Abstract
Objectives
Although the co-occurrence of multiple risk factors increases the risk of cardiovascular disease (CVD) morbidity/mortality, few studies have examined the prevalence of risk factor clustering among African Americans in community-based faith settings. This study examined the prevalence and clustering of CVD risk factors in a sample of church members from South Carolina.
Design
Cross-sectional analysis of baseline data from a faith-based intervention, Faith, Activity, and Nutrition (FAN).
Setting
African Methodist Episcopal churches in four geographically-defined districts in South Carolina.
Participants
1119 church members.
Main Outcome Measures
Self-reported presence or absence of healthcare provider diagnosed diabetes, high cholesterol, and hypertension. Objectively measured blood pressure, height, and weight (body mass index) were also taken. The prevalence of single, multiple, and clustering of risk factors was computed.
Results
62% of participants were obese, 64% had hypertension, 23% had diabetes, and 39% had high cholesterol; 15% had no risk factors, 24% had 1 risk factor, 30% had 2 risk factors, 22% had 3 risk factors, and 10% had 4 risk factors. The most common clusters of risk factors were: obese and hypertensive (18%), obese, hypertensive and hypercholesterolemic (13%), and obese, hypertensive, hypercholesterolemic, and diabetic (10%).
Conclusions
The prevalence of risk factors and risk factor clustering in church members in South Carolina is exceedingly high. Culturally-relevant behavioral interventions targeting risk factor reduction in this population should be a public health goal.
Keywords: Cardiovascular Disease, Risk Factors, African Americans, Community Health, Faith-based Settings, Church Members
Introduction
Since 1900, cardiovascular disease (CVD) has been the leading cause of death in the United States every year except 1918.1 The prevalence of CVD and associated risk factors, as well as death rates from CVD, is higher in African Americans than Caucasians.1 The prevalence of high blood pressure in African Americans in the United States is among the highest in the world, and is continuing to increase.1 The prevalence of stroke and other CVDs is particularly high in the Southeastern United States,1–4 designated as the Stroke Belt in 1980 by the National Heart, Lung, and Blood Institute. South Carolina has the 6th highest death rate from stroke nationally and the 15th highest death rate from CVD.1 The leading cause of death among African American adults in South Carolina is heart disease, accounting for nearly 25% of all deaths in 2007.5
Cardiovascular disease risk factors tend to cluster.6–7 The co-occurrence of multiple risk factors increases the risk of CVD morbidity/mortality.8–11 Data from the 2003 Behavioral Risk Factor Surveillance System (BRFSS) indicate that the prevalence of having two or more risk factors (high blood pressure, high cholesterol, diabetes, obesity, smoking, physical inactivity) for heart disease and stroke is highest among African Americans (48.7%).12 In South Carolina, 17.6% of adults aged ≥18 years have no risk factors, 34.0% have one risk factor, and 48.4% have multiple risk factors.13 The high prevalence of risk factors among African Americans and South Carolinians may put these groups at a substantially higher risk for developing CVD or premature death due to CVD. Efforts to reduce risk should be a public health priority.
The clustering patterns of CVD risk factors among African American South Carolinians, a particularly high-risk population, have not been adequately described. Furthermore, few studies have examined the prevalence of risk factor clustering among African Americans in community-based faith settings. The purpose of this study was to quantify the percentage of African American adults from a church-based sample who had the following clinical/biological risk factors for CVD: obesity, hypertension, diabetes, and high cholesterol, and to examine the clustering of these risk factors among participants.
Methods
The Faith, Activity, and Nutrition (FAN) program is a 5-year physical activity and nutrition intervention implemented in African Methodist Episcopal (AME) churches in South Carolina. The FAN program uses a community-based participatory research approach in which a planning committee consisting of church leaders, church lay members, and university staff work together at all stages of the research project to develop, implement and evaluate the program. The primary goals of FAN are to increase moderate to vigorous intensity physical activity (PA) and fruit and vegetable consumption, and to improve blood pressure.14 The intervention targets are guided by the structural ecologic model; intervention activities aim to: 1) provide opportunities for PA and healthy eating; 2) make opportunities for PA and healthy eating enjoyable and relevant; 3) set organizational guidelines that support PA and healthy eating; and 4) get the message about PA and healthy eating out through cultural and media messages within the church.15 The present study uses baseline data only.
Church Recruitment and Data Collection
As reported in more detail elsewhere,14 pastors from four geographically-defined districts in South Carolina were sent letters from their presiding elder introducing the FAN program and inviting participation. Pastors from churches agreeing to participate in the FAN program typically asked the health director or another church member (FAN coordinator) to act as the liaison between the church and the FAN program staff to schedule and coordinate measurement sessions.
The liaisons from interested churches were asked to recruit members of their congregation to take part in a measurement session. At each measurement session, participants completed an informed consent form that was approved by the Institutional Review Board at the University of South Carolina and by the FAN planning committee. To be eligible, participants had to be aged ≥18 years, be free of serious medical conditions or disabilities that would make PA difficult, and attend worship services at least once a month.
Upon providing consent to participate, FAN staff administered physical assessments (eg, objectively measured blood pressure, height, and weight) with each participant. In addition, participants were asked to complete a survey that assessed: sociodemographic characteristics; physical activity, dietary, and other health-related practices; and psychosocial variables.
Measures
Sociodemographic and Health-related Variables
Participants were asked to self-report their age, sex, race, marital status, and highest grade or years of education completed. Participants also rated their general health status on a scale from 1 (excellent) to 5 (poor). Self-reported presence of diabetes, high cholesterol, and hypertension was defined as the participant reporting having been told by a doctor that he or she had that specific condition.16 Finally, participants were asked whether they had seen a healthcare provider in the past 12 months.
Blood Pressure
Resting blood pressure was taken three times on the right arm (60 second rest between each reading) after participant sat quietly for five minutes with legs uncrossed, with the automated DinaMap ProCare Monitor (DPC-100X-EN).17 The average of the second and third measures was used for statistical analyses. Participants with a systolic blood pressure ≥140mm Hg, diastolic blood pressure ≥90mm Hg,18 or self-reporting hypertension16 were classified as hypertensive.
Body Mass Index
Height to the nearest quarter inch and weight to the nearest 1/10 kilogram were obtained by trained staff. Body mass index (BMI) was calculated as kg/m2 using standard procedures. Participants with a BMI ≥30 kg/m2 were classified as obese.
Statistical Analyses
Risk factors were defined as: 1) BMI≥30 kg/m2; 2) healthcare provider diagnosis of hypertension or objectively measured blood pressure ≥140/90; 3) self-reported healthcare provider diagnosis of diabetes; and 4) self-reported healthcare provider diagnosis of high cholesterol.
Basic descriptive statistics included frequencies and means of key survey variables for the total sample and across risk factor groups (ie, participants with 0–4 total risk factors). Differences in demographic, health-related, and other key variables across risk factor groups were examined with χ2 or ANOVAs. The prevalence of single risk factors was calculated first, followed by the prevalence of multiple risk factors. A risk factor index was calculated by assigning a score of 1 each for the presence of obesity, hypertension, diabetes, and high cholesterol. Finally, each possible combination of risk factors (ie, risk factor clustering) was examined.
Results
Demographic and health-related characteristics of the total sample and for participants in each risk factor category are shown in Table 1. Information on the presence/absence of all risk factors was provided by 1191 participants. The mean age of the total sample was 54.1 ± 14.0 and the mean BMI was 32.9 ± 7.4 kg/m2. A majority of participants were female (75.9%), married (54.6%), had at least some college education (59.2%), and had total household incomes under $40,000 (56.6%). A majority of participants (94.0%) reported seeing a health professional in the past 12 months. In general, as the number of risk factors increased, so did age, BMI, and systolic and diastolic blood pressure. Those with the highest number of risk factors also reported lower levels of education and poorer self-rated health. Finally, those with two or more risk factors were more likely to have seen their healthcare provider in the past 12 months than those with fewer risk factors.
Table 1.
Baseline characteristics for the total sample (N=1119) and for each risk factor category
| n | Total sample (N=1119)
|
0 risk factors (n= 168)
|
1 risk factor (n=264)
|
2 risk factors (n=332)
|
3 risk factors (n=241)
|
4 risk factors (n=114)
|
|
|---|---|---|---|---|---|---|---|
| % or mean (SD) | |||||||
| Age, years† | 1119 | 54.1 (14.0) | 43.9 (13.5) | 49.3 (15.6) | 55.9 (12.1) | 60.1 (10.4) | 61.8 (9.4) |
| BMI, kg/m2† | 1119 | 32.9 (7.4) | 25.4 (3.1) | 31.9 (7.1) | 34.2 (7.3) | 35.2 (6.7) | 37.7 (6.0) |
| Sex | |||||||
| Male | 270 | 24.1 | 31.0 | 25.8 | 20.8 | 22.4 | 23.7 |
| Female | 849 | 75.9 | 69.1 | 74.2 | 79.2 | 77.6 | 76.3 |
| Education† | |||||||
| <HS grad | 107 | 9.6 | 6.6 | 7.6 | 9.3 | 12.0 | 14.0 |
| HS grad or GED | 350 | 31.3 | 26.2 | 23.5 | 31.6 | 34.0 | 50.0 |
| Some college | 332 | 29.7 | 31.6 | 36.4 | 27.4 | 30.3 | 16.7 |
| College grad | 330 | 29.5 | 35.7 | 32.6 | 31.6 | 23.7 | 19.3 |
| Marital status | |||||||
| Married | 608 | 54.6 | 54.5 | 52.7 | 53.8 | 56.9 | 56.6 |
| Not married | 506 | 45.4 | 45.5 | 47.3 | 46.2 | 43.2 | 43.4 |
| Income | |||||||
| <$20,000 | 276 | 27.8 | 22.6 | 20.8 | 30.7 | 30.6 | 38.0 |
| $20–$39,999 | 286 | 28.8 | 27.7 | 33.1 | 28.0 | 26.7 | 27.0 |
| $40–$59,999 | 220 | 22.2 | 27.1 | 22.9 | 19.3 | 22.8 | 20.0 |
| ≥$60,000 | 211 | 21.2 | 22.6 | 23.3 | 22.0 | 19.9 | 15.0 |
| Self-rated health† | |||||||
| Excellent | 54 | 4.8 | 15.5 | 4.6 | 2.4 | 3.3 | 0 |
| Very good | 279 | 24.9 | 41.1 | 29.6 | 27.1 | 14.5 | 6.1 |
| Good | 578 | 51.7 | 37.5 | 50.8 | 56.3 | 56.9 | 50.0 |
| Fair | 187 | 16.7 | 5.4 | 14.4 | 12.4 | 22.8 | 38.6 |
| Poor | 21 | 1.9 | 0.6 | 0.8 | 1.8 | 2.5 | 5.3 |
| Blood pressure, mm Hg | |||||||
| Systolic† | 1113 | 128.5 (20.7) | 113.5 (11.2) | 123.8 (17.0) | 134.3 (22.3) | 133.8 (20.3) | 133.3 (21.3) |
| Diastolic† | 1113 | 70.6 (10.6) | 66.1 (8.7) | 70.2 (9.6) | 73.1 (10.8) | 71.7 (11.1) | 68.4 (11.2) |
| Health care provider*† | |||||||
| No | 67 | 6.0 | 8.9 | 10.6 | 4.5 | 2.9 | 1.8 |
| Yes | 1050 | 94.0 | 91.1 | 89.4 | 95.5 | 97.1 | 98.3 |
Seen healthcare provider in past 12 months
Significant difference across risk factor groups (P<.05)
The prevalence of individual risk factors is shown in Table 2. Of the total sample, 61.9% were obese, 63.9% had self-reported and/or objectively measured hypertension, 39.4% had self-reported high cholesterol, and 23.1% had self-reported diabetes. When examining the prevalence of multiple risk factors, 15.0% had no risk factors, 23.6% had 1 risk factor, 29.7% had 2 risk factors, 21.5% had 3 risk factors, and 10.2% had 4 risk factors.
Table 2.
Prevalence of risk factors African American church members
| Risk factor | n (%) |
|---|---|
| Obese | |
| No | 426 (38.1) |
| Yes | 693 (61.9) |
| Hypertension | |
| No | 404 (36.1) |
| Yes | 715 (63.9) |
| Diabetes | |
| No | 861 (76.9) |
| Yes | 258 (23.1) |
| High Cholesterol | |
| No | 678 (60.6) |
| Yes | 441 (39.4) |
| Number of risk factors | |
| 0 | 168 (15.0) |
| 1 | 264 (23.6) |
| 2 | 332 (29.7) |
| 3 | 241 (21.5) |
| 4 | 114 (10.2) |
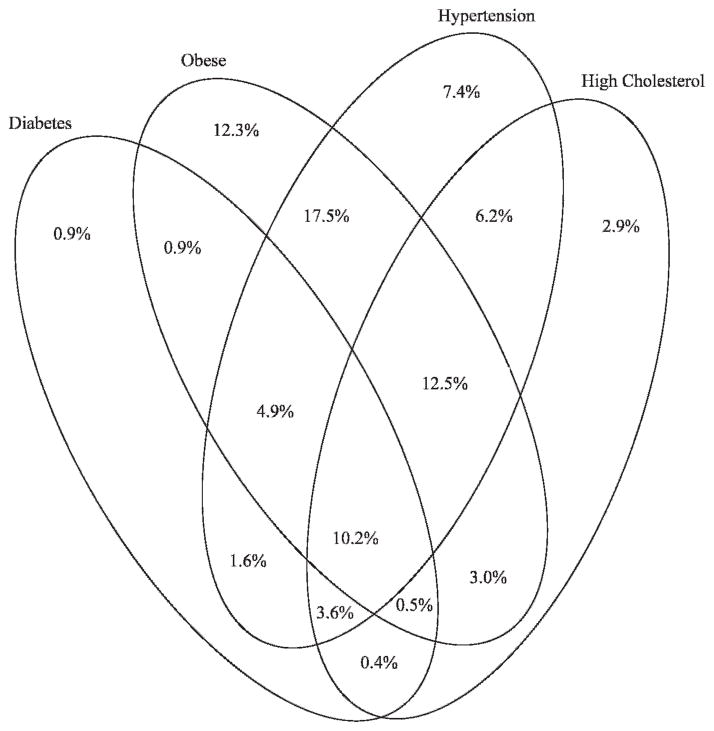
The cluster pattern of multiple risk factors is shown in Figure 1. The most common cluster of risk factors was being obese and hypertensive, occurring in 17.5% of participants. Following this cluster, 12.5% of participants were obese, hypertensive and hypercholesterolemic, and 10.2% of participants were obese, hypertensive, hypercholesterolemic and diabetic.
Fig. 1.
Risk factor clustering among African American church members
Discussion
Cardiovascular disease is a major public health problem and the leading cause of death among adults in the United States.1 Disproportionate rates of CVD risk factors are seen in minority populations, particularly African Americans.1,19 This study examined the prevalence and clustering of CVD risk factors in a sample of African American church members from South Carolina, a state with a high percentage of African Americans. The prevalence of risk factors in African American church members in our study was quite high, and a large percentage of participants had multiple risk factors, putting this population at an increased risk for CVD and premature death.
With the exception of high cholesterol, which was nearly identical (39%), the prevalence of risk factors in our sample was substantially higher than the prevalence estimated from the BRFSS. According to the BRFSS, in 2009, 39% of African American adults in South Carolina were obese, compared to the 62% in our sample; 13% had self-reported diabetes, compared to the 25% in our sample; and 35% had hypertension compared to the 64% in our sample.20 The BRFSS uses self-reported BMI and hypertension, whereas we used objectively measured BMI, and included both self-reported and objectively measured hypertension. However, 59% of our sample self-reported hypertension, which is still considerably higher than what was reported by the BRFSS. One potential explanation for these discrepancies is the differences in samples; our sample of African Americans was older and had fewer men than the BRFSS sample. Furthermore, a number of the counties or areas (eg, Williamsburg county) where we recruited were rural, had a higher-than-average percentage of African Americans, and had higher rates of poverty compared to the rest of the state.21 This could, in part, explain the higher prevalence of risk factors in our sample compared to the rest of South Carolina.
A small percentage (15%) of participants in this study had no risk factors, whereas 61% had at least 2 risk factors, and 32% had at least 3 risk factors. The most common clustering of risk factors was being obese and hypertensive, followed by being obese, hypertensive, and having high cholesterol. These findings are quite alarming and warrant a substantial public health effort to prevent and/or control these potentially hazardous risk factors. Studies have shown that African Americans with a specific set of factors (ie, risk factor clustering) are at a considerably higher risk for CVD.11,22
The clustering of risk factors among African American populations has not been adequately described in most faith-based studies targeting African Americans. In a previous study by Wilcox et al targeting African Americans (n=571) from AME churches in South Carolina, 42% of participants were obese, 53% had self-reported hypertension, 25% had self-reported diabetes, and 32% had self-reported high cholesterol.23 Project Joy was a faith-based physical activity and nutrition intervention targeting CVD risk profiles among African American women aged ≥40 years in Baltimore.24 In that sample (n=529) the mean BMI was 32 kg/m2, 55% had hypertension (≥140/90 or on medication), and 18% had diabetes (blood glucose ≥126 or on medication). Finally, Gittner and colleagues described CVD risk factors in a random population of African Americans from Cleveland participating in health screenings at their church.25 Of the sample (n=144), 42% were obese, 51% had high total cholesterol (≥200), 48% had a high systolic blood pressure (≥140), 16% had a high diastolic blood pressure (≥90), and 13% had diabetes (blood glucose ≥140). Although it is difficult to make direct comparisons due to sex and age differences across studies, the prevalence of risk factors in our sample was higher for most factors, indicating that our sample may be at an even higher risk than other groups of church members. None of the studies reported the prevalence of risk factor clustering among participants.
Although the overall health of our sample was fairly poor, most participants (94%) reporting seeing a health-care provider in the past 12 months. Nearly all participants reported getting their blood pressure checked by a health professional at some point, most within the past year. Despite the healthcare visits and screenings, 25% of participants still had uncontrolled hypertension (data not shown). There are multiple possible explanations for these discrepancies. Less-than-ideal compliance with medication and medical advice has been shown in underserved, financially disadvantaged populations,26–28 with limited financial resources and distrust of healthcare professionals as potential explanations.29 Furthermore, medical care may be of a lower quality in some of these medically underserved areas.30
The high prevalence of risk factors, and more importantly the frequent clustering of risk factors among participants, substantiates the need for interventions targeting these multiple risk factors in African Americans. The church is important in the African American community, therefore one possible approach to more effectively improve health is for universities to partner with churches to develop and implement health-behavior change programs. Working together could help assure that programs are culturally and ethnically relevant, while at the same time include evidence-based intervention strategies that have been shown to successfully change behavior. A number of interventions targeting health behaviors such as diet, physical activity, and weight loss in African Americans have been implemented in faith-based settings, and results have been promising thus far.31
This study has a number of strengths including the very large sample of South Carolinian African American adults and the objective BMI and blood pressure measures. We also recognize study limitations including the self-report measures of diabetes and high cholesterol. Although we have no reason to necessarily believe that AME church members differ substantively from other African Americans in South Carolina or the southeastern United States, we acknowledge that state level differences in risk factors do exist which may limit the generalizabilty of this study.
This study describes an unpleasant reality for a sample of church members from South Carolina that includes an exceptionally high prevalence of risk factors and risk factor clustering. Culturally relevant behavior change interventions targeting risk factor reduction should be made an important public health target.
Acknowledgments
This work was supported by the National Heart, Lung, and Blood Institute [grant number R01 HL083858]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
We wish to thank The Right Reverend Preston Warren Williams II and other church leaders for their support of FAN. We thank the churches and members who have taken time out of their busy lives to participate in measurements and trainings and to implement FAN in their churches. We also wish to acknowledge key staff and students who have contributed to FAN: Alisa Brewer, Harriet Cunningham, Kara Goodrich, Deborah Kinnard, Gilbert Smalls, and Cassandra Wineglass. We thank Dr. Marci Campbell for consulting on FAN and sharing many useful lessons learned from her work. Finally, we thank the many additional students and staff members who have supported measurement and intervention activities.
Footnotes
Author Contributions
Design concept of study: Baruth, Wilcox, Laken, Warren
Acquisition of data: Baruth, Wilcox, Laken, Warren
Data analysis and interpretation: Baruth, Wilcox, Egan, Dowda, Laken, Warren
Manuscript draft: Baruth, Egan, Dowda, Laken, Warren
Statistical expertise: Wilcox, Dowda
Acquisition of funding: Wilcox
Administrative: Baruth, Laken, Warren
Supervision: Wilcox, Egan
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Rich DQ, Gaziano JM, Kurth T. Geographic patterns in overall and specific cardiovascular disease incidence in apparently healthy men in the United States. Stroke. 2007;38(8):2221–2227. doi: 10.1161/STROKEAHA.107.483719. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Changes in mortality from heart failure–United States, 1980–1995. MMWR Morb Mortal Wkly. 1998;47(30):633–637. [PubMed] [Google Scholar]
- 4.Gillum RF. Prevalence of cardiovascular and pulmonary diseases and risk factors by region and urbanization in the United States. J Natl Med Assoc. 1994;86(2):105–112. [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; [Last accessed on March 24, 2011.]. Available at: http://webappa.cdc.gov/sasweb/ncipc/leadcaus10.html. [Google Scholar]
- 6.Suh DC, Choi IS, Plauschinat C, Kwon J, Baron M. Impact of comorbid conditions and race/ethnicity on glycemic control among the US population with type 2 diabetes, 1988–1994 to 1999–2004. J Diabetes Complications. 2010;24(6):382–391. doi: 10.1016/j.jdiacomp.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Belletti DA, Zacker C, Wogen J. Effect of cardiometabolic risk factors on hypertension management: a cross-sectional study among 28 physician practices in the United States. Cardiovasc Diabetol. 2010;9:7. doi: 10.1186/1475-2840-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159(10):1104–1109. doi: 10.1001/archinte.159.10.1104. [DOI] [PubMed] [Google Scholar]
- 9.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 10.Yusuf HR, Giles WH, Croft JB, Anda RF, Casper ML. Impact of multiple risk factor profiles on determining cardiovascular disease risk. Prev Med. 1998;27(1):1–9. doi: 10.1006/pmed.1997.0268. [DOI] [PubMed] [Google Scholar]
- 11.Taylor H, Liu J, Wilson G, et al. Distinct component profiles and high risk among African Americans with metabolic syndrome: the Jackson Heart Study. Diabetes Care. 2008;31(6):1248–1253. doi: 10.2337/dc07-1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke–United States, 2003. MMWR Morb Mortal Wkly. 2005;54(5):113–117. [PubMed] [Google Scholar]
- 13.South Carolina Department of Health and Environmental Control. The Burden of Heart Disease and Stroke in South Carolina. 2006. [Google Scholar]
- 14.Wilcox S, Laken M, Parrott AW, et al. The faith, activity, and nutrition (FAN) program: design of a participatory research intervention to increase physical activity and improve dietary habits in African American churches. Contemp Clin Trials. 2010;31(4):323–335. doi: 10.1016/j.cct.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen DA, Scribner RA, Farley TA. A structural model of health behavior: a pragmatic approach to explain and influence health behaviors at the population level. Prev Med. 2000;30(2):146–154. doi: 10.1006/pmed.1999.0609. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 17.de Greeff A, Reggiori F, Shennan AH. Clinical assessment of the DINAMAP ProCare monitor in an adult population according to the British Hypertension Society Protocol. Blood Press Monit. 2007;12(1):51–55. doi: 10.1097/MBP.0b013e3280858b73. [DOI] [PubMed] [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–152. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. South Carolina Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 21.U.S. Census Bureau. State and County Quick Facts. South Carolina: 2010. [Last accessed on July 12, 2010.]. Available at: http://quickfacts.census.gov/qfd/states/45000.html. [Google Scholar]
- 22.Eberly LE, Prineas R, Cohen JD, et al. Metabolic syndrome: risk factor distribution and 18-year mortality in the multiple risk factor intervention trial. Diabetes Care. 2006;29(1):123–130. doi: 10.2337/diacare.29.1.123. [DOI] [PubMed] [Google Scholar]
- 23.Wilcox S, Laken M, Anderson T, et al. The Health-e-AME Faith-Based Physical Activity Initiative: description and baseline findings. Health Promot Pract. 2007;8(1):69–78. doi: 10.1177/1524839905278902. [DOI] [PubMed] [Google Scholar]
- 24.Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep. 2001;116 (Suppl 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gittner LS, Hassanein SE, Murphy PJ. Church-based heart health project: Health status of urban African Americans. Perm J. 2007;11(3):21–25. doi: 10.7812/tpp/06-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ndumele CD, Shaykevich S, Williams D, Hicks LS. Disparities in adherence to hypertensive care in urban ambulatory settings. J Health Care Poor Underserved. 2010;21(1):132–143. doi: 10.1353/hpu.0.0259. [DOI] [PubMed] [Google Scholar]
- 27.Bosworth HB, Powers B, Grubber JM, et al. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23(5):692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120(1):26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 29.Lewis LM, Askie P, Randleman S, Shelton-Dunston B. Medication adherence beliefs of community-dwelling hypertensive African Americans. J Cardiovasc Nurs. 2010;25(3):199–206. doi: 10.1097/JCN.0b013e3181c7ccde. [DOI] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Research and Quality. [Last accessed on July 13, 2010.];National Healthcare Disparities Report. 2008 Available at: http://www.ahrq.gov/qual/qrdr08.htm.
- 31.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]