Abstract
Background
Disturbed folate metabolism is associated with an increased risk of some cancers. Our objective was to determine whether blood levels of folate, vitamin B12 and related metabolites were associated with prostate cancer risk.
Methods
Matched case-control study nested within the UK population-based ProtecT study of PSA-detected prostate cancer in men aged 50–69 years. Plasma concentrations of folate, B12 (cobalamin), holo-haptocorrin, holo- and total-transcobalamin, and total homocysteine (tHcy) were measured in 1,461 cases and 1,507 controls. ProtecT study estimates for associations of folate, B12, and tHcy with prostate cancer risk were included in a meta-analysis, based on a systematic review.
Results
In the ProtecT study, increased B12 and holo-haptocorrin concentrations showed positive associations with prostate cancer risk (highest vs lowest quartile of B12 odds ratio (OR)=1.17 (95% CI 0.95–1.43), P-for-trend=0.06; highest vs lowest quartile of holo-haptocorrin OR=1.27 (1.04–1.56), P-for-trend=0.01); folate, holo-transcobalamin and tHcy were not associated with prostate cancer risk. In the meta-analysis, circulating B12 levels were associated with an increased prostate cancer risk (pooled OR=1.10 (1.01–1.19) per 100 pmol/L increase in B12, P=0.002); the pooled OR for the association of folate with prostate cancer was positive (OR=1.11 (0.96–1.28) per 10 nmol/L, P=0.2) and conventionally statistically significant if ProtecT (the only case-control study) was excluded (OR=1.18 (1.00–1.40) per 10 nmol/L, P=0.02).
Conclusion
Vitamin B12 and (in cohort studies) folate were associated with increased prostate cancer risk.
Impact
Given current controversies over mandatory fortification, further research is needed to determine whether these are causal associations.
Keywords: folate, vitamin B12, cobalamin, transcobalamin, haptocorrin, homocysteine, folate-mediated one-carbon metabolism, prostate cancer
Introduction
The folate-mediated one-carbon metabolic pathway is fundamental to DNA synthesis, repair and methylation (1). The role of folate antagonists in treating haematological (2) and trophoblastic (3) malignancies is well-known, and genetic studies have suggested that folate-pathway gene polymorphisms may be associated with colorectal and gastric cancers (4). Several epigenetic mechanisms related to folate metabolism, including CpG island and histone methylation, DNA uracil mis-incorporation, and chromosomal re-arrangements, have been observed in prostate tumour cells (5, 6).
Studies of dietary intake and blood levels of folate, vitamin B6, methionine, and homocysteine have generally found no associations with risk of prostate cancer (7–17), although there is some evidence that high dietary intake and blood levels of vitamin B12 are associated with increased risk (12–15). One recent study reported a positive association between folic acid supplementation and prostate cancer risk (18). However, results from the same study suggested inverse associations with baseline dietary and plasma folate, as did three other studies (8, 19, 20), and the main trial finding was not replicated in a larger trial (21). Although differences in study design may partly explain these contradictory findings (22), any role of folate metabolism is likely to be complex, possibly involving a dual effect in which low folate concentrations are associated with increased risk of cancer initiation, while high concentrations, or folic acid supplementation, are associated with more rapid progression following disease onset (23). Answers to these research questions are urgently needed to inform the debate over mandatory fortification of food with folic acid and vitamin B12.
We used data from a cross-sectional case-control study nested within the UK population-based Prostate testing for cancer and Treatment (ProtecT) study to investigate whether plasma concentrations of folate, vitamin B12, and total homocysteine (tHcy) were associated with risk of localized and/or advanced prostate cancer detected by means of prostate-specific antigen (PSA) testing. We included our results in a meta-analysis of data from studies identified by systematic review of the literature.
In the ProtecT case-control study, we also measured concentrations of total- and holo-transcobalamin, and calculated the concentration of holo-haptocorrin. Haptocorrin and transcobalamin are B12 transport proteins to which total circulating B12 is bound, as holo-haptocorrin and holo-transcobalamin, in an approximate 80:20 ratio (24). Holo-transcobalamin is an alternative marker of impaired B12 absorption (25), and decreased levels have been associated more strongly than total B12 with conditions related to impaired folate and B12 metabolism (26, 27). Raised levels of holo-haptocorrin have been reported in some cancers (28, 29), possibly as a result of up-regulated haptocorrin production by tumour cells (30).
Methods
Study population
The ProtecT study is a randomized controlled trial of treatments for localized prostate cancer. Between 2001 and 2009, all (approximately 227,300) men aged 50–69 years in 300 general practices located around nine UK cities (centres) were invited to have a PSA test at a prostate check clinic appointment. Participants with a PSA level between 3.0 and 19.9 ng/mL (approximately 10% of men tested) were invited to attend the centre’s urology department for digital rectal examination and 10-core trans-rectal ultrasound-guided biopsy. Men with a PSA level ≥ 20 ng/mL were referred as a matter of urgency to a urologist, and were eligible to participate in the treatment trial only if localized cancer was confirmed. A diagnosis of localized prostate cancer was defined as a positive biopsy, clinical stage T1–T2, NX, M0; advanced prostate cancer was defined as positive biopsy, clinical stage T3–T4 or N1 or M1. All men provided written informed consent. Trent Multicentre Research Ethics Committee approved the ProtecT study and allied prostate cancer research under the auspices of ProMPT (Prostate Mechanisms of Prostate cancer and Treatment).
Selection of cases and controls
The study size (1,500 cases and 1,500 controls) was determined a priori to detect an effect estimate (odds ratios) of 1.26 (exposure odds in cases = 0.42) comparing the highest vs lowest three quartiles of vitamin and metabolite concentration at 5% significance, 80% power. Cases were selected at random from among all men diagnosed (by July 2008) with localized or advanced cancer who had consented to a blood sample for research. Eligible controls were men who had a PSA level < 3 ng/mL, or who had a PSA level ≥ 3 ng/mL and a negative biopsy result, and who had consented to provide a research blood sample. Controls were stratum-matched to cases by five-year age group and by the primary care practice from which they were recruited, thereby matching for calendar time as prostate check clinics were completed sequentially. For the assays investigated in the current analysis, one control per case was selected at random from the pool of eligible controls in each stratum.
Blood sample handling
A standardized blood collection and storage protocol was in place across all collecting centres. Blood was drawn from non-fasting participants at the time of their initial PSA test. Plasma samples were collected using the BD Vacutainer® PPT™ 8.5 mL polymer gel and spray-dried K2EDTA separator tube (Becton, Dickinson & Co, Oxfordshire, UK; catalogue number 362799), centrifuged at 2,200 relative centrifugal force within 10 minutes of blood draw and transported upright at 4 °C to the local processing laboratory. The plasma was transferred to intermediate cryo-vials for medium-term storage and frozen at −80 °C within 36 hours of draw. Samples were transferred to the central bio-repository hub on dry ice. Plasma samples were thawed at 4 °C in a shaking water bath, mixed thoroughly using the Stuart SB3 Blood Rotator Mixer (Bibby Scientific Ltd, Staffordshire, UK) for 10 minutes, centrifuged for 10 minutes at 4 °C at 4,500 revolutions per minute in the Beckman 25R Allegra centrifuge (Beckman Coulter Ltd, Buckinghamshire, UK), and aliquotted into Starlab 1.5 mL cryo-tubes (STARLAB Ltd, Buckinghamshire, UK). The plasma was then stored at −80 °C and transferred on dry ice to the Department of Physiology, Anatomy and Genetics, University of Oxford for assay.
Biochemical analyses
Plasma concentrations of folate, B12, holo- and total-transcobalamin were measured by automated (Perkin Elmer MultiProbe 11 liquid handling system, Perkin Elmer Life and Analytical Sciences (LAS), Buckinghamshire, UK) microbiological assay using Lactobacillus casei for folate (31) and Lactobacillus leichmannii for B12 (32), holo- and total-transcobalamin (33). Plasma tHcy was measured by automated (Abbott IMx system, Abbott Laboratories, Chicago, IL, USA) fluorescence polarization immunoassay (34). Between-batch coefficients of variation were, respectively: folate 7.4%; B12 7.1%; holo-and total-transcobalamin 8.2%; holo-haptocorrin 10%; tHcy 3.3%. Each batch contained an approximate 1:1 mix of case and control samples and laboratory staff were blind to case-control status. Assays that gave out-of-range results were repeated with diluted (if too high) or larger (if too low) samples. Full results were obtained for all bar one sample (insufficient volume for tHcy assay). Folate was measured as <2 nmol/L in 4 participants and holo-transcobalamin as <9 pmol/L in 13 participants; values of 1.8 nmol/L and 8 pmol/L, respectively, were substituted for these results. Holo-haptocorrin concentration was calculated by subtracting holo-transcobalamin concentration from B12 concentration, hence does not include cobalamin analogues.
Other Covariates
Self-reported data on ethnicity, smoking, alcohol, medications and dietary supplements, family history of prostate cancer (father and brother), height and weight were collected from Diet, Health and Lifestyle (DHL) questionnaires which are completed before receipt of the initial PSA test result. Self-reported height was used to calculate body mass index (BMI, kg/m2), along with nurse-measured weight where available (92.5% of cases and 92.8% of controls) and self-reported weight otherwise.
Systematic review and data extraction
Eligible studies of the association of prostate cancer risk with serum or plasma folate, B12 or tHcy levels were identified by searching the Medline and Embase online databases using text search terms for “folate/folic”, “B12/cobalamin”, and “tHcy”; each in conjunction with the MeSH term “prostatic neoplasm” and text terms “prostate cancer” and “prostatic carcinoma”. No language or publication date restrictions were imposed. All databases were last searched on 26/09/2009. References of retrieved articles were screened. Case-control and cohort studies that reported associations of blood (serum or plasma) levels of folate, B12 and tHcy with prostate cancer risk were included. We also included data from the placebo arms of randomized controlled trials of folic acid and B12 supplementation. Studies reported their results in a number of different ways and presented various models with different adjustments. We selected the age-adjusted estimate, or a more fully adjusted estimate where available, except where the model was deemed by us to be over-adjusted (eg. adjusted for vegetable intake). Data were extracted independently by two investigators (SMC and RH).
Statistical methods
Vitamins and metabolites
Circulating vitamin and metabolite concentrations were categorized into quartiles (with cut-points based on the their distributions among controls), and odds ratios as a measure of relative risk of prostate cancer per quartile of vitamin and metabolite were estimated by conditional logistic regression to account for the matching variables (5-year age group and recruiting general practice), further adjusted for exact age as a continuous variable. Linear trends across quartiles were tested in these models using the mean value for each quartile. Odds ratios for associations with advanced and localized cancer versus controls were compared using a multinomial logistic regression model. This model provides a statistical test for heterogeneity in odds ratios comparing associations of the vitamins and metabolites of interest with localized vs advanced prostate cancers. It is an unconditional model, hence it was adjusted for exact age and the study centre where the recruiting general practice was based (9-level variable). Pairwise correlations between circulating vitamin and metabolite concentrations (and with PSA level) in controls were measured by Spearman’s rank correlation coefficient. Given previous suggestions of possible U-shaped relationships (23), we used fractional polynomials to investigate possible departures from linearity in the relationships between vitamin and metabolite levels (as continuous measures) and prostate cancer risk (35). Circulating vitamin and metabolite concentrations were natural log-transformed (all had non-normal distributions) for inclusion in multivariable linear regression models. These models were used to assess potential confounders (see “other covariates”), to assess the effects of mutually adjusting vitamin and metabolite levels for each other, and to test for interaction between folate and B12 and between folate and alcohol on prostate cancer risk. We investigated by linear regression whether log-transformed vitamin and metabolite concentrations were associated with PSA level among controls, because any such association could bias the PSA-based detection of prostate cancer.
Meta-analysis
To compare across studies, we calculated the log odds ratio (OR) or hazard ratio (HR) per unit increase in vitamin and metabolite concentration. For studies presenting their results within categories of exposure (e.g. quantiles), we used the mean or median exposure in each category when they were reported, and calculated the log OR per unit increase in exposure using the method of Greenland and Longnecker (36). When the mean or median in each group was not reported, and a range of exposure in each group was given, we estimated the mean exposure in each group using the method of Chêne and Thompson (37). Having fitted means to each group, the data were analyzed using the Greenland and Longnecker method (36). We used Stata’s metainf command to investigate whether exclusion of any one study would significantly change the pooled estimate, i.e. whether the pooled point estimate with one study excluded would lie outside the 95% confidence interval of the pooled estimate with all studies included (38).
Software
All statistical analyses were performed using Stata Release 11 (StataCorp. 2009, College Station, TX).
Results
Baseline characteristics
Of the 3,019 cases and controls for whom plasma concentrations were measured, 51 were in unmatched strata. The remaining 2,968 men were in 587 strata. There was a small surplus of controls in 66 strata and a small deficit in 29 strata, hence the final analysis was based on 1,461 cases (1,298 (89%) localized, 163 (11%) advanced) and 1,507 controls. There were no differences in baseline characteristics of cases and controls (Table 1), but anthropometric (height and weight) and lifestyle data (smoking, alcohol consumption, vitamin supplement) were missing (mainly due to non-return of questionnaires) for a higher proportion of controls (26–27%) than cases (18–19%).
Table 1.
Baseline characteristics of participants stratified by case-control status
| Characteristic | Measure | Cases (N=1,461) | Controls (N=1,507) | P* |
|---|---|---|---|---|
| Age | mean (SD) | 62.5 (5.1) | 62.3 (5.1) | 0.2 |
| Ethnicity (white) | 98.5% | 98.7% | 0.3 | |
| BMI (kg/m2)** | mean (SD) | 27.9 (3.7) | 28.2 (4.1) | 0.1 |
| Tobacco use** | Current smoker | 20.2% | 17.3% | 0.1 |
| Ever smoked | 63.3% | 65.5% | 0.3 | |
| Alcohol consumption in the past 12 months** | Almost daily or more often | 38.5% | 37.8% | 0.5 |
| Once or twice per week | 41.2% | 42.4% | ||
| Once or twice per month | 8.5% | 6.9% | ||
| Special occasions or never | 11.9% | 12.9% | ||
| Vitamin supplement use in past 12 months (yes/no)** | 7.8% | 7.9% | 0.9 | |
| Circulating vitamin and metabolite concentrations | median (5th – 95th percentile) | median (5th – 95th percentile) | |
|---|---|---|---|
| Folate (nmol/L) | 15.9 (6.1 – 51.4) | 15.8 (6.2 – 52.3) | 0.6 |
| Vitamin B12 (pmol/L) | 307 (156 – 542) | 299 (158 – 521) | 0.1 |
| Holo-haptocorrin (pmol/L) | 247 (119 – 439) | 240 (120 – 425) | 0.04 |
| Holo-transcobalamin (pmol/L) | 57 (23 – 117) | 56 (24 – 119) | 0.9 |
| Total-transcobalamin (pmol/L) | 860 (612 – 1269) | 874 (602 – 1270) | 0.1 |
| Total homocysteine (μmol/L) | 11.1 (7.8 – 17.6) | 11.1 (7.7 – 17.7) | 0.9 |
Chi-squared test (proportions), Student’s t-test (means) or two-sample Wilcoxon rank-sum (Mann-Whitney) test (medians)
Numbers of cases and controls for whom these data were available: BMI (1,183 cases, 1,105 controls); current smoker (846 cases, 808 controls); ever smoked (1,208 cases, 1,117 controls); alcohol consumption (1,204 cases, 1,116 controls); vitamin supplementation (875 cases, 831 controls)
The majority of pairwise combinations of folate, B12, holo-haptocorrin, holo- and total-transcobalamin, and tHcy were correlated (Supplementary Table 1). Folate was most strongly correlated with tHcy (correlation coefficient = −0.51), but was also correlated with holo-transcobalamin (correlation coefficient = 0.31) and with B12 (correlation coefficient = 0.22). None of the vitamin or metabolite concentrations were associated with PSA levels among controls.
Plasma vitamin and metabolite levels and prostate cancer risk
Of the six vitamins and metabolites, circulating concentrations of B12, holo-haptocorrin, and total-transcobalamin were associated with prostate cancer risk in the basic conditional logistic regression models (Table 2). Higher quartiles of B12 showed a trend (P-for-trend = 0.06) towards increased risk, although this positive association was evident only weakly for the highest vs lowest quartile (OR=1.17, 95% CI 0.95–1.43, P=0.1). Holo-haptocorrin concentration was positively associated (P-for-trend = 0.006) with prostate cancer risk (OR=1.27, 95% CI 1.04 – 1.56, P=0.02 comparing highest vs lowest quartiles). Total-transcobalamin had an inverse association (P-for-trend = 0.04) with risk of localized prostate cancer, evident only weakly for the highest vs lowest quartile (OR=0.80, 95% CI 0.64–1.00, P=0.1).
Table 2.
Odds ratios for prostate cancer by categorical (quartiles) and continuous (loge-transformed) measures of plasma vitamin and metabolite concentrations
| Metabolite | Quartiles in controls (n=1,507) | All cases (n=1,461) vs controls | Localized cases (n=1,298) vs controls | Advanced cases (n=163) vs controls |
|---|---|---|---|---|
| Odds Ratio* (95% CI) | Odds Ratio* (95% CI) | Odds Ratio* (95% CI) | ||
| Folate (nmol/L) | <10.8 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 10.8 – 15.8 | 1.12 (0.91 – 1.37) | 1.18 (0.96 – 1.46) | 0.67 (0.39 – 1.18) | |
| 15.9 – 26.2 | 1.18 (0.96 – 1.44) | 1.17 (0.94 – 1.44) | 1.47 (0.89 – 2.45) | |
| >26.2 | 1.01 (0.82 – 1.24) | 1.07 (0.86 – 1.34) | 0.71 (0.42 – 1.22) | |
| P for trend** | 0.7 | 1.0 | 0.4 | |
| per loge | 0.94 (0.84 – 1.06) | 0.96 (0.86 – 1.08) | 0.90 (0.67 – 1.21) | |
| P for heterogeneity*** 0.5 | ||||
|
| ||||
| Vitamin B12 (pmol/L) | <239 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 239 – 299 | 0.91 (0.74 – 1.12) | 0.95 (0.77 – 1.18) | 0.70 (0.40 – 1.22) | |
| 300 – 376 | 0.99 (0.80 – 1.22) | 0.99 (0.80 – 1.24) | 0.93 (0.55 – 1.57) | |
| >376 | 1.17 (0.95 – 1.43) | 1.20 (0.97 – 1.48) | 1.00 (0.61 – 1.65) | |
| P for trend** | 0.06 | 0.05 | 0.7 | |
| per loge | 1.19 (0.98 – 1.43) | 1.21 (0.99 – 1.48) | 1.04 (0.64 – 1.68) | |
| P for heterogeneity*** 0.4 | ||||
|
| ||||
| Holo-haptocorrin (pmol/L) | <187 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 187 – 240 | 0.94 (0.76 – 1.16) | 0.95 (0.76 – 1.19) | 0.85 (0.50 – 1.44) | |
| 241 – 304 | 0.99 (0.80 – 1.22) | 1.04 (0.84 – 1.29) | 0.68 (0.39 – 1.19) | |
| >304 | 1.27 (1.04 – 1.56) | 1.27 (1.02 – 1.57) | 1.24 (0.75 – 2.04) | |
| P for trend** | 0.006 | 0.01 | 0.3 | |
| per loge | 1.21 (1.01 – 1.44) | 1.23 (1.02 – 1.48) | 1.05 (0.67 – 1.64) | |
| P for heterogeneity*** 0.3 | ||||
|
| ||||
| Holo-transcobalamin (pmol/L) | <42 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 42 – 56 | 1.08 (0.88 – 1.33) | 1.11 (0.89 – 1.37) | 1.02 (0.60 – 1.75) | |
| 57 – 78 | 1.09 (0.89 – 1.34) | 1.12 (0.90 – 1.38) | 1.00 (0.61 – 1.65) | |
| >78 | 1.04 (0.84 – 1.28) | 1.09 (0.87 – 1.35) | 0.85 (0.50 – 1.44) | |
| P for trend** | 0.9 | 0.6 | 0.5 | |
| per loge | 0.99 (0.86 – 1.14) | 1.01 (0.87 – 1.18) | 0.93 (0.66 – 1.32) | |
| P for heterogeneity*** 0.7 | ||||
|
| ||||
| Total-transcobalamin (pmol/L) | <749 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 749 – 874 | 1.05 (0.86 – 1.29) | 1.00 (0.81 – 1.23) | 1.63 (0.94 – 2.83) | |
| 875 – 1024 | 1.02 (0.83 – 1.25) | 1.00 (0.80 – 1.24) | 1.36 (0.78 – 2.37) | |
| >1024 | 0.84 (0.68 – 1.05) | 0.80 (0.64 – 1.00) | 1.36 (0.77 – 2.40) | |
| P for trend** | 0.09 | 0.04 | 0.6 | |
| per loge | 0.76 (0.55 – 1.05) | 0.71 (0.50 – 0.99) | 1.45 (0.65 – 3.25) | |
| P for heterogeneity*** 0.06 | ||||
|
| ||||
| Total homocysteine (3mol/L) | <9.52 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 9.52 – 11.13 | 1.10 (0.90 – 1.35) | 1.11 (0.89 – 1.37) | 0.93 (0.54 – 1.59) | |
| 11.14 – 13.21 | 1.03 (0.84 – 1.27) | 1.01 (0.81 – 1.26) | 1.16 (0.68 – 1.95) | |
| >13.21 | 1.04 (0.84 – 1.28) | 1.01 (0.81 – 1.26) | 1.05 (0.61 – 1.79) | |
| P for trend** | 1.0 | 0.8 | 0.8 | |
| per loge | 0.90 (0.69 – 1.19) | 0.88 (0.66 – 1.17) | 0.94 (0.47 – 1.91) | |
| P for heterogeneity*** 0.3 | ||||
from conditional logistic regression matching on 5-year age group and recruiting centre, further adjusted for exact age (continuous)
from conditional logistic regression matching on 5-year age group and recruiting centre, further adjusted for exact age (continuous)
from multinomial logistic regression, adjusted for age (continuous) and study centre, using log-transformed concentration
For B12, total-transcobalamin, and holo-haptocorrin, the lowest (or highest) odds ratios appeared in the second quartile, but models incorporating fractional polynomial terms for each vitamin or metabolite as continuous variables gave no indication of departure from linearity (all P > 0.1). There were no differences in the associations of vitamin or metabolite concentrations with prostate cancer according to whether the cancer was localized or advanced with the exception of total transcobalamin concentration, which was inversely associated with risk of localized cancer but not associated with advanced cancer (P-for-heterogeneity = 0.06).
Table 2 also shows age-adjusted estimates for each vitamin and metabolite as continuous log-transformed variables (OR per loge approximates to a doubling in concentration) that were included in multivariable conditional logistic regression models. We found little or no change in the estimates for each vitamin and metabolite when mutually adjusted for each other, and there was no interaction between levels of folate and B12. In multivariable conditional logistic regression based on men for whom anthropometric (BMI) and lifestyle (smoking, alcohol consumption, vitamin supplementation) data were available (811 cases, 779 controls), these covariates did not confound the associations of vitamin and metabolite concentrations with prostate cancer risk, and there was no interaction between levels of folate and alcohol intake.
Systematic review and meta-analysis
Our literature search identified 414 studies, of which 20 were eligible. Of these, 6, 5, and 3 studies provided data on blood concentrations of folate (7, 13, 15, 18, 19, 21), B12 (7, 13, 15, 18, 21) and tHcy (7, 13, 21), respectively (Supplementary Table 2). The excluded studies reported data on dietary folate or B12 intake only, or concentrations of other folate-pathway vitamins and metabolites, or outcomes other than prostate cancer risk. The results of the Hultdin et al study (13) were replicated in a subgroup analysis by Johansson et al (15) using the same samples but a different assay (Lactobacillus leichmannii microbiological assay instead of Quantaphase II radioassay) and adjusted for BMI, smoking and concentrations of folate and tHcy. We used the Hultdin et al data, although the Johansson et al data gave very similar results. We used unpublished data from the placebo arms of two randomized controlled trials: one of folic acid and aspirin supplementation for the chemoprevention of colorectal adenomas (18); one of folic acid, vitamin B12 and vitamin B6 supplementation for the lowering of tHcy among patients with ischaemic heart disease (21).
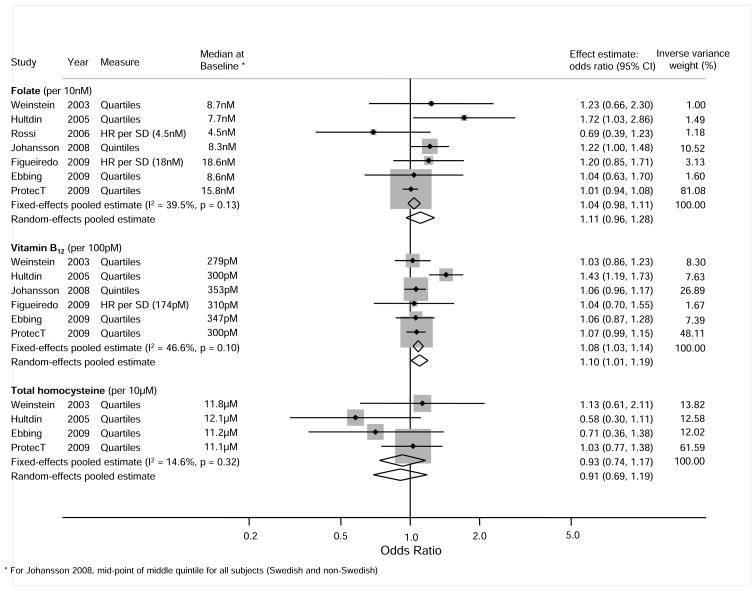
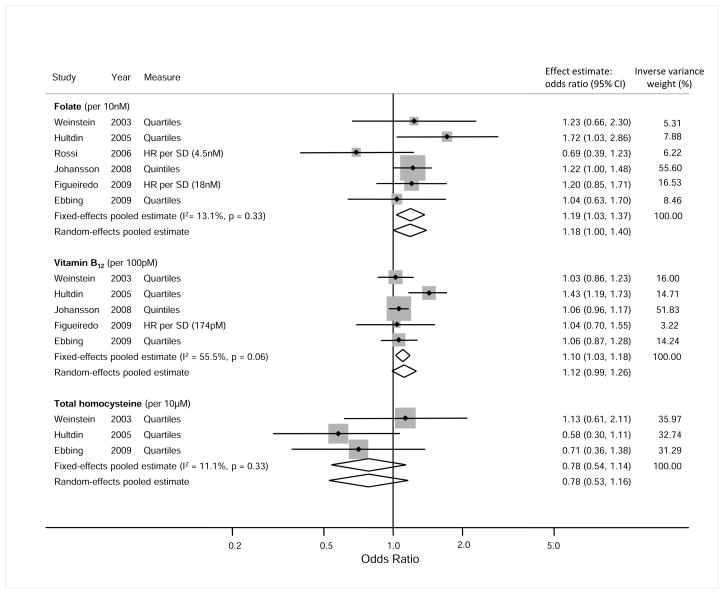
We conducted dose-response meta-analyses, combining our results for serum concentrations of folate, B12 and tHcy with those extracted from the literature and those obtained directly from authors (Figure 1). The pooled (random effects) estimates were: OR=1.11 (95% CI 0.96–1.28) per 10nmol/L folate (P=0.2); OR=1.10 (95% CI 1.01–1.19) per 100pmol/L B12 (P=0.002); and OR=0.91 (95% CI 0.69–1.19) per 10μmol/L tHcy (P=0.5). Hence, there was no strong statistical evidence for an association of folate or tHcy with prostate cancer risk, but there was evidence to support a 10% higher odds per 100pmol/L increase in circulating B12. There was some heterogeneity in the associations of folate (I2=40%) and B12 (I2=47%) with prostate cancer risk. There were too few published studies to assess small-study bias. Influence analysis using Stata’s metainf command showed that excluding any one study from the meta-analysis of associations of B12 and tHcy with prostate cancer risk did not significantly change either the fixed or random effects pooled estimates (Figure 2). However, exclusion of the ProtecT case-control study from the meta-analysis of the associations of folate with prostate cancer risk changed the fixed-effects pooled estimate to OR=1.19 (95% CI 1.03–1.37) per 10nmol/L folate (P=0.02), and left little heterogeneity between the remaining studies (I2=13%), all of which were prospective cohort studies (Figure 2). The median baseline concentrations of B12 and tHcy were similar in all studies, but baseline concentrations of folate were higher in the Figueiredo (USA) and ProtecT studies (Figure 2), and among non-Swedish subjects in the Johansson (pan-European) study. The number of studies was too small to support meta-regression analysis to test whether the measures of effect in each study were related to these baseline values. However, examination of effect estimates against the median baseline values of folate, vitamin B12 and tHcy gave no indication that heterogeneity between studies was attributable to differences in baseline concentrations.
Figure 1.
Meta-analyses of associations of circulating folate, vitamin B12 and tHcy concentrations with prostate cancer risk
Figure 2.
Meta-analyses of associations of circulating folate, vitamin B12 and tHcy concentrations with prostate cancer risk in prospective cohort studies
Discussion
Data from the ProtecT study, when combined with results from all other studies, suggest that high circulating concentrations of vitamin B12 may be associated with increased risk of prostate cancer (Figure 1). The ProtecT data also showed that high circulating concentrations of holo-haptocorrin were associated with increased risk, and high circulating concentrations of total-transcobalamin with decreased risk of prostate cancer. We found no association of folate with prostate cancer risk in the ProtecT data. This result strongly influenced the meta-analysis, which would otherwise have shown a clear positive association of circulating folate with increased prostate cancer risk (Figure 2). It is possible that folate is positively associated with the rate of progression of localized prostate cancer, hence the ProtecT study (based on PSA-detected prevalent cases) would not detect an effect observed in European cohort studies based mainly on clinically-detected cases. We found no associations of tHcy with prostate cancer risk, either in our own data or in the meta-analysis. Although there was considerable variation in baseline folate levels between studies, this did not appear to explain between-study differences in the measures of association of folate with prostate cancer risk. This is consistent with Johansson et al (15), who found no difference of effect between Swedish vs non-Swedish subjects in their pan-European study, even though baseline levels of folate were much lower in Sweden.
The ProtecT study is by far the largest study to date of associations of circulating folate-pathway vitamin and metabolite concentrations with risk of prostate cancer, contributing 81%, 48% and 62% by (inverse variance) weight to the fixed effects meta-analytical results for folate, B12 and tHcy, respectively (Figure 1). The coefficients of variation for our assay results were low, and any measurement error would attenuate effect estimates to the null rather than generate the observed associations. The study’s main limitation is that blood samples were drawn after occurrence of disease, hence causality cannot be directly inferred from our results. However, men were unaware of their disease status so were unlikely to have changed their behaviour or diet in response to disease. Also, our results were similar for advanced and localised disease, which is contrary to what would be expected if effects were secondary to disease status. As with all prostate cancer case-control studies based on PSA testing followed by biopsies, some measurement error would be present due to the imperfect nature of the diagnostic process (39). Non-Caucasian men were not represented in the ProtecT study, or in any of the other studies in our meta-analysis (except for a small proportion (7%) in the Aspirin/Folic Acid Polyp Prevention trial), therefore our findings may not be generalizable to all populations. The small number of advanced cases in ProtecT means we may have been underpowered to detect true differences in associations of vitamin or metabolite concentrations with prostate cancer according to whether the cancer was localized or advanced. Fractional polynomial analysis of the ProtecT data did not indicate departure from linearity for the associations of B12, holo-haptocorrin and total-transcobalamin with prostate cancer risk, but these associations were evident only in the top quartiles when analysed as categorical variables. Whether there really is only an effect at extreme elevations could not be discerned from our review of the literature, although two studies showed a similar pattern, with associations evident only in the top quartile of circulating folate (13, 15).
That we found no confounding or effect modification by BMI, smoking or alcohol consumption of associations between vitamin and metabolite concentrations and prostate cancer is consistent with other studies (7, 13, 14, 40). Among men with prostate cancer in the ProtecT study, those who reported little or no sexual activity had higher plasma B12 concentrations [data not shown]. However, among men with raised PSA levels in the ProtecT study, there was no association between sexual dysfunction and prostate cancer, hence confounding by sexual activity is unlikely to explain our findings (41).
The positive association of B12 with prostate cancer risk could be causal, or due to reverse-causation or coincidental. A causal association would be consistent with epigenetic mechanisms of prostatic carcinogenesis if these were triggered by elevated levels of B12 independently of folate and tHcy. Although some associations of B12 with DNA methylation have been observed in rats (42, 43) and humans (44, 45), such a process as a cause of prostate cancer remains speculative. Vitamin B12 is an essential co-factor of methionine synthase (MTR), and we reported in a previous meta-analysis that the A2756G polymorphism of this enzyme is associated with increased risk of prostate cancer (46). We proposed a causal ‘activating polymorphism’ mechanism that might be consistent with our finding for B12, but this is speculative.
One possible mechanism of reverse causation could be prostate tumour cells having an increased demand for B12 due to increased biosynthesis of polyamines (47), which in turn up-regulate the activity of MTR (48). Another mechanism could be that elevated levels of plasma B12 are due to increased production of haptocorrin by prostate tumour cells (49), an effect which may explain high levels of B12 observed in myelogeneous leukemias and metastatic cancers (30). Whether prostate carcinomas can raise plasma concentrations of haptocorrin and B12 by such processes remains hypothetical, and we did not observe stronger positive associations of plasma B12 and holo-haptocorrin with advanced vs localized prostate cancer. However, the plausibility of reverse-causation as an explanation for our findings is perhaps reinforced by the absence of an association of holo-transcobalamin, representing the bioavailable fraction of B12, with prostate cancer risk. We cannot suggest a clear biological explanation for the inverse association of total-transcobalamin with localized prostate cancer. Finally, it is conceivable that folate-pathway genes could be affected coincidentally by epigenetic alterations which play a causal role in prostate cancer. For example, the multidrug resistance protein gene (MRP1), which is over-expressed in several cancers including prostate cancer (50), has recently been shown to play a role in cellular efflux of B12 (51).
That we found similar associations of folate, B12 and tHcy with advanced and localized prostate cancer is consistent with previous studies (7, 13–15), although Johansson et al reported (from a cohort study) borderline heterogeneity (P=0.05) between localized and advanced cases for B12: a doubling in vitamin B12 concentration was associated with an OR=1.69 (95% CI 1.05–2.72, P = 0.03) of advanced cancer, whereas B12 concentrations were not associated with risk for localized disease (OR=0.96; 95% CI 0.71–1.29, P = 0.8) (15). We found marginal evidence of similar heterogeneity (P=0.09) for total-transcobalamin (advanced disease OR=1.46 (95% CI 0.65–3.26); localized disease OR=0.70 (95% CI 0.50 – 0.99)). Levels of B12 and total-transcobalamin in our data were uncorrelated, and our finding may be due to chance rather than a corroboration of Johansson et al’s finding for B12.
The only studies to date of dietary B12 intake and prostate cancer risk both reported positive associations: Vlajinac et al found two-fold higher odds (OR=2.07, 95% CI 1.08–3.97; P-for-trend=0.02) for the highest vs lowest tertile (12); Weinstein et al (among smokers) found 36% higher odds in the highest vs lowest quintile (OR=1.36, 95% CI 1.14–1.62; P-for-trend=0.01) (14). Both studies reported that these results withstood adjustment for dietary covariates; Vlajinac et al for intake of total energy, protein, total fat, saturated fatty acids, carbohydrate, total sugar, fibre, retinol equivalent, α-tocopherol, folate, sodium, potassium, calcium, phosphorus, magnesium and iron (12); Weinstein et al for total energy, total protein, animal protein, total fat, animal fat, folate, B6, methionine, iron, and specific foods which are correlates of B12 intake (fish, organ meats, sausages, cholesterol, fatty acids, vitamins and minerals) (14). Hence, there was no confounding by other nutrients which co-occur in foods high in B12, and which may be associated with prostate cancer risk. Both studies also adjusted for non-dietary covariates. Although these results may suggest a possible causal relationship, the limitations of studies based on food-frequency questionnaires are well-known, particularly with regard to diet-cancer associations (52). Indeed, the B12 dietary intake finding by Weinstein et al was not found in their earlier, albeit smaller, study of circulating concentrations of B12 (7).
We conclude that our finding of a positive association of circulating B12 with increased prostate cancer risk could be explained by reverse-causality. However, given current controversies over mandatory B12 fortification (53), further research to eliminate a causal role of vitamin B12 in prostate cancer initiation and/or progression is required, including Mendelian randomisation analyses (54) and repeat measurements of B12 and holo-haptocorrin levels during prostate cancer development and/or before and after treatment. Our meta-analysis did not entirely rule out a positive association of circulating folate with increased prostate cancer risk. As with B12, even a weak positive association would be a significant public health issue, given the high prevalence of prostate cancer, and legitimate concern about the potential harms vs benefits of mandatory folic acid fortification (23).
Supplementary Material
Acknowledgments
Funding/Support: This research was funded by World Cancer Research Fund (WCRF) UK (grant number: 2007/07). The National Cancer Research Institute (administered by the Medical Research Council) provided support for the development of the ProtecT epidemiological database through the ProMPT (Prostate Mechanisms of Progression and Treatment) collaborative. The ProtecT study is supported by the UK NIHR Health Technology Assessment Programme (projects 96/20/06, 96/20/99). Support for the ProtecT biorepository in Cambridge is provided by NIHR through the Biomedical Research Centre.
Role of the Funders: The funders were nonprofit organizations with no participating role in the study.
Footnotes
Financial Disclosures: No authors reported any conflicts of interest or financial disclosures.
Additional Contributions: The authors would like to acknowledge the tremendous contribution of all members of the ProtecT study research group, and especially the following who were involved in this research: Prasad Bollina, Sue Bonnington, Debbie Cooper, Andrew Doble, Alan Doherty, Emma Elliott, David Gillatt, Pippa Herbert, Peter Holding, Joanne Howson, Liz Down, Mandy Jones, Roger Kockelbergh, Howard Kynaston, Teresa Lennon, Norma Lyons, Hilary Moody, Philip Powell, Stephen Prescott, Liz Salter, Pauline Thompson. We would like to thank Cynthia Prendergast (University of Oxford) for her invaluable help with the biochemical analyses.
Author Contributions: Collin, Metcalfe and Martin had full access to all of the data in the study and take final responsibility for the integrity of the data, the accuracy of the data analysis and the decision to submit for publication. Hypothesis development and acquisition of funding: Martin (principal investigator), Davey Smith, Refsum, Smith, Lewis, Metcalfe, Donovan, Neal, Hamdy (co-investigators). Original ProtecT study design: Donovan, Neal, Hamdy. Acquisition of data: Collin, Martin, Davis, Marsden, Johnston, Lane, Ebbing, Bønaa, Nygård, Ueland, Grau, Baron. Analysis and interpretation of data: Collin, Metcalfe, Refsum, Harris, Ebbing, Grau, Martin. Drafting of the manuscript: Collin. Critical revision of the manuscript for important intellectual content: Collin, Metcalfe, Refsum, Lewis, Zuccolo, Davey Smith, Chen, Harris, Lane, Ebbing, Bønaa, Nygård, Ueland, Grau, Baron, Donovan, Neal, Hamdy, Smith, Martin. Statistical analysis: Collin, Metcalfe, Ebbing, Grau.. Administrative, technical, or material support: Collin, Davis, Marsden, Johnston, Lane. Day to day senior study supervision: Martin, Metcalfe..
Reference List
- 1.Choi SW, Mason JB. Folate and carcinogenesis: an integrated scheme. J Nutr. 2000;130:129–32. doi: 10.1093/jn/130.2.129. [DOI] [PubMed] [Google Scholar]
- 2.Farber S. Some observations on the effect of folic acid antagonists on acute leukemia and other forms of incurable cancer. Blood. 1949;4:160–7. [PubMed] [Google Scholar]
- 3.Hertz R, Li MC, Spencer DB. Effect of methotrexate therapy upon choriocarcinoma and chorioadenoma. Proc Soc Exp Biol Med. 1956;93:361–6. doi: 10.3181/00379727-93-22757. [DOI] [PubMed] [Google Scholar]
- 4.Dong LM, Potter JD, White E, et al. Genetic susceptibility to cancer: the role of polymorphisms in candidate genes. JAMA. 2008;299:2423–36. doi: 10.1001/jama.299.20.2423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yegnasubramanian S, Haffner MC, Zhang Y, et al. DNA hypomethylation arises later in prostate cancer progression than CpG island hypermethylation and contributes to metastatic tumor heterogeneity. Cancer Res. 2008;68:8954–67. doi: 10.1158/0008-5472.CAN-07-6088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bistulfi G, Vandette E, Matsui SI, Smiraglia DJ. Mild folate deficiency induces genetic and epigenetic instability and phenotype changes in prostate cancer cells. BMC Biol. 2010;8:6. doi: 10.1186/1741-7007-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinstein SJ, Hartman TJ, Stolzenberg-Solomon R, et al. Null association between prostate cancer and serum folate, vitamin B(6), vitamin B(12), and homocysteine. Cancer Epidemiol Biomarkers Prev. 2003;12:1271–2. [PubMed] [Google Scholar]
- 8.Pelucchi C, Galeone C, Talamini R, et al. Dietary folate and risk of prostate cancer in Italy. Cancer Epidemiol Biomarkers Prev. 2005;14:944–8. doi: 10.1158/1055-9965.EPI-04-0787. [DOI] [PubMed] [Google Scholar]
- 9.Stevens VL, Rodriguez C, Pavluck AL, et al. Folate nutrition and prostate cancer incidence in a large cohort of US men. Am J Epidemiol. 2006;163:989–96. doi: 10.1093/aje/kwj126. [DOI] [PubMed] [Google Scholar]
- 10.Lu QY, Hung JC, Heber D, et al. Inverse associations between plasma lycopene and other carotenoids and prostate cancer. Cancer Epidemiol Biomarkers Prev. 2001;10:749–56. [PubMed] [Google Scholar]
- 11.McCann SE, Ambrosone CB, Moysich KB, et al. Intakes of selected nutrients, foods, and phytochemicals and prostate cancer risk in western New York. Nutr Cancer. 2005;53:33–41. doi: 10.1207/s15327914nc5301_4. [DOI] [PubMed] [Google Scholar]
- 12.Vlajinac HD, Marinkovic JM, Ilic MD, Kocev NI. Diet and prostate cancer: a case-control study. Eur J Cancer. 1997;33:101–7. doi: 10.1016/s0959-8049(96)00373-5. [DOI] [PubMed] [Google Scholar]
- 13.Hultdin J, van Guelpen BR, Bergh A, Hallmans G, Stattin P. Plasma folate, vitamin B12, and homocysteine and prostate cancer risk: a prospective study. Int J Cancer. 2005;113:819–24. doi: 10.1002/ijc.20646. [DOI] [PubMed] [Google Scholar]
- 14.Weinstein SJ, Stolzenberg-Solomon R, Pietinen P, et al. Dietary factors of one-carbon metabolism and prostate cancer risk. Am J Clin Nutr. 2006;84:929–35. doi: 10.1093/ajcn/84.4.929. [DOI] [PubMed] [Google Scholar]
- 15.Johansson M, Appleby PN, Allen NE, et al. Circulating concentrations of folate and vitamin B12 in relation to prostate cancer risk: results from the European prospective investigation into cancer and nutrition study. Cancer Epidemiol Biomarkers Prev. 2008;17:279–85. doi: 10.1158/1055-9965.EPI-07-0657. [DOI] [PubMed] [Google Scholar]
- 16.Johansson M, van Guelpen BR, Vollset SE, et al. One-carbon metabolism and prostate cancer risk: prospective investigation of seven circulating B vitamins and metabolites. Cancer Epidemiol Biomarkers Prev. 2009;18:1538–43. doi: 10.1158/1055-9965.EPI-08-1193. [DOI] [PubMed] [Google Scholar]
- 17.Kasperzyk JL, Fall K, Mucci LA, et al. One-carbon metabolism-related nutrients and prostate cancer survival. Am J Clin Nutr. 2009;90:561–9. doi: 10.3945/ajcn.2009.27645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Figueiredo JC, Grau MV, Haile RW, et al. Folic acid and risk of prostate cancer: results from a randomized clinical trial. J Natl Cancer Inst. 2009;101:432–5. doi: 10.1093/jnci/djp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rossi E, Hung J, Beilby JP, et al. Folate levels and cancer morbidity and mortality: prospective cohort study from Busselton, Western Australia. Ann Epidemiol. 2006;16:206–12. doi: 10.1016/j.annepidem.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Shannon J, Phoutrides E, Palma A, et al. Folate intake and prostate cancer risk: a case-control study. Nutr Cancer. 2009;61:617–28. doi: 10.1080/01635580902846593. [DOI] [PubMed] [Google Scholar]
- 21.Ebbing M, Bonaa KH, Nygard O, et al. Cancer Incidence and Mortality After Treatment With Folic Acid and Vitamin B12. JAMA. 2009;302:2119–26. doi: 10.1001/jama.2009.1622. [DOI] [PubMed] [Google Scholar]
- 22.Martinez ME, Marshall JR, Giovannucci E. Diet and cancer prevention: the roles of observation and experimentation. Nat Rev Cancer. 2008;8:694–703. doi: 10.1038/nrc2441. [DOI] [PubMed] [Google Scholar]
- 23.Smith AD, Kim YI, Refsum H. Is folic acid good for everyone? Am J Clin Nutr. 2008;87:517–33. doi: 10.1093/ajcn/87.3.517. [DOI] [PubMed] [Google Scholar]
- 24.Seetharam B, Yammani RR. Cobalamin transport proteins and their cell-surface receptors. Expert Rev Mol Med. 2003;5:1–18. doi: 10.1017/S1462399403006422. [DOI] [PubMed] [Google Scholar]
- 25.Bor MV, Nexo E, Hvas AM. Holo-transcobalamin concentration and transcobalamin saturation reflect recent vitamin B12 absorption better than does serum vitamin B12. Clin Chem. 2004;50:1043–9. doi: 10.1373/clinchem.2003.027458. [DOI] [PubMed] [Google Scholar]
- 26.Afman LA, van der Put NM, Thomas CM, Trijbels JM, Blom HJ. Reduced vitamin B12 binding by transcobalamin II increases the risk of neural tube defects. QJM. 2001;94:159–66. doi: 10.1093/qjmed/94.3.159. [DOI] [PubMed] [Google Scholar]
- 27.Refsum H, Smith AD. Low vitamin B-12 status in confirmed Alzheimer’s disease as revealed by serum holotranscobalamin. J Neurol Neurosurg Psychiatry. 2003;74:959–61. doi: 10.1136/jnnp.74.7.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carmel R. Extreme elevation of serum transcobalamin I in patients with metastatic cancer. N Engl J Med. 1975;292:282–4. doi: 10.1056/NEJM197502062920603. [DOI] [PubMed] [Google Scholar]
- 29.Wakatsuki Y, Inada M, Kudo H, et al. Immunological characterization and clinical implication of cobalamin binding protein in human gastric cancer. Cancer Res. 1989;49:3122–8. [PubMed] [Google Scholar]
- 30.Ermens AA, Vlasveld LT, Lindemans J. Significance of elevated cobalamin (vitamin B12) levels in blood. Clin Biochem. 2003;36:585–90. doi: 10.1016/j.clinbiochem.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 31.Molloy AM, Scott JM. Microbiological assay for serum, plasma, and red cell folate using cryopreserved, microtiter plate method. Methods Enzymol. 1997;281:43–53. doi: 10.1016/s0076-6879(97)81007-5. [DOI] [PubMed] [Google Scholar]
- 32.Kelleher BP, Broin SD. Microbiological assay for vitamin B12 performed in 96-well microtitre plates. J Clin Pathol. 1991;44:592–5. doi: 10.1136/jcp.44.7.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Refsum H, Johnston C, Guttormsen AB, Nexo E. Holotranscobalamin and total transcobalamin in human plasma: determination, determinants, and reference values in healthy adults. Clin Chem. 2006;52:129–37. doi: 10.1373/clinchem.2005.054619. [DOI] [PubMed] [Google Scholar]
- 34.Shipchandler MT, Moore EG. Rapid, fully automated measurement of plasma homocyst(e)ine with the Abbott IMx analyzer. Clin Chem. 1995;41:991–4. [PubMed] [Google Scholar]
- 35.Royston P, Sauerbrei W. Multivariable modelling. Chichester: Wiley; 2008. [Google Scholar]
- 36.Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–9. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- 37.Chene G, Thompson SG. Methods for summarizing the risk associations of quantitative variables in epidemiologic studies in a consistent form. Am J Epidemiol. 1996;144:610–21. doi: 10.1093/oxfordjournals.aje.a008971. [DOI] [PubMed] [Google Scholar]
- 38.Tobias A. sbe26: Assessing the influence of a single study in the meta-analysis estimate. Stata Technical Bulletin. 1999;47:15–7. [Google Scholar]
- 39.Iguchi T, Wang CY, Delongchamps NB, et al. Occult prostate cancer effects the results of case-control studies due to verification bias. Anticancer Res. 2008;28:3007–10. [PMC free article] [PubMed] [Google Scholar]
- 40.Shannon J, Phoutrides E, Palma A, et al. Folate intake and prostate cancer risk: a case-control study. Nutr Cancer. 2009;61:617–28. doi: 10.1080/01635580902846593. [DOI] [PubMed] [Google Scholar]
- 41.Collin SM, Metcalfe C, Donovan JL, et al. Associations of sexual dysfunction symptoms with PSA-detected localised and advanced prostate cancer: A case-control study nested within the UK population-based ProtecT (Prostate testing for cancer and Treatment) study. Eur J Cancer. 2009;45:3254–61. doi: 10.1016/j.ejca.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 42.Brunaud L, Alberto JM, Ayav A, et al. Vitamin B12 is a strong determinant of low methionine synthase activity and DNA hypomethylation in gastrectomized rats. Digestion. 2003;68:133–40. doi: 10.1159/000075307. [DOI] [PubMed] [Google Scholar]
- 43.Choi SW, Friso S, Ghandour H, et al. Vitamin B-12 deficiency induces anomalies of base substitution and methylation in the DNA of rat colonic epithelium. J Nutr. 2004;134:750–5. doi: 10.1093/jn/134.4.750. [DOI] [PubMed] [Google Scholar]
- 44.Al-Ghnaniem R, Peters J, Foresti R, Heaton N, Pufulete M. Methylation of estrogen receptor alpha and mutL homolog 1 in normal colonic mucosa: association with folate and vitamin B-12 status in subjects with and without colorectal neoplasia. Am J Clin Nutr. 2007;86:1064–72. doi: 10.1093/ajcn/86.4.1064. [DOI] [PubMed] [Google Scholar]
- 45.Piyathilake CJ, Johanning GL, Macaluso M, et al. Localized folate and vitamin B-12 deficiency in squamous cell lung cancer is associated with global DNA hypomethylation. Nutr Cancer. 2000;37:99–107. doi: 10.1207/S15327914NC3701_13. [DOI] [PubMed] [Google Scholar]
- 46.Collin SM, Metcalfe C, Zuccolo L, et al. Association of Folate-Pathway Gene Polymorphisms with the Risk of Prostate Cancer: a Population-Based Nested Case-Control Study, Systematic Review, and Meta-analysis. Cancer Epidemiol Biomarkers Prev. 2009;18:2528–39. doi: 10.1158/1055-9965.EPI-09-0223. [DOI] [PubMed] [Google Scholar]
- 47.Goodwin AC, Jadallah S, Toubaji A, et al. Increased spermine oxidase expression in human prostate cancer and prostatic intraepithelial neoplasia tissues. Prostate. 2008;68:766–72. doi: 10.1002/pros.20735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kenyon SH, Nicolaou A, Ast T, Gibbons WA. Stimulation in vitro of vitamin B12-dependent methionine synthase by polyamines. Biochem J. 1996;316:661–5. doi: 10.1042/bj3160661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Waibel R, Treichler H, Schaefer NG, et al. New derivatives of vitamin B12 show preferential targeting of tumors. Cancer Res. 2008;68:2904–11. doi: 10.1158/0008-5472.CAN-07-6771. [DOI] [PubMed] [Google Scholar]
- 50.Munoz M, Henderson M, Haber M, Norris M. Role of the MRP1/ABCC1 multidrug transporter protein in cancer. IUBMB Life. 2007;59:752–7. doi: 10.1080/15216540701736285. [DOI] [PubMed] [Google Scholar]
- 51.Beedholm-Ebsen R, van de Wetering K, Hardlei T, et al. Identification of multidrug resistance protein 1 (MRP1/ABCC1) as a molecular gate for cellular export of cobalamin. Blood. 2010;115:1632–9. doi: 10.1182/blood-2009-07-232587. [DOI] [PubMed] [Google Scholar]
- 52.Kristal AR, Peters U, Potter JD. Is it time to abandon the food frequency questionnaire? Cancer Epidemiol Biomarkers Prev. 2005;14:2826–8. doi: 10.1158/1055-9965.EPI-12-ED1. [DOI] [PubMed] [Google Scholar]
- 53.Green R. Is it time for vitamin B-12 fortification? What are the questions? Am J Clin Nutr. 2009;89:712S–6S. doi: 10.3945/ajcn.2008.26947E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–63. doi: 10.1002/sim.3034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.