | 76.6% | |||
| Marital status | Married | 63.1% | Work at least part-time for pay | Yes | 44.7% |
| Widowed | 28.1% | ||||
| Other | 8.8% | ||||
| Living status | Home | 89.4% | Relationship to patient | Spouse | 55% |
| Retirement home | 6.9% | Child | 36.3% | ||
| Nursing home | 3.8% | Other relative/friend | 8.7% | ||
| Site | Columbia University | 44.4% | Lives with patient | Yes | 89.4% |
| Johns Hopkins | 29.4% | ||||
| Mass General | 26.3% | ||||
| Diagnosis | AD | 86.3% | Assists patient with ADLs | Yes | 44.9% |
| DLB | 13.7% | ||||
| Neurologist estimation of duration of illness in years | Mean ± SD (range 1–18) | 4.8 ± 2.5 | Time spent daily assisting with IADLs | None | 18.9% |
| Up to 3 h | 52% | ||||
| 3 to 5 h | 20.3% | ||||
| 6 to 9 h | 4.1% | ||||
| 9 to 12 h | 1.4% | ||||
| >12 h | 3.4% | ||||
| MMSE score | Mean ± SD (range 9–30) | 22.7 ± 3.7 | |||
| Blessed Functional Activity scale score | Mean ± SD (range 0–13) | 3.7 ± 2.3 | |||
| Total dependence | Mean ± SD (range 0–12) | 5.0 ± 2.4 | |||
| Home health aide in last 3 months | Yes | 11.9% | |||
| Modified comorbidity index | 0 | 51.6% | |||
| ≥1 | 48.4% | ||||
| Extrapyramidal signs | Yes | 17.2% | |||
Note: SD = standard deviation; HS = High School; MMSE = Modified Mini-Mental State Examination; ADLs = Activities of daily living and include bathing, eating; IADLS = Instrumental activities of daily living and include shopping, housekeeping.
At the onset of the Caregivers Study, caregivers were on average 65.3 years old, females (76.3%), predominantly white, highly educated, and just less than half of caregivers worked outside the home. More than half of caregivers (55.0%) were spouses of patients. The vast majority (89.4%) lived with the patient and reported high involvement with patient activities. Fifteen percent of caregivers were categorized as depressed at any time during follow-up.
The presence of BPSD of any kind was common (58.0%) at early stages of dementia when patients were enrolled in the Predictors 2 study. Depressive symptoms were reported in 18.0% of the patients, psychotic behavioral symptoms were reported in 36.9% of the patients, and agitation/aggression symptoms were reported in 34.2% of the patients. Any persistent BSPD (present at least two times over the course of the first year) were also common (42.5%). Among individual BPSD, persistent depressive symptoms were least common (6.3%) and psychotic symptoms and persistent agitation/aggression symptoms were more commonly reported (26.9% and 26.3%, respectively) during the first year of illness.
The presence of any documented BPSD in the earliest stages of illness was not independently associated with subsequent caregiver depressive symptoms when controlling for potential confounding variables (OR = 1.03; 95% CI = 0.61–1.73) in a fully adjusted model (see Table 2). With the possible exception of agitation/aggression trending toward significance (p < 0.1), individual dementia patient behavior symptoms measured at initial baseline assessment were not associated with subsequent caregiver behaviors.
Table 2.
Associations between presence of symptom clusters at baseline in early dementia and subsequent caregiver depressive symptoms (n = 160)*
| MODEL 1
|
MODEL 2
|
MODEL 3
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Depressive symptoms | 0.87 | 0.36–2.12 | 0.71 | 0.29–1.76 | 0.79 | 0.33–1.87 |
| Agitation/aggression | 1.65 | 0.98–2.79 | 1.46 | 0.86–2.45 | 1.17 | 0.70–1.95 |
| Psychotic symptoms | 1.35 | 0.78–2.35 | 1.16 | 0.67–2.01 | 0.98 | 0.58–1.64 |
| Accusatory/aggressive behavior | 0.94 | 0.44–2.03 | 0.96 | 0.47–1.95 | 0.82 | 0.43–1.54 |
| Any behavioral symptoms | 1.36 | 0.81–2.27 | 1.21 | 0.71–2.07 | 1.03 | 0.61–1.73 |
Note:
Multiple time points (mean = 4) included per patient–caregiver dyad.
Model 1 = unadjusted; Model 2 = adjusted for concurrent patient symptom cluster; Model 3 = simultaneously adjusted for other concurrent patient symptom clusters, patient functional status, whether caregiver is the spouse.
Persistent depressive, psychotic, and accusatory/aggressive symptoms early in dementia were not associated with later caregiver depressive symptoms (see Table 3). When controlling for concurrent patient agitation/aggression, the presence of persistent agitation/aggression over the course of one year resulted in an increase in caregiver depressive symptoms (OR = 1.76; 95% CI = 1.04–2.97), although this relationship was no longer significant in fully adjusted models. In post hoc analyses (data not shown) we also examined patients who consistently exhibited agitation/aggression behaviors persistently at the baseline, six-month, and one-year assessments and had similar trends toward significance.
Table 3.
Associations between presence of persistent symptom clusters in the first year of dementia diagnosis and subsequent caregiver depressive symptoms (n = 160)*
| MODEL 1
|
MODEL 2
|
MODEL 3
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Depressive symptoms | 1.37 | 0.39–4.8 | 1.09 | 0.29–4.02 | 1.22 | 0.34–4.44 |
| Agitation/aggression | 2.02** | 1.20–3.04 | 1.76** | 1.04–2.97 | 1.41 | 0.83–2.39 |
| Psychotic symptoms | 1.52 | 0.83–2.77 | 1.14 | 0.64–2.05 | 1.32 | 0.74–2.36 |
| Accusatory/aggressive behavior | 1.03 | 0.48–2.20 | 1.03 | 0.52–2.08 | 0.85 | 0.45–1.60 |
| Any behavioral symptoms | 1.65 | 0.97–2.80 | 1.5 | 0.88–2.57 | 1.28 | 0.75–2.18 |
Note:
Multiple time points (mean = 4) included per patient–caregiver dyad.
p < 0.05.
Model 1 = unadjusted; Model 2 = adjusted for concurrent patient symptom cluster; Model 3 = simultaneously adjusted for concurrent patient symptom cluster, patient functional status, whether caregiver is the spouse.
Discussion
The current study is one of the few studies to examine the impact of BPSD during a sensitive time period in the course of dementia: early in the disease trajectory. We examined the impact of individual and summary measures of BPSD that occurred in mild dementia prospectively on subsequent caregiver depressive symptoms for 160 patient–caregiver dyads up to six years of follow-up or until patient’s death.
While we hypothesized that behavioral symptoms that occurred early in the dementia patient–caregiver relationship would independently impact subsequent caregiver depressive symptoms, our findings suggest that this is not the case. It appears that only aggression/agitation that occurs early in illness is associated with subsequent caregiver depressive symptoms and warrants further study. The effect of the presence of this persistent behavior on subsequent caregiver depressive symptoms remained significant when controlling for concurrent aggression/agitation in patients, although this effect was reduced (OR = 1.41) and no longer statistically significant in fully adjusted models (95% CI = 0.83–2.39). Although the literature is not consistent as to which individual behavioral symptoms result in most depressive symptoms for caregivers (Ornstein and Gaugler, 2012), the negative impact of patient’s aggression and agitation on caregivers is well documented (Covinsky et al., 2003). The documentation of persistent symptoms through repeat assessments over the first year of the course of dementia may be a more meaningful marker of symptom burden given the often sporadic nature of BPSD. Given that we were unable to see statistically significant findings in fully adjusted models, we recommend that other studies continue to examine this issue. In post hoc sub-group analyses we found that the association between early persistent aggression/agitation was significantly associated with caregiver depressive symptoms in fully adjusted models among caregivers of patients who were still living at home (OR = 1.99; 95% CI = 1.04–3.80), while there was no effect among patients living in facilities (OR = 1.01; 95% CI = 0.46–2.22). While further study is necessary, this suggests that early and persistent aggression/agitation may only have negative effects for caregivers of non-institutionalized patients. Moreover, this finding highlights the importance of understanding the role of timing when studying the impact of BPSD on institutionalization and other critical caregiver outcomes.
As one of the first studies related to caregiver depression that is informed by a life-course approach (Ben-Shlomo and Kuh, 2002), this study examines the early experience of caregivers on future outcomes. While the Predictors 2 cohort is not a dementia inception cohort, patients are enrolled, and by design, assessed at the earliest stages of illness when they have mild dementia. This unique study feature has thus allowed for the first comprehensive assessment of how individual behaviors that occur early in the patient’s illness course may impact caregiver depressive symptoms once disease has progressed. One previous study demonstrated a relationship between the presence of behavioral problems that occurred early in the caregiving career and institutionalization as well as change in caregiver burden and depression (Gaugler et al., 2005). However, this study examined symptoms reported earlier in the patient–caregiver relationship (based on a measure of duration of caregiving), which is not necessarily when the patient had early dementia (care recipients in this study had an average MMSE = 12.7 at the baseline of this study, indicating at least moderate cognitive impairment; see Gaugler et al., 2005). Future work in this area should consider examining caregiver depression and the caregiving career from a life-course perspective, especially given the increasing length of the caregiver–patient relationship. We examined the occurrence of BPSD when patients were first diagnosed with AD or a related dementia and still had high cognitive function. There may be other sensitive time periods in the dementia caregiving career in which the occurrence of patient BPSD has a lasting and negative impact. Instead of examining onset of specific BPSD relative to time of disease diagnosis, we may instead want to examine the occurrence of BPSD at certain thresholds of patient cognitive or functional decline.
This study included patients with both AD and DLB. While the findings did not change when restricting the study to patients with AD only, additional research is warranted especially given that these diseases are characterized by marked differences in symptom trajectories, particularly among psychotic symptoms (McKeith et al., 2004). While caregivers of patients with DLB are highly burdened (Leggett et al., 2011), future work may find extensive variability in DLB caregivers’ emotional and psychological responses to the occurrence of DLB-related symptoms. In addition, given the lengthy follow-up period of this study (on average, caregiver depressive symptoms were measured 4.5 years after patient baseline assessment), we restricted the analyses to examine the impact of early dementia symptoms on caregiver depressive symptoms within three years only, but found no association. Caregivers in this study were providing high level of care and were likely to live with the patient. Future work in this area will have to consider how level of care provided may vary over time which may impact symptom development.
While this study importantly includes patients with mild dementia, it is not in fact a true dementia inception cohort (i.e., a cohort of patients initially free of dementia). Examination of our findings in a true dementia inception cohort is necessary to truly understand the impact of early disease’s features on subsequent caregiver depressive symptoms and to examine the impact of early behaviors on all subsequent caregiver outcomes. Similarly, we do not have caregiver depressive symptoms data for all dyads at the Predictors 2 Study baseline, so we cannot control for caregiver depressive symptoms at the baseline, limiting our ability to determine whether the caregiver depressive symptoms we are measuring are new or have changed from baseline. Furthermore, change in caregiver stress (e.g., role overload), which is more likely to be impacted by change in overall patient behaviors (Gaugler et al., 2000), was not measured in the Predictors 2 study. In addition, this study assumes that caregivers were involved with patients in their early stages of dementia when baseline BPSD were measured. While the vast majority of our caregivers lived with the patient and most were spousal caregivers, it is possible that a small number of caregivers did not know patients during early stages of dementia and were not impacted by BSPD in early dementia.
Another limitation is this study’s reliance on self-report data, including caregiver self-report of depressive symptoms. Validated clinical data on caregiver depression and depressive symptoms would have provided greater insight into how caregiver outcomes change over time. Furthermore, while we aimed to capture persistent symptoms in early dementia through subsequent six-month assessments, the CUSPAD only asks about symptom occurrence over the last month. Thus, the presence of other symptoms may not have been captured in these data. Future studies would benefit from repeat assessment of BPSD multiple times over the first year of dementia to better assess persistent behavioral symptoms. In addition, we were unable to assess severity of symptoms given the structure of the CUSPAD questionnaire. Future studies may want to focus on severe as well as persistent agitation and aggression in early stages of dementia. Finally, this was a fairly homogenous sample of well-educated white patients and caregivers which may not be generalizable to other populations.
Strengths of this study include a sample of patients with mild dementia who were carefully diagnosed in a consensus conference and well characterized. Because caregivers were followed beyond a patient’s nursing home placement, the study design eliminates attrition biases noted in previous studies in which only caregivers who can adjust to the challenges of daily patient care remain in follow-up studies (Gaugler et al., 2005). In addition, caregiver data were available on 98% of all patients with caregivers who were alive at the time of study inception. Furthermore, few longitudinal studies of caregiving consider multiple points of follow-up beyond one to two years, thereby compressing analysis of care provision and failing to capture the full spectrum of the prolonged dementia caregiving experience. Finally, instead of only using a cumulative measure of BPSD that includes a wide range of behavioral symptoms exhibited by persons with dementia (e.g., depression, psychosis, wandering), we examined individual symptom clusters that do not have uniform effect on caregiver outcomes (Ornstein et al., 2013).
Although this study suggests that persistent agitation/aggression in early dementia is associated with subsequent caregiver outcomes, this association was not significant in fully adjusted models. Further studies are required to better understand this relationship. We recommend studies examine the impact of persistent symptoms using more frequent and proximal assessments due to the sporadic nature of BPSD. It is possible, for example, that the true nature of BPSD cannot be reliably tracked by traditional paper and pencil surveys administered biannually or even more frequently. Prospective longitudinal analyses should continue to examine other sensitive time periods during the course of dementia which may adversely influence caregiver and care recipient outcomes, as such inquiries may help researchers and clinicians identify when stressors (such as BPSD) have the most long-lasting and negative impact to maximize limited resources for caregiving families.
Acknowledgments
The Predictors Study is supported by NIA RO1 AG07370 (Y. Stern). This research was supported by NIMH T32 MH013043-36 (K. A. Ornstein).
Footnotes
Conflict of interest
None.
Description of authors’ roles
K. A. Ornstein was responsible for all aspects of study design, analysis, and manuscript preparation. Y. Stern collected the data and assisted with study design and writing the paper. J. Gaugler assisted with study design and writing the paper. C. W. Zhu, N. Scarmeas, and D. Devanand assisted with study analysis and writing the paper.
References
- Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. Alzheimer and Dementia. 2012;8:131–168. doi: 10.1016/j.jalz.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlach CJ. Profiles in Caregiving: The Unexpected Career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- Anthony-Bergstone CR, Zarit SA. Symptoms of psychological distress among caregivers of dementia patients. Psychology and Aging. 1988;3:245–248. doi: 10.1037//0882-7974.3.3.245. [DOI] [PubMed] [Google Scholar]
- Ballard C, Corbett A, Chitramohan R, Aarsland D. Management of agitation and aggression associated with Alzheimer’s disease: controversies and possible solutions. Current Opinions in Psychiatry. 2009;22:532–540. doi: 10.1097/YCO.0b013e32833111f9. [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31:285–293. [PubMed] [Google Scholar]
- Black W, Almeida OP. A systematic review of the association between the behavioral and psychological symptoms of dementia and burden of care. International Psychogeriatrics. 2004;16:295–315. doi: 10.1017/s1041610204000468. [DOI] [PubMed] [Google Scholar]
- Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. British Journal of Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cottrell LS. The adjustment of the individual to his age and sex roles. American Sociological Review. 1942;7:617–620. [Google Scholar]
- Covinsky KE, et al. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. Journal of General Internal Medicine. 2003;18:1006–1014. doi: 10.1111/j.1525-1497.2003.30103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L. The Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual. Minneapolis, MN: NCS Pearson; 1993. [Google Scholar]
- Devanand DP, et al. The Columbia University scale for psychopathology in Alzheimer’s disease. Archives of Neurology. 1992;49:371–376. doi: 10.1001/archneur.1992.00530280051022. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Davey A, Pearlin LI, Zarit SH. Modeling caregiver adaptation over time: the longitudinal impact of behavior problems. Psychology and Aging. 2000;15:437–450. doi: 10.1037//0882-7974.15.3.437. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Zarit SH, Pearlin LI. The onset of dementia caregiving and its longitudinal implications. Psychology and Aging. 2003;18:171–180. doi: 10.1037/0882-7974.18.2.171. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Kane RA, Newcomer R. The longitudinal effects of early behavior problems in the dementia caregiving career. Psychology and Aging. 2005;20:100–116. doi: 10.1037/0882-7974.20.1.100. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Kane RL, Newcomer R. Resilience and transitions from dementia caregiving. Journal of Gerontology B Psychological and Social Sciences. 2007;62:38–44. doi: 10.1093/geronb/62.1.p38. [DOI] [PubMed] [Google Scholar]
- Leggett AN, Zarit S, Taylor A, Galvin JE. Stress and burden among caregivers of patients with Lewy body dementia. Gerontologist. 2011;51:76–85. doi: 10.1093/geront/gnq055. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288:1475–1483. doi: 10.1001/jama.288.12.1475. [DOI] [PubMed] [Google Scholar]
- Marcus R, Marder K, Bell K, Dooneief G, Mayeux R, Stern Y. Interrater reliability of extrapyramidal signs in a group assessed for dementia. Archives of Neurology. 1991;48:1147–1149. doi: 10.1001/archneur.1991.00530230055021. [DOI] [PubMed] [Google Scholar]
- McKeith I, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology. 1996;47:1113–1124. doi: 10.1212/wnl.47.5.1113. [DOI] [PubMed] [Google Scholar]
- McKeith I, et al. Dementia with Lewy bodies. Lancet Neurology. 2004;3:19–28. doi: 10.1016/s1474-4422(03)00619-7. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving and AARP. Caregiving in the US. Washington, DC: National Alliance for Caregiving and AARP; 2004. [Google Scholar]
- Ornstein K, Gaugler JE. The problem with “problem behaviors”: a systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. International Psychogeriatrics. 2012;24:1536–1552. doi: 10.1017/s1041610212000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornstein K, Gaugler JE, Devanand DP, Scarmeas N, Zhu C, Stern Y. The differential impact of unique behavioral and psychological symptoms for the dementia caregiver: how and why do patients’ individual symptom clusters impact caregiver depressive symptoms? American Journal of Geriatric Psychiatry. 2013 doi: 10.1097/JGP.0b013e31826d6b31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Soto ME, Andrieu S, Gillette-Guyonnet S, Cantet C, Nourhashemi F, Vellas B. Risk factors for functional decline and institutionalisation among community-dwelling older adults with mild to severe Alzheimer’s disease: one year of follow-up. Age Ageing. 2006;35:308–310. doi: 10.1093/ageing/afj059. [DOI] [PubMed] [Google Scholar]
- Steinberg M, et al. The incidence of mental and behavioral disturbances in dementia: the cache county study. Journal of Neuropsychiatry and Clinical Neurosciences. 2003;15:340–345. doi: 10.1176/jnp.15.3.340. [DOI] [PubMed] [Google Scholar]
- Stern Y, Paulson J, Mayeux R. Modified mini-mental state examination: validity and reliability. Neurology. 1987;37:179–179. [Google Scholar]
- Stern Y, et al. Predicting time to nursing home care and death in individuals with Alzheimer disease. JAMA. 1997;277:806–812. [PubMed] [Google Scholar]


