Abstract
Buruli ulcer (BU) is a cutaneous neglected tropical disease caused by Mycobacterium ulcerans. Participation of Community Health Workers (CHWs) is an integral part of the management of BU, yet their impact has not been systematically evaluated in sub-Saharan Africa. METHODS: Our objectives were to summarize the evidence on the impact of CHWs on the control of BU in sub-Saharan Africa by looking at their recruitment, training, non-governmental support and performance. We searched the following electronic databases from January 1998 to July 2012: Medline, EMBASE (Excerpta Medica Database), The Cochrane Library, Google Scholar, CINAHL (Cumulative Index to Nursing and Allied Health Literature), WHOLIS (World Health Organization Library Database), LILACS (Latin American and Caribbean Literature on Health Sciences) and contacted experts in the field. There were no restrictions to language or publication status. All study designs that could provide the information we sought were eligible, provided the studies were conducted in sub-Saharan Africa. Critical appraisal of all identified citations was done independently by two authors to establish the possible relevance of the articles for inclusion in the review. Of 195 hits, 17 papers met the inclusion criteria. For the management of Buruli Ulcer, CHWs are often recruited from the communities they will serve. Communities play a role in CHW selection. Larger numbers of CHWs are needed in order to improve the detection and management of cases. One of the major obstacles to the control of BU is inadequate and poorly- equipped health facilities in the affected areas. Evidence from this review suggests that CHW programmes can have large impacts on the control of BU in sub-Saharan Africa. Large-scale rigorous studies, including RCTs, are needed to assess whether the CHWs programs promote equity and access.
Keywords: Systematic review, impact, Community Health Workers, Buruli ulcer, sub-Saharan Africa
Introduction
Buruli ulcer (BU) is a cutaneous Neglected Tropical Disease (NTD) caused by Mycobacterium ulcerans [1, 2]. It is the third most frequent mycobacterial infection after tuberculosis and leprosy [1, 2]. It is characterized initially by a nodule that later progresses to vast cutaneous ulcerations, mediated by Mycolactone, a toxin secreted by M. ulcerans [3, 4]. The exact mode of transmission is the subject of research [5]. BU is endemic in thirty countries, and is suspected to exist in 10 other countries of the African Region [1]. The World Health Organization (WHO) initiated the Global Buruli Ulcer Initiative (GBUI), in response to the growing spread of BU [6], and since 1998 the GBUI has been supporting research and improving the management of BU.
In developing countries, the health systems are weakened by human resources shortages. Therefore, evidence-based interventions may not be implemented as required [7–9]. Community Health Workers (CHWs) are essential components of the healthcare workforce who do not require the lengthy and costly training of health personnel and can have a considerable impact in health care [8, 9].
The WHO describes CHWs as follows: “(they) should be members of the communities where they work, should be selected by the communities, should be answerable to the communities for their activities, should be supported by the health system but not necessarily a part of its organization, and have shorter training than professional workers” [9]. CHWs find themselves in the best position to deliver services in well mobilised communities. They work in hand-in-hand with other health workers to provide primary health care (PHC) [1, 10, 11]. This is particularly true for poor, rural communities for whom the provision of preventive and curative services is the main entry point into the health system [1, 2, 8].
CHWs, by virtue of their proximity with the communities are able to play an important role in the detection and referral of cases of BU [2, 4, 6, 12]. In fact, they are members of the community and have equally high stakes in the health of the community. This can lead to timely management and therefore reduce the morbidity and mortality suffered by those infected with BU [12]. Lehmann et al. [13] and Lewin et al. [14] reviewed the evidence on CHW interventions in low- and middle-income countries (LMIC). They found lay health workers to be effective in specific areas of child health, when compared to usual care - community members fending for themselves [14]. Haines et al. [15] highlighted the context specific nature of a CHW's performance.
Synthesizing the evidence on their impact in the management of BU can help to better define their roles, identify weaknesses in how their activities are implemented and inform health systems on relevant measures that can be used to control BU. We therefore conducted a systematic review to summarize the evidence of the impact of CHWs on the control of BU in sub-Saharan Africa.
Our objectives were to summarize the evidence on the impact of CHWs in the control of BU in sub-Saharan Africa. The specific objectives of the studies were to describe CHWs in the control of BU in sub-Saharan Africa with special emphasis on their recruitment, training and involvement of non-governmental association; to describe the impact of CHWs on BU in term of the number of cases identified, referred and confirmed.
Methods
Search strategy: We searched the following electronic databases from January 1998 to July 2012: Medline, EMBASE (Excerpta Medica Database), The Cochrane Library, Google Scholar, CINAHL (Cumulative Index to Nursing and Allied Health Literature), WHOLIS (World Health Organization Library Database), LILACS (Latin American and Caribbean Literature on Health Sciences) and contacted four experts in the field. The following search strategy was modified for the various databases and search engines: («Impact» OR «Contribution» AND «Community Health Worker» OR «Lay Health Worker» AND «Mycobaterium ulcerans» OR «Buruli ulcer» AND «Sub Saharan Africa» OR «Endemic country»). Along with MeSH terms and relevant keywords, we used the Cochrane Highly Sensitive Search Strategy for identifying reports of articles in Pubmed. There were no restrictions to language or publication status. Our search was limited to the last fourteen years, as they correspond to the period of enactment of the GBUI [6]. Prior to the GBUI, efforts to control BU, especially with CHWs were almost inexistent.
Study design: All study designs were eligible for inclusion provided they were on CHWs working on BU in sub-Saharan Africa.
Study participants: Owing to the wide range of functions that fall under the umbrella term “community health worker” we designed a definition of our own. For this review, we defined CHWs as lay individuals trained in the particular role of delivering curative or preventive care in the control of BU.
Types of interventions: We included interventions if the description was adequate for us to establish that it was a CHW intervention aimed at the control of BU. Where such details were unclear, we contacted the study authors, whenever possible, to establish whether the personnel described were CHWs. Four study authors were contacted.
>b>Data sought Any of the following data were sought: Type of training; Recruitment; Involvement of NGOs; Impact, defined as: number of cases identified, number of case referred and number of referred cases confirmed.
Data extraction and management: Critical appraisal of all identified citations was done independently by two authors (MZV and VCT) to establish the possible relevance of the articles for inclusion in the review. Studies were reviewed for relevance based on types of participants (CHWs), interventions (control of BU), and outcome measures. We retrieved full text copies of the articles identified as potentially relevant by either one or both review authors. Where appropriate, we contacted study authors for further information and clarification. Disagreements were resolved by consensus or by arbitration of a third review author (LM). The flow of study selection is described in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram [16]. Data are reported in a narrative manner.
Assessment of quality in included studies: The included studies were not scored for quality.
Current status of knowledge
Our searches retrieved 195 studies, of which 17 are included in the review (Figure 1, Table 1).
Figure 1.
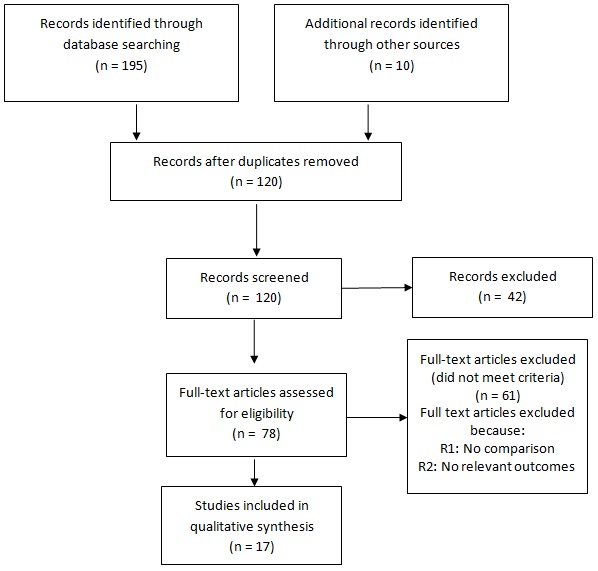
PRISMA flow diagram
Table 1.
Characteristics of included studies, CHWs performance and training; and NGO affiliation
| Reference | Type of study | Country of study | Recruitment of CHWs | Training | NGO affiliation | Impact measures | |
|---|---|---|---|---|---|---|---|
| 1 | Nsom Mba, 2006 [26] | cross-sectional | Cameroon | By the community | Training of CHWS (general training) | None | Not reported |
| 2 | Um Boock, 2008 [34] | Case-control | Cameroon | By the community | Training of CHWS (general training) | Fairmed Foundation | Not reported |
| 3 | Um Boock et Deffo 2004 [35] | Case-control | Cameroon | Not reported | Training of CHWS (general training) | Fairmed Foundation | Not reported |
| 4 | Comte, 2006 [17] | Case-control | Cameroon | Village health committees | Not reported | “Médecins Sans Frontières” | Not Reported |
| 5 | China et Sopoh 2006 [22] | cross-sectional | Benin | By the community | Not reported | Raoul Foullereau. | Not reported |
| 6 | Sopoh et al. 2007 [23] | Cohort study | Benin | By the community | Support in the implementation of CHWs activities | None | Not reported |
| 7 | Malda, 2006 [18] | cross-sectional | Ivory Coast And Benin | Village health committees | Not reported | ANESVAD | Not reported |
| 8 | Ake, 2006 [19] | cross-sectional | Ivory Coast | By the community | Not reported | MAP International | Referral rate : 67% |
| 9 | Saunderson, 2006 [25] | cross-sectional | Ghana | By the community | Not reported | American Leprosy Missions | Not reported |
| 10 | Weeb et al. 2007 [12] | Randomed Controlled Trial | Ghana, Ivory coast | Village health committees | Not reported | None | Not reported |
| 11 | Adamba, 2011 [21] | controlled before and after | Ghana | Village health committees | Training of CHWs (general training) | None | Not reported |
| 12 | Kibadi et al. 2008 [24] | Cohort studies | Democratic republic of Congo | Not Reported | Training of CHWs in the early detection of cases | None | Not reported |
| 13 | Kibadi et al. 2009 [42] | cross-sectional studies | Democratic republic of Congo | By the community | Not reported | None | Not reported |
| 14 | Jonhson, 2005 [27] | cross-sectional studies | Benin | Not reported | Training of CHWs in case identification in | None | Not reported |
| 15 | Kanga et al. 2003 [30] | cross-sectional studies | Ivory Coast | By the community | Not reported | None | Referral rate : 65% |
| 16 | Vouking el al. 2010 [20] | cross-sectional studies | Cameroon | By the community | Training of CHWs in case identification | None | Referral rate : 95% |
| 17 | Ackumey et al. 2011 [41] | cross-sectional studies | Ghana | Not reported | Training of CHWs in case identification | None | Not reported |
Recruitment of CHWs
CHWs were nominated by village health committees or leaders in four studies [12, 17, 18, 21] and by community members in nine studies [19–26, 30, 34, 42]. Very little information was provided on their levels of education [20–24, 26].
Training of CHWs
Here as well, many studies did not report on the training received by the CHWs. When it was reported, the training approaches varied greatly between studies and were not described on the same level of detail in all of them [20–27, 34, 35, 41]. The terms used included: courses, classes, seminars, workshops, discussion groups, practical training, and in-class practice [20–22, 24, 26, 27]. Facilitation was often done by national level facilitators who were from the Ministry of Health or NGOs [17–19, 22, 25, 34, 35].
Role of NGOs
NGOs often initiated training activities [34, 35]. CHWs are often uniquely placed to attract resources for PHC initiatives from private individuals, corporations, foundations, bilateral and multilateral institutions [17, 18, 34, 35]. However we found that there was a mix of public, private, NGO, and traditional providers operating with variable population coverage and quality of services against BU [17, 18, 34, 35]. Advocating on behalf of PHC programmes that involve CHWs was frequently done by individual NGOs or groups of NGOs such as the FAIRMED Foundation, ANESVAD, “Médecins Sans Frontières”, “Fondation Nipponne”, Raoul Foullereau, MAP International, and American Leprosy Missions [17–19, 22, 25, 34, 35].
Impact of CHWs
Three studies assessed the impact of CHWs activities over 12 months [19, 20, 30]. The studies demonstrated varying impacts of CHWs programmes on BU, ranging from a 67% [30] to 95% referring cases to the health centre [20]. CHWs identified and referred suspected cases of BU, of which 91% were confirmed cases. Most CHWs (78%) identified at least one suspected case of BU [20]. Two authors [19, 30] in Ivory Coast found that 67% and 65% of the cases referred by CHWs were confirmed by the medical staff. As concerns the proportion of pre-ulcerative forms of disease referred by CHWs, Vouking et al. [20] reported 85% in Cameroun and Ake et al. [19] found 38% in Ivory Coast.
The most important qualification of CHWs is implicit within the job title; the individual must be from the community that he or she will serve [20, 22, 23, 35]. The cultural, political and social contexts of the programme area influence the recruitment methods that are used and the quality criteria for CHWs. Overall, they are those that are most acceptable to the community [14, 32, 36]. In all the included studies, the CHWs were indeed recruited from the community [20–25].The training of CHWs is an important step in the fight against this disease [1, 29, 36, 37]. There is a very great need to train a large number of CHWs in order to improve the detection and management of cases [1, 29, 36]. While a large number of articles discuss or at least mention the training of CHWs, not surprisingly, the length, depth, organization of, responsibility for and approaches to training vary greatly across programmes [3, 29, 36]. When it was reported, the training approaches varied greatly between studies [20–27]. The terms used included: courses, classes, seminars, workshops, discussion groups, practical training, and in-class practice [20–22, 24, 26, 27].
One of the major obstacles to the control of BU is inadequate and poorly- equipped health facilities in the affected areas [6, 28, 29]. In line with the Yamoussoukro Declaration on BU [6], which called for the development of health systems so that effective treatment can reach all those affected, the actions of several NGOs are contributing to visible improvements in health facilities and the delivery of health services in the affected areas [3, 6, 28]. The crucial integration of CHWs programmes within the existing formal health systems and other programmes in the community is often initiated by NGOs [6, 37]. Unfortunately, those personnel who work closely with CHWs, in BU activities are not involved in the development and supervision of CHWs and therefore lend little support [29, 32, 36, 38, 39]. Strengthening the management capacity of district health teams to focus limited resources on priority problems can be done effectively in low-income settings, as shown by a BU programme that has placed powerful, but easy to use, decision-making methods, in the hands of local decision makers [40]. If CHWs are not trained, supported and supervised regularly on BU, the benefits of their work may be lost; therefore more efforts should be expended on the training of CHWs [12, 32] and the health personnel who work with them.
Our findings show the impact of health education and community surveillance strategies in BU control [20, 22, 41, 42]. This outcome could be explained by a good knowledge of the disease, and a good referral system in the endemic areas [20, 27, 42]. Early detection could reduce the cost of treatment and length of hospitalization as simple cases are treated within the health area [12, 20, 41].
Only three studies assessed the impact of CHWs activities over 12 months, showing impressive referral rates [19, 20, 30]. A recent review found that there is very little evidence on the effectiveness of CHWs in low-income countries [43, 44]. We found that their impact varied greatly. Thus, a key consideration for the design, implementation, and ongoing management of programmes for CHWs is how high-quality performance by CHWs will be achieved and maintained [45, 46]. Implementing CHWs programmes may require a little more than evidence of impact [44]. Factors such as feasibility and acceptability will vary by context and lead to different health and social outcomes [14, 43, 45].
Study limitations
This review has several potential limitations. Firstly, it is possible that some published and unpublished CHWs evaluations were not identified through the search strategies used. However, considerable effort was made to identify additional studies by contacting the authors of included studies and scanning the reference lists of identified literature. Secondly, our definition of CHWs may have excluded some untrained lay health workers. Thirdly, the lack of uniformity in the study designs and reports rendered it impossible to make a comparative assessment of their quality. Finally, only three studies reported on the impact of CHWs, largely undermining our attempts to provide a detailed description of CHW impact in the control of BU.
Conclusion
Evidence from this review suggests that CHWs programmes can have a considerable impact on the control of BU in sub-Saharan Africa. This may be related to high levels of knowledge of the disease by the CHWs, the early detection and a good referral system in the endemic areas. Facilitative supervision and availability of infrastructural support are critical issues for programme success; yet they are usually overlooked. Further studies are needed to assess the quality of care provided by CHWs for the management of BU.
Acknowledgments
Our thanks to the many study authors who gave us additional information regarding study designs and interventions.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MZV and VCT conceived and designed the study. MZV and LM contributed to the analysis. MZV, LM and VCT critically reviewed and edited the manuscript. MZV, LM and VCT read and approved the final paper.
References
- 1.WHO. Geneva: World Health Organisation; 2010. Working to overcome the global impact of neglected tropical diseases: First WHO report on neglected tropical diseases; p. 25. WHO/HTM/NTD/2013. [Google Scholar]
- 2.WHO. Geneva: World Health Organisation; 2007. Everybody's Business: Strengthening Health Systems to Improve Health Outcomes: WHO's framework for action; p. 56. [Google Scholar]
- 3.World Health Organization Buruli ulcer disease. Mycobacterium ulcerans infection: an overview of reported cases globally. Wkly Epidemiol Rec. 2004;79:194–200. [Google Scholar]
- 4.WHO. Geneva: World Health Organisation; 2006. Buruli ulcer: Prevention of disability (POD) WHO/CDS/NTD/GBUI/2006.12. [Google Scholar]
- 5.Merritt RW, Walker ED, Small PLC, Wallace JR, et al. Ecology and Transmission of Buruli Ulcer Disease: A Systematic Review. PLoS Negl Trop Dis. 2010 Dec;4(12):911. doi: 10.1371/journal.pntd.0000911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.OMS. Genève: Suisse; Rapport 5ème réunion du groupe consultatif spécial de l'OMS sur l'ulcère de buruli 11-14 mars 2002; p. 153. WHO/CDS/CPE/GBUI/2003.7. [Google Scholar]
- 7.Stienstra Y, van der Graaf WT, Asamoa K, van der Werf TS. Beliefs and attitudes toward Buruli ulcer in Ghana. Am J Trop Med Hyg. 2002;(67):207–213. doi: 10.4269/ajtmh.2002.67.207. [DOI] [PubMed] [Google Scholar]
- 8.Asiedu K, Etuaful S. Socioeconomic implications of Buruli ulcer in Ghana: a three-year review. Am J Trop Med Hyg. 1998;(59):1015–1022. doi: 10.4269/ajtmh.1998.59.1015. [DOI] [PubMed] [Google Scholar]
- 9.Strengthening the performance of Community Health Workers in primary care; WHO Technical Report Series 780, 198. [Google Scholar]
- 10.Speybroeck N, Kinfu Y, Dal Poz MR, Evans DB. Evidence and Information for Policy. Geneva: World Health Organization; 2006. Reassessing the relationship between human resources for health, intervention coverage and health outcomes. [Google Scholar]
- 11.Webb BJ, Hauck FR, Houp E, Portaels F. Buruli ulcer in West Africa: Strategies for early detection and treatment in the antibiotic era. East Afr J Public Health. 2009 Aug;6(2):144–7. doi: 10.4314/eajph.v6i2.51744. [DOI] [PubMed] [Google Scholar]
- 12.Lehmann U, Friedman I, Sanders D. Review of the utilisation and effectiveness of community-based health workers in Africa; 2004. Working paper of the Joint Learning Initiative. [Google Scholar]
- 13.Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD004015. doi: 10.1002/14651858.CD004015.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bull World Health Organ. 2004;(82):724–733. [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comte E. Médecins Sans Frontieres. Programme de lutte contre l'ulcère de Buruli à Akonolinga (Cameroun) - Résultats de 2005. 9e Réunion annuelle de l'Initiative mondiale contre l'ulcère de Buruli de l'OMS; 15 au 17 mars 2006; p. 138. [Google Scholar]
- 17.Malda V. La stratégie d'ANESVAD dans le domaine de la lutte contre l'ulcère de Buruli en 2005. 9e Réunion annuelle de l'Initiative mondiale contre l'ulcère de Buruli de l'OMS; 15 au 17 mars 2006; p. 138. [Google Scholar]
- 18.Ake J. Intérêt de la mobilisation communautaire dans la lutte contre l'ulcère de Buruli: Cas du projet pilote de Taabo, Côte d'Ivoire. MAP International, Côte d'Ivoire. Réunion annuelle de l'OMS sur l'ulcère de Buruli, CICG; 15-17 mars 2006; Genève, Suisse. [Google Scholar]
- 19.Vouking ZM, Takougang I, Mbam ML. Université Catholique d'Afrique Centrale; 2010. Contribution des agents relais communautaires de l'aire de santé de Ngoantet II dans la lutte contre l'ulcère de Buruli. Mémoire de Master en Santé Publique. [Google Scholar]
- 20.Adamba C, Owusu AY. Burden of Buruli ulcer: how affected households in a Ghanaian District Cope. African Study Monographs. 2011;32(1):1–23. [Google Scholar]
- 21.China E, Sopoh G. Appui de la Fondation luxembourgeoise Raoul Follereau aux activités de lutte contre l'ulcère de Buruli au Benin en 2005 et perspectives. 9e Réunion annuelle de l'Initiative mondiale contre l'ulcère de Buruli de l'OMS; 15 au 17 mars 2006; p. 155. [Google Scholar]
- 22.Sopoh GE, Johnson RC, Chauty A, Dossou AD, Aguiar J, et al. Surveillance ulcère de Buruli, Bénin, 2003-2005. Emerg Infect Dis. 2007;13(9):1374–1376. doi: 10.3201/eid1309.061338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kibadi K, Panda M, Tamfum JM, Fraga AG, Filho AL, et al. New foci of Buruli ulcer, Angola and Democratic Republic of Congo. Emerging Infectious Diseases. 2008;(14):1790–1792. doi: 10.3201/eid1411.071649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saunderson P. Participation de ALM à la lutte contre l'ulcère de Buruli (2005-2006). 9e Réunion annuelle de l'Initiative Mondiale contre l'ulcère de Buruli de l'OMS; 15 au 17 mars 2006; p. 155. [Google Scholar]
- 25.Nsom Mba C. Réunion annuelle de l'OMS sur l'ulcère de Buruli: Activités menées au Cameroun en 2005; p. 138. [Google Scholar]
- 26.Johnson PD, Stinear T, Small PL, Pluschke G, Merritt RW, et al. Buruli ulcer (M ulcerans infection): New insights, new hope for disease control. PloS Med. 2005;(2):e108. doi: 10.1371/journal.pmed.0020108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.OMS. Rapport de la 6ème réunion du groupe consultatif spécial de l'OMS sur l'ulcère de Buruli; 10 au 13 Mars 2003; Genève, suisse. p. 154. WHO/CDS/CPE/GBUI/2003.8. [Google Scholar]
- 28.Valérie Simonet. Genève: OMS; 2008. Prévention des incapacités dans l'ulcère de Buruli: Rééducation de base; p. 104. [Google Scholar]
- 29.Kanga JM, Kacou ED, Kouame Kassi E, Kaloga M, et al. L'ulcère de Buruli: Aspects épidémiologiques, cliniques et thérapeutiques en Côte d'ivoire. Med Trop. 2006;(64):238–242. [PubMed] [Google Scholar]
- 30.Grietens KP, Boock AU, Peeters H, Hausmann-Muela S, Toomer E, et al. “It is me who endures but my family that suffers”: social isolation as a consequence of the household cost burden of Buruli ulcer free of charge hospital treatment. PloS Negl Trop Dis. 2008;(2):321. doi: 10.1371/journal.pntd.0000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mulder AA, Boerma RP, Barogui Y, Zinsou C, Johnson RC, et al. Healthcare seeking behaviour for Buruli ulcer in Benin: A model to capture therapy choice of patients and healthy community members. Trans R Soc Trop Med Hyg. 2008;(102):912–920. doi: 10.1016/j.trstmh.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 32.UNICEF/WHO. UNICEF/WHO; 2006. Management of sick children by Community Health Workers intervention models and programme; p. 80. [Google Scholar]
- 33.Um Boock A. Intégration de la lutte contre l'ulcère de Buruli dans le paquet minimum des activités, cas du Centre de santé Intégré de Ngoantet II au Cameroun. Rapport. Aide aux Lépreux Emmaüs-Suisse. Bureau régional pour l'Afrique; 2008; Yaoundé. [Google Scholar]
- 34.Um Boock A, Deffo M. Interprétation de l'ulcère de Buruli par les populations d'Ayos et d'Akonolinga dans la province du centre au Cameroun. Rapport. Aide aux Lépreux Emmaüs-Suisse. Bureau régional pour l'Afrique; 2004; Yaoundé. [Google Scholar]
- 35.Bigirwa P. Effectiveness of Community Health Workers (CHWs) in the provision of basic preventive and curative maternal, Newborn and Child Health (MNCH) interventions: a systematic review. Effectiveness of Community Health Workers (CHWs) in the provision of basic preventive. UMU Press. 2009;7(3):162–172. [Google Scholar]
- 36.OMS. L'ulcère de Buruli. Reconnaître et agir. Un guide pour le personnel de santé de terrain; 2011. p. 92. WHO/HTM/NTD/IDM/2011.2. [Google Scholar]
- 37.Prasad BM, Muraleedharan VR. Chennai, India: Community Health Workers: a review of concepts, practice and policy concerns, Department of Humanities and Social Sciences, IT Madras; 2007. p. 32. [Google Scholar]
- 38.Habicht JP, Victoria CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol. 1999 Feb;28(1):10–8. doi: 10.1093/ije/28.1.10. [DOI] [PubMed] [Google Scholar]
- 39.Kibadi K, Aujourat I, Meyers WM, Mokassa L, Muyembe T, Portaels F. Etudes des appellations et des représentations attachées dans différents pays endémiques d'Afrique. Med Trop. 2007;(67):241–248. [PubMed] [Google Scholar]
- 40.Ackumey MM, Kwakye-Maclean C, Ampadu EO, de Savigny D, Weiss MG. Health services for Buruli ulcer control: lessons from a field study in Ghana. PLoS Negl Trop Dis. 2011 Jun;5(6):e1187. doi: 10.1371/journal.pntd.0001187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kibadi K, Boelaert M, Kayinua M, Minuku JB, et al. Therapeutic itineraries of patients with ulcerated forms of Mycobacterium ulcerans (Buruli ulcer) disease in a rural health zone in the Democratic Republic of Congo. Trop Med Int Health. 2009 Sep;14(9):1110–6. doi: 10.1111/j.1365-3156.2009.02324.x. [DOI] [PubMed] [Google Scholar]
- 42.Christopher JB, May AL, Lewin S, Ross DA. Thirty years after Alma-Ata: A systematic review of the impact of community health workers delivering curative interventions against malaria, pneumonia and diarrhoea on child mortality and morbidity in sub-Saharan Africa. Hum Resour Health. 2011 Oct 24;9(1):27. doi: 10.1186/1478-4491-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chopra M, Munro S, Lavis JN, Vist G, Bennett S. Effects of policy options for human resources for health: an analysis of systematic reviews. Lancet. 2008;(371):668–74. doi: 10.1016/S0140-6736(08)60305-0. [DOI] [PubMed] [Google Scholar]
- 44.Dudley L, Garner P. Strategies for integrating primary health services in low-and middle-income countries at the point of delivery. Cochrane Database Syst Rev. 2011 Jul 6;(7):CD003318. doi: 10.1002/14651858.CD003318.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haines ASD, Lehmann U, Rowe AK, Lawn JE, et al. Achieving child survival goals: Potential contribution of Community Health Workers. Lancet. 2007 Jun 23;369(9579):2121–31. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]


