Abstract
Background
Childhood psychotic symptoms have been used as a subclinical phenotype of schizophrenia in etiological research and as a target for preventative interventions. However, recent studies have cast doubt on the specificity of these symptoms for schizophrenia, suggesting alternative outcomes such as anxiety and depression. Using a prospective longitudinal birth cohort we investigated whether childhood psychotic symptoms predicted a diagnosis of schizophrenia or other psychiatric disorders by 38 years of age.
Method
Participants were drawn from a birth cohort of 1037 children from Dunedin, New Zealand, who were followed prospectively to 38 years of age (96% retention rate). Structured clinical interviews were administered at age 11 to assess psychotic symptoms and study members underwent psychiatric assessments at ages 18, 21, 26, 32 and 38 to obtain past-year DSM-III-R/IV diagnoses and self-reports of attempted suicides since adolescence.
Results
Psychotic symptoms at age 11 predicted elevated rates of research diagnoses of schizophrenia and post-traumatic stress disorder (PTSD) and also suicide attempts by age 38, even when controlling for gender, social class and childhood psychopathology. No significant associations were found for persistent anxiety, persistent depression, mania or persistent substance dependence. Very few of the children presenting with age-11 psychotic symptoms were free from disorder by age 38.
Conclusions
Childhood psychotic symptoms were not specific to a diagnosis of schizophrenia in adulthood and thus future studies of early symptoms should be cautious in extrapolating findings only to this clinical disorder. However, these symptoms may be useful as a marker of adult mental health problems more broadly.
Keywords: Childhood, longitudinal, post-traumatic stress disorder, psychosis, suicide
Introduction
Psychotic symptoms have been shown to occur in several countries to a substantial minority of people in the general population (van Os et al. 2009), especially in childhood and early adolescence (Laurens et al. 2007; Kelleher et al. 2012a). Over a decade ago, we demonstrated in the Dunedin Multidisciplinary Health and Development birth cohort study that psychotic symptoms among 11-year-olds were associated with the development of schizophrenia-spectrum disorders in early adulthood (Poulton et al. 2000). A similar relationship was subsequently reported by Welham et al. (2009) between auditory hallucinations reported by 14-year-olds and the presence of a psychotic disorder at 21 years of age. A large body of research has now accumulated indicating that these early psychotic phenomena also have etiological features in common with clinically relevant psychotic disorders (Laurens et al. 2008; Polanczyk et al. 2010). Therefore, a strong case has been made for these more prevalent psychotic symptoms to be used in longitudinal research designs as a subclinical phenotype to provide further insights into the origins of schizophrenia (Kelleher & Cannon, 2011), in addition to forming a target for preventive interventions (Morrison et al. 2004).
In the original paper we also found an association between early psychotic symptoms and the presence of anxiety disorders at 26 years of age (Poulton et al. 2000). This finding was largely overlooked and only recently have researchers begun to explore this potential non-specificity. Recently, Werbeloff et al. (2012) reported that psychotic symptoms were a precursor to hospitalizations for non-affective psychosis and several other non-psychotic psychiatric disorders in their longitudinal follow-up of Israeli adults. Kelleher et al. (2012b) also reported that psychotic symptoms in both early and mid-adolescence tended to co-occur with at least one non-psychotic psychiatric disorder (most often affective disorders). High levels of co-morbidity have also been demonstrated in childhood, along with worryingly elevated rates of self-harm (Polanczyk et al. 2010). This recent evidence has resulted in calls for psychotic symptoms to be regarded as a non-specific marker for later mental health problems (Murray & Jones, 2012) and brings into question the use of these symptoms as potential subclinical phenotypes of psychotic disorders in both research and clinical contexts.
However, the existing studies exploring the specificity of psychotic symptoms for later adult psychiatric disorder have several methodological limitations. In the original study (Poulton et al. 2000) we only followed individuals up to 26 years of age and children in the Welham et al. (2009) study were only followed to age 21. As participants in both of these studies were only part-way through the main period of risk for developing schizophrenia (Hafner et al. 1993), it is possible that some cases of schizophrenia had not yet developed, resulting in an underestimate of the predictive utility of childhood psychotic symptoms for later schizophrenia. Similarly, the samples reported in Kelleher et al. (2012b) had an upper age limit of 16 years, only explored the presence of non-psychotic psychiatric disorders (thus providing no information on schizophrenia risk), and only focused on current co-occurrence with psychotic symptoms, which does not tell us about their future predictive value for disorders in adulthood. Finally, Werbeloff et al. (2012) included only individuals whose psychotic symptoms were present in adulthood, which is not informative about the potential for early detection and prevention efforts. This latter study was also limited to individuals who had been hospitalized and thus their findings may not generalize to the wider population of individuals with psychiatric disorders who are treated solely within the community or never come to the attention of psychiatric services.
A more comprehensive approach to the issue of specificity is required to enable firmer conclusions to be drawn. Therefore, we sought to investigate whether childhood psychotic symptoms specifically predicted schizophrenia rather than other major psychiatric disorders using subsequent waves of data collection from the original Dunedin birth cohort up to 38 years of age. This study redresses the limitations of previous reports highlighted above by using prospectively collected data from a general population sample assessed for psychotic symptoms in childhood, following them further into the period of risk for developing schizophrenia, and including treated and untreated cases of schizophrenia and other major psychiatric disorders.
Method
Sample
Participants are drawn from the Dunedin Multidisciplinary Health and Development Study, a longitudinal investigation of the health and behavior of a complete birth cohort of consecutive births between 1 April 1972 and 31 March 1973, in Dunedin, New Zealand. The original cohort comprised 1037 children (91% of consecutive births, 52% boys) and was first assessed when the children were 3 years of age. Cohort families represent the full range of socioeconomic status in the general population of New Zealand’s South Island and are primarily of white European ancestry. Follow-up assessments were conducted at 5, 7, 9, 11, 13, 15, 18, 21, 26, 32 and, most recently, 38 years of age, when 96% of the 1004 living study members underwent assessment in 2010–2012. Each phase of the study has been approved by the Otago Ethics Committee. Study members gave written informed consent to participate in each phase following a detailed explanation of the assessments involved.
Measures
Psychotic symptoms at age 11
As described previously by Poulton et al. (2000), the schizophrenia section of the Diagnostic Interview Schedule for Children (DISC-C; Costello et al. 1982) for DSM-III was administered by a child psychiatrist when the children were aged 11 years to assess possible psychotic symptoms (Anderson et al. 1987). These interviews were completed for the 789 cohort members who were seen at the Dunedin Unit at age 11 (one quarter of the cohort was assessed at school, and unfortunately did not see the psychiatrist). Those with and without age-11 psychotic symptom data available did not differ significantly in their rates of schizophrenia (χ2 =0.69, p=0.406), other psychiatric diagnoses [persistent anxiety: χ2 =0.04, p=0.841; persistent depression: χ2 =0.05, p=0.827; post-traumatic stress disorder (PTSD): χ2 =1.83, p=0.176; persistent substance dependence: χ2 =1.04, p=0.308] or suicide attempts (χ2 =0.33, p=0.567) by age 38. Study members were asked five questions: (1) ‘Some people believe in mind reading or being psychic. Have other people ever read your mind?’; (2) ‘Have you ever had messages sent just to you through television or radio?’; (3) ‘Have you ever thought that people are following you or spying on you?’; (4) ‘Have you heard voices other people can’t hear?’; and (5) ‘Has something ever gotten inside your body or has your body changed in some strange way?’ The psychiatrist scored their response to each item as not present (0), possibly present (1) or definitely present (2) and the scores were added together.
Because of the small number of children with a total score of 2 or more, these children were grouped together. This resulted in the majority of children scoring 0 (n=673, 85.3%; 50.2% boys), classified as having no psychotic symptoms; just over one in 10 scoring 1 (n=103, 13.1%; 66.0% boys), classified as experiencing a ‘weak’ symptom; and 13 children scoring 2 or more (1.7%; 61.5% boys) who were considered to be experiencing ‘strong’ psychotic symptoms. At minimum, study members could enter the strong symptom group by obtaining a score of 1 (yes, likely) for two symptoms or a score of 2 (yes, definitely) for one symptom. The descriptions provided by the children were reviewed by two psychiatrists specializing in psychosis and two clinical psychologists who independently agreed that the symptoms seemed to be genuine in content.
Adult psychiatric disorder by age 38
Clinically trained interviewers conducted private interviews with the study members at 18, 21, 26, 32 and 38 years of age using the Diagnostic Interview Schedule (DIS; Robins et al. 1981, 1995) to assess the presence of psychiatric disorders over the previous 12 months. The Life History Calendar (LHC) interview was used to ascertain treatment in the years between our past-year research diagnoses. Our four past-year diagnoses were found to capture all of the cases ever treated. Diagnoses of anxiety disorders, depression, mania, PTSD, schizophrenia and substance dependence were made at each age according to both the symptom and impairment criteria from DSM-III-R (APA, 1987) (at ages 18 and 21) or DSM-IV (APA, 1994) (from age 26 onwards). Interviewers were blind to previous diagnoses. Each disorder was diagnosed regardless of the presence of other disorders and therefore an individual could have more than one psychiatric diagnosis. The control group comprised those who did not meet criteria for any of the disorders listed below at any assessment point. Additional criteria and prevalence rates for each psychiatric disorder are detailed in the following sections.
Schizophrenia
Schizophrenia was considered present within adulthood if the study member had received a diagnosis at 21, 26, 32 or 38 years of age. Additional steps were taken to enhance the validity of the Dunedin study’s research diagnosis of schizophrenia. First, we required hallucinations (which were not substance use related) in addition to at least two other positive symptoms. This requirement is stricter than DSM-IV (APA, 1994), which does not require hallucinations. Second, because self-reports can be compromised by poor insight in schizophrenia, we required objective evidence of impairment resulting from psychosis, as reported by informants and as recorded in the study’s LHCs, which documented histories of employment and relationships (or the lack of them). Third, the DIS (Robins et al. 1981, 1995) was administered by experienced mental health professionals, not lay interviewers, and they recorded detailed case-notes. Our staff also rated observable symptoms manifested in affect, grooming and speech during the full day participants spent at the research unit. Fourth, participants brought their medications, which were classified by a pharmacist. Fifth, informants reported study members’ positive and negative psychotic symptoms through postal questionnaires. Finally, study members’ parents were interviewed about their adult child’s psychotic symptoms and treatment as part of the Dunedin Family Health History Study (2003–2005). These data, accumulated in the Dunedin study at ages 21, 26, 32 and 38, were compiled into dossiers reviewed by four clinicians to achieve best-estimate diagnoses.
By 38 years of age, 2% of the cohort (n=20/1004) met the above criteria for schizophrenia and had been hospitalized and prescribed antipsychotic medications. An additional 1.7% (n=17) met all the above criteria for schizophrenia but had not yet been registered with the New Zealand health service as schizophrenia patients. Together, these two groups constituted a total of 37 cases of diagnosed schizophrenia in the cohort. Of these 37 schizophrenia cases, 10 had not been assessed at age 11 for psychotic symptoms, leaving an effective group size of n=27 for the current study.
The cohort’s 3.7% prevalence rate seems high at first. However, our birth cohort, with a 96% participation rate, enables us to count psychotic individuals overlooked by prior surveys because individuals with psychotic disorders often refuse to participate in surveys and/or die prematurely (Dutta et al. 2012), and surveys often exclude homeless or institutionalized individuals with psychosis. Therefore, Dunedin’s prevalence rate matches that of Perälä et al. (2007), who found a >3% prevalence of psychosis in the population using multisource methods.
Persistent anxiety
By 38 years of age, 216 study members (27.8% of those assessed for age-11 psychotic symptoms and seen at age 38) were classified as having persistent anxiety disorder as they had been diagnosed with at least one of six anxiety disorders (generalized anxiety disorder, panic disorder, agoraphobia, social phobia, obsessive–compulsive disorder or specific phobia) at two or more assessment phases between 18 and 38 years. This persistence criterion was also applied to depression and substance dependence (see below) to make these common psychiatric disorders more comparable to schizophrenia, which is rarer and tends to persist for a much longer period of time.
Persistent depression
Study members who were diagnosed with depression on two or more occasions between ages 18 and 38 years were classified in the persistent depression group. This group comprised 171 study members (22.0% of those assessed for age-11 psychotic symptoms and seen at age 38).
Mania
Manic episodes were assessed at 26, 32 and 38 years of age. Only six study members (0.8% of those assessed for age-11 psychotic symptoms and seen at age 38) had been diagnosed with mania in this sample. As there were no mania cases among those study members who had weak or strong psychotic symptoms at age 11, mania was not included in the analysis.
PTSD
There were 123 study members who met diagnostic criteria for PTSD when interviewed between ages 18 and 38 years (15.6% of those assessed for age-11 psychotic symptoms and seen at age 38). PTSD was considered separately from anxiety disorders in this analysis (unlike the original study by Poulton et al. 2000) as recent evidence suggests that it has a distinct phenomenology (Resick & Miller, 2009) and the next proposed version of the Diagnostic and Statistical Manual of Mental Disorders, DSM-V, classifies PTSD under a separate diagnostic category to anxiety (namely Trauma and Stressor-Related Disorders).
Persistent substance dependence
Cannabis and alcohol dependence were assessed at ages 18, 21, 26, 32 and 38, and hard-drug (e.g. heroin, cocaine, amphetamines) dependence was assessed at ages 26, 32 and 38. Study members who were diagnosed at two or more of these assessments were considered persistently dependent on substances (not necessarily the same substance on both occasions). This persistent substance dependence group contained 177 study members (22.8% of those assessed for age-11 psychotic symptoms and seen at age 38).
Attempted/completed suicide
During the standardized clinical interviews at ages 18, 21, 26, 32 and 38, study members were questioned about suicide attempts in the previous year. This information was supplemented with lifetime self-reports of suicide attempts on the LHC for the periods between assessments and prior to age 17. Information about completed suicides was initially obtained in the course of longitudinal tracking and checked against death records; only those clearly stating suicide as the cause were included. All information was combined to create an overall variable of any attempted or completed suicide during the lifetime. Two individuals who reported attempting suicide prior to 12 years of age were removed from this analysis to ensure that all attempts occurred after the age-11 psychosis assessment. The final group comprised 97 study members (12.3% of those assessed for age-11 psychotic symptoms and seen at age 38). This rate may seem high but a greater prevalence of suicide has been found in New Zealand than in most European countries and the Americas, especially among adolescents and young adults (Ministry of Health, 2012).
Confounders
The socio-economic status of the family was measured on a scale that places occupations into one of six categories (1=professional, 6=unskilled laborer) based on education and income associated with that occupation in data from the New Zealand census (Elley & Irving, 1976). The higher of either parent’s occupation was averaged across the assessments from birth to age 11. Childhood diagnoses of anxiety, attention deficit hyperactivity disorder (ADHD), conduct disorder and depression were made at age 11 according to DSM-III-R using the information obtained during the DISC (Costello et al. 1982). Childhood psychopathology was considered present if a study member was diagnosed with any of these disorders at age 11 years.
Analysis
Poisson regressions were conducted to estimate relative risks (RRs) for developing each psychiatric disorder (schizophrenia, persistent anxiety, persistent depression, PTSD and persistent substance dependence) and attempted/completed suicide by 38 years among children with (i) weak or (ii) strong psychotic symptoms at age 11 years, compared to children reporting no psychotic symptoms. Initial analyses showed that the presence of weak psychotic symptoms at 11 years of age had little impact on the development of schizophrenia by age 38 [RR 1.76, 95% confidence interval (CI) 0.65–4.77, p=0.269] and was not significantly associated with substantially elevated rates of the other disorders investigated (persistent anxiety: RR 1.15, 95% CI 0.77–1.71, p=0.499; persistent depression: RR 1.04, 95% CI 0.65–1.67, p=0.856; PTSD: RR 1.31, 95% CI 0.80–2.16, p=0.280; persistent substance dependence: RR 1.32, 95% CI 0.89–1.95, p=0.170; attempted/completed suicide: RR 1.32, 95% CI 0.75–2.31, p=0.330). Therefore, the remaining analyses were conducted comparing study members with strong age-11 psychotic symptoms to the rest of the sample (individuals with no or weak symptoms combined). All associations were adjusted for gender and family socio-economic status. Statistically significant associations were further adjusted for the presence of one or more psychiatric disorders at age 11 (ADHD, anxiety, conduct disorder or depression).
Results
Fig. 1 shows the prevalence of schizophrenia, persistent anxiety, persistent depression, PTSD, persistent substance dependence and attempted/completed suicides by age 38 among the children with versus without psychotic symptoms at age 11. The statistical associations between childhood psychotic symptoms and each adult psychiatric disorder are presented in Table 1.
Fig. 1.
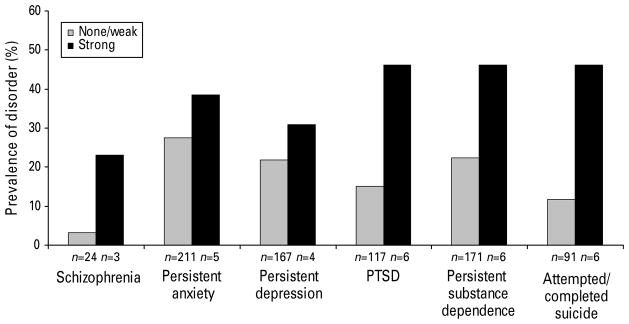
Proportion of children with (n=13) and without (n=776) strong psychotic symptoms at age 11 who had been diagnosed with schizophrenia, persistent anxiety, persistent depression, post-traumatic stress disorder (PTSD), persistent substance dependence or attempted/completed suicide by age 38.
Table 1.
Association between strong psychotic symptoms at age 11 years and adult psychiatric diagnoses by 38 years of age
| Psychiatric diagnosis by age 38 years | None/weak versus strong age-11 symptoms RR (95% CI) |
|---|---|
| Schizophrenia | 7.24 (2.17–24.13) |
| Persistent anxiety | 1.47 (0.60–3.56) |
| Persistent depression | 1.50 (0.56–4.05) |
| Post-traumatic stress disorder | 3.03 (1.33–6.89) |
| Persistent substance dependence | 1.91 (0.85–4.31) |
| Attempted/completed suicide | 3.82 (1.67–8.75) |
RR, Relative risk; CI, confidence interval.
All RRs are adjusted for sex and family socio-economic status.
Do childhood psychotic symptoms predict development of schizophrenia by age 38?
Children with psychotic symptoms at age 11 were at significantly elevated risk of developing schizophrenia by age 38 when compared to the rest of the cohort (RR 7.24, 95% CI 2.17–24.13, p=0.001). This association was slightly attenuated but remained significant after adjustment for childhood psychopathology (RR 4.86, 95% CI 1.37–17.27, p=0.015).
Is the association specific to schizophrenia or common to other psychiatric disorders ?
There were no significantly elevated risks for persistent anxiety, persistent depression or persistent substance dependence among study members with age-11 psychotic symptoms (Table 1). However, children with psychotic symptoms at age 11 were significantly more likely to receive a diagnosis of PTSD (RR 3.03, 95% CI 1.33–6.89, p=0.008) and attempt/complete suicide by age 38 (RR 3.82, 95% CI 1.67–8.75, p=0.001) than the rest of the sample. These associations were largely unchanged when further adjusted for the presence of psychiatric disorders at age 11 (PTSD: RR 2.35, 95% CI 1.01–5.47, p=0.048; suicide: RR 2.58, 95% CI 1.10–6.08, p=0.030).
Are any children reporting psychotic symptoms still healthy by age 38?
Fig. 1 suggests that children presenting with psychotic symptoms at age 11 go on to be diagnosed with a range of psychiatric disorders by 38 years of age. Among study members with the strong age-11 psychotic symptoms, almost a quarter were later diagnosed with schizophrenia (n=3, 23.1%), over a third with persistent anxiety (n=5, 38.5%), just under a third with persistent depression (n=4, 30.8%), approximately half with PTSD (n=6, 46.2%) and a similar proportion with persistent substance dependence (n=6, 46.2%) and attempted/completed suicide (n=6, 46.2%).
There were only two study members who were assessed as having strong psychotic symptoms at 11 years of age who did not meet criteria for any of the disorders investigated here. Closer examination of their longitudinal assessments revealed that neither of them escaped without any problems by age 38. One of them had experienced one episode of clinical depression and one episode of clinical anxiety and has had persistent problems with alcohol but failed to meet substance dependence criteria. The second reported mild anxiety and persistent cannabis use but has never met any clinical diagnostic criteria. Therefore, only one of the original 13 individuals (7.7%) with strong psychotic symptoms at age 11 did not have any diagnosable psychiatric problems by age 38.
Discussion
Using repeated standardized assessments in adulthood, this longitudinal birth cohort study found that individuals with strong psychotic symptoms at age 11 were at increased risk of developing schizophrenia by 38 years of age. This confirms a previous report (Poulton et al. 2000) from this cohort when the study members were aged 26 and extends the results further into the period of risk for development of schizophrenia (Hafner et al. 1993), providing us with greater confidence that we have captured the majority of likely adult schizophrenia cases. The association between strong age-11 psychotic symptoms and adult schizophrenia was also robust to a range of potential confounders including gender, family socio-economic background and the presence of childhood psychiatric disorders.
However, we did not find complete specificity of childhood psychotic symptoms for schizophrenia. The 11-year-olds with psychotic symptoms were also at increased risk of developing PTSD by age 38. This association was weaker than that found for schizophrenia but it was robust to demographic factors and childhood psychopathology. The study members with these early psychotic symptoms also had a range of other outcomes in adulthood including anxiety, depression and substance dependence, with only one escaping reasonably unscathed. Worryingly, these children were also more likely to attempt or complete suicide during adolescence or adulthood, consistent with a recent study of Irish adolescents (Kelleher et al. 2012c).
Our finding that age-11 psychotic symptoms were associated with increased rates of both schizophrenia and PTSD in adulthood fits with a broader literature that indicates some etiological overlap between the two disorders. For instance, a history of maltreatment during childhood has been shown to be more common in adults with schizophrenia and other psychotic disorders (Fisher et al. 2010; Varese et al. 2012) and also in those with PTSD (Brewin et al. 2000) when compared to rates in the general population. These two disorders can also co-occur (Schäfer & Fisher, 2011), which might suggest that the relationship we found between childhood psychotic symptoms and PTSD may have been driven by those individuals with co-morbid schizophrenia. In this sample, 17 of the 123 study members with PTSD (13.8%) also had a diagnosis of schizophrenia by age 38, but removing these comorbid individuals from the analysis still resulted in increased rates of adult PTSD among children with age-11 psychotic symptoms (RR 3.19, 95% CI 1.17–8.66, p=0.023). It will be important, therefore, for future studies to investigate why some children with psychotic symptoms go on to develop schizophrenia whereas others develop PTSD (or indeed other psychiatric disorders) in adulthood.
The lack of association found in this study between age-11 psychotic symptoms and either anxiety or depression in adulthood contradicts previous research on correlates (Kelleher et al. 2012b) and outcomes of these early symptoms (Poulton et al. 2000; Werbeloff et al. 2012). For instance, in the same cohort assessed at 26 years of age, we found that the age-11 symptoms predicted anxiety disorder (Poulton et al. 2000). The most likely reason for this inconsistency is that we have considered PTSD as a separate disorder in line with recent thinking (Resick & Miller, 2009) whereas Poulton et al. (2000) grouped it with anxiety disorders. Our assessment of psychotic symptoms occurred at a much younger age than in the Werbeloff et al. (2012) study and incorporated all cases of major psychiatric disorder, not just those who had been hospitalized, which could have led to the differential results. Our use of persistent clinical episodes of anxiety and depression may also explain some of the discrepancy between our findings and those of previous studies (Poulton et al. 2000; Kelleher et al. 2012b; Werbeloff et al. 2012), but we see this as an advantage because it has allowed us to capture the more severe, persistent cases with these disorders.
The findings presented in this paper have some potential implications. First, the ‘transition’ rate in our sample from childhood psychotic symptoms to adult schizophrenia (23.1%) is reasonably similar to the conversion rate of 22–36% reported in a recent meta-analysis (Fusar-Poli et al. 2012) of adolescents and young adults considered at high clinical risk for psychosis. That we find such a similar rate is remarkable as the symptoms in our cohort were measured many years before conversion was likely to have occurred, they were drawn from a less highly selected sample (general population and not seeking help for their symptoms) and they were also not characterized by the additional risk factors required to meet high clinical risk criteria. However, the fact that the majority of children in this cohort with psychotic symptoms did not develop schizophrenia in adulthood suggests that early screening programs based solely on these symptoms would generate a large number of false positives (at least in terms of schizophrenia). These results therefore further emphasize the importance of using additional risk factors such as a decline in social functioning or family history of psychosis to identify those at greatest risk who may require intervention to prevent transition to clinical psychotic disorders rather than merely relying on the presence of positive psychotic symptoms (Yung et al. 2004; Laurens et al. 2007).
Second, our results raise the question of whether psychotic symptoms in childhood (and potentially at older ages) can continue to be used by researchers as a subclinical phenotype or proxy measure of schizophrenia to investigate the possible risk factors for this clinical disorder in large, general population studies. This is in keeping with other recent studies (Kelleher et al. 2012b; Werbeloff et al. 2012) and commentaries (Lin et al. 2012; Murray & Jones, 2012), which also suggest that it may no longer be useful to extrapolate findings based on early psychotic symptoms solely to psychotic disorders, as it can no longer be assumed that individuals with these symptoms will eventually develop a psychotic disorder. Indeed, the lack of specificity of these early psychotic symptoms should not be that surprising because in childhood they co-occur with other mental health problems (including self-harm; Polanczyk et al. 2010) and both prodromal (Kelleher et al. 2012d) and clinical schizophrenia (Murray et al. 2003; Weich et al. 2011) have high rates of co-morbidity.
A related implication is that it might be more fruitful to consider these childhood symptoms as early markers for poor mental health more generally in adulthood. In the current study, more than 90% of the children with strong psychotic symptoms were found to have some form of clinically diagnosable mental health or substance dependence problem by 38 years of age, in addition to having significantly increased rates of suicide attempts. This suggests that getting these children help early on may substantially improve their later well-being in a broader sense and reduce the burden on health-care systems and society. This adds further weight to the suggestion by Murray & Jones (2012) and others (Kelleher et al. 2012b) that screening for psychotic symptoms in late childhood and early adolescence might be a useful and important way of identifying those who might benefit from non-invasive interventions (e.g. cognitive behavioral therapy; Maddox et al. 2012) to improve their general psychological well-being and arm them with suitable coping strategies to tackle the challenges of adolescence. Clinical trials are required to test this proposition with affected children and such research should assess a broad range of potential mental health outcomes (Lin et al. 2012).
The findings should be considered in light of several limitations. First, we recognize that the number of individuals within this cohort who had strong psychotic symptoms at age 11 was small and thus may have limited our ability to detect associations with a larger number of adult disorders. For example, children with psychotic symptoms did have elevated rates of persistent anxiety, depression and substance dependence but we were underpowered to detect significant associations for these disorders. The base rate of mania was also low, which may have prevented us from finding any associations with this disorder. However, as this was the sample that initially drew attention to the issue of the specificity of childhood psychotic symptoms for schizophrenia, we considered it was important to investigate what had happened to these individuals following assessments conducted over a decade later. Moreover, this sample has many distinct advantages over prior studies in that it has prospectively followed a complete cohort of children into middle adulthood with extremely low levels of attrition and comprehensively assessed them in face-to-face interviews and obtained informant reports on multiple occasions. Nonetheless, these findings require replication among cohorts comprising larger numbers of individuals with early psychotic symptoms.
We also used a stringent definition of schizophrenia and it is possible that if we had used a broader definition of clinical psychosis we may have found that childhood psychotic symptoms resulted in even greater relative risks. However, this is made less likely as age-11 symptoms did not increase risk for affective disorders that usually form part of the broader psychosis spectrum. Finally, to date, our sample only extends up to 38 years of age and although this is reasonably far into the period of risk for developing schizophrenia (Hafner et al. 1993), it will be important to follow these individuals for several more decades to be completely confident that we have captured all relevant cases, especially among women, who can continue to develop schizophrenia well into late adulthood (Hafner et al. 1993).
In conclusion, psychotic symptoms assessed at age 11 were found to predict onset of both schizophrenia and PTSD by 38 years of age in addition to attempted/completed suicides, but not persistent anxiety, persistent depression, mania or persistent substance dependence in this longitudinal cohort. Very few of the children with psychotic symptoms were free from mental health problems in adulthood. Therefore, we recommend that future studies of early psychotic symptoms should be more cautious in extrapolating etiological findings to schizophrenia and suggest that it would be useful to detect and potentially intervene with children displaying psychotic symptoms to prevent the development of poor mental health more generally in adulthood.
Acknowledgments
We thank the Dunedin Study members, their families, Unit research staff and Study founder P. Silva. This work was supported by grants from the Medical Research Council (MRC; G0601483, MR/K00381X/1) and the National Institute of Aging (AG032282). Additional support was provided by the National Institute of Child Health and Human Development (HD061298) and the Jacobs Foundation; H.L.F. was supported by an MRC Population Health Scientist Award (G1002366) and M.H.M. was supported by the National Institute on Drug Abuse (P30 DA023026). The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council.
Footnotes
Declaration of Interest
None.
References
- Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children: prevalence in a large sample from the general population. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 3. American Psychiatric Publishing; Arlington, VA: 1987. Revised. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Publishing; Arlington, VA: 1994. [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Costello A, Edelbrock C, Kalas R, Kessler M, Klaric S. NIMH Diagnostic Interview for Children: Child Version. National Institute of Mental Health; Rockville, MD: 1982. [Google Scholar]
- Dutta R, Murray RM, Allardyce J, Jones PB, Boydell JE. Mortality in first-contact psychosis patients in the UK: a cohort study. Psychological Medicine. 2012;42:1649–1661. doi: 10.1017/S0033291711002807. [DOI] [PubMed] [Google Scholar]
- Elley WB, Irving JC. Revised socio-economic index for New Zealand. New Zealand Journal of Educational Studies. 1976;7:153–167. [Google Scholar]
- Fisher HL, Jones PB, Fearon P, Craig TK, Dazzan P, Morgan K, Hutchinson G, Doody GA, McGuffin P, Leff J, Murray RM, Morgan C. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychological Medicine. 2010;40:1967–1978. doi: 10.1017/S0033291710000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry. 2012;69:220–229. doi: 10.1001/archgenpsychiatry.2011.1472. [DOI] [PubMed] [Google Scholar]
- Hafner H, Maurer K, Loffler W, Reicher-Rosller A. The influence of age and sex on the onset and early course of schizophrenia. British Journal of Psychiatry. 1993;16:280–286. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychological Medicine. 2011;41:1–6. doi: 10.1017/S0033291710001005. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychological Medicine. 2012a;42:1857–1863. doi: 10.1017/S0033291711002960. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Keeley H, Corcoran P, Lynch F, Fitzpatrick C, Devlin N, Molloy C, Roddy S, Clarke MC, Harley M, Arseneault L, Wasserman C, Carli V, Sarchiapone M, Hoven C, Wasserman D, Cannon M. Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. British Journal of Psychiatry. 2012b;201:26–32. doi: 10.1192/bjp.bp.111.101543. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Lynch F, Harley M, Molloy C, Roddy S, Fitzpatrick C, Cannon M. Psychotic symptoms in adolescence index risk for suicidal behavior: findings from 2 population-based case-control clinical interview studies. Archives of General Psychiatry. 2012c doi: 10.1001/archgenpsychiatry.2012.164. Published online: 29 October 2012. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Murtagh A, Molloy C, Roddy S, Clarke MC, Harley M, Cannon M. Identification and characterization of prodromal risk syndromes in young adolescents in the community: a population-based clinical interview study. Schizophrenia Bulletin. 2012d;38:239–246. doi: 10.1093/schbul/sbr164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurens KR, Hodgins S, Maughan B, Murray RM, Rutter ML, Taylor EA. Community screening for psychotic-like experiences and other putative antecedents of schizophrenia in children aged 9–12 years. Schizophrenia Research. 2007;90:130–146. doi: 10.1016/j.schres.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Laurens KR, West SA, Murray RM, Hodgins S. Psychotic-like experiences and other antecedents of schizophrenia in children aged 9–12 years: a comparison of ethnic and migrant groups in the United Kingdom. Psychological Medicine. 2008;38:1103–1111. doi: 10.1017/S0033291707001845. [DOI] [PubMed] [Google Scholar]
- Lin A, Nelson B, Yung AR. ‘At-risk’ for psychosis research: where are we heading? Epidemiology and Psychiatric Sciences. 2012 doi: 10.1017/S2045796012000388. Published online: 30 July 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox L, Jolley S, Laurens KR, Hirsch C, Hodgins S, Browning S, Bravery L, Bracegirdle K, Smith P, Kuipers E. Cognitive behavioural therapy for unusual experiences in children: a case series. Behavioral and Cognitive Psychotherapy. 2012 doi: 10.1017/S1352465812000343. Published online: 5 July 2012. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Suicide Facts: Deaths and Intentional Self-harm Hospitalisations 2010. Ministry of Health; Wellington, New Zealand: 2012. [Google Scholar]
- Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, Parker S, Bentall RP. Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomized controlled trial. British Journal of Psychiatry. 2004;185:291–297. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- Murray GK, Jones PB. Psychotic symptoms in young people without psychotic illness: mechanisms and meaning. British Journal of Psychiatry. 2012;201:4–6. doi: 10.1192/bjp.bp.111.107789. [DOI] [PubMed] [Google Scholar]
- Murray RM, Jones PB, Susser ES, van Os J, Cannon M. The Epidemiology of Schizophrenia. Cambridge University Press; Cambridge, UK: 2003. [Google Scholar]
- Perälä J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsä E, Pirkola S, Partonen T, Tuulio-Henriksson A, Hintikka J, Kieseppä T, Härkänen T, Koskinen S, Lönnqvist J. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Archives of General Psychiatry. 2007;64:19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, Moffitt TE, Arseneault L, Cannon M, Ambler A, Keefe RS, Houts R, Odgers CL, Caspi A. Childhood psychotic symptoms share etiological and clinical features with adult schizophrenia: results from a representative birth cohort. Archives of General Psychiatry. 2010;67:328–338. doi: 10.1001/archgenpsychiatry.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Archives of General Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- Resick PA, Miller MW. Posttraumatic stress disorder: anxiety or traumatic stress disorder ? Journal of Traumatic Stress. 2009;22:384–390. doi: 10.1002/jts.20437. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler L, Bucholz KK, Compton W. Diagnostic Interview Schedule for DSM-IV. Washington University School of Medicine; St Louis, MO: 1995. [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Schäfer I, Fisher HL. Childhood trauma and posttraumatic stress disorder in patients with psychosis: clinical challenges and emerging treatments. Current Opinion in Psychiatry. 2011;24:514–518. doi: 10.1097/YCO.0b013e32834b56c8. [DOI] [PubMed] [Google Scholar]
- van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychological Medicine. 2009;39:179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J, Bentall RP. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weich S, McBride O, Hussey D, Exeter D, Brugha T, McManus S. Latent class analysis of co-morbidity in the Adult Psychiatric Morbidity Survey in England 2007: implications for DSM-5 and ICD-11. Psychological Medicine. 2011;41:2201–2212. doi: 10.1017/S0033291711000249. [DOI] [PubMed] [Google Scholar]
- Welham J, Scott J, Williams G, Najman J, Bor W, O’Callaghan M, McGrath J. Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychological Medicine. 2009;39:625–634. doi: 10.1017/S0033291708003760. [DOI] [PubMed] [Google Scholar]
- Werbeloff N, Drukker M, Dohrenwend BP, Levav I, Yoffe R, van Os J, Davidson M, Weiser M. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Archives of General Psychiatry. 2012;69:467–475. doi: 10.1001/archgenpsychiatry.2011.1580. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophrenia Research. 2004;67:131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]


