Abstract
Background:
Poor care and hygiene of contact lens (CL) results in eye problems and infections. Healthcare workers have an important role in advocating correct lens care.
Objectives:
To determine the practices of CL care and the adverse consequences of poor CL care among healthcare workers.
Setting and Design:
A cross-sectional study in one public and three private sector hospitals in Karachi, Pakistan, in 2009–2010.
Materials and Methods:
We questioned 500 healthcare workers of all ages and both sexes, who wore CL, about compliance with advice on care and any complications due to improper hygiene practices. Ethical approval was obtained. Chi-square tests were used to determine significance and p-value less than 0.05 was considered statistically significant.
Results:
Of the total CL users, 385 (77%) were females. Most (75%) respondents wore CL to correct myopia, whereas 54% wore CL only occasionally. Surprisingly, only 24% knew the CL cleaning protocol. Lens solution was changed daily by 33% of users and after more than 2 weeks by 42%. Although 412 (82%) participants practised reasonable hand hygiene before inserting CL, 88 (18%) did not. Infection and eye dryness were statistically significantly (P < 0.01) associated with sex, hand-washing, and frequency of CL use.
Conclusion:
Noncompliance with the CL protocol was common among healthcare workers in our society. This behavior calls for targeted health education and awareness programs for healthcare workers.
Keywords: Contact lens, healthcare workers, health professionals
Contact lens (CL) offers many advantages over eyeglasses, in addition to correcting refractive errors. A growing body of research shows that CL is safe and convenient, even for children and adolescents.[1,2,3,4,5,6] Nevertheless, complications have been associated with CL wear, ranging from conjunctivitis and dryness symptoms to microbial keratitis, which in rare instances lead to loss of vision.[7,8,9]
Usually, such complications tend not to be severe, as they are often attributable to poor CL care and hygiene. One in three eye problems suffered by lens users is a direct result of improper lens care and cleaning.[10,11] A recent survey showed significant noncompliance with lens care, case hygiene, and lens case replacement procedures.[11] Furthermore, prolonged wear and overnight use of CL increases the risk of infection.[12]
Healthcare professionals are role models for their patients. They are the immediate source of recommendation for CL to patients and have a key role in advocating correct practices for the use and care of CL.[10,13] Although a few studies have documented contamination of CL in Pakistan,[14,15] a literature review showed that the practices of health professionals wearing CL and their compliance with CL care have not been studied. Eye health professionals are in an obvious position to communicate better understanding of the value of vision care and vision wear, provided they themselves are well informed. The objective of this study was to determine the practices of CL care and to document the adverse consequences of poor CL use among health professionals in Pakistan.
Materials and Methods
A cross-sectional study was conducted between October 2009 and April 2010. A total of 1620 healthcare workers in one public and three private sector hospitals in Karachi were approached. According to the World Health Organization, a healthcare worker is anyone whose focus or activity is to improve health, including doctors, dentists, nurses, and midwives, as well as technicians and managers.[16,17] Those who wore CL were asked to participate in the study. The order of priority was doctors, dentists, and then paramedical staff; individuals with other occupations in the hospital setting and those wearing rigid CL were excluded. With an estimated prevalence of 50%, a 95% level of confidence, and an absolute precision of 0.05, a sample size of 385 was calculated. Nonetheless, 500 CL users filled in a self-administered questionnaire.
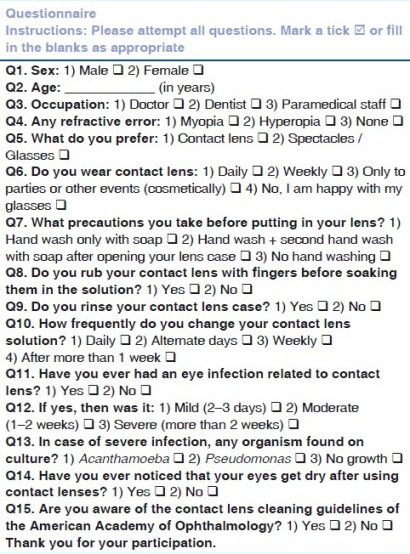
The questionnaire [Appendix 1] was developed on the basis of the Contact Lens Care Guidelines[18] of the American Academy of Ophthalmology [Box 1]. It included questions on compliance with recommendations for CL care and complications due to improper hygiene practices and also elicited data on the sex, age, and occupation of the respondents. Additional hand-washing with soap before opening the lens case, changing the lens solution daily, rubbing the CL with fingers, and rinsing the lenses with solution before soaking were taken as strong adherence to the CL protocol, whereas omission of any of these acts was considered as poor adherence to the protocol. Eye infections were graded as mild, moderate, or severe. An infection lasting 2–3 days was considered mild, one lasting 1–2 weeks was considered moderate, and one lasting for more than 2 weeks was considered severe. Mild and moderate cases were included in the broader category of “contact lens-induced red eye,” while corneal abscess formation and anterior chamber inflammation were considered severe infections. The participants were asked to recall the infection caused by using CL, and those with severe infections were asked to identify the organism (if any) found on culture. Eligibility criteria included all healthcare personnel irrespective of age and sex, while individuals with other occupations in the hospital setting and those wearing rigid CL were excluded from the study.
Box 1.
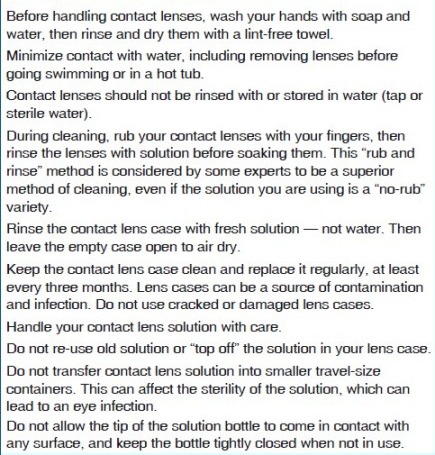
Contact Lens Care Guidelines
The aim, objectives, and rationale of the study were verbally explained to the participants in a plain language statement, and filling in the questionnaire was taken as consent to participate in the study. The participants were allowed to withdraw at any time during filling in the questionnaire. The research protocol was approved by the Ethics Review Board of the university to which the researchers belong.
The data variables of completely filled questionnaires were entered into SPSS version 18.0 software. Frequencies of reported variables were reported as percentages, and chi-square test was used to analyze categorical variables where appropriate; p-value < 0.05 was taken as statistically significant.
Results
Women represented the majority of the 500 respondents (385, 77%), with 115 (23%) male participants. The participants consisted of 340 (68%) doctors, 113 (22%) dentists, and 47 (9.4%) paramedical staff. Most (75%) of the participants wore CL to correct myopia, while 25% used them for aesthetic or cosmetic purposes; 54% wore CL only occasionally. Surprisingly, only 24% of the respondents were aware of the CL cleaning protocol.
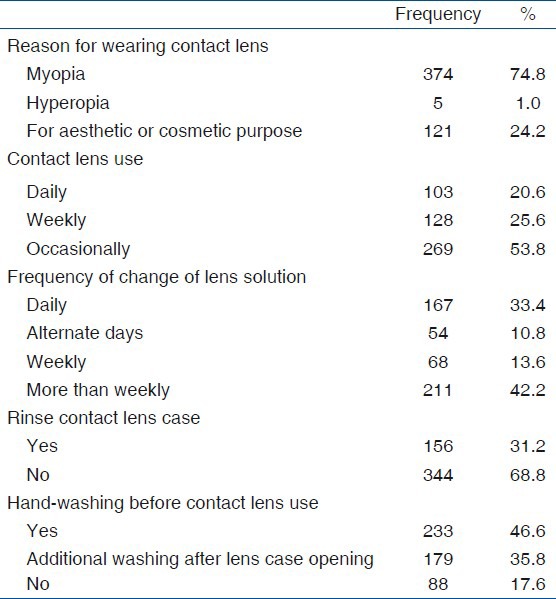
Regarding CL practices, 167 (33%) respondents changed the lens solution daily, while 211 (42%) changed it after more than 1 week. Only 31.2% of the participants rinsed the contact lens case. Although 412 (82%) practised reasonable hand hygiene before inserting their CL, this was not observed by 88 (18%) respondents [Table 1].
Table 1.
Reason for use of contact lenses, frequency of use, frequency of changing lens solution and handwashing practices among 500 health professionals
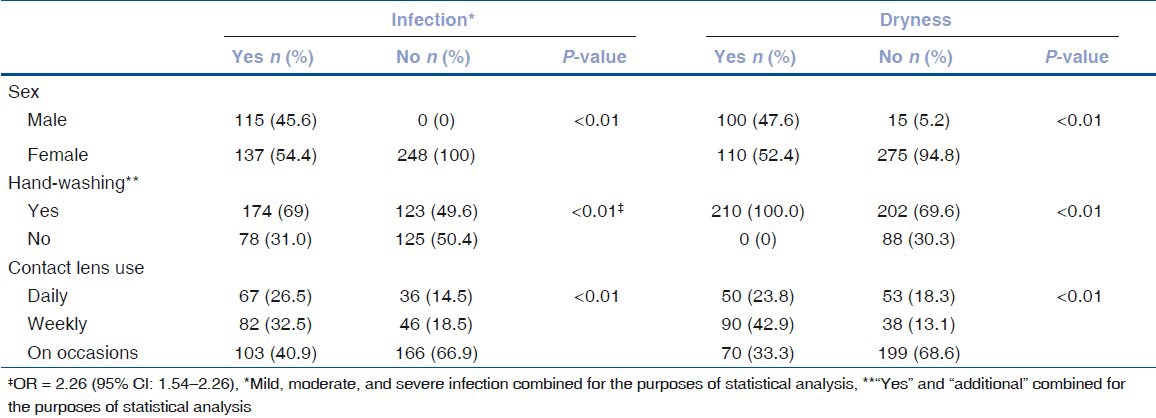
Half of the respondents complained of varying degrees of eye infection after recurrent use of CL [Table 2]. Of the 36 respondents with severe infection, 17 reported a positive culture of Acanthamoeba, while the rest recorded no growth in culture. Of those with less severe conditions, 210 (42%) had eye dryness after CL use. When infections and dryness were cross-tabulated with sex, hand-washing practices, and frequency of CL use, all the variables were found to be statistically significant (P < 0.01). Surprisingly, the odds ratio for infection after hand-washing was 2.26 (95% CI: 1.54–3.32) [Table 3].
Table 2.
Eye complaints due to use of contact lens among 500 health professionals
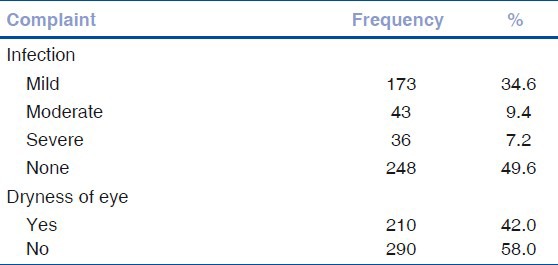
Table 3.
Eye complaints according to sex and contact lens care practices among 500 health professionals
Discussion
An unexpected result of this study was the lack of awareness of most healthcare providers about standard CL care, which is even more remarkable as all the participants were CL users. Although no guidelines for CL care have been published in Pakistan, guidelines have been published for the general public in Australia[10] and the USA[13,18,19] and specifically for general practitioners in the United Kingdom.[9] Knowledge about CL care and hygiene for healthcare personnel is needed in developing countries, including Pakistan. Nevertheless, a study in Australia reported inconsistent, inadequate recommendations for CL hygiene by various advisory bodies, including optometrists.[20]
One of the well-established risk factors for CL-related complications is poor hand hygiene, the presence of which has been reported to be between 11% and 50%.[7,21] In the present study, however, participants who did not wash their hands had a significantly lower odds ratio for having eye infection than those who washed their hands. Hand-washing might have been ineffective because of (a) use of a wrong technique for hand-washing; (b) use of polluted water, especially in the light of the positive cultures of Acanthamoeba, a ubiquitous organism; (c) changing the lens solution only at an interval of more than 1 week; or (d) poor CL case hygiene. Although these healthcare providers took the specific precautionary step of hand-washing, they should also stress other measures of CL care and transmit such practices to CL users in their clinical practice.
Dryness of eyes is a common complication of CL use. Slightly less than half the respondents in the present study complained of eye dryness, which was statistically significant (P < 0.01) for men. In contrast, Chalmers and Begley (2006) analyzed dryness symptoms among patients with and without CL and found dryness in a higher proportion of women. Although a similar proportion of dryness was also found among male users in another study,[8] the occasional use of CL only for cosmetic reasons by women in our study might explain this gender trend. A recent French study reported a highly increased relative risk for infections among cosmetic CL wearers.[22] As more than half the respondents in the present study wore CL only occasionally, they probably did not change their solution daily, and it is unlikely that they replaced their disinfecting solution at least 6 h before using the CL. These results support those of the previously mentioned study.
Regardless of sustained hand-washing by most participants in the present study, a delay in changing the CL solution might have contributed significantly to the development of infections, including microbial keratitis. Another survey showed that although nearly two-thirds of medical practitioners advised their patients to clean the CL cases after each use, only half the patients actually did so.[19]
The target population of this study was a specific group of professionals, and the results cannot be generalized. A larger study would be required to determine the knowledge and practices of the general population regarding CL care.
Conclusion
Noncompliance with CL care practices was found among healthcare professionals in our study, for whom promoting correct CL care should be a priority. The behavior might be due partly to a lack of emphasis on lens care hygiene during their training. Targeted health education and awareness programs, especially for young people, could go a long way to improving compliance with CL care and preventing CL-related complications.
Appendix 1
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kemper AR, Bruckman D, Freed GL. Prevalence and distribution of corrective lenses among school-age children. Optom Vis Sci. 2004;81:7–10. doi: 10.1097/00006324-200401000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walline JJ, Long S, Zadnik K. Daily disposable contact lens wear in myopic children. Optom Vis Sci. 2004;81:255–9. doi: 10.1097/00006324-200404000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Charm J, Cheung SW, Cho P. Practitioners’ analysis of contact lens practice in Hong Kong. Cont Lens Anterior Eye. 2010;33:104–11. doi: 10.1016/j.clae.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Morgan PB, Efron N, Helland M, Itoi M, Jones D, Nichols JJ, et al. Demographics of international contact lens prescribing. Cont Lens Anterior Eye. 2010;33:27–9. doi: 10.1016/j.clae.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Woods CA, Morgan PB. Contact lens prescribing in the Australian states and territories 2001. Clin Exp Optom. 2002;85:279–83. doi: 10.1111/j.1444-0938.2002.tb03083.x. [DOI] [PubMed] [Google Scholar]
- 6.Cheung SW, Cho P, Edwards MH. Contact lens practice in Hong Kong in the new millennium. Clin Exp Optom. 2002;85:358–64. [PubMed] [Google Scholar]
- 7.Wu Y, Carnt N, Stapleton F. Contact lens user profile, attitudes and level of compliance to lens care. Cont Lens Anterior Eye. 2010;33:183–8. doi: 10.1016/j.clae.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Chalmers RL, Begley CG. Dryness symptoms among an unselected clinical population with and without contact lens wear. Cont Lens Anterior Eye. 2006;29:25–30. doi: 10.1016/j.clae.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Terry P. Contact lenses: GP guide to choice and the complications. Prescriber. 2009;5:53–7. [Google Scholar]
- 10.Sweeney D, Holden B, Evans K, Ng V, Cho P. Best practice contact lens care: A review of the Asia Pacific Contact Lens Care Summit. Clin Exp Optom. 2009;92:78–89. doi: 10.1111/j.1444-0938.2009.00353.x. [DOI] [PubMed] [Google Scholar]
- 11.Hickson-Curran S, Chalmers RL, Riley C. Patient attitudes and behavior regarding hygiene and replacement of soft contact lenses and storage cases. Cont Lens Anterior Eye. 2011;34:207–15. doi: 10.1016/j.clae.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Efron N, Morgan PB. Rethinking contact lens associated keratitis. Clin Exp Optom. 2006;89:280–98. doi: 10.1111/j.1444-0938.2006.00069.x. [DOI] [PubMed] [Google Scholar]
- 13.St Louis: Missouri; 2006. [accessed on 2011 Feb 19]. American Optometric Association. What you need to know about contact lens hygiene & compliance. Available from: http://www.aoa.org/documents/AOA-Contactlens-hygiene.pdf . [Google Scholar]
- 14.Ghadjari A. Contamination of soft contact lenses and their storage cases with fungi: A problem which causes fungal keratitis. Pak J Biol Sci. 2006;9:2927–9. [Google Scholar]
- 15.Rahim N, Bano H, Naqvi B. Sensitivity pattern of bacteria isolated from contact lens wearers in the faculty of Pharmacy, Karachi University student population. Iran J Pharm Res. 2008;7:131–4. [Google Scholar]
- 16.Washington DC: 2000. [accessed on 2011 Mar 25]. Global Health Council. Health Care Workers. Available from: http://www.globalhealth.org/health_systems/health_care_workers/#2 . [Google Scholar]
- 17.Geneva: 2006. [accessed on 2010 Mar 12]. World Health Organization. Global Atlas of Health Workforce. Available from: http://apps.who.int/globalatlas/docs/HRH/HTML/Dftn.htm . [Google Scholar]
- 18.Washington DC: 2008. [accessed on 2010 Mar 12]. American Academy of Ophthalmology. Leading ophthalmology organizations provide FDA with recommendations to improve contact lens product testing and universal lens care guidelines for consumers. Available from: http://www.aao.org/newsroom/release/20080610.cfm . [Google Scholar]
- 19.Gromacki SJ. Standards of contact lens and case hygiene. Rev Cornea Contact Lenses. 2010;147:20–2. [Google Scholar]
- 20.Wu Y, Carnt N, Willcox M, Stapleton F. Contact lens and lens storage case cleaning instructions: Whose advice should we follow? Eye Contact Lens. 2010;36:68–72. doi: 10.1097/ICL.0b013e3181cf8aff. [DOI] [PubMed] [Google Scholar]
- 21.Radford CF, Woodward EG, Stapleton F. Contact lens hygiene compliance in a university population. J Br Lens Assoc. 1993;16:105–11. [Google Scholar]
- 22.Sauer A, Abry F, Berrod JP, Bron A, Burillon C, Chiquet C, et al. [Study and prevention of contact lens-related microbial keratitis with a standardized questionnaire] J Fr Ophtalmol. 2010;33:701–9. doi: 10.1016/j.jfo.2010.09.022. [DOI] [PubMed] [Google Scholar]


