Abstract
Objectives
Accreditation in France relies on a mandatory 4-year cycle of self-assessment and a peer review of 82 standards, among which 14 focus priority standards (FPS). Hospitals are also required to measure yearly quality indicators (QIs—5 in 2010). On advice given by the accreditation committee of HAS (Haute Autorité en Santé), based on surveyors proposals and relying mostly on compliance to standards, accreditation decisions are taken by the board of HAS. Accreditation is still perceived by hospitals as a burdensome process and a simplification would be welcomed. The hypothesis was that a more limited number of criteria might give sufficient amount of information on hospitals overall quality level, appraised today by accreditation decisions.
Design
The accuracy of predictions of accreditation decisions given by a model, Partial Least Square-2 Discriminant Analysis (PLS2-DA), using only the results of FPS and QIs was measured. Accreditation decisions (full accreditation (A), recommendations or reservation (B), remit decision or non-accreditation (C)), results of FPS and QIs were considered qualitative variables. Stability was assessed by leave one out cross validation (LOOCV).
Setting and participants
All French 489 acute care organisations (ACO) accredited between June 2010 and January 2012 were considered, 304 of them having a rehabilitation care sector (RCS).
Results
Accuracy of prediction of accreditation decisions was good (89% of ACOs and 91% of ACO-RCS well classified). Stability of results appeared satisfactory when using LOOCV (87% of ACOs and 89% of ACO-RCS well classified). Identification of worse hospitals was correct (90% of ACOs and 97% of ACO-RCS predicted C were actually C).
Conclusions
Using PLS2-DA with a limited number of criteria (QIs and FPS) provides an accurate prediction of accreditation decisions, especially for underperforming hospitals. This could support accreditation committees which give advices on accreditation decisions, and allow fast-track handling of ‘safe’ reports.
Article summary.
Article focus
Can we simplify hospitals accreditation's process?
Can we reduce accreditation's burden?
Can we use a small number of criteria to predict accreditation's results?
Key messages
A prediction model was shown 90% accurate in predicting accreditation decisions.
Detecting high-risk quality hospitals was effective (97%).
If focus priority standards (FPS) were to be assessed annually, we could have a regular estimation of the level of quality of hospitals.
Strengths and limitations of this study
Leave one out cross validation showed excellent stability of the prediction model.
The choice of the criteria (FPS and quality indicators) can be discussed.
Only acute care organisations with an eventual additional rehabilitation sector were considered.
Introduction
In many countries, hospitals’ quality is assessed through accreditation reports and quality indicators (QIs).1–3 Accreditation has been developed to improve the quality of care and patient safety.4–11 Moreover, quality indicators have been introduced in the accreditation process in order to give a quantitative assessment of hospitals’ quality. For instance, the Joint Commission has integrated accountability measures into the accreditation process1; the Australian Council on Healthcare Standards (ACHS) clinical indicator (CI) programme was established to facilitate the measurement of important aspects of health services for the members of the ACHS EQuIP accreditation programme.12
The French accreditation programme, set since 1999, nowadays in France called certification, is a government-sponsored initiative, patient centred and orientated to continuous quality improvement (CQI).13 14 Hospitals’ accreditation procedure is a mandatory 4-year cycle organised in a few steps. First, a hospital assesses itself on 82 standards defined by the National Authority for Health (‘Haute Autorité de Santé’—HAS), 14 of which being Focus Priority Standards (FPS). Hospitals evaluate their compliance to each standard with a score from 0% to 100%, which leads to four classes (A, B, C or D) from best to worst. FPS are weighted according to achieved steps in continuous improvement programmes concerning these specific standards. Five months later, surveyors conduct an external evaluation of several of the same standards during a structured visit where hospitals’ assessments are confirmed or modified. They assess all FPS, other standards where hospitals are low and a couple of standards randomly selected. A report is then submitted to the hospital, which has an opportunity to question it within a month, and then to an independent review panel—HAS accreditation committee—which then prepares an advice, according to standards quotations, on the level of accreditation.15 Unlike other countries where accreditation decisions are built entirely on computed algorithms,16 accreditation decisions are finally taken by the board of HAS and reports are made public and transmitted to regulatory agencies.
In the healthcare accreditation context, a standard is defined as “a desired and achievable level of performance against which actual performance is measured.”17 Standards are generally considered as important means by which to improve clinical practices and organisational performance. They were also reported to improve organisational and staff efficiency.18
Several countries have developed the use of FPS considered as essential or priority for accredited centres. Such essential standards are used within the national accreditation programme for breast centres in the USA.19 20 The Joint Commission has also developed a set of essential standards focused ‘on important patient, individual or resident care and organisation functions that are essential to providing safe, high quality care’.21 In the Canadian accreditation programme, nine Required Organisational Practices were integrated within the standards.22 In Australia, the EQuIP accreditation programme contains 13 essential standards that are assessed by the ACHS surveyors during the accreditation process.23 In France, among the 82 standards available in the accreditation manual, 14 FPS have been defined.15 These 2010 FPS linked to critical activities, on which HAS expects a high level of compliance. They are especially focused on the quality and safety of care in hospitals and are systematically assessed during accreditation visits.
In addition, since 2008, a mandatory collection of standardised QIs has been set in France. They have been publicly reported since 2010, and partially integrated in the accreditation decision process. In other countries, QIs have also been used in the accreditation programme. For instance, since 2012, the Joint Commission has integrated performance expectations on accountability measures into accreditation standards when it introduced the following performance improvement requirement: the hospital improves its performance on ORYX accountability measures; the hospital achieves a composite performance rate of at least 85% on the ORYX accountability measures.24 In Australia, the ACHS Clinical Indicator programme has been set to facilitate the measurement of important aspects of health services during the EQuIP accreditation programme. Indeed, performance monitoring provides evidence for use in accreditation as indicators are collected, monitored and benchmarked and as participation in the CI programme is included in all ACHS healthcare accreditation.25 Implementing QIs has been proved useful by promoting development of quality measurement, answering to the public demand for transparency and stimulating quality improvement when publicly reported.26
Even though measuring quality and safety of care in hospitals seem an essential step, the accreditation process was found bureaucratic and time consuming.7 The French procedure has already been revised in 201015 but hospitals as well as surveyors may still resent its burden. Simplification of the accreditation procedure may be useful and welcome.
Our hypothesis was that a limited number of criteria may give a sufficient amount of information on hospital performance concerning quality improvement, which could help surveyors to better organise the visits and provide decision support to HAS accreditation committee. To test this hypothesis we assessed the accuracy of a prediction model of accreditation decisions based only on the results of FPS and QIs.
Methods
Population and dataset
The study was based on a dataset of all 489 acute care hospitals accredited between June 2010 and January 2012, including 304 hospitals with an additional rehabilitation care sector (RCS).
Accreditation decisions were divided in three classes: full accreditation (A); recommendation or reservation (B) and respite of accreditation decision or non-accreditation (C).
Among the 82 standards of the 2010 accreditation procedure, 14 FPS concerned the acute care sector and 7 additional FPS were specific to the RCS. FPS were standards that the HAS considers as essential. No selection of FPS was undertaken (table 1). Each FPS was assessed by surveyors with four possible decisions: ‘Compliance’, ‘Recommendation’, ‘Reservation’ and ‘Major Reservation’. For hospitals without RCS, FPS concerning the RCS were scored ‘Not Applicable’ (NA).
Table 1.
List of FPS and QIs
| FPS | QIs |
|---|---|
| 1f—continuous professional development and organisation | PR—quality of patient record |
| 8a—quality and safety improvement programme | DSI—delay in sending information at hospital discharge |
| 8f—management of adverse events | PS—pain status evaluation |
| 8g—control of infection risk | NS—nutritional status evaluation |
| 9a—system for managing claims and complaints | PAN—quality of patient anaesthetic record |
| 12a—pain management | |
| 13a—care and rights of patients at the end of life | |
| 14a—management of the patient record | |
| 14b—patients’ access to their medical record | |
| 15a—patient identification at all stages of treatment | |
| 20a—drug management (hospital level) | |
| 20abis—drug management (patient level) | |
| 25a—management of emergencies and unscheduled care | |
| 26a—organisation of the operating room |
A detailed description of FPS (criteria and modality of assessment) can be found in: http://www.has-sante.fr/portail/jcms/r_1439924/fr/manuel-de-certification-des-etablissements-de-sante-v2010-revise-2011
Information on quality indicators may be obtained from: http://www.has-sante.fr/portail/jcms/fc_1249986/fr/indicateurs-de-qualite-et-de-securite.
FPS, focus priority standards; QI, quality indicator.
In addition, the values of all five mandatory QIs collected in each hospital in 2010 and 2011 were considered, plus four QIs specific to RCS (table 1). In France, values of QIs could not be extracted automatically, as, in 2011, only 6% of hospitals had fully computerised medical records. QIs were thus computed from a random sample of 80 medical records in each hospital.25 Hospitals were classified depending on the QI value and its normal CI into four classes: hospital's score was: (1) significantly higher (t test) than the target of 80% demanded in France (class ‘1’); (2) not significantly different from 80% (class ‘2’); (3) lower than 80% (class ‘3’); and hospital did not respond to its obligation to collect data (class ‘4’). Hospitals with less than 30 patient records were scored ‘Not Applicable’ (NA).
A dataset was obtained for each hospital, including its initial accreditation level coded into three classes; the surveyors’ decisions for the 14 FPS (21 FPS for ACO-RCS) coded into five classes; and the class level for the five mandatory QIs (9 for ACO-RCS) coded into five classes.
We conducted a univariate analysis of the variables in the dataset in order to describe the frequency of hospitals in the different classes for each FPS and QI. We also investigated the link between the accreditation classes and both FPS and QIs by running χ² tests. We then performed a multivariate analysis in order to predict initial accreditation decisions from FPS’ assessments and QIs’ classes. A statistical method was considered: Partial Least Square-2 Discriminant analysis (PLS2-DA).26–28
PLS2-DA model
PLS2-DA is an efficient statistical technique that is especially suited to deal with a large number of predictors with multicollinearity,29 which is the case in our study. Considering that the response variable (accreditation decision) is multivariate, PLS components explain all the responses simultaneously and the method is called PLS2 in contrast to the univariate PLS regression. The PLS2 model was run on the complete disjunctive table in order to produce a set of PLS2-components summarising the explanatory variables and taking into account the categorical response variable. Discriminant analysis was then run on the PLS2 components to predict an accreditation class for each hospital.30 31 For example, if a hospital has a posteriori probabilities of being respectively, A, B, C: 0.30, 0.60, 0.10 then the given hospital will be ranged in the B accreditation class.
Validation of the model
Agreement levels between predicted and actual accreditation classes were determined by Cohen-weighted κ coefficients and a percentage of well-classified hospitals.32 With the weighted form of κ, different kinds of disagreement are not equivalent (eg, a top vs bottom disagreement is worse than a top vs neutral disagreement).33
In addition, leave one out cross validation (LOOCV) was computed in order to assess the stability of the model:34 PLS2-DA was run on all hospitals but one to construct the model. The hospital left apart had its actual class compared with its predicted class. This process was repeated for each hospital. Predicted and observed responses were then compared to assess the stability of the method: external confusion matrices were developed. A Wald proportion statistical test was carried out to compare the proportion of hospitals well classified with LOOCV and without LOOCV.
Distribution of a posteriori probabilities was given for each class.
Results
Most hospitals belonged to the medium accreditation class (77%), 12% of hospitals were ranged A and 11% C.
Distribution of FPS and QIs in classes is given by table 2. Some FPS, had a high level (‘Compliance’) for almost all hospitals such as ‘Pain Management’; ‘Patient needs at the end of life’; ‘Patient access to medical record’; ‘Patient identification’; ‘Operating room’; ‘Adverse event’; ‘Infectious risk’ and ‘Claims and complaints’. For some other FPS, such as ‘Drug management—hospital level’, the distribution of hospitals across the classes was more balanced. For example, for FPS_20a, 41% of hospitals were ranged ‘Compliance’, 31% had a recommendation of improving the quality of care, 25% a reservation and 3% a major reservation.
Table 2.
Distribution of variables (focus priority standards – FPS and quality indicators-QIs) in classes and χ2 tests (p value)
| FPS | Compliance | Recommandation | Reservation | Major reservation | NA | p Value |
|---|---|---|---|---|---|---|
| 1f—evaluation of clinical practices policy | 74% | 17% | 8% | 1% | <0.0001 | |
| 8a—quality and safety improvement programme | 78% | 17% | 5% | 0.0331 | ||
| 8f—adverse events | 81% | 12% | 7% | <0.0001 | ||
| 8g—infectious risk | 95% | 4% | 1% | 0.0107 | ||
| 9a—claims and complaints | 98% | 2% | 0.0002 | |||
| 12a—pain management | 85% | 14% | 1% | <0.0001 | ||
| 12a—(RCS)-pain management | 50% | 8% | 0% | 42% | <0.0001 | |
| 13a—patient needs at the end of life | 81% | 10% | 1% | 8% | 0.0003 | |
| 13a—(RCS)-patient needs at the end of life | 45% | 6% | 0% | 49% | 0.0004 | |
| 14a—patient record | 62% | 30% | 8% | <0.0001 | ||
| 14a—(RCS)-patient record | 34% | 20% | 4% | 42% | <0.0001 | |
| 14b—patient access to medical record | 96% | 4% | 0.0007 | |||
| 14b—(RCS)-patient access to medical record | 54% | 5% | 42% | <0.0001 | ||
| 15a—patient identification | 80% | 15% | 5% | <0.0001 | ||
| 15a—(RCS)-patient identification | 45% | 9% | 4% | 42% | <0.0001 | |
| 20a—drug management (hospital level) | 41% | 31% | 25% | 3% | <0.0001 | |
| 20a—(RCS)-drug management (hospital level) | 28% | 18% | 12% | 0% | 42% | <0.0001 |
| 20abis—drug management (patient level) | 53% | 5% | 2% | 0% | 40% | 0.0449 |
| 20abis—(RCS)-drug management (patient level) | 35% | 4% | 0% | 0% | 61% | 0.1130 |
| 25a—emergency room | 53% | 6% | 2% | 0% | 39% | 0.0005 |
| 26a—operating room | 81% | 4% | 6% | 1% | 9% | <0.0001 |
| QIs | ‘1’ | ‘2’ | ‘3’ | ‘4’ | ‘NA’ | p Value |
| PR—quality of patient record | 11% | 16% | 73% | 0.0155 | ||
| PR—quality of patient record RCS | 3% | 5% | 46% | 3% | 43% | 0.0418 |
| DSI—delay in sending information at hospital discharge | 2% | 4% | 94% | 0.5492 | ||
| DSI—(RCS)-delay in sending information at hospital discharge | 14% | 15% | 26% | 3% | 43% | 0.0092 |
| PS—pain status evaluation | 29% | 12% | 58% | 0.0004 | ||
| PS—(RCS)-pain status evaluation | 13% | 4% | 38% | 3% | 43% | 0.0006 |
| NS—nutritional status evaluation | 39% | 29% | 32% | 0.0274 | ||
| NS—(RCS)-nutritional status evaluation | 8% | 11% | 36% | 3% | 43% | 0.0437 |
| PAN—quality of patient anaesthetic record | 35% | 14% | 27% | 0.0022 | ||
QI, quality indicator; RCS, rehabilitation care sector.
Concerning QIs’ distributions, a high proportion of hospitals belonged to a low class (26–94% in class ‘3’ or ‘4’) and a low percentage to the high class (2–39% in class ‘1’ or ‘2’).
Significant associations were shown between accreditation decisions and the results of each FPS and each QI (χ² tests, p values in table 2), except for the delay in sending information QI.
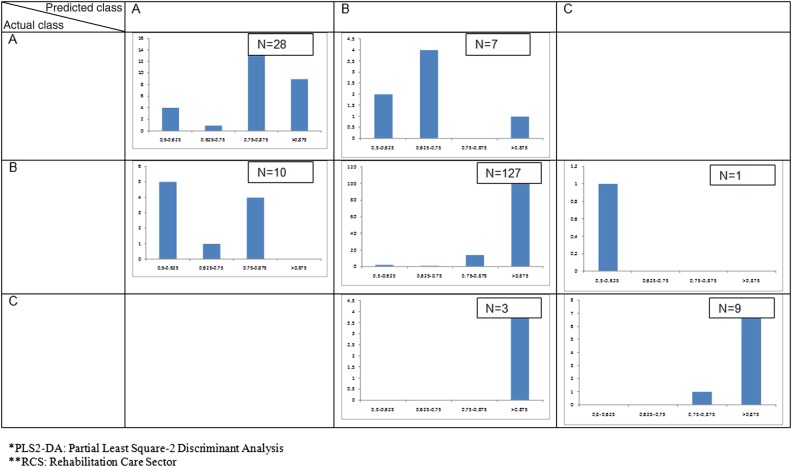
The PLS2-DA model was used to predict accreditation decisions. Contingency tables were produced: table 3 shows the concordance between actual and predicted accreditation classes, and the same results given by LOOCV, first for acute care organisations (ACO) without an RCS, second for hospitals with an RCS (ACO-RCS). Substantial agreement was observed between actual versus predicted accreditation decisions (κ=0.70 for ACOs, 0.73 for ACO-RCS). Prediction was found consistent: for ACOs, 89% of hospitals were well classified (respectively, 91% for ACO-RCS). Prediction was accurate in 80% of the 35 ACO ranged A (72% of 25 ACO-RCS). Likewise, 9 of 10 ACO (97% of 33 ACO-RCS) ranged C were actually C. In addition, on the 35 ACOs actually A, 80% were ranged A (72% of the 25 ACO-RCS). Seventy-five per cent of ACOs actually ranged C were predicted C for (80% of ACO-RCS).
Table 3.
Actual versus predicted accreditation level without and with LOOCV for (1) acute care organisations; (2) acute care organisations with a rehabilitation care sector (number of hospitals)
| ACO | 1. PLS2-DA Prediction |
ACO | 1. PLS2-DA Prediction with LOOCV |
||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | A | B | C | ||||
| Actual | A | 28 | 7 | 0 | Actual | A | 26 | 9 | 0 |
| B | 10 | 127 | 1 | B | 10 | 127 | 1 | ||
| C | 0 | 3 | 9 | C | 0 | 4 | 8 | ||
| ACO-RCS | 2. PLS2-DA Prediction | ACO-RCS | 2. PLS2-DA Prediction with LOOCV | ||||||
| A | B | C | A | B | C | ||||
| Actual | A | 18 | 7 | 0 | Actual | A | 15 | 10 | 0 |
| B | 12 | 226 | 1 | B | 13 | 224 | 2 | ||
| C | 0 | 8 | 32 | C | 0 | 8 | 32 | ||
ACO: acute care organization; LOOCV: leave one out cross-validation; PLS2-DA: Partial Least Square-2 Discriminant Analysis; RCS: rehabilitation care sector.
When computing LOOCV, we observed no difference concerning stability: the percentage of well-classified hospitals remained at 87% for ACOs; 89% for ACO-RCS. A Wald test showed no statistical difference between the proportions of well-classified hospitals with and without LOOCV (p=0.647 for ACO; p=0.65 for ACO-RCS).
For each hospital, a posteriori probabilities of belonging to each of the three accreditation classes were computed, the sum being of 1 for each hospital. Figure 1 shows a posteriori probabilities distributions for ACO-RCS (similar results were observed for ACOs). A hospital was ranged in a class according to its higher probability. We observed that hospitals predicted A and actually A had a posteriori probabilities of actually being A always close to 1, which means that we can be confident in the result given by the model. On the contrary, when a posteriori probabilities were close to 0.5, there were misclassifications (for instance for hospitals actually ranged A and predicted B). To resume, we highlighted the fact that when a posteriori probabilities were close to 1, hospitals were well classified. Nevertheless, when the model made a mistake in predicting hospitals’ class, a posteriori probabilities were close to 0.5 in most hospitals. This is true but for three ACOs and eight ACO-RCS whose actual class was C and which were given a high a posteriori probability of belonging to the class B.
Figure 1.
Distribution of a posteriori probabilities in each class, actual and predicted, computed from Partial Least Square-2 Discriminant Analysis, in hospitals without Rehabilitation Care Sector.
Discussion
In France, accreditation is a mandatory 4-year procedure, built on the same method than those used in many countries.35 36 Even though the accreditation procedure supports the quality of care, it has been criticised, particularly owing to the important workload of hospitals’ self-assessment. The self-assessment validation process by surveyors has also been considered time consuming. At last, the accreditation procedure represents an important financial expenditure considering that surveyors are made available for hospitals and compensated by HAS. Simplification and priorisation efforts are unanimously requested by stakeholders, all the more considering the obligation for French hospitals to collect regularly mandatory QIs. Moreover, they are only partly taken into account in the accreditation process. Our aim was to test if a restricted number of all essential standards and all 2010 French QIs were sufficient to assess the level of quality reached by hospitals, currently measured by its accreditation decision, and to detect underperforming hospitals.
The most important result of this study was that a model based on these few variables, using the PLS2-DA method, reproduced satisfying accreditation decisions (89% of ACOs were well classified, this number is 91% for ACO-RCS) taken by the French National Authority for Health after the surveyors’ visit validating 82 standards. Even though some hospitals were misclassified by the model, the results are stimulating. This is true especially for hospitals predicted C by the model, which actually had a C level in 97% of cases for ACO-RCS (90% for ACOs). Results were reproducible and trustworthy as LOOCV showed stability of the model: percentage of well-classified hospitals is a good tool to appraise validity of statistical models.37 LOOCV has been considered as a standard procedure for an almost unbiased assessment of the error rate of classification models.38–40 In our study, 89% of ACO-RCS (87% of ACOs) were shown well classified with this method.
A posteriori probabilities could be used to increase confidence in the model predictions: when hospitals were correctly predicted, a posteriori probabilities were always close to 1, whereas when hospitals were misclassified, a posteriori probabilities were mostly closer to 0.5. Consequently, with the PLS2-DA method, a predicted accreditation class should be given with its a posteriori probability. PLS2-DA method can be used to detect underperforming hospitals with a very small risk of error (3%). However, 11 hospitals (3 ACOs, 8 ACO-RCS) were predicted B when their actual accreditation class was C. It appeared regretful that not all worse hospitals were detected. These 11 hospitals were more deeply examined. Their QI scores and FPS decisions were close to those of the actual class B and their a posteriori probability of being classified B was high. However, in these hospitals surveyors gave a major reservation on other standards than FPS, concerning the proper use of antibiotics, safety of information system or management of endoscopy, not taken into account in the model (because non FPS).
The PLS2-DA model was chosen as there were constraints regarding the dataset: qualitative variables, multicollinearity issue and not applicable data. We can regret that these models do not take into account the ordinal characteristic of the variables (‘Compliance’ is better than ‘Major Reservation’) and thus some information could have been lost. However, the choice was made to consider all variables as qualitative in order to use models best suited to data and to avoid both the multicollinearity and the missing data issues.
The PLS2-DA method was stable as most hospitals were ranged in the actual accreditation class when using LOOCV. The method has been used in several studies to analyse genomic data. For instance, it was used to predict tumour classification from cDNA microarray gene expression data,41–43 and in the fields of bioinformatics, genomics and proteomics or chemometrics sciences.29 43–46 The technique is suited to deal with a large number of predictors with multicollinearity.29 It was reported to lead to high prediction accuracy.47 48 In our study it gave a strong answer to the multicollinearity issue and did take the accreditation variable into account when constructing PLS2 components. In addition, no selection of initial variables was needed.
There are limits to this study. First, the choice of the variables taken into account in this study can be discussed. Only FPS were kept among the 82 standards assessed by hospitals and validated by surveyors. However, all FPS were considered as they are unavoidable standards for the accreditation visit. This choice seemed relevant as FPS explore issues most relevant to safety and quality of care. A good compliance to these standards implied that the hospital had been through a complete cycle of quality improvement and achieved a sufficient level of quality. However, the list of FPS could be updated since compliance to some of them is already very high and since other standards than FPS can lead to major reservations. Considering the choice of QIs, all 2010 mandatory QIs were included in the study. QIs are only partly taken into account in the accreditation process, thus there was a slight duplication issue by considering them in the model. The number of mandatory QIs has recently increased in France; in 2014, 26 QIs will be mandatory, including, for example, appropriate care of acute myocardial infarction patients at discharge and of postpartum haemorrhage. The hospitals’ involvement in the collection of patients’ experiences will also be assessed by accreditation. The study will therefore have to be reproduced with all mandatory QIs and with an updated list of FPS at this time. Thus, the ideal set of variables is still to be found in order to detect underperforming hospitals and the model might be improved.
Second, a performance assessment based on a reduced set of variables could lead to bias. Hospitals could be tempted to manipulate data. A quality control of QIs is already organised in randomly selected patients’ files and the survey can detect improper assessment of FPS compliance. Hospitals may also concentrate their efforts on these topics, which could lead to undermine the benefits of a hospital-wide programme. However the aim of our study was not to propose a substitute to the accreditation process. The 2014 to come accreditation version will recentre hospitals towards continuous improvement activity.49 It will ask hospitals to provide, annually or every 2 years, statements on the achieved level and planned actions concerning CQI of processes, particularly of those assessed by FPS. These informations will be used to prepare more targeted, customised visits. We believe that a model based on FPS and QIs results, by highlighting poor performers, could allow fast-track handling of ‘safe’ reports, and therefore help accreditation committee, and help surveyors to prepare customised visits.
Third, only ACO with an eventual additional rehabilitation sector were considered. This study should thus be completed with all hospital sectors, including psychiatric and home care sectors.
As a conclusion, even though there are limits to this study, we succeeded in predicting accreditation decisions using only FPS and QIs. As most hospitals were ranged in the actual accreditation class with the PLS2-DA method, the prediction of accreditation decisions from a reduced set of FPS and QIs was found accurate enough to conceive a simple assessment of hospital performance concerning quality improvement. Detecting high-risk quality hospitals was effective. The results given by the model at an early phase of the visit could help surveyors in organising their on-site time more effectively and centre a valuable survey time on priority processes and systems, enhancing the value of accreditation to the hospital. This could also support the HAS accreditation committee, when proposing final accreditation decisions according to surveyors reports, by highlighting poor performers and thus allowing fast-track handling of ‘safe’ reports. Finally, if FPS were to be assessed on an annual or biannual basis, which is relevant if one assumes that a CQI programme is necessary in these priority topics, we could have a regular estimation of the level of quality of hospitals. However, it would not replace the whole visit process, which offers additional advantages.
Supplementary Material
Acknowledgments
The authors would like to thank members of the National Authority for Health (HAS) team and especially Marie-Hélène Toupin, who took part in the project.
Footnotes
Contributors: This article is based on a research on quality indicators and focus priority standards of the French accreditation procedure carried out by the French National Authority for Health (Haute Autorité de Santé—HAS). SG and PL contributed in writing the article. BR and SG did the statistical analysis. M-ALP, MLV, BL, CGa and CGr critically revised the article. PL gave final approval of the submitted version. Each of the listed authors meets each of the three authorship requirements stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. All authors (1) made substantial contributions to conception and design, acquisition of data or analysis and interpretation of data; (2) drafted the article or revisited it critically for important intellectual content and (3) approved the version to be published.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.The Joint Commission Facts about hospital accreditation Report. 2012
- 2.Accreditation Canada Canadian Health Accreditation Report. 2011
- 3.HCIS. Health Care Improvement Scotland 2012. http://www.healthcareimprovementscotland.org. [Google Scholar]
- 4.Shaw CD. External quality mechanisms for health care: summary of the ExPeRT project on visitatie, accreditation, EFQM and ISO assessment in European Union countries. External Peer Review Techniques. European Foundation for Quality Management. International Organization for Standardization. Int J Qual Health Care 2000;12:169–75 [DOI] [PubMed] [Google Scholar]
- 5.Collopy B. Clinical indicators in accreditation: an effective stimulus to improve patient care. Int J Qual Health Care 2000;12:211–16 [DOI] [PubMed] [Google Scholar]
- 6.Almoajel AM. Relationship between accreditation and quality indicators in hospital care: a review of the literature. World Appl Sci J 2012;17:598–606 [Google Scholar]
- 7.Pomey MP, Contandriopoulos AP, Francois P, et al. Accreditation: a tool for organizational change in hospitals? Int J Health Care Qual Assur Inc Leadersh Health Serv 2004;17(2–3):113–24 [DOI] [PubMed] [Google Scholar]
- 8.Duckett SJ. Changing hospitals: the role of hospital accreditation. Soc Sci Med 1983;17:1573–9 [DOI] [PubMed] [Google Scholar]
- 9.Juul AB, Gluud C, Wetterslev J, et al. The effects of a randomised multi-centre trial and international accreditation on availability and quality of clinical guidelines. Int J Health Care Qual Assur Inc Leadersh Health Serv 2005;18:321–8 [DOI] [PubMed] [Google Scholar]
- 10.Ito H, Sugawara H. Relationship between accreditation scores and the public disclosure of accreditation reports: a cross sectional study. Qual Saf Health Care 2005;14:87–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braithwaite J, Greenfield D, Westbrook J, et al. Health service accreditation as a predictor of clinical and organisational performance: a blinded, random, stratified study. Qual Saf Health Care 2010;19:14–21 [DOI] [PubMed] [Google Scholar]
- 12.The Australian Council on Healthcare Standards Australasian Clinical Indicator Report—13th Edition 2004–2011. 2012
- 13.Pomey MP, Francois P, Contandriopoulos AP, et al. Paradoxes of French accreditation. Qual Saf Health Care 2005;14:51–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giraud A. Accreditation and the quality movement in France. Qual Health Care 2001;10:111–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. French Certification manual. http://www.has-sante.fr/portail/jcms/r_1439924/fr/manuel-de-certification-des-etablissements-de-sante-v2010-revise-avril-2011.
- 16.The Council for Health Service Accreditation in Southern Africa. http://www.cohsasa.co.za/
- 17.International Society for Quality in Health Care. Glossary of Terms. 2006. http://www.isqua.org/Uploads/CONTENT/ISQua%20Glossary%20of%20Terms.pdf.
- 18.Greenfield D, Pawsey M, Hinchcliff R, et al. The standard of healthcare accreditation standards: a review of empirical research underpinning their development and impact. BMC Health Serv Res 2012;12:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moran MS, Goss D, Haffty BG, et al. Quality measures, standards, and accreditation for breast centers in the United States. Int J Radiat Oncol Biol Phys 2010;76:1–4 [DOI] [PubMed] [Google Scholar]
- 20.Winchester DP. The National Accreditation Program for Breast Centers: quality improvement through standard setting. Surg Oncol Clin N Am 2011;20:581–6 [DOI] [PubMed] [Google Scholar]
- 21.The Joint Commission Facts about Joint Commission accreditation standards. 2012
- 22.ACCREDITATION Canada. http://www.internationalaccreditation.ca/accreditation/PatientSafety.aspx. [Google Scholar]
- 23.The Australian Council on Healthcare Standards. 2009–2010. National Report on Health services—Accreditation performance.
- 24.The Joint Commission. 2012. Improving America's Hospitals—The Joint Commission's Annual Report on Quality and Safety.
- 25.The Australian Council on Healthcare Standards. http://www.achs.org.au/publications-resources/clinical-indicator-program/ [Google Scholar]
- 26.Meyer GS, Nelson EC, Pryor DB, et al. More quality measures versus measuring what matters: a call for balance and parsimony. BMJ Qual Saf 2012;21:964–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corriol C, Daucourt V, Grenier C, et al. How to limit the burden of data collection for quality indicators based on medical records? The COMPAQH experience. BMC Health Serv Res 2008;8:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tenenhaus M. La régression PLS. Théorie et Pratique. Paris: Editions Technip, 1998 [Google Scholar]
- 29.Bastien P, Esposito Vinzi V, Tenenhaus M. PLS generalised linear regression. Comput Stat Data Anal 2005;48:17–46 [Google Scholar]
- 30.Höskuldsson A. PLS regression methods. J Chemometr 1988;2:211–28 [Google Scholar]
- 31.Perez-Enciso M, Tenenhaus M. Prediction of clinical outcome with microarray data: a partial least squares discriminant analysis (PLS-DA) approach. Hum Genet 2003;112:581–92 [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213–20 [DOI] [PubMed] [Google Scholar]
- 33.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74 [PubMed] [Google Scholar]
- 34.Hastie T, Tibshirani RJ, Friedman JH. The elements of statistical learning: data mining, inference, and Prediction. New York: Springer, 2001 [Google Scholar]
- 35.Australian Council on Healthcare Standards The ACHS EQulP 4 Guide. Part 1. Accreditation, standards, guidelines. Sydney: ACHS, 2006 [Google Scholar]
- 36.Joint Commission on Accreditation of Health care Organizations 2009 Comprehensive Accreditation Manual for Hospitals (CAMH). OakbrookTerrace: The Official Handbook, 2008 [Google Scholar]
- 37.Efron B. Estimating the error rate of a prediction rule improvement on cross-validation. J Biopharm Stat 1983;78:316–30 [Google Scholar]
- 38.Kohavi R. A study of cross-validation and bootstrap for accuracy estimation and model selection. IJCAI, 2012 [Google Scholar]
- 39.Tan Y, Shi L, Tong W, et al. Multi-class tumor classification by discriminant partial least squares using microarray gene expression data and assessment of classification models. Comput Biol Chem 2004;28:235–44 [DOI] [PubMed] [Google Scholar]
- 40.Nguyen DV, Rocke DM. Tumor classification by partial least squares using microarray gene expression data. Bioinformatics 2002;18:39–50 [DOI] [PubMed] [Google Scholar]
- 41.Nguyen DV, Rocke DM. Multi-class cancer classification via partial least squares with gene expression profiles. Bioinformatics 2002;18:1216–26 [DOI] [PubMed] [Google Scholar]
- 42.Ross DT, Scherf U, Eisen MB, et al. Systematic variation in gene expression patterns in human cancer cell lines. Nat Genet 2000;24:227–35 [DOI] [PubMed] [Google Scholar]
- 43.Boulesteix AL, Strimmer K. Partial least squares: a versatile tool for the analysis of high-dimensional genomic data. Brief Bioinform 2007;8:32–44 [DOI] [PubMed] [Google Scholar]
- 44.Guinot C, Latreille J, Tenenhaus M, et al. Global classification of human facial healthy skin using PLS discriminant analysis and clustering analysis. Int J Cosmet Sci 2001;23:67–73 [DOI] [PubMed] [Google Scholar]
- 45.Matte-Tailliez O, Lepage E, Tenenhaus M, et al. Use of predictive modeling for Propionibacterium strain classification. Syst Appl Microbiol 2002;25:386–95 [DOI] [PubMed] [Google Scholar]
- 46.Huang X, Pan W, Grindle S, et al. A comparative study of discriminating human heart failure etiology using gene expression profiles. BMC Bioinform 2005;6:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Man MZ, Dyson G, Johnson K, et al. Evaluating methods for classifying expression data. J Biopharm Stat 2004;14:1065–84 [DOI] [PubMed] [Google Scholar]
- 48.Boulesteix AL. PLS dimension reduction for classification with microarray data. Stat Appl Genet Mol Biol 2004;3:33. [DOI] [PubMed] [Google Scholar]
- 49.National Authority for Health—The 2014 French Accreditation. http://www.has-sante.fr/portail/jcms/r_1495044/fr/enjeux-de-la-v2014
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.