Abstract
Background
This study examines the clinical and radiologic results of ceramic-on-ceramic total hip arthroplasties with regard to wear, osteolysis, and fracture of the ceramic after a minimum follow-up of six years.
Methods
We evaluated the results of a consecutive series of 148 primary ceramic-on-ceramic total hip arthroplasties that had been performed between May 2001 and October 2005 in 142 patients. The mean age was 57.2 years (range, 23 to 81 years). The mean follow-up period was 7.8 years (range, 6.1 to 10.1 years). Preoperative diagnosis was avascular necrosis in 77 hips (52%), degenerative arthritis in 36 hips (24.3%), femur neck fracture in 18 hips (12.2%), rheumatoid arthritis in 15 hips (10.1%), and septic hip sequelae in 2 hips (1.4%). Clinical results were evaluated with the Harris hip score, and the presence of postoperative groin or thigh pain. Radiologic analysis was done with special attention in terms of wear, periprosthetic osteolysis, and ceramic failures.
Results
The mean Harris hip score improved from 58.3 (range, 10 to 73) to 92.5 (range, 79 to 100) on the latest follow-up evaluation. At final follow-up, groin pain was found in 4 hips (2.7%), and thigh pain was found in 6 hips (4.1%). Radiologically, all femoral stems demonstrated stable fixations without loosening. Radiolucent lines were observed around the stem in 25 hips (16.9%), and around the cup in 4 hips (2.7%). Endosteal new bone formation was observed around the stem in 95 hips (64.2%) and around the cup in 88 hips (59.5%). No osteolysis was observed around the stem and cup. There were 2 hips (1.4%) of inclination changes of acetabular cup, 2 hips (1.4%) of hip dislocation, 1 hip (0.7%) of ceramic head fracture, and 1 hip (0.7%) of squeaking. The Kaplan-Meier survival rate of the prostheses was 98.1% at postoperative 7.8 years.
Conclusions
The ceramic-on-ceramic total hip arthroplasty produced excellent clinical results and implant survival rates with no detectable osteolysis on a minimum six-year follow-up study. The ceramic-on-ceramic couplings could be a reasonable option of primary total hip arthroplasty for variable indications.
Keywords: Hip, Total hip arthroplasty, Ceramic-on-ceramic
Total hip arthroplasty refers to reconstruction of the hip joint with artificial femoral head and acetabulum. However, over a long term of follow-up period, problems such as osteolysis and acetabular component loosening have been reported with shortened functional lifespan of artificial hip joint. Osteolysis is one of the most important factors for maintaining long-term durability after total hip arthroplasty.1) Many studies revealed that it is associated with production of wear debris.1-3) To reduce osteolysis on olyethylene wear debris, the ceramic-on-ceramic total hip arthroplasty was introduced as a substitute articulation.2,3) The first clinical usage of ceramic was alumina-on-ceramic articulation since the beginning of 1970s. Problems related to alumina-on-ceramic articulations are the loosening of acetabular component, osteolysis in vivo, and the possibility of ceramic fracture during activities of daily living. Unlike the first and second generation of ceramics, the current third generation ceramics have rare complications because of improved mechanical strength due to sleek and highly-densed ceramic surface created by high temperature uniform to the compression process.4,5)
In the present study, we evaluated the clinical and radiologic results of ceramic-on-ceramic total hip arthroplasties with regards to wear, osteolysis, and fracture of the ceramics after a minimum follow-up of six years.
METHODS
Study Group
Approval for the present study was obtained from the institutional review board. Nine patients were excluded from this study. Four patients had died and five were lost on follow-ups. The subject of this study is composed of 142 patients and 148 hips which were able to be followed up for minimum of 6 years. The first author (WSC) performed all of the procedures between May 2001 and October 2005. Eighty four hips belonged to males and sixty four hips were females. The mean age was 57.2 years old which ranged from 23 to 81 years. The mean follow-up period was 7.8 years ranging from at least 6.1 years to 10.1 years.
Preoperative diagnosis was avascular necrosis of femoral heads in 77 hips (52%), degenerative arthritis in 36 hips (24.3%), femur neck fractures in 18 hips (12.2%), rheumatoid arthritis in 15 hips (10.1%), and septic hip sequelae in 2 hips (1.4%).
Surgical Procedures and Postoperative Management
All the surgical procedures are performed under the general or spinal anesthesia. The anterolateral approach was used for all procedures. The acetabular component, DURALOC Option cup (DePuy, Warsaw, IN, USA), was fully hemisphere-shaped. It was composed of titanium in the edge, and the outer surface is fully coated with atypical hydroxyapatite. Regardless of the size of variable acetabular components, a 28 mm diameter articulation was used for all hips. It was made of BIOLOX forte (CeramTec, Plochingen, Germany) and a pure alumina ceramic head. The cementless femoral component, SPH C2 stem (Lima-Lto, Udine, Italy), was tapered straight, rectangular, and rough-sandblasted surface in titanium alloy (Ti6Al4V). Acetabular and femoral components were fixed by cementless press fit fixation. The size of acetabular implant was 2 mm larger in diameter than the final reamer size and additional 2 to 3 screws were used for firm fixation. All patients were encouraged quadriceps strengthening exercises from the first day after the operation. Partial weight bearing with crutches was allowed within postoperative 1 week, and full weight bearing was allowed within postoperative 3 months.
Clinical and Radiologic Evaluation
The clinical assessments consisted of Harris hip score6) measured at preoperative and at final follow-up, presence of postoperative groin or thigh pain, and functional capabilities. Harris hip scores at final follow-up above 90 were assessed as excellent, between 80 and 89 as good, between 70 and 79 as fair, and below 70 as poor.
Periodic radiographs were examined with regards to acetabular loosening, migration of component. Acetabular loosening was assessed whether the changes are greater than 3° in inclination, or of vertical and horizontal migration greater than 2 mm. According to the system of DeLee and Charnley,7) the radiolucent line, new bone formation, and osteolysis around acetabular component were also observed. Femoral stem loosening was assessed for varus and valgus greater than 3°, or subsidence greater than 2 mm. We also investigated radiolucent line, osteolysis, endosteal new bone formation around femoral stem according to the system of Gruen et al.8)
The end point for survival was defined as revisions. The 95% confidence intervals were calculated using Kaplan-Meier method. All the data was analyzed statistically using SPSS ver. 20.0 (SPSS Inc., Chicago, IL, USA) and a p < 0.05 was considered significant.
RESULTS
Clinical Results
Harris Hip Scores were compared between preoperative and final follow-ups, respectively. The mean Harris hip scores improved from preoperatives of 58.3 (range, 10 to 73) to 92.5 (range, 79 to 100) on the final follow-up (p < 0.05). Out of total 148 hips, 110 hips (74.3%) were assessed as excellent, 36 hips (24.3%) as good, and two hips (1.4%) as fair. At the final follow-up, inguinal pain was found in four hips (2.7%), and thigh pain was found in six hips (4.2%). However, all patients complained of mild pains and none was accompanied by the loosening of implant or osteolysis. Two patients (1.4%) were able to ambulate with the aid of a cane due to claudication. Three patients (2.0%) could ambulate with the aid of a walker or two crutches due to their generalized weakness.
Radiologic Results
Around acetabular component, the acetabular loosening was observed in two hips (1.4%). The radiolucent line was observed in four hips (2.7%): three hips (2.0%) in zone II and one hip (0.7%) in zone III. New bone formation was found in 88 hips (59.5%) out of total 148 hips; 64 hips (43.2%) in zone I, 60 hips (40.5%) in zone II, and 72 hips (48.6%) in zone III (Table 1). Most of new bone formation was found in two or more zones.
Table 1.
Radiologic Findings Around the Acetabular Cup
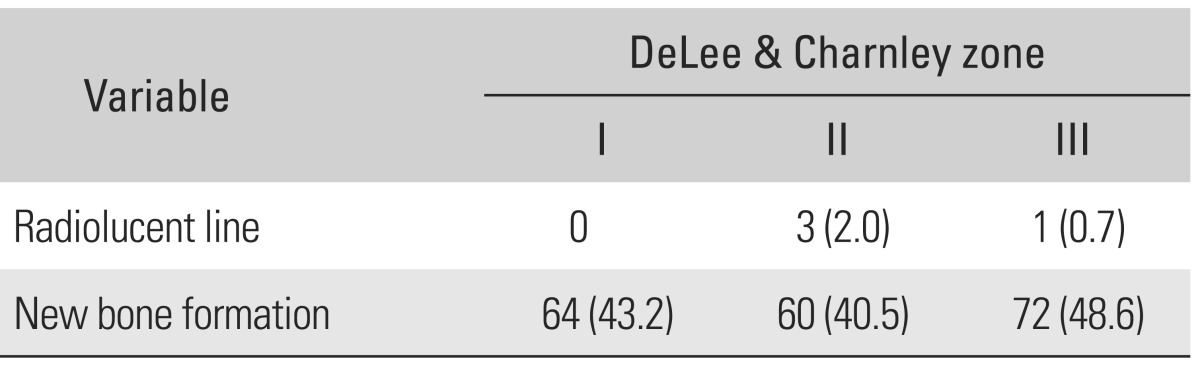
Values are presented as number (%).
Around femoral component, radiolucent line was observed in 25 hips (16.9%) out of total 148 hips: 23 hips (15.5%) in zone I, four hips (2.7%) in zone II, two hips (1.4%) in zone III, eight hips (5.4%) in zone IV, 12 hips (8.1%) in zone V, two hips (1.4%) in zone VI, and seven hips (4.7%) in zone VII. Endosteal new bone formation was found in 95 hips (64.2%): one hip (0.7%) in zone I, 68 hips (45.9%) in zone II, 44 hips (29.7%) in zone III, 10 hips (6.8%) in zone IV, 48 hips (32.4%) in zone V, 80 hips (54.1%) in zone VI, and 8 hips (5.4%) in zone VII. Cortical bone hypertrophy was found in 2 hips (1.4%), all were found in both zone VI and zone VII (Table 2).
Table 2.
Radiologic Findings Around the Femoral Stem
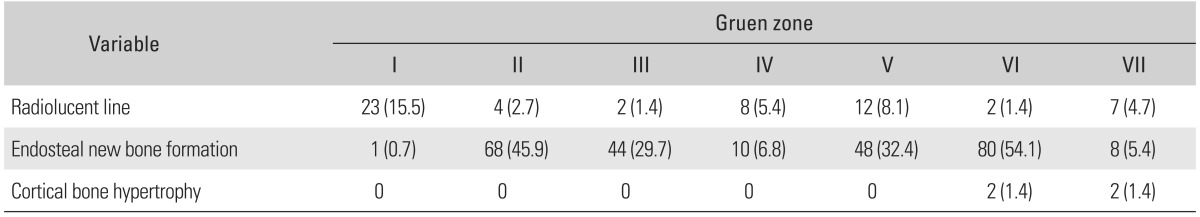
Values are presented as number (%).
In femoral component, none of the hips had alignment change until the point of final follow-up, and none of the vertical migration progressed more than 2 mm and alignment sustained its stability. Two hips showed aseptic loosening in acetabular component. Osteolysis and signs of wear were not found around implant. It was difficult to measure the exact degree of wear because it was impossible to distinguish ceramic liner and head via plain radiographic image.
Complications
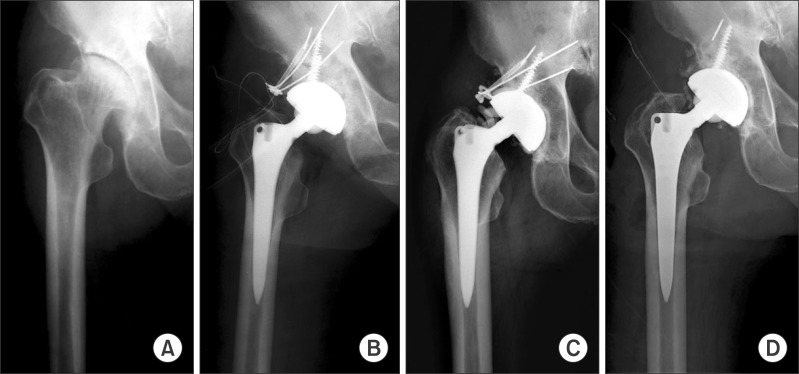
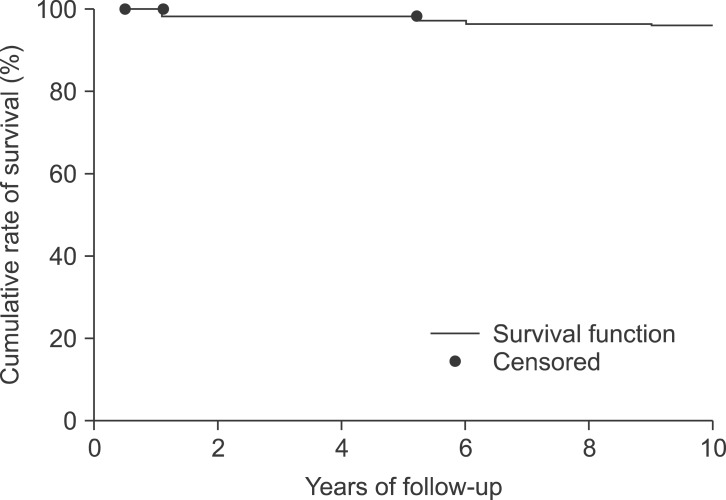
Complications occurred in six hips (4.2%): acetabular loosening in two hips (1.4%), hip dislocation in two hips (1.4%), ceramic head fracture in one hip (0.7%), and squeaking in one hip (0.7%) (Table 3). Acetabular revision was done in two hips (1.4%) which changed the angle of acetabular inclination caused by acetabular aseptic loosening. We experienced two hips of joint dislocations. One hip occurred at postoperative 1 month during attempting to cross-leg position, the other hip occurred at postoperative 72 months caused by pedestrian traffic accident with combining of tibial fracture at opposite site. Both were treated with closed reduction and abduction brace. Ceramic head fracture occurred in one hip (0.7%) with the use of short neck at postoperative 62 months. The patient was 65 years old male and when he was getting up from sitting position, he heard a breaking sound. Radiograph revealed the ceramic head fracture. Reoperation was done immediately. All broken ceramic particles were removed and the new ceramic head and liner were implanted (Fig. 1). Squeaking sound was heard in one hip (0.7%) during hip flexion at postoperative 84 months. It was asymptomatic, and thus, close observation was needed. The Kaplan-Meier survival rate of prostheses was 98.1% at postoperative 7.8 years (95% confidence interval) (Fig. 2).
Table 3.
Details of Complications
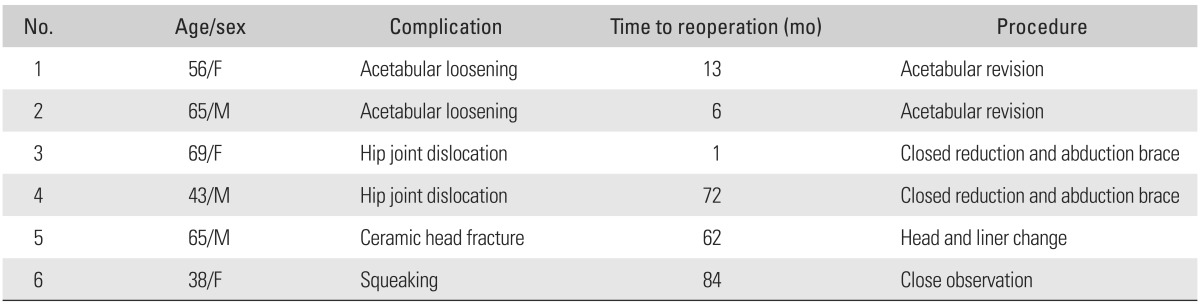
Fig. 1.
Radiographs of the right hip of a 65-year-old male showing avascular necrosis of femoral head (A) whom underwent ceramic-on-ceramic total hip arthroplasty (B). Radiograph showing ceramic head fracture at postoperative 62 months (C). Fractured ceramic head particles were removed and revision total hip arthroplasty was done (D).
Fig. 2.
The Kaplan-Meier survival rate of prostheses was 98.1% at postoperative 7.8 years (95% confidence interval).
DISCUSSION
Osteolysis is a major complication after the total hip arthroplasty, and is referred to as the major cause of aseptic hip joint loosening and failures. Polyethylene wear debris and tissue hypersensitivity due to foreign body reaction are considered to be the cause of such complications. To reduce these complications, highly cross-linked polyethylene, metal-on-metal articulation, and ceramic-on-ceramic articulation have been advocated. There had been no long term follow-up studies about highly cross-linked polyethylene, however, only several short term studies have reported that there were no differences between control groups for preventing osteolysis.9-11) Metal-on-metal articulation was used since the beginning of 1960s and it showed less wear than metal-on-polyethylene articulation. However, there was a significant increase in metal particle levels in the body, and the cytotoxicity of metal particles was a major concern which led to carcinogenic.12) Ceramic-on-ceramic articulation was introduced to supplement the weakness of previous materials. Ceramic-on-ceramic had better benefits over wear resistance, fracture strength, low friction coefficient, moisture absorption, and biocompatibility.13-15)
One of the main complications of total hip arthroplasty using ceramic-on-ceramic articulation is a fracture of ceramic head and liner. Due to the remarkable improvements of ceramic qualities after 1990s, there have been significant decreases in ceramic head fracture and the wear at articulation site. The new third generation ceramic has improved in mechanical strength, as compared with the first and second generation ceramics due to sleek and highly-densed ceramic surfaces created by high temperatures uniform with the compression process. Willmann16) reported that the development of ceramic material and its design have lessened the ceramic head fracture up to 0.004%. Hasegawa et al.17) reported a case of liner fracture at postoperative 16 months in patients who underwent ceramic-on-ceramic total hip arthroplasty using ceramic sandwich liner. Koo et al.18) reported 5 cases of ceramic head fractures out of total 367 hips using 28 mm ceramic head. Short femoral neck was used in all five hips. Koo et al.18) suggested that the thickness between short femoral neck and outer surface of ceramic head was too thin for the ceramic head fracture. In our study, one case of ceramic head fracture occurred with the use of short femoral neck.
Squeaking noises usually develop in about 0.3% to 20.9% in ceramic-on-ceramic total hip arthroplaties.19,20) It is known that squeaking is more common in hard-on-hard articulations. Chevillotte et al.21) suggested that squeaking in ceramic-on-ceramic articulation might occur via disruptions of fluid lubrication. In a lubricated joint, squeaking occurs due to metal transfers. Metal transfer as primary mode leading to fluid lubrication disruption might explain why squeaking was more common in certain designs.21) Most of squeaking in total hip arthroplasties are asymptomatic and do not need reoperation.22,23) Morlock et al.24) reported the mismatch between alumina liner and zirconium head might cause squeaking. There were several reports that mention squeaking seemed to be caused by many factors such as patient-related, implant-related, and surgery-related factors.19,25,26) Walter et al.25) reported squeaking develops more commonly among younger, taller and obese patients. Baek and Kim22) suggested that younger, more active and Asians who do squatting or crouched sitting positions were prone to squeaking. Keurentjes et al.19) reported that the shorter femur neck length might also cause squeaking. Mai et al.23) reported that patients with the short femoral neck length might have 2.2 times higher chances of squeaking and it might cause wider ranges of motion for short femoral necks. Taylor et al.26) suggested that strip wear was correlated with squeaking. Strip wear took place when there was a marginal overload in their experimental study. McCollum and Gray27) recommended that the optimal inclination and anteversion of acetabular cup might be from 20° to 40°. Walter et al.25) suggested that if the acetabular cup positioned from 15° to 35° of anteversion and from 35° to 45° in inclination, squeaking might significantly decrease. In the present study, we experienced the one case of squeaking which was 10° of anteversion and 36° of acetabular inclination via torsional computed tomography. The squeaking took place during hip flexion, and this might be caused by small degrees of anteversion which led to inadequate coverage of ceramic head during hip flexion. Therefore, it caused marginal overloading at posterior side of ceramic head.
In conclusion, ceramic-on-ceramic total hip arthroplasty produced excellent clinical results and implant survival rates, with no detectable osteolysis at a minimum of six-year follow-up study. The ceramic-on-ceramic total hip arthroplasty was a reasonable option of variable indications for primary total hip arthroplasties. Surgeons should be aware of the potential risks of ceramic fracture, squeaking, and dislocation.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Maloney WJ, Jasty M, Harris WH, Galante JO, Callaghan JJ. Endosteal erosion in association with stable uncemented femoral components. J Bone Joint Surg Am. 1990;72(7):1025–1034. [PubMed] [Google Scholar]
- 2.Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty: polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992;74(6):849–863. [PubMed] [Google Scholar]
- 3.Sedel L. Evolution of alumina-on-alumina implants: a review. Clin Orthop Relat Res. 2000;(379):48–54. doi: 10.1097/00003086-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87(3):530–535. doi: 10.2106/JBJS.D.01753. [DOI] [PubMed] [Google Scholar]
- 5.Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010;92(8):1715–1719. doi: 10.2106/JBJS.I.01019. [DOI] [PubMed] [Google Scholar]
- 6.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 7.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;(121):20–32. [PubMed] [Google Scholar]
- 8.Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;(141):17–27. [PubMed] [Google Scholar]
- 9.Olyslaegers C, Defoort K, Simon JP, Vandenberghe L. Wear in conventional and highly cross-linked polyethylene cups: a 5-year follow-up study. J Arthroplasty. 2008;23(4):489–494. doi: 10.1016/j.arth.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 10.Shia DS, Clohisy JC, Schinsky MF, Martell JM, Maloney WJ. THA with highly cross-linked polyethylene in patients 50 years or younger. Clin Orthop Relat Res. 2009;467(8):2059–2065. doi: 10.1007/s11999-008-0697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009;24(4):505–510. doi: 10.1016/j.arth.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Langkamer VG, Case CP, Collins C, et al. Tumors around implants. J Arthroplasty. 1997;12(7):812–818. doi: 10.1016/s0883-5403(97)90013-9. [DOI] [PubMed] [Google Scholar]
- 13.Bierbaum BE, Nairus J, Kuesis D, Morrison JC, Ward D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002;(405):158–163. doi: 10.1097/00003086-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Saikko VO, Paavolainen PO, Slatis P. Wear of the polyethylene acetabular cup: metallic and ceramic heads compared in a hip simulator. Acta Orthop Scand. 1993;64(4):391–402. doi: 10.3109/17453679308993653. [DOI] [PubMed] [Google Scholar]
- 15.D'Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470(2):373–381. doi: 10.1007/s11999-011-2076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willmann G. Ceramic femoral head retrieval data. Clin Orthop Relat Res. 2000;(379):22–28. doi: 10.1097/00003086-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa M, Sudo A, Hirata H, Uchida A. Ceramic acetabular liner fracture in total hip arthroplasty with a ceramic sandwich cup. J Arthroplasty. 2003;18(5):658–661. doi: 10.1016/s0883-5403(03)00193-1. [DOI] [PubMed] [Google Scholar]
- 18.Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90(2):329–336. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 19.Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466(6):1438–1443. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lusty PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Joint Surg Am. 2007;89(12):2676–2683. doi: 10.2106/JBJS.F.01466. [DOI] [PubMed] [Google Scholar]
- 21.Chevillotte C, Trousdale RT, Chen Q, Guyen O, An KN. The 2009 Frank Stinchfield Award: "Hip squeaking": a biomechanical study of ceramic-on-ceramic bearing surfaces. Clin Orthop Relat Res. 2010;468(2):345–350. doi: 10.1007/s11999-009-0911-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baek SH, Kim SY. Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Joint Surg Am. 2008;90(6):1314–1320. doi: 10.2106/JBJS.G.00755. [DOI] [PubMed] [Google Scholar]
- 23.Mai K, Verioti C, Ezzet KA, Copp SN, Walker RH, Colwell CW., Jr Incidence of 'squeaking' after ceramic-on-ceramic total hip arthroplasty. Clin Orthop Relat Res. 2010;468(2):413–417. doi: 10.1007/s11999-009-1083-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty. 2001;16(8):1071–1074. doi: 10.1054/arth.2001.27233. [DOI] [PubMed] [Google Scholar]
- 25.Walter WL, O'toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22(4):496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 26.Taylor S, Manley MT, Sutton K. The role of stripe wear in causing acoustic emissions from alumina ceramic-on-ceramic bearings. J Arthroplasty. 2007;22(7 Suppl 3):47–51. doi: 10.1016/j.arth.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 27.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990;(261):159–170. [PubMed] [Google Scholar]