Abstract
Background
Due to the anatomical nature of the radial nerve, dissection and attainment of an adequate operative field in mid to distal humerus fracture is dangerous and limited. We devised a combined anterolateral and lateral approach that ensures protection of the radial nerve. This is achieved by performing bimodal dissection of the proximal humerus anteriorly and the distal humerus laterally.
Methods
Thirty-five consecutive patients were treated using a combined anterolateral and lateral approach for a minimum follow-up period of 24 months. We analyzed time to bony union, time to return to daily work, range of motion, elbow joint function as assessed by the Mayo elbow performance index and complications.
Results
Radiologic bony union was observed at 11.2 weeks (range, 8 to 20 weeks) on average. Four cases of incomplete radial nerve palsy before surgery all recovered. Time to return to work was 10.2 weeks (range, 2 to 32 weeks) on average. The average range of motion of the elbow was 3.3° (range, 0° to 10°) of extension and 135.9° (range, 125° to 145°) of flexion. There were 21 cases of excellent and 13 cases of good or better recovery, comprising over 97.1% on the Mayo elbow performance index. There were no complications of radial nerve palsy, non-union, mal-union, or infection.
Conclusions
Our a modified combined anterolateral and lateral approach is a clinically effective surgical method of achieving protection of the radial nerve and securing easy and firm internal fixation.
Keywords: Humerus, Radial nerve, Distal shaft fracture, Surgical approach, Plate fixation
The treatment of humerus fracture employs conservative and/or surgical methods and successful results are usually obtained from both. Ward et al.1) stated that surgical treatment should be selected when it is difficult to obtain a reduction or there is intra-articular fracture, presence of nerve injury (radial nerve), accompanying ipsilateral fracture of the forearm, multiple injuries, pathologic fracture, transverse fracture in active patients, or short oblique fracture. Long term immobilization to achieve bony union and inadequate fixation also induce various complications such as non-union, mal-union, or joint stiffness. In order to avoid such complications, surgical internal fixation is preferred.2,3) Especially in the treatment of distal humerus fracture, internal fixation with a plate and screw is more preferred than any other surgical method due to secure fixation of the distal fracture fragment.
A number of surgical approaches have been introduced, and each has limitations with respect to the location of the fracture because of the neurovascular characteristics of the fracture. An anterolateral approach is used easily and safely in most proximal and middle humerus fractures, but in the distal humerus fracture, it is difficult to obtain sufficient space for fixation. This approach allows only exposure up to the proximal portion of the olecranon fossa of the humerus which means that the lateral supracondyle of the humerus can not be exposed for the fixation.
In order to expose the lateral supracondyle of the humerus and achieve sufficient fixation space, we have to choose either the lateral or posterior approach. However, these approaches also increase the risk of nerve irritation and injury because exploration of the radial nerve is inevitable during proximal fragment fixation and the inserted plate is always in contact with the radial nerve, a situation that can lead to nerve injury, irritation, and adhesion. Shao et al. reported that the incidence of radial nerve palsy that accompanies humerus fracture is 11.8%, and 12.4% of these injuries are secondary nerve injuries.4) And the incidence of iatrogenic radial nerve injury during plate fixation has been reported to be from 5.1%5) to 17.6%.6) This makes the selection of an approach difficult, and even if a selection is made, nerve exploration is unavoidable when obtaining sufficient fixation space.7-9)
The authors suggest a modified combined anterolateral and lateral approach for the surgical treatment of distal humerus fracture, and this study evaluates the safety, clinical effectiveness and clinical outcome of this approach.
METHODS
Patients
Thirty-five consecutive patients who received surgery for distal humerus fracture were prospectively selected from March 2000 to March 2010. In this study we included patients who had main extra-articular fractures on the distal third of the humerus and who were also examined for more than 24 months. However, we excluded patients who needed other kinds of approaches in order to fix their fractures (for example, patients with extra-articular fractures combined with intra-articular fracture that were fixed with olecranon osteotomy and complicated extra-articular fractures that were fixed with additional medial approaches) and also excluded patients who needed additional techniques, such as external fixations, due to severe open fractures or combined injuries.
Twenty-six males and nine females were included, and their mean age was 37.7 years (range, 14 to 70 years). The average follow-up period was 28.1 months (range, 24 to 50 months). The cause of fracture included 12 traffic accidents, 5 cases of falling down or slipping down, 5 cases of occupational accidents, and 13 cases that occurred during physical exercise. Four cases involved open fracture and seven involved radial nerve palsy. One case of brachial plexus palsy was observed.
Surgical Technique
The patient was positioned in the supine manner. The size of the incision was determined after drawing a line between the lateral epicondyle of the humerus distally and the coracoid process of the scapula proximally. Dissection of fascia and muscle following skin incision was applied in two parts. Proximal to 10 cm from the lateral epicondyle is the point where the radial nerve passes from the posterior to the anterior compartment. For this reason, if the proximal aspect is dissected with an anterolateral approach, the radial nerve is located laterally and posteriorly to the operative field. If the distal aspect is dissected with the lateral approach, the radial nerve is positioned medially and anteriorly to the operative field (Fig. 1).10)
Fig. 1.
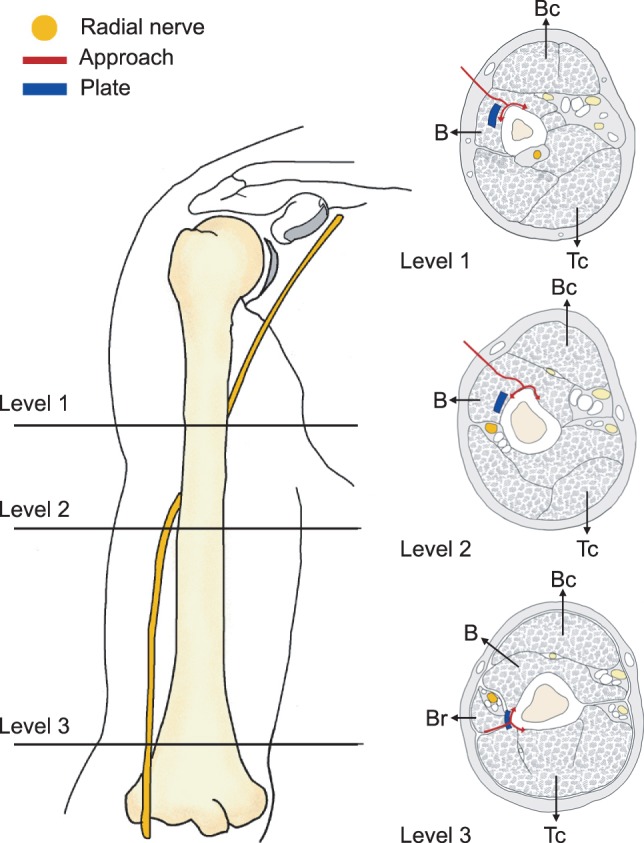
Cross-sectional anatomy of the distal humeral shaft. Cross-sectional level of the distal humeral shaft and anatomic course of radial nerve. Anterolateral approach regarding the proximal humerus (level 1 and 2): surgical dissection is made through the middle portion of the brachialis muscle. Lateral approach regarding the distal humeral shaft (level 3): surgical dissection is made between the triceps muscle and the lateral intermuscular septum. Note the radial nerve between the brachialis and brachioradialis muscles. Bc: biceps muscle, B: brachialis muscle, Tc: triceps muscle, Br: brachioradialis muscle.
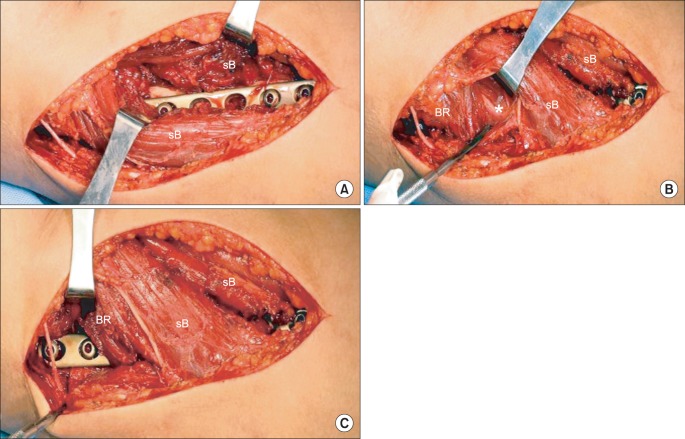
We designated a reference point which was 10 centimeters proximal to the lateral epicondyle of the humerus (Fig. 2).11-13) The proximal region with respect to the reference point was approached by the anterolateral method. After confirming the brachialis muscle was under the biceps muscle, dissection was further advanced through the middle portion of the brachialis muscle (Fig. 3A). If dissection is made through the middle portion of the brachialis muscle, the radial nerve is naturally protected (Fig. 3B); thus, one can approach the fracture site without having to worry about radial nerve injury. Most fracture reductions and manipulations can be performed through a wide operative field using the anterolateral approach. However, for sufficient fixation space, the lateral supracondyle of the humerus should be exposed through an extra incision.
Fig. 2.

Skin incision marking between the coracoid process and lateral epicondyle of the humerus.
Fig. 3.
Intraoperative photograph of distal humerus fracture. Surgical incision in the combined anterolateral and lateral approach that is marked between the lateral epicondyle of the humerus distally and the coracoid process of the scapula proximally. (A) The plate is inserted through the submuscular extraperiosteal tunnel (brachioradialis, radial nerve, and lateral portion of the split brachialis). Fracture reduction is maintained by the plate and screw. (B) The radial nerve is shown between the split brachialis muscle and brachioradialis muscle. (C) Distal location of the plate shows sufficient space for screw fixation in the distal short remnant. BR: brachioradialis muscle, sB: split brachialis muscle, asterisk: radial nerve.
For this reason, the distal region with respect to the reference point was approached by the lateral method. Fascia was longitudinally dissected posteriorly to the lateral intermuscular septum. The triceps was placed posteriorly from the operative field, and the lateral intermuscular septum and brachioradialis were located anteriorly ensuring sufficient exposure of the lateral epicondyle of the humerus (Fig. 3C). Dissection towards the proximal aspect must not exceed 10 cm from the superior to lateral epicondyle, and one is advised to work only in the safe zone where the radial nerve can be automatically protected.
The separate and exposed distal and proximal areas should be reconnected in the form of a submuscular extraperiosteal tunnel, and the roof becomes the brachioradialis and the lateral portion of the split brachialis. Further, the radial nerve is located between the brachioradialis and the lateral portion of the split brachialis, and is protected naturally by them (Fig. 3B).
For the fixation of the plate in order to maintain final reduction, the plate should be bent appropriately by anterior-posterior bending and twisting to fit the contour of the lateral curve of the humerus. The insertion of the plate should be carried out from the inferior aspect of the tunnel through a distal dissection; the plate should be fixed in the proximal dissection area (Fig. 4). This ensures sufficient space for the fixing of more than four screws in the distal short remnant.
Fig. 4.
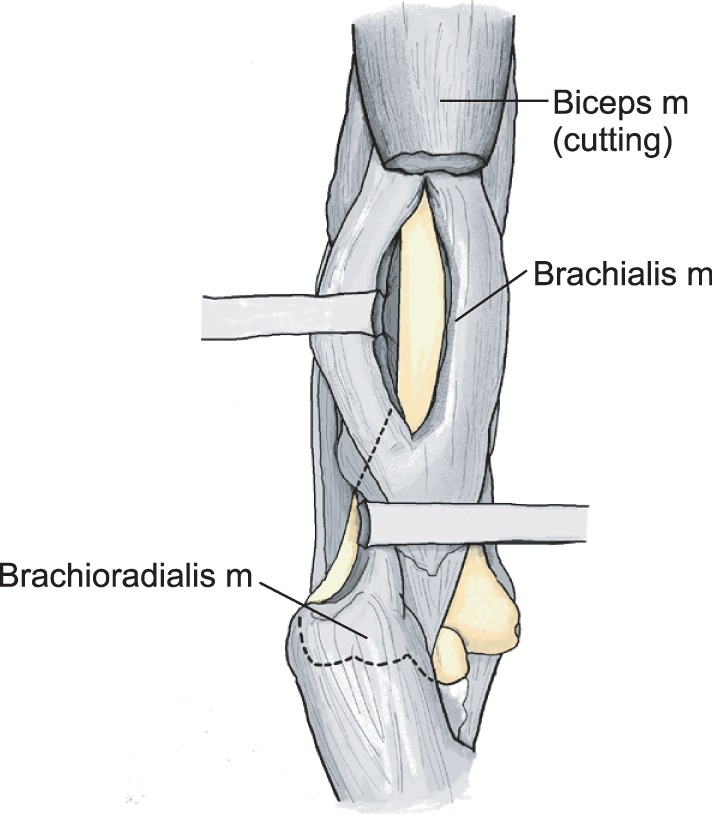
Exposure of the distal humeral shaft in the combined approach. The proximal part is approached through the middle portion of the brachialis muscle (m). The distal part is approached posteriorly to the lateral intermuscular septum. The distal humeral shaft and lateral epicondyle are exposed. The plate is inserted from the distal dissection area to the proximal dissection area though the submuscular extraperiosteal tunnel.
When exploration of the radial nerve is necessary, an approach medial to the brachioradialis muscle and lateral to the brachialis muscle facilitates the search for the radial nerve. All patients achieved accurate reduction and firm fixation through the combined approach (Fig. 5).
Fig. 5.
A 33-year-old man sustained a fracture in an accident. (A) The initial radiograph shows multifragmentary fracture of the distal humerus. (B) The radiograph after operation shows anatomical reduction and alignment by open reduction and internal fixation with a plate and circlage wires. (C) The radiograph shows bony union of the distal humerus.
A Velpeau sling was applied postoperatively, and joint exercise with gravity was allowed one or two days postoperatively. A functional brace without angular limitation was applied one week postoperatively for active and passive exercise of the shoulder and elbow joint.
Postoperative Evaluation
The results were analyzed by assessing bone union in plain radiographs to evaluate the true anteriorposterior and lateral view of the humerus, and clinical analysis was carried out using the Mayo elbow performance index (MEPI).14) The analysis of the radiographs was done immediately after surgery, two weeks postoperatively, and every month thereafter to assess bone union. Clinical analysis was undertaken six months postoperatively when bone union was complete. The MEPI evaluates the pain, range of motion, stability, and elbow joint function. It deems 100 as the maximum score, 90-100 as excellent, 75-89 as good, 60-74 as fair, and below 60 as poor. The analysis also spanned the back-to-work period and complications regarding the initial radial nerve injury, postoperative radial nerve injury, and infection.
RESULTS
We analyzed a total of 35 patients who had humeral distal fracture and were treated with the modified combined anterolateral and lateral approach. They were followed up for a minimum of two years. The average time to bone union was 11.2 weeks (range, 8 to 20 weeks). On average, patients took 10.2 weeks (range, 2 to 32 weeks) to return to work; male patients with advanced work loading took 11 weeks (range, 2 to 32 weeks), while the female group took 8.7 weeks (range, 4 to 12 weeks). The average range of motion of the elbow joint was 132.6° (range, 3.3° to 135.9°). The MEPI revealed 21 cases of excellent performance and 13 cases of good performance; the average functional score was 92.86. New development of radial nerve injury was not observed. Four cases with radial nerve palsy that existed preoperatively completely recovered 31 weeks postoperatively on average. There was no operative wound infection. and no case of complication such as displacement, non-union, or mal-union. Forty percent of the cases (14/35) exhibited mild and intermittent elbow pain, and there was no case of elbow instability or discomfort with normal activity.
DISCUSSION
There is a high risk of iatrogenic radial nerve injury during plate fixation in the treatment of distal humerus fracture5,6,15) and nonunion usually develops due to inadequate space. This may raise serious concerns even for well-trained specialists. Thus, the surgical outcome may depend on attainment of protection of the radial nerve and the securing of adequate space for firm fixation. The authors investigated the need for a modified surgical approach.
Commonly used humerus approaches are anterolateral, posterior, posterolateral, and lateral approaches.3,9,16-19) Each has its own limitations due to the location of the fracture, patient's position, and possibility of radial nerve damage. The anterolateral approach is widely used for proximal and mid-shaft humerus fracture as it is safe, without the need for dissection of the radial nerve. But when the fracture is located distally, there is a high risk of traction radial nerve injury because the nerve is forcefully pushed laterally for reduction and internal fixation. Regarding distal humerus fracture, posterior or posterolateral approaches are mostly used because these methods do not require radial nerve traction.7,17,20) These approaches can easily expose the posterior aspect of the distal humerus; therefore, acute anatomical reduction is possible, and it is easy to apply the internal device. But as the triceps is divided longitudinally with dissection, complications such as bleeding, triceps muscle weakness, and limitation of elbow motion may occur. As well, when proximal dissection is needed, exploration of the radial nerve is difficult due to its anatomical course: it runs through the triceps and is tethered to the triceps and radial groove of the humerus.7,17) Further access to the proximal humeral neck is completely blocked because of the axillary nerve and the posterior humeral circumflex artery. Also, because patients should be maintained in a lateral or prone position, this approach has limitations in patients with multiple injuries and unstable spine damage.
Recently, lateral approaches have been widely used and it has many advantages such as easy examination of the radial nerve, practicability of the operation in the supine position, and wide range of accessibility. One of its disadvantages is that radial nerve exploration is always required in accessing the proximal humerus. As a result of nerve exploration, the radial nerve is placed directly above the internal device and this can lead to formation of undesired fibrosis around the internal device and nerve.21)
To overcome the drawbacks of the above approaches, we thought of alternative ways that allow access with just one skin dissection over the entire humerus, do not require dissection of the radial nerve, offer enough fixation space without excessive traction to prevent nerve damage, and allow expansion to proximal or distal aspects to treat accompanying injuries. We designed a combined anterolateral and lateral approach. Through this method, broad access to the proximal aspect of the humerus is easily achieved, as it is in the anterolateral approach. Likewise, the risk of radial nerve injury during the approach towards the distal humerus portion, which is a disadvantage of the anterolateral approach, is prevented by using the lateral approach. The radial nerve is protected in its course between the brachialis and brachioradialis.
Specialists tend to agree that the safest technique for the protection of the radial nerve is to explore the nerve initially and practise caution during the operation. When our technique is performed extraperiosteally and is free of muscle tension, it provides a similar level of safety even without direct radial nerve dissection. If there is a need for nerve exploration, it can be done easily without an additional incision. Finally, the plate is positioned slightly anterior and inferior to the radial nerve without direct contact. Thus fibrosis around the nerve is avoided, and a safe operation is possible as the metal plate and radial nerve are separated from each other by a certain distance.
Non-union of a distal humerus fracture may occur from fixation failure. To prevent this, it is necessary to secure adequate fixation. Our method lets operators secure enough space up to the lateral supracondylar ridge of the humerus with respect to the olecranon fossa and allows the use of a metal plate with sufficient length and four or more screw fixations. One of the disadvantages of metal plate insertion is that the metal plate can be placed unnaturally because it has to be placed in a very narrow area in the lateral humerus, and so the shape may not fit along the lateral supracondyle of the humerus. There have been a few cases of patients complaining of discomfort due to the metal plate's extrusion from the lateral epicondyle. Therefore, if a metal plate can be placed in such a way that it anatomically fits with the lateral epicondyle of the humerus, it will be more useful and yield much more stable internal fixation (Fig. 6).
Fig. 6.

Precontoured anatomical plate for the distal humeral shaft.
Minimally invasive plate osteosynthesis is another option for treating humerus fracture. This technique offers a theoretical decrease in soft tissue dissection but cannot avoid the occurrence of iatrogenic radial nerve palsies and inadequate fixation. Pospula and Abu Noor22) reported two cases with perioperative complications. From this clinical study, we consider that our approach can be usefully applied when the plate is inserted from the distal lateral cortex toward the proximal anterior cortex of the humerus through a submuscular extraperiosteal tunnel. We presume that use of the newly designed plate (Fig. 6) will avoid the problems of radial nerve injury and inadequate fixation space.
A modified combined anterolateral and lateral approach for the treatment of distal humeral fracture and non-union ensures an easy approach to the entire humerus, a lowered risk of radial nerve injury and the performance of complication-free revision surgery during the distal humerus approach and harmless revision surgery during the distal humerus approach. This approach also provides adequate fixation space and therefore makes delicate fixation of the plate easy.
ACKNOWLEDGEMENTS
We thank Inha University research for allowing us to submit our manuscript to Clinics in Orthopedic Surgery for publication and considering a grant upon acceptance. We also thank Sang Hyun Shin, MD, for providing medical advice for the work.
This research was funded by an Inha University grant.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ward EF, Savoie FH, Hughes JL. Fractures of the diaphyseal humerus. In: Browner BD, Jupiter JB, Levine AM, editors. Skeletal trauma: fractures, dislocations, ligamentous injuries. Philadelphia: Saunders; 1992. pp. 1177–1200. [Google Scholar]
- 2.Heim D, Herkert F, Hess P, Regazzoni P. Surgical treatment of humeral shaft fractures: the Basel experience. J Trauma. 1993;35(2):226–232. [PubMed] [Google Scholar]
- 3.Henry AK. Extensile exposure applied to limb surgery. Edinburgh: Churchill Livingstone; 1945. [Google Scholar]
- 4.Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87(12):1647–1652. doi: 10.1302/0301-620X.87B12.16132. [DOI] [PubMed] [Google Scholar]
- 5.Paris H, Tropiano P, Clouet D'orval B, Chaudet H, Poitout DG. Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(4):346–359. [PubMed] [Google Scholar]
- 6.Lim KE, Yap CK, Ong SC, Aminuddin Plate osteosynthesis of the humerus shaft fracture and its association with radial nerve injury: a retrospective study in Melaka General Hospital. Med J Malaysia. 2001;56(Suppl C):8–12. [PubMed] [Google Scholar]
- 7.Dabezies EJ, Banta CJ, 2nd, Murphy CP, d'Ambrosia RD. Plate fixation of the humeral shaft for acute fracture, with and without radial nerve injuries. J Orthop Trauma. 1992;6(1):10–13. [PubMed] [Google Scholar]
- 8.Holsetin A, Lewis GM. Fractures of the humerus with radial-nerve paralysis. J Bone Joint Surg Am. 1963;45(7):1382–1388. [PubMed] [Google Scholar]
- 9.Hoppenfeld S, deBoer P. Surgical exposures in orthopedics: the anatomic approach. Philadelphia: JB Lippincott; 1984. [Google Scholar]
- 10.Kwon DG, Moon KH, Na SI, Shin BK, Lee TJ. Combined anterolateral and lateral approaches in treatment of extra-articular fracture of the distal humerus. J Korean Fract Soc. 2012;25(3):185–190. [Google Scholar]
- 11.Artico M, Telera S, Tiengo C, et al. Surgical anatomy of the radial nerve at the elbow. Surg Radiol Anat. 2009;31(2):101–106. doi: 10.1007/s00276-008-0412-8. [DOI] [PubMed] [Google Scholar]
- 12.Fleming P, Lenehan B, Sankar R, Folan-Curran J, Curtin W. One-third, two-thirds: relationship of the radial nerve to the lateral intermuscular septum in the arm. Clin Anat. 2004;17(1):26–29. doi: 10.1002/ca.10181. [DOI] [PubMed] [Google Scholar]
- 13.Bodner G, Buchberger W, Schocke M, et al. Radial nerve palsy associated with humeral shaft fracture: evaluation with US--initial experience. Radiology. 2001;219(3):811–816. doi: 10.1148/radiology.219.3.r01jn09811. [DOI] [PubMed] [Google Scholar]
- 14.Morrey BF, An KN. Functional evaluation of the elbow. In: Morrey BF, editor. The elbow and its disorders. 4th ed. Philadelphia: WB Saunders; 2009. pp. 80–91. [Google Scholar]
- 15.McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: a prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336–339. doi: 10.1302/0301-620x.82b3.9675. [DOI] [PubMed] [Google Scholar]
- 16.Cooney WP. Humeral fractures: operative treatment, complication, and reconstruction surgery. In: Evarts CM, editor. Surgery of the musculoskeletal system. 2nd ed. New York: Churchill Livingstone; 1990. pp. 1600–1633. [Google Scholar]
- 17.Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996;78(11):1690–1695. doi: 10.2106/00004623-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Jupiter JB. Complex non-union of the humeral diaphysis: treatment with a medial approach, an anterior plate, and a vascularized fibular graft. J Bone Joint Surg Am. 1990;72(5):701–707. [PubMed] [Google Scholar]
- 19.Thompson JE. Anatomical methods of approach in operations on the long bones of extremities. Ann Surg. 1918;68(3):309–329. doi: 10.1097/00000658-191809000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swanson TV, Gustilo RB, Kyle RF, Templeman DC. Fracture of the humeral shaft. In: Gustilo RB, Kyle RF, Templeman DC, editors. Fractures and dislocations. 4th ed. St. Louis: Mosby; 1993. pp. 365–386. [Google Scholar]
- 21.Mills WJ, Hanel DP, Smith DG. Lateral approach to the humeral shaft: an alternative approach for fracture treatment. J Orthop Trauma. 1996;10(2):81–86. doi: 10.1097/00005131-199602000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Pospula W, Abu Noor T. Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital, Kuwait. Med Princ Pract. 2006;15(6):423–426. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]