Abstract
Background
There is growing interest in how frequently patients undergoing coronary artery bypass graft (CABG) surgery require hospital readmission within 30-days of discharge. Readmissions, however, may not capture all hospital-based, acute care needs after discharge. The purpose of this study is to describe the frequency of and diagnoses associated with emergency department (ED) visits and hospital readmissions within 30-days of discharge following CABG surgery and to compare outcomes across hospitals.
Methods
Using the California State Inpatient and Emergency Department Databases, we identified all adults who underwent isolated CABG surgery between January 2005 and June 2009. We then calculated hospital's 30-day, risk-standardized readmission and ED visit rates using hierarchical generalized linear models. The correlation between hospital readmission and ED visit rates was estimated, weighting for hospital volume.
Results
We identified 63,911 adults who underwent isolated CABG surgery at 114 hospitals. Hospital 30-day, risk-standardized ED visit without readmission rates (median ED visit rate = 11.9%, 25th-75th percentile, 10.5%-13.7%) nearly equaled the hospital 30-day risk-standardized readmission rates (median readmission rate = 15.0%, 25th-75th percentile, 13.5%-16.5%). Both outcomes varied widely among hospitals. A composite of these outcomes, the median 30-day risk-standardized hospital-based, acute care rate was 23.9% (25th-75th percentile, 22.2%-25.5%). Post-operative infections, congestive heart failure, and chest discomfort were among the most common reasons for both readmissions and ED visits. Hospitals' 30-day risk-standardized ED visit and readmission rates were not significantly correlated (weighted correlation coefficient = -0.07, p = 0.44).
Conclusions
Patients discharged after CABG surgery frequently experienced ED visits and hospital readmissions within 30 days, often for similar diagnoses. Monitoring both hospital readmissions and ED visits following CABG surgery is important to our understanding of hospital-based, acute care needs following discharge.
Keywords: Coronary artery bypass graft surgery, readmission, emergency department visits, health policy
Introduction
Over 200,000 coronary artery bypass graft (CABG) surgeries are performed in the United States annually.1 CABG surgery is often considered a high-risk procedure associated with a 30-day, morbidity and mortality rate up to 14.0% and 2.0%, respectively.2 However, these rates do not capture the additional acute health care needs of patients undergoing CABG surgery. For instance, nearly 14% of the Medicare population is readmitted within 30 days of discharge, many for complications from and care related to the surgery.3-5 Moreover, not all patients with acute health care needs are readmitted. Recent studies of hospitalized patients suggest a growing number are returning to emergency departments (ED) without being readmitted.6 These visits also represent meaningful clinical events for patients, add costs to care, and their frequency may be inversely related to the quality of care received.7-8
Understanding how often patients discharged following CABG surgery require hospital-based, acute care, including hospital readmissions and ED visits, is critical to improving care for patients because states are increasingly reporting readmission rates as a quality measure. Hospitals with better than average rates could be studied more closely to identify best practices in discharge care for CABG surgery patients. Furthermore, if hospitals with low readmission rates are found to have very high ED rates, it would suggest that currently used performance measures are not likely to steer patients towards the highest quality hospitals.
Using data from the Healthcare Cost and Utilization Project, we studied post-discharge outcomes among patients undergoing CABG surgery in California. Our objectives included defining hospital-level, 30-day readmission and ED visit rates among all California hospitals performing CABG surgery; describing variation across hospitals for both outcomes; determining the relationship between readmissions and ED visits; and exploring how measurement of readmissions alone versus readmissions plus ED visits impacts hospitals' estimated performance when using these measures to determine quality of care.
Material and Methods
We used data from the 2005-2009 California State Inpatient9 and Emergency Department Databases.10 The inpatient database contains all inpatient discharges from short-term, acute-care, non-federal hospitals, whereas the emergency department database contains all ED visits not resulting in hospital admission. For both databases, each discharge abstract includes socio-demographic, hospital, and clinical variables, as well as up to 25 diagnostic and 21 procedure codes based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coding. Additionally, these datasets contain two variables to facilitate longitudinal studies of patient care across healthcare settings: 1) an encrypted patient identifier that is consistent across databases; and 2) a variable to specify the time that has elapsed between each encounter.
Study sample
From the inpatient database, we identified California residents at least 18 years of age who underwent isolated CABG surgery between January 1, 2005 and June 30, 2009. Isolated CABG surgery was defined as evidence of CABG (ICD-9-CM codes 36.1x) without a concurrent valve procedure (ICD-9-CM codes 35.10-35.14, 35.20-35.28) or major organ transplant (ICD-9-CM codes 33.50-33.52, 50.51, 50.59, 52.80, 52.82, 52.83, 55.61, 55.69). From this population (N = 70,698), we excluded discharges for pregnancy (N = 5); where the disposition was missing (N = 93), against medical advice (N = 78), or in-hospital death (N = 1,532); and discharges with a length of stay < 1 or > 100 days (N = 38); a missing patient identifier (N = 3,310); and those resulting in transfer to another acute care hospital (N = 883). If a patient had more than 1 discharge meeting these criteria (N = 121), the first discharge was used for analysis. Finally, we excluded patients who underwent CABG surgery at hospitals that did not have at least 1 CABG discharge during each year of the study to ensure only hospitals with active CABG surgery programs were included (N = 14 hospitals, affecting 727 patients; see Figure 1).
Figure 1.
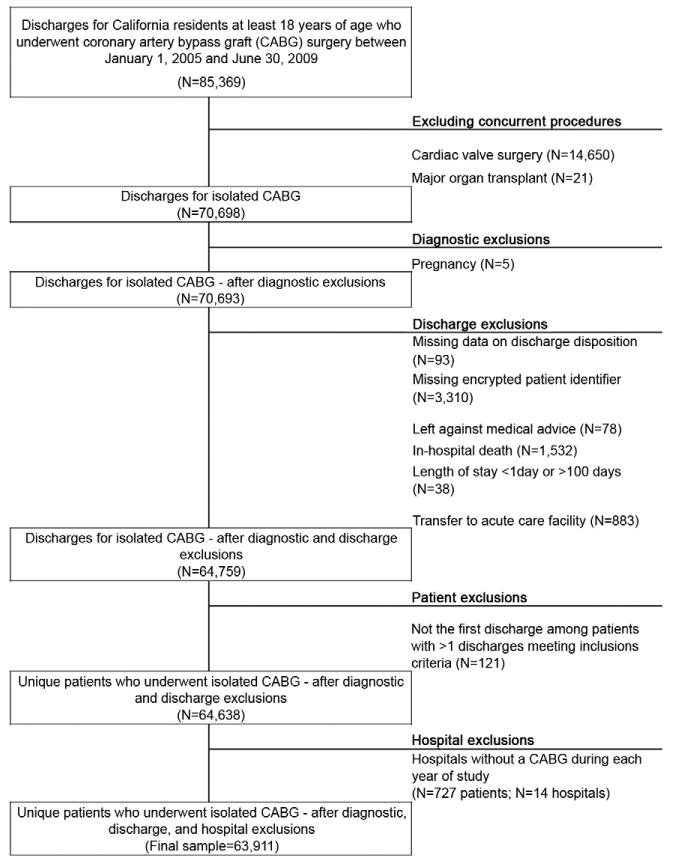
Patient selection process.
Main Outcome Measures
Our main outcome measures were 30-day, hospital-level, risk-standardized readmission, ED visit, and hospital-based, acute care rates. For this study, a readmission was defined as any hospital readmission excluding admissions related to rehabilitation services (ICD-9-CM V52.0-V52.1, V52.4, V52.8-V52.9, V53.8, V57.0-V57.22, V57.3-V57.4, V57.81, V57.89, V57.9, V58.82). An ED visit was defined as any ED visit that did not result in hospital. The hospital-based, acute care rate was a composite measure of any readmission or ED visit within 30 days of discharge. In cases where a patient experienced a readmission and an ED visit during the 30-day period, they were counted only once in the composite measure.
Confounders for adjustment
In order to risk adjust the observed hospital outcomes and account for differences in patient characteristics, we first identified 41 candidate variables for risk-adjustment based on current public reporting programs11 and recent publications.3, 12-13,14-15 Next, we entered these as independent variables into a logistic regression model with hospital based, acute care within 30 days as the dependent variable. Using stepwise selection with an entry P value of 0.15 and a retention P value of 0.05, we identified 30 variables significantly associated with the outcome and had face validity from clinician review (JPF, LGS, JSR). Four variables were added based on prior literature review, although they were not significantly associated with hospital-based, acute care within 30-days: alcohol abuse, chronic deficiency anemia (ICD-9-CM 280.1-280.9, 281.x), coagulopathy (ICD-9-CM 286.x, 287.1, 287.3- 287.5), and metastatic cancer. The final variables for risk-adjustment included: age, sex, primary payer, acuity of admission, 26 co-morbid medical conditions, whether the internal mammary artery was used for revascularization (ICD-9-CM codes 36.15, 36.16), if acute myocardial infarction was a primary diagnosis, if acute myocardial infarction was a secondary diagnosis (ICD-9-CM codes 410.x), and the number of vessels bypassed (see Appendix for full models). The final model is similar to those used for the public reporting of hospital readmission rates following CABG surgery.11, 16 In-hospital complications, which may influence the need for hospital-based, acute care following discharge, were not included in the final model to prevent “risk-adjusting” for low quality care.
Calculation of the Risk-Standardized Outcomes
We created 2-level (patient and hospital) hierarchical logistic regression models for each of 30 day outcome of interest: readmission, ED visit, and hospital-based, acute care, based on methods currently used by the Center for Medicare and Medicaid Services hospital quality outcomes measurement program.17-18 The covariates included in the models are those described above. Models included hospital-level random intercepts to account for clustering of patients within hospitals and permit separation of the within and between hospital variation in outcomes after accounting for patient characteristics. The predicted-to-estimated ratio obtained from these models was then multiplied by the mean, unadjusted outcome rate among all hospitals included in the study to yield the risk-standardized rates.
Relationship among Risk-Standardized Outcomes
We assessed the correlation between hospitals' risk-standardized readmission rates and the risk-standardized hospital-based, acute care rates, weighted by hospital volume. To determine how inclusion of ED visits would impact hospitals' performance relative to peer hospitals, we ranked all hospital's performance into tertiles based on the risk-standardized readmission and the risk-standardized hospital-based, acute care rates. Then, we determined the “inter-rater reliability” between these measures using the percent agreement and kappa scores.
All analyses were conducted using SAS version 9.2 (Cary, North Carolina). All statistical tests were 2-sided and p-values <0.05 were considered significant. Because this study used publicly available data without patient identifiers, it was considered exempt from review by the Yale University Human Investigations Committee.
Results
Between January 2005 and June 2009, 63,911 California residents underwent isolated CABG surgery at 114 hospitals. Most patients were over 60 years of age (72.4%), male (74.5%), White, non-Hispanic (63.7%), and had Medicare as their primary form of insurance (52.4%). In this sample of patients who survived to discharge, 3,631 (5.7%) patients experienced intra-operative complications; 14,680 (23.0%) had at least one post-operative complication; and the median length of stay was 8.0 days (standard deviation = 6.6 days; Table 1).
Table 1. Characteristics of California residents who underwent isolated cardiac bypass.
| Overall | ||
|---|---|---|
|
| ||
| N | (%) | |
| Overall | 63,911 | 100 |
| Age group | ||
| 18-49 years | 4,289 | 6.7 |
| 50-59 years | 13,360 | 20.9 |
| 60-69 years | 20,852 | 32.6 |
| 70-79 years | 18,825 | 29.5 |
| 80+ years | 6,585 | 10.3 |
| Sex | ||
| Male | 47,620 | 74.5 |
| Female | 16,291 | 25.5 |
| Race and ethnicity | ||
| White, non-Hispanic | 40,716 | 63.7 |
| Black, non-Hispanic | 2,148 | 3.4 |
| Hispanic | 10,226 | 16 |
| Other | 8,060 | 12.6 |
| Missing | 2,761 | 4.3 |
| Primary payer | ||
| Medicare | 33,467 | 52.4 |
| Medicaid | 4,789 | 7.5 |
| Private | 22,118 | 34.6 |
| Other | 3,537 | 5.5 |
| Comorbid medical conditions1 | ||
| 0 | 2,172 | 3.4 |
| 1-2 | 22,784 | 35.7 |
| 3-4 | 23,848 | 37.3 |
| 5 + | 15,107 | 23.6 |
| Scheduled admission | 29,141 | 45.6 |
| Primary diagnosis of myocardial infarction | 15,681 | 24.5 |
| Secondary diagnosis of myocardial infarction | 4,053 | 6.3 |
| Percutaneous coronary intervention during same hospitalization | 963 | 1.5 |
| Revascularization with internal mammary artery | 56,949 | 89.1 |
| Vessels bypassed | ||
| 1 vessel | 47,925 | 75.0 |
| 2 vessels | 6,651 | 10.4 |
| 3 vessels | 5,100 | 8.0 |
| 4+ vessels | 3,082 | 4.8 |
| Not specified | 1,153 | 1.8 |
| Off-pump surgery | 13,879 | 21.7 |
| In-hospital outcomes | ||
| Intra-operative morbidity | 3,631 | 5.7 |
| Post-operative morbidity | 14,680 | 23.0 |
| Median length of stay, days (standard deviation) | 8 | (6.6) |
Number of Elixhauser14 comorbidities present
Risk-Standardized Outcomes Post-CABG Surgery
The median risk-standardized, 30-day readmission rate was 15.0% (25th-75th percentile, 13.5%-16.5%). In addition, the risk-standardized ED visit rate was 11.9% (25th-75th percentile, 10.5%-13.7%). Collectively, the overall risk-standardized, hospital-based, acute care rate was 23.9% (25th-75th percentile, 22.2%-25.5%; Figure 2A-C). Our final risk adjustment model for hospital-based, acute care within 30-days had a c-statistic of 0.63. Several patient demographic and clinical variables were associated with higher odds of returning to the hospital (see Appendix 1).
Figure 2.
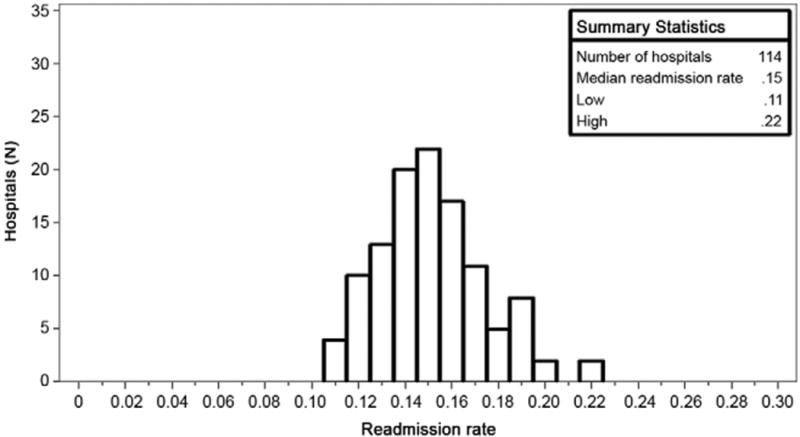
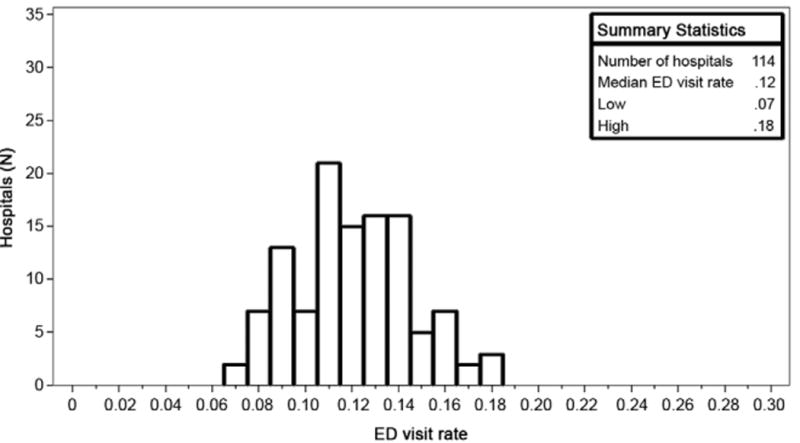
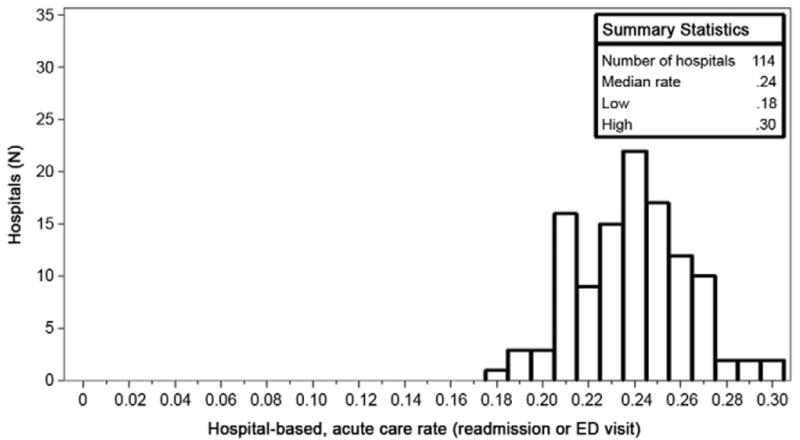
A-C. Distributions of hospital-level outcome rates.
Description of Readmission and ED Visits
Within our sample, 6.2% of patients experienced more than one readmission or ED visit within 30 days. Including these multiple visits, there were 32 hospital-based, acute care encounters per 100 discharges after CABG surgery. While no single diagnosis accounted for the majority of readmissions, three of the most common readmission diagnoses were also among the most common diagnoses listed for ED visits: post-operative infections, congestive heart failure, and chest discomfort. For emergency department visits specifically, symptoms of pain were common associated diagnoses (Table 2). Because the first listed diagnosis is based on ICD-9-CM coding, related diagnoses (i.e., chest pain and chest discomfort) are listed separately among the most common conditions.
Table 2. 30-day hospital utilization rates among 63,911 patients undergoing isolated CABG in 114 California.
| Readmissions | ED visits1 | Hospital-based, acute care | |
|---|---|---|---|
|
|
|||
| Hospital-level rates | |||
| Observed rate, median (IQR) | 15.2 (4.9) | 11.5 (4.3) | 24.0 (5.2) |
| Risk standardized rate, median (IQR) | 15.0 (2.9) | 11.9 (3.3) | 23.9 (3.3) |
| Occurred at a hospital other than the discharging hospital for coronary artery bypass (%) | 63.0% | 53.7% | 58.9% |
| Most common associated primary diagnoses (% of all encounters) | |||
|---|---|---|---|
|
|
|||
| Most common | Post-operative infection (11.6%) | Chest pain (6.9%) | Post-operative infection (8.1%) |
| 2nd | Congestive heart failure (9.9%) | Chest discomfort (4.0%) | Congestive heart failure (6.9%) |
| 3rd | Pleural effusion (3.3%) | Post-operative infection (3.4%) | Chest pain (3.6%) |
| 4th | Pneumonia (3.0%) | Painful respirations (3.3%) | Chest discomfort (3.4%) |
| 5th | Chest discomfort (2.9%) | Congestive heart failure (3.2%) | Pleural effusion (3.1%) |
Only includes encounters which did not result in admission
Comparing Hospital Performance When Measured By Readmission or Hospital-based, Acute Care Rates
There was no correlation between hospital risk-standardized, 30-day readmission and ED visit rates (weighted correlation coefficient=-0.07, p=0.44; Figure 3). When comparing performance based on the risk-standardized readmission and the risk-standardized hospital-based, acute care rates separately, 52 out of 114 hospitals (45.6%) would appear in a different tertile of performance. Specifically, of the 38 hospitals in the best performing tertile for the risk-standardized readmission rates, 16 hospitals would move to the middle (N=13; 11.4%) or lowest tertile (N=3; 2.6%) of the risk-standardized hospital-based, acute care rates. Conversely, 10 (8.8%) hospitals in the lowest performing tertile for the risk-standardized readmission rates would move to the middle and 3 (2.6%) would move to the highest tertile of the hospital-based, acute care measure. The overall agreement between readmission and hospital-based, acute care measures was moderate (weighted kappa = 0.43 [95% CI=0.30-0.56, p = 0.99]).
Figure 3.
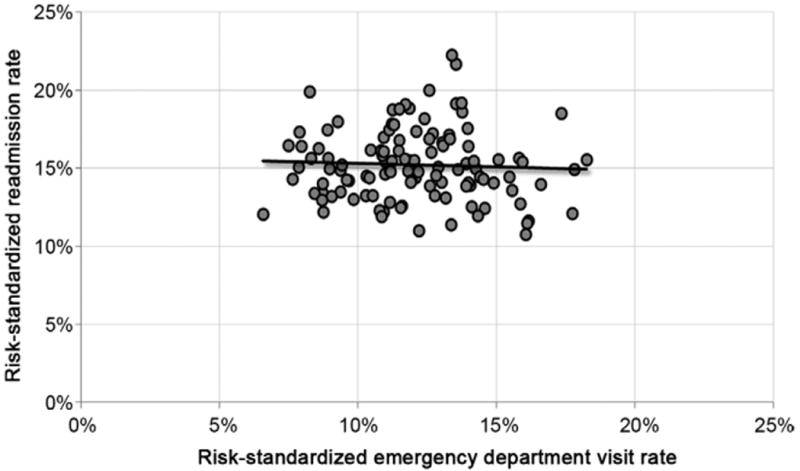
Correlation of hospital 30-day, risk-standardized readmission and ED visit rates.
Comment
Our analysis suggests that a substantial proportion of patients discharged after isolated CABG surgery in California hospitals receive hospital-based, acute care within 30-days. Nearly 12% of patients discharged after CABG surgery returned to the ED but did not require a subsequent hospitalization. Of these encounters, many were likely a consequence of the initial CABG surgery, including post-operative complications and pain. Similarly, more than 15% of patients discharged after CABG surgery were readmitted to a hospital within 30 days. Taken together, our findings indicate that there is a heavier burden on patients following isolated CABG surgery than had been previously understood, with nearly 25% of patients requiring hospital-based, acute care within 30 days of discharge.
As nearly half of the post-CABG surgery acute care needs of these patients were successfully managed in the emergency department without subsequent hospitalization, perhaps pre-discharge interventions and greater continuity of care post-discharge could help avoid the need for ED visits or even subsequent readmissions. For example, a more integrated discharge process geared toward empowering patients in their own care,19-20 ensuring timely outpatient follow-up with a healthcare provider familiar with the patient's in-hospital treatment,21 and making available an “after hours” point of contact all may help avoid emergency department visits.22 However, published studies of these interventions were in the setting of reducing readmissions after CABG surgery and their impact on reducing emergency department visits after CABG surgery is unknown. Further studies should focus on identifying patients “at-risk” for either ED utilization or readmission to identify potential targets for intervention.
While the median rate of hospital-based, acute care post-discharge after isolated CABG surgery was 24%, this ranged from a low of 18% to a high of 30% despite adjustment for hospitals' case mix. Though variation in readmission rates was recently described,3 also using California data, this work focused explicitly on readmissions and did not evaluate rates or variation in ED visits, which we demonstrate to be nearly equal in number to readmissions. The wide variation in need for acute care post-discharge suggests that significant improvements can be made among hospitals, particularly those with the highest rates. It is important to note that hospitals' risk-standardized readmission and ED visit rates were not correlated. Hospitals with the highest ED visit rates did not have the lowest readmission rates. Conversely, hospitals with the highest readmission rates did not have the lowest ED visit rates.
Monitoring ED use post-discharge is valuable and may provide additional insights into the quality of care provided. If emergency department visits were included with readmissions as an overall measure of hospital-based, acute care needs following discharge, there could be substantial changes to hospitals' perceived performance. In the current study, nearly half of the hospitals examined would be ranked in a different tertile of performance upon comparison to their peers. The policy implications for this scenario deserve careful consideration as legislation mandating financial penalties for hospitals with excess readmission rates following hospitalization for some acute conditions will soon be implemented. Formal monitoring of the impact of reducing readmissions on utilization of care in other healthcare settings, such as the emergency department, as well as patient outcomes like mortality, is needed. Decreasing reimbursement for high readmission rates could cause a shift in patient care to “unmeasured” settings like emergency departments or observational units at some institutions. While these care settings may be less costly, they are no less meaningful to patients nor do they necessarily improve the quality of care provided.
The findings of this study should be viewed in the context of several limitations. First, CABG surgery cases were identified by administrative coding and could be susceptible to error, however prior studies suggest identification of CABG surgery from ICD-9-CM coding has a positive predictive value between 96-98%.23 Second, we are unable to determine if a patient died during the 30-day window in a non-hospital setting. Because of this, patients who died during the 30-day period were no longer “at-risk” for readmission. As we were unable to exclude them from the denominator, hospitals with high 30-day out of hospital mortality may appear as if they were performing well in terms of readmissions or revisits. Because the overall, 30-day mortality following CABG surgery is generally low (<3%)24 this should not have a significant impact on our results. Third, risk-adjustment based on administrative data can be imperfect and may not adequately account for variation in patient mix across hospitals. For instance, relevant clinical information, such as pre-operative ejection fraction, was not available in our data. Finally, the current study does not include patients who were cared for in other ambulatory care environments, including observation units without a preceding emergency department visit or subsequent hospital admission.
In conclusion, patients undergoing CABG surgery frequently require hospital-based acute care within 30-days of discharge. Nearly 25% of patients discharged after CABG surgery were either seen within an emergency department or readmitted to a hospital within 30 days. Considering both readmissions and ED visits as an overall hospital-based, acute care measure may provide additional information about hospital performance not captured by measuring readmission alone.
Acknowledgments
Support for this project was provided in part by the Robert Wood Johnson Foundation's Clinical Scholar Program. The sponsor played no role in the design of the study, analysis or interpretation of findings, or drafting the manuscript and did not review or approve the manuscript prior to submission. The authors assume full responsibility for the accuracy and completeness of the ideas presented. Drs. Suter, Krumholz and Ross and Mr. Wang receive support from Contract Number HHSM-500-2008-0025I/HHSM-500-T0001, Modification No. 000005, entitled “Measure & Instrument Development and Support (MIDS)-Development and Re-evaluation of the CMS Hospital Outcomes and Efficiency Measures,” funded by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. Dr. Suter receives support from the Department of Veterans Affairs Connecticut Healthcare System, West Haven, Connecticut. Dr. Krumholz receives support from grant U01 HL105270-03 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute in Bethesda, Maryland. Dr. Ross receives support from the National Institute on Aging (K08 AG032886) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program.
Appendix 1: Final risk-adjustment model for associations with hospital-based, acute care within 30-days of discharge
| N | Hospital-based, acute care in 30-days (%) | Point Estimate | 95% Confidence Limits | ||
|---|---|---|---|---|---|
|
|
|||||
| Age | |||||
| 18-49 years | 4,289 | 24.7 | Reference | ||
| 50-59 years | 13,360 | 22.4 | 0.88 | 0.81 | 0.96 |
| 60-69 years | 20,852 | 21.8 | 0.78 | 0.71 | 0.85 |
| 70-79 years | 18,825 | 24.9 | 0.83 | 0.76 | 0.90 |
| 80+ years | 6,585 | 29.0 | 0.98 | 0.89 | 1.08 |
| Female | 16,291 | 29.4 | 1.30 | 1.25 | 1.37 |
| Primary payer | |||||
| Medicare | 33,467 | 25.8 | Reference | ||
| Medicaid | 4,789 | 31.1 | 1.19 | 1.11 | 1.28 |
| Private | 22,118 | 19.0 | 0.78 | 0.73 | 0.82 |
| Other | 3,537 | 24.3 | 0.93 | 0.84 | 1.02 |
| Scheduled admission | 29,141 | 20.7 | 0.83 | 0.80 | 0.86 |
| Comorbid medical conditions | |||||
| Congestive Heart Failure | 15,137 | 31.2 | 1.22 | 1.17 | 1.27 |
| Cardiac Arrhythmia | 24,912 | 26.4 | 1.17 | 1.12 | 1.22 |
| Valvular Disease | 6,826 | 27.9 | 1.07 | 1.01 | 1.12 |
| Peripheral Vascular Disorders | 9,070 | 28.7 | 1.13 | 1.07 | 1.19 |
| Hypertension Uncomplicated | 42,149 | 22.5 | 1.02 | 0.97 | 1.08 |
| Hypertension Complicated | 10,042 | 31.7 | 0.97 | 0.88 | 1.07 |
| Paralysis | 422 | 31.3 | 1.12 | 0.89 | 1.42 |
| Other Neurological Disorders | 2,170 | 32.5 | 1.25 | 1.15 | 1.36 |
| Chronic Pulmonary Disease | 14,699 | 27.7 | 1.21 | 1.16 | 1.27 |
| Diabetes Uncomplicated | 22,807 | 25.7 | 1.21 | 1.16 | 1.27 |
| Diabetes Complicated | 5,218 | 33.7 | 1.40 | 1.27 | 1.53 |
| Hypothyroidism | 5,172 | 26.5 | 1.00 | 0.94 | 1.07 |
| Renal Failure | 8,651 | 33.5 | 1.39 | 1.26 | 1.53 |
| Liver Disease | 1,172 | 32.3 | 1.28 | 1.13 | 1.45 |
| Metastatic Cancer | 93 | 22.6 | 0.85 | 0.49 | 1.47 |
| Solid Tumor without Metastasis | 793 | 25.5 | 1.10 | 0.93 | 1.31 |
| Rheumatoid Arthritis/collagen | 949 | 29.4 | 1.21 | 1.03 | 1.42 |
| Coagulopathy | 5,312 | 26.9 | 1.07 | 1.00 | 1.14 |
| Obesity | 11,630 | 26.3 | 1.09 | 1.05 | 1.14 |
| Weight Loss | 911 | 35.5 | 1.12 | 0.99 | 1.28 |
| Fluid and Electrolyte Disorders | 9,787 | 28.9 | 1.07 | 1.02 | 1.13 |
| Deficiency Anemia | 1,067 | 29.8 | 1.00 | 0.88 | 1.14 |
| Alcohol Abuse | 1,897 | 25.6 | 1.00 | 0.89 | 1.13 |
| Drug Abuse | 1,154 | 33.4 | 1.41 | 1.26 | 1.59 |
| Psychoses | 538 | 32.9 | 1.24 | 1.03 | 1.51 |
| Depression | 3,281 | 31.8 | 1.32 | 1.22 | 1.43 |
| Revascularization with internal mammary artery | 56,949 | 23.4 | 0.93 | 0.86 | 1.00 |
| Primary diagnosis of myocardial infarction | 15,681 | 27.0 | 1.06 | 1.00 | 1.12 |
| Secondary diagnosis of myocardial infarction | 4,053 | 27.8 | 1.12 | 1.04 | 1.20 |
| Vessels bypassed | |||||
| 1 vessel | 47,925 | 21.6 | Reference | ||
| 2 vessels | 6,651 | 23.7 | 1.18 | 1.03 | 1.36 |
| 3 vessels | 5,100 | 23.8 | 1.18 | 1.03 | 1.35 |
| 4+ vessels | 3,082 | 25.0 | 1.16 | 1.00 | 1.36 |
| Not specified | 1,153 | 24.5 | 1.15 | 1.00 | 1.34 |
c-statistic = 0.63
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Riley RF, Don CW, Powell W, Maynard C, Dean LS. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes. 2011 Mar;4(2):193–197. doi: 10.1161/CIRCOUTCOMES.110.958744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shahian DM, O'Brien SM, Normand SL, Peterson ED, Edwards FH. Association of hospital coronary artery bypass volume with processes of care, mortality, morbidity, and the Society of Thoracic Surgeons composite quality score. J Thorac Cardiovasc Surg. 2010 Feb;139(2):273–282. doi: 10.1016/j.jtcvs.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Hannan EL, Zhong Y, Lahey SJ, et al. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011 May;4(5):569–576. doi: 10.1016/j.jcin.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 4.MedPAC. June 2007 Report to Congress Promoting Greater Efficiency in Medicare. [Accessed Jan 13, 2012];2007 http://www.medpac.gov/chapters/Jun07_Ch05.pdf.
- 5.Li Z, Amstrong EJ, Parker JP, Danielsen B, Romano PS. Hospital Variation in Readmission After Coronary Artery Bypass Surgery in California. Circ Cardiovasc Qual Outcomes. 2012 Sep;5(5):729–37. doi: 10.1161/CIRCOUTCOMES.112.966945. [DOI] [PubMed] [Google Scholar]
- 6.Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013 Jan;309(4):364–371. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown DL. Measuring outcomes of coronary artery bypass surgery: what is important and to whom? Arch Int Med. 2010 Jul;170(14):1189–1190. doi: 10.1001/archinternmed.2010.238. [DOI] [PubMed] [Google Scholar]
- 8.Gordon J, Sheppard LA, Anaf S. The patient experience in the emergency department: A systematic synthesis of qualitative research. Int Emerg Nurs. 2010 Apr;18(2):80–88. doi: 10.1016/j.ienj.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 9.HCUP. State Inpatient Database (SID). Healthcare Cost and Utilization Project (HCUP) 2009 www.hcup-us.ahrq.gov/nisoverview.jsp.
- 10.HCUP. State Emergency Department Database (SEDD). Healthcare Cost and Utilization Project (HCUP) 2009 www.hcup-us.ahrq.gov/nisoverview.jsp.
- 11.Pennsylvania Health Care Cost Containment Council. Cardiac Surgery in Pennsylvania, 2008-2009. [Accessed Jan 16, 2012]; http://www.phc4.org/reports/cabg/09/docs/cabg2009report.pdf.
- 12.Slamowicz R, Erbas B, Sundararajan V, Dharmage S. Predictors of readmission after elective coronary artery bypass graft surgery. Aust Health Rev. 2008 Nov;32(4):677–683. doi: 10.1071/ah080677. [DOI] [PubMed] [Google Scholar]
- 13.Auerbach AD, Hilton JF, Maselli J, et al. Shop for quality or volume? Volume, quality, and outcomes of coronary artery bypass surgery. Ann Intern Med. 2009 May;150(10):696–704. doi: 10.7326/0003-4819-150-10-200905190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 16.The Leapfrog Group. The Leapfrog Hospital Survey Reference Book. [Accessed Jan, 2012]; http://www.leapfroggroup.org/media/file/2011SurveyReference.pdf.
- 17.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008 Sep;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 18.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011 Mar;4(2):243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med Care. 1993 Apr;31(4):358–370. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 21.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010 May;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 22.Kwok T, Lum CM, Chan HS, Ma HM, Lee D, Woo J. A randomized, controlled trial of an intensive community nurse-supported discharge program in preventing hospital readmissions of older patients with chronic lung disease. J Am Geriatr Soc. 2004 Aug;52(8):1240–1246. doi: 10.1111/j.1532-5415.2004.52351.x. [DOI] [PubMed] [Google Scholar]
- 23.Lee DS, Stitt A, Wang X, et al. Administrative Hospitalization Database Validation of Cardiac Procedure Codes. Med Care. 2013 Apr;51(4):e22–6. doi: 10.1097/MLR.0b013e3182329778. [DOI] [PubMed] [Google Scholar]
- 24.Shahian DM, O'Brien SM, Sheng S, et al. Predictors of Long-Term Survival Following Coronary Artery Bypass Grafting Surgery: Results from The Society of Thoracic Surgeons Adult Cardiac Surgery Database (The ASCERT Study) Circulation. 2012 Mar;125(12):1491–500. doi: 10.1161/CIRCULATIONAHA.111.066902. [DOI] [PMC free article] [PubMed] [Google Scholar]


