Abstract
Purpose:
To compare the safety and efficacy of trabeculectomy with Ologen implant vs. trabeculectomy with Mitomycin C (MMC).
Materials and Methods:
In a prospective, randomized, pilot study, 39 eyes of 33 subjects with medically uncontrolled primary glaucoma, aged 18 years or above underwent trabeculectomy either with MMC (20 eyes) or with Ologen implant (19 eyes). The primary outcome measure was cumulative success probability, defined as complete if the intraocular pressure (IOP) was > 5 and ≤ 21 mm Hg without anti-glaucoma medications or additional surgery and qualified if an IOP was > 5 and ≤ 21 mm Hg with or without anti-glaucoma medications.
Results:
Mean (± standard deviation) follow-up in Ologen group was 19.1 ± 8.1 months, and in MMC group was 18.0 ± 8.4 months. Mean IOP reduction at 6 months was significantly lower (P = 0.01) in the MMC group (11.9 ± 2.9 mm Hg) as compared to Ologen group (14.6 ± 2.7 mm Hg). However, at 12 months (P = 0.81) and 24 months (P = 0.32), the mean IOP was similar between the 2 groups. Complete success probability at the end of 6 months in Ologen group was 100% (95% confidence interval: 59.1 - 99.0) was similar (P = 0.53) to that in MMC group (93.8%, 95% CI: 63.2 - 99.1). The incidences of early post-operative complications were similar in the 2 groups, except hyphema, which was significantly more in Ologen group (P = 0.02).
Conclusion:
In this pilot study, the success of trabeculectomy and complications were similar in both Ologen and MMC groups at the end of 6 months.
Keywords: Collagen implant, mitomycin C, ologen, trabeculectomy
Trabeculectomy, introduced by Cairns in 1968, remains the standard surgical procedure for the reduction of intraocular pressure (IOP) in patients with medically uncontrolled glaucoma worldwide.[1,2] The reported success rates for primary trabeculectomies range from 67% to 84%.[3,4] However, fibrosis of the sub-conjunctival tissue may lead to bleb failure, decreasing the long term success of trabeculectomy.[5,6,7] With the introduction of adjunctive anti-metabolites, such as 5-fluorouracil (5-FU) and mitomycin-C (MMC), which significantly decrease the post-operative sub-conjunctival scarring, have improved the long term success of trabeculectomy.[8,9,10,11] However, the use of adjunctive anti-metabolites during surgery have increased the incidence of bleb-related complications like thin avascular blebs, hypotony maculopathy, blebitis, and endophthalmitis.[12,13,14]
Ologen (OculusGen Biomedical Inc. Taipei, Taiwan), a biodegradable, porous, porcine, collagen implant, was designed aiming to improve the long term success of trabeculectomy by decreasing the sub-conjunctival scarring but with less bleb-related complications.[15] At the end of the trabeculectomy, the collagen implant is placed sub-conjunctivally over the scleral flap. The implant helps to facilitate the formation of loose connective tissue matrix by acting as a scaffold for growth of fibroblast into the pores of the implant and thus aims to help tissue remodeling and decrease the scar formation. The implant not only acts as a reservoir but also helps to mechanically separate the conjunctiva and episcleral surface and prevent adhesions between them.[15,16]
Collagen implants have been used to modify the sub-conjunctival wound healing process in animal studies during trabeculectomy,[15,16] during non-penetrating glaucoma surgery,[17,18] and during phacotrabeculectomy.[19] In a recent pilot study, comparing trabeculectomy with and without Ologen implant,[20] the authors found no difference in IOP control between the ologen group compared to simple trabeculectomy. In another pilot study, comparing trabeculectomy augmented with MMC and Ologen in 10 Caucasian eyes, showed MMC group to have significantly low IOP compared to Ologen group at the end of 1 year.[21] It is known that the scarring profile and success after trabeculectomy surgery is different in different ethnicities,[22] and hence the purpose of our study was to compare the outcomes of trabeculectomy with Ologen implant against trabeculectomy with MMC in Indian eyes.
Materials and Methods
This was a prospective, randomized, pilot study conducted at L V Prasad Eye Institute between May 2007 and December 2008. The institutional review board approved the study, and all the study procedures adhered to the tenets of the Declaration of Helsinki. All the subjects were explained the benefits and risks of the procedure, the composition, and the source of the collagen implant before obtaining an informed consent. The study subjects included individuals’ ≥ 18 years of age with medically uncontrolled primary open angle glaucoma (POAG) or primary angle closure glaucoma (PACG) with no previous intraocular surgery. POAG was defined in the presence of an IOP > 21 mmHg, open anterior chamber angle on gonioscopy, glaucomatous optic disc damage on clinical examination, and corresponding glaucomatous visual field defects. PACG was defined in the presence of an occludable angle on gonioscopy (posterior trabecular meshwork not seen in at least 180° of the total circumference of the angle in primary position), glaucomatous optic disc damage, and corresponding glaucomatous visual field defects. The IOP was measured using Goldmann Applanation Tonometer, and gonioscopy was performed using a Sussmann's 4 mirror gonioscope under appropriate testing conditions. Optic disc changes that were considered to be glaucomatous were focal or diffuse neuroretinal rim thinning, localized notching or nerve fiber layer defects. Visual field defects were considered glaucomatous if at least 2 of the 3 Anderson's criteria (3 or more non-edged points in a cluster depressed to P < 5% and 1 of which is depressed to P < 1%, Glaucoma Hemifield Test outside normal limits and Pattern Standard Deviation depressed to P < 5%) were fulfilled. Age, gender, type of glaucoma, presence of systemic diseases (diabetes mellitus and systemic hypertension in particular), presenting IOP, highest recorded IOP, number of anti-glaucoma medications and visual field parameters were noted. After enrollment, patients were randomized into 1 of the 2 groups; Trabeculectomy with Ologen implant was group 1 (Ologen group), and trabeculectomy with MMC was group 2 (MMC group). Randomization was done using a permuted block randomization. Block size of 4 was determined, and 2 eyes of group 1 and 2 eyes of group 2 were randomly allocated into each block. All the surgeries were performed by 1 of the 4 experienced surgeons.
Surgical Technique
Under peribulbar anesthesia (Bupivacaine 0.5% + Xylocaine 2%), a superior rectus bridle suture was applied with 4’0 silk and fornix-based conjunctival flap at the superior limbus was dissected. A 4 × 4 mm triangular, partial thickness scleral flap was reflected, a trabeculectomy of 2 × 2 mm was performed using a Vanna's scissors, and a peripheral iridectomy was completed. The scleral flap was closed with single 10-0 Nylon suture at the apex, and conjunctiva was secured with two 8-0 Vicryl wing sutures. The procedure was the same for both the groups, except that the eyes randomized to Ologen group had scleral flap closure with a single apical loose suture (as per the manufacturers recommendation), and a 6 mm × 2 mm Ologen implant was placed on top of the sclera and the conjunctiva was then closed [Fig. 1]. The MMC Group had 4 MMC (0.4 mg/ml) soaked sponges placed sub-conjunctivally over a wide area for 2 minutes (after making the superficial scleral flap). The sponges were removed, and the area was copiously irrigated with 20 cc of ringer lactate. Postoperatively, all patients were treated with prednisolone acetate 1% eye drops in tapering doses over 5 weeks, antibiotic eye drops 4 times-a-day for a week and cyclopentolate 1% eye drops 3 times-a-day for 2 to 3 weeks.
Figure 1.
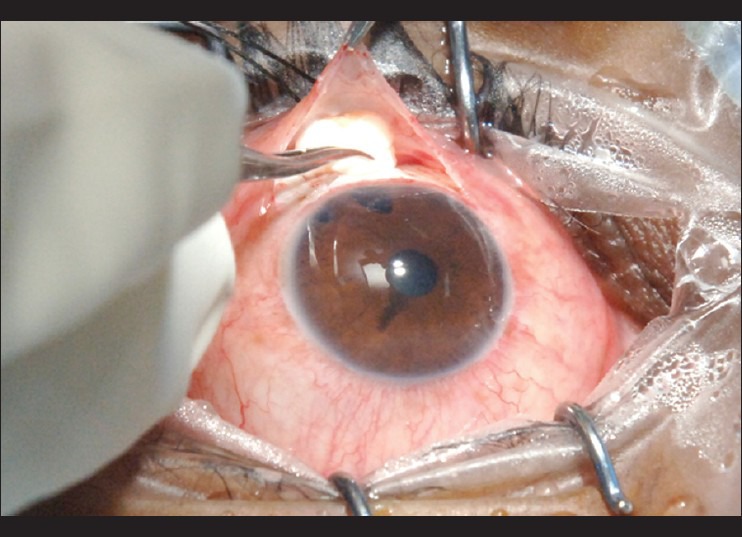
Biodegradable collagen matrix implant positioned directly above the scleral flap. Note the laser peripheral iridotomy at 11’0 clock and a surgical PI at 12’0 clock
Post-operative visits were scheduled at day 1, day 7, 1 month, 3 months, 6 months, and 6-monthly thereafter. At each visit, BCVA, IOP, complications including the need for anti-glaucoma medications were recorded. Primary outcome measure was success, which was defined as complete success if an IOP was > 5 and ≤ 21 mm Hg without any glaucoma medications or re-surgery. Qualified success was defined as IOP ≤ 21 mm Hg with or without anti-glaucoma medications. Secondary outcome measures were number of eyes achieving IOP ≤ 18 mm Hg and ≤ 15 mm Hg in both the groups without anti-glaucoma medications and complications in the 2 groups. Failure was defined as IOP ≥ 22 mm Hg despite medications or ≤ 5 mm Hg (on 2 or more examinations) with hypotony maculopathy or if an additional procedure like needling or repeat trabeculectomy was required to control the IOP or if there was loss of light perception.
Statistical Analysis
Both the study groups were compared using student's t test for continuous variables and Fisher's exact test for discrete variables. Kaplan-Meier survival curves were used to assess cumulative probability of success. Success probabilities between the groups were compared using Mantel-Cox log rank test. Factors predicting failure were assessed using Cox proportional hazard regression model. A P value of ≤ 0.05 was considered statistically significant. Statistical analysis was performed using commercial software (Stata ver. 10.0; StataCorp, College Station, Tx).
Results
We enrolled 39 eyes of 33 subjects into 2 groups: 19 eyes to trabeculectomy with Ologen group and 20 eyes to MMC group. Of these, 7 eyes of 5 patients, who had less than 6 months of follow-up, were excluded from the outcome analysis, but were included in the analysis of complications. For the outcome analysis, there were 16 eyes of 14 patients in trabeculectomy with Ologen group and 16 eyes of 14 patients in trabeculectomy with MMC group. The demographic and clinical features of these patients are summarized in Table 1. All the pre-operative parameters were similar between the 2 groups, except severity of disease at presentation, which was significantly worse in Ologen group, (P = 0.05, mean MD in Ologen group was −22.87 ± 9.04 as compared to −16.43 ± 9.75 in MMC group).
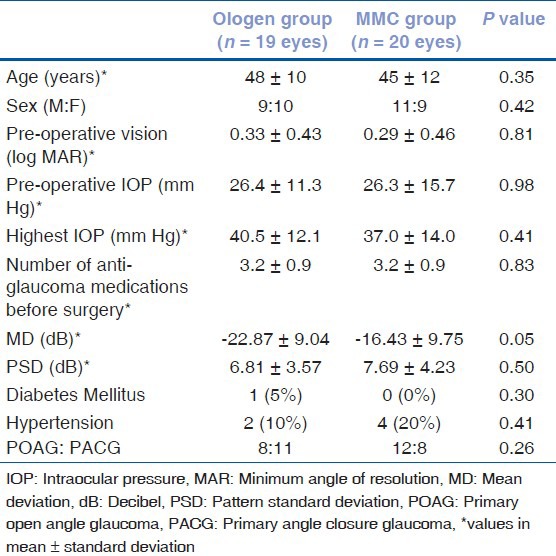
Table 1.
Comparison of demographic and clinical features between the 2 groups
Compared to the pre-operative IOP, the mean IOP after surgery was significantly less at all time points in both the groups (P < 0.05). The post-operative features between the 2 groups are shown in Table 2. The post-operative IOP was similar in the 2 groups at all post-operative visits, except at 1 month and at 6 months where the IOP in the MMC group was significantly lower (P = 0.01) than that in Ologen group. Fig. 2 shows 2 weeks post-operative bleb appearance following trabeculectomy with MMC, and Fig. 3 shows, 2 weeks post-operative bleb appearance with Ologen implant. The IOP reduction (both absolute and percentage) as well as the number of anti-glaucoma medications post-surgery was similar between the 2 groups.
Table 2.
Post-operative features in the ologen and MMC groups
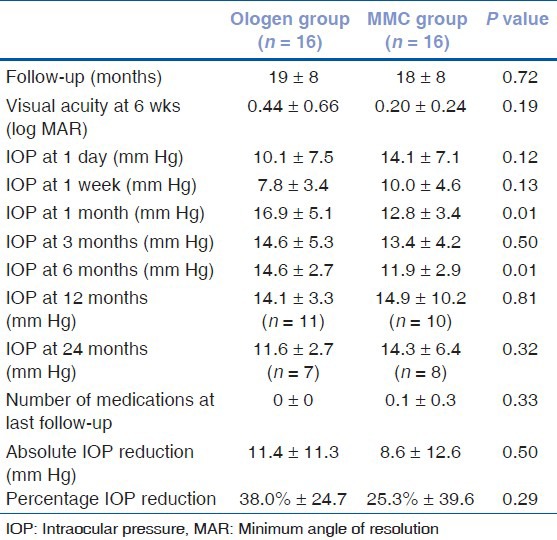
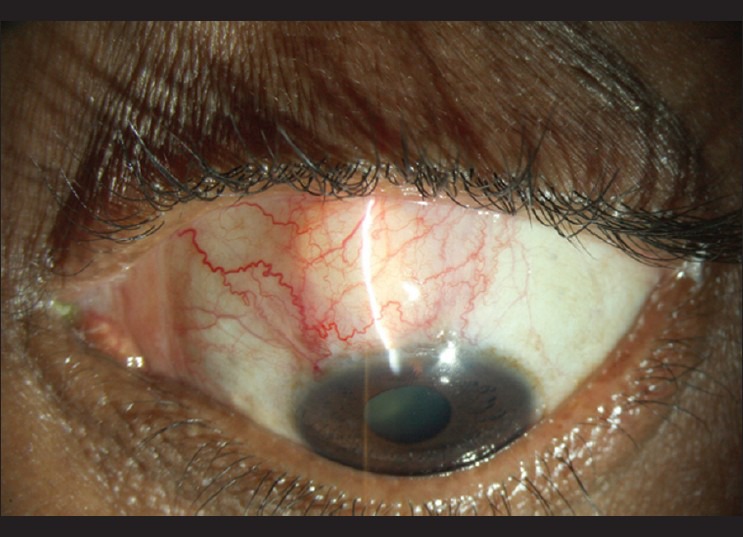
Figure 2.
2-week postoperative slitlamp photograph following trabeculectomy with Mitomycin C, showing a diffuse well formed bleb
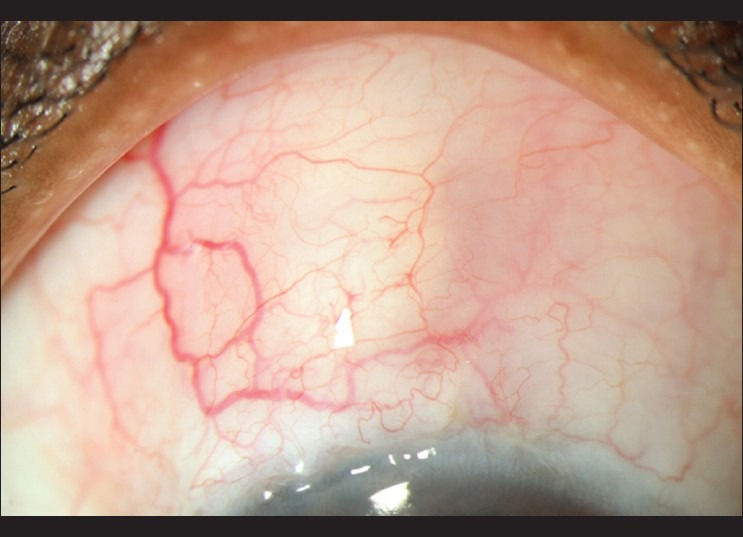
Figure 3.
2-week post-operative slitlamp photograph following trabeculectomy with collagen implant, showing an elevated bleb and sub-conjunctival implant
Probability of success was looked at using Kaplan-Meier graphs [Fig. 4]. Considering complete success criteria, survival probability in Ologen group was 100% at 6 months, 92.9% (95% CI: 59.1 - 99.0) at 12 months, and 82.5% (45.1 - 95.1) at 24 months. The corresponding survival probability in MMC group was 93.8% (63.2 - 99.1) at 6 months and 12 months and 56.3% (13.1 - 85.0) at 24 months. Considering qualified success criteria, survival probability in Ologen group was 100% at 6 months, 92.9% (59.1 - 99.0) at 12 months, and 92.9% (59.1 - 99.0) at 24 months. The corresponding survival probability in MMC group was 100.0% at 6 and 12 months and 83.3% (27.3 - 97.5) at 24 months. The difference in the success rates (complete as well as qualified) was not statistically significantly different (P > 0.5) between the groups. Number of eyes achieving an IOP of less than or equal to 18 mm Hg at 6 months follow-up were similar between the groups (15/16 in Ologen vs. 15/16 in Trab MMC group, P = 1.0, Chi-square test). Number of eyes achieving an IOP of less than or equal to 15 mm Hg at 6 months follow-up were also similar between the groups (10/16 in Ologen vs. 14/16 in Trab MMC group, P = 0.1). Associations between failure and age, sex, highest IOP, severity of visual field damage (MD), number of pre-operative anti-glaucoma medications, presence of systemic hypertension and diabetes mellitus, type of glaucoma, and type of surgery (trabeculectomy with Ologen or MMC) were investigated using Cox proportional hazard regression models. None of the associations were statistically significant (P > 0.05 for all associations).
Figure 4.
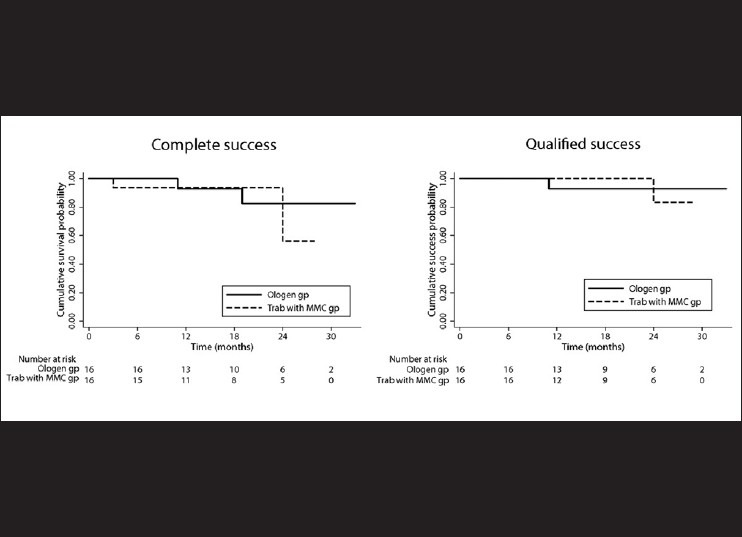
Kaplan-Meier survival analysis showing the survival probability of the 2 groups considering complete (a) and qualified (b) success criteria separately. The number of eyes at risk in both the groups at each time point is given below the graph
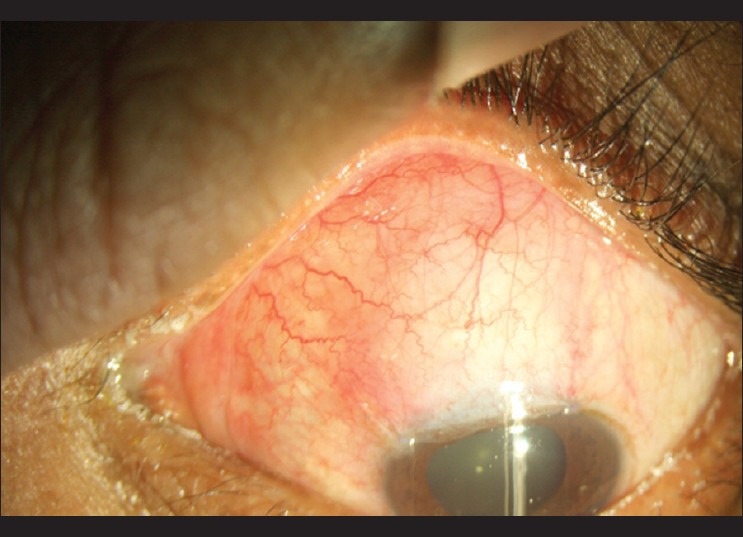
There were no intra-operative complications in any of the eyes in both the groups. The early post-operative complications in the 2 groups are shown in Table 3. The incidences of early post-operative complications were similar in the 2 groups, except hyphema, which was significantly more in Ologen group. The number of eyes, which experienced one or more of the complications, was 12/19 in the Ologen group and 7/20 in the MMC group (P = 0.08). The number needed to experience a complication (Number needed to harm, NNH) was 3.5 (95% Confidence Interval: 1.5, infinity), which means that for every 3.5 eyes treated with Ologen, 1 eye experienced a complication beyond that occurred when MMC was used. However, most of the complications were minor and subsided within 3-4 weeks after surgery (with conservative management) in both the groups, except hypotony in 1 eye in MMC group, which resolved by 8 weeks. None of the eyes in either group required any intervention for the management of early post-operative complication, and none of the eyes lost any lines of visual acuity. Fig. 5 shows partially absorbed Ologen implant at 8 weeks post-operative period.
Table 3.
Early post-operative complications between the 2 groups
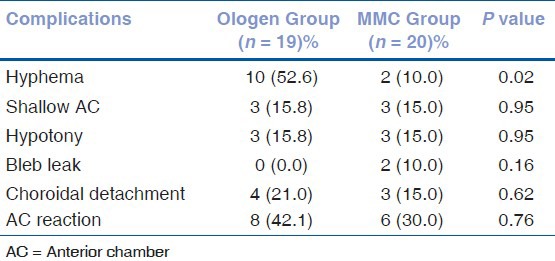
Figure 5.
8-week postoperative slit lamp photograph of an eye with partially absorbed sub-conjunctival collagen implant
Discussion
The higher success rate of trabeculectomy with MMC as compared to simple trabeculectomy has made this procedure a preferred surgical choice for primary glaucoma.[8,9,10,11] However, MMC application is associated with higher long-term bleb-related complications.[12,13,14] Aimed to improve the long-term surgical success of trabeculectomy but with less attendant complications of MMC, Ologen, a bioengineered porcine collagen, has been developed.[15,16]
In this prospective, pilot study, we found the success rate of trabeculectomy at 6 months was similar in eyes with adjunctive MMC use compared to Ologen (100% in the Ologen group and 93.8% in the MMC group, P > 0.5). Although the IOP at 6 months was significantly less in MMC group (P = 0.01), the same trend was not seen during subsequent follow-up visits at 12 and 24 months. The complete and qualified success probabilities were similar between the 2 groups over all these time points. Hence, the results have to be interpreted with caution. Further studies with larger sample size and longer duration of follow-up would be required to come to a meaningful conclusion.
Collagen implants have been used as an adjunct during trabeculectomy to modulate post-operative wound healing in various animal studies with an improved success.[15,16] They have been used along with deep sclerectomy with better long term success,[17,18] and have been used as a spacer following capsule excision after failed GDD surgery.[23]
There are recent reports on the use of Ologen implant during trabeculectomy.
Papaconstantinou et al.,[20] in their pilot study, have compared trabeculectomy with and without Ologen implant. With a 6 month follow-up, and a sample size of 20 eyes in each group, they reported similar success rate of 90% in both the groups, similar to what we have shown in our study.
Rosentreter et al.,[21] compared 10 eyes each in trabeculectomy with MMC and Ologen groups and reported significantly higher complete success rate (IOP ≤ 18 mm Hg and at least 20% reduction of pre-operative IOP) at the end of 12 months in trabeculectomy with MMC group (100% with MMC vs. 50% with Ologen, P = 0.01).
Boey et al.,[19] in their prospective case-control study comparing phacotrabeculectomy with MMC and Ologen implants, have reported significantly greater (P < 0.001) IOP control in MMC group at 3 months follow-up.
We found the post-operative complications to be similar in the 2 groups, except for transient hyphema, which was more in Ologen group. The possible explanation is a loose apical scleral suture, recommended with Ologen implant, would have allowed the ooze from the cut-ends of the sclera to enter into the AC. We did not notice any serious post-operative complications, and none of the eyes needed any 5 FU injection, needling, or re-surgery in our study.
The complications noted in the study by Papaconstantinou et al.[20] were bleb leaks (2 eyes in Ologen group, which resolved on re-suturing), encapsulated blebs (2 eyes in Ologen group and 5 eyes in trabeculectomy group needing 2 to 7 5FU injections), and endophthalmitis (1 eye in the Ologen group).
In the study by Rosentreter et al.,[21] 2 cases in Ologen group developed tenons’ cyst that required needling and 1 case in MMC group needed re-suturing for bleb leak. The other transient complications were similar to our study.
There is a theoretical risk of increased inflammation in eyes with Ologen implant as the implant is non-human (porcine) in origin. Reports in reconstructive surgery have shown an increased inflammation with signs of foreign body reaction related to the porcine cross-linked collagen implants when used in the repair of incisional hernia.[24] There are no such reports when used in ocular procedures, and we did not notice any increase in inflammation in our study, either in the form of increased anterior chamber reaction or hyperemic blebs.
The number of eyes lost to follow-up at 2 years was close to 50%, and this was a limitation of our study. Since our sample size was small, the statistical differences should be interpreted with caution.
A study with higher sample size and a longer follow-up would be required to conclusively evaluate the equivalence or superiority of the collagen implant over MMC augmentation during trabeculectomy.
In summary, from our pilot study, we found that success of trabeculectomy in eyes with MMC was similar to the eyes with Ologen implant. The complication rates were similar in the 2 groups.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66:673–9. [PubMed] [Google Scholar]
- 2.Watson PG, Barnett F. Effectiveness of trabeculectomy in glaucoma. Am J Ophthalmol. 1975;79:831–45. doi: 10.1016/0002-9394(75)90745-x. [DOI] [PubMed] [Google Scholar]
- 3.Mills KB. Trabeculectomy: A retrospective long-term follow-up of 444 cases. Br J Ophthalmol. 1981;65:790–5. doi: 10.1136/bjo.65.11.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sihota R, Gupta V, Agarwal HC. Long-term evaluation of trabeculectomy in primary open angle glaucoma and chronic primary angle closure glaucoma in an Asian population. Clin Experiment Ophthalmol. 2004;32:23–8. doi: 10.1046/j.1442-9071.2004.00752.x. [DOI] [PubMed] [Google Scholar]
- 5.Watson PG, Jakeman C, Ozturk M. The complications of trabeculectomy: A 20-year follow-up. Eye (Lond) 1990;4:425–38. doi: 10.1038/eye.1990.54. [DOI] [PubMed] [Google Scholar]
- 6.Skuta GL, Parrish RK., 2nd Wound healing in glaucoma filtering surgery. Surv Ophthalmol. 1987;32:149–70. doi: 10.1016/0039-6257(87)90091-9. [DOI] [PubMed] [Google Scholar]
- 7.Jampel HD, McGuigan LJ, Dunkelberger GR, L’Hernault NL, Quigley HA. Cellular proliferation after experimental glaucoma filtration surgery. Arch Ophthalmol. 1988;106:89–94. doi: 10.1001/archopht.1988.01060130095036. [DOI] [PubMed] [Google Scholar]
- 8.Bindlish R, Condon GP, Schlosser JD, D’Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy: Five-year follow-up. Ophthalmology. 2002;109:1336–41. doi: 10.1016/s0161-6420(02)01069-2. discussion 41-2. [DOI] [PubMed] [Google Scholar]
- 9.Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol. 2003;48:314–46. doi: 10.1016/s0039-6257(03)00038-9. [DOI] [PubMed] [Google Scholar]
- 10.Beckers HJ, Kinders KC, Webers CA. Five-year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2003;241:106–10. doi: 10.1007/s00417-002-0621-5. [DOI] [PubMed] [Google Scholar]
- 11.Katz GJ, Higginbotham E, Lichter PR, Skuta GL, Musch DC, Bergstrom TJ, et al. Mitomycin C versus 5-fluorouracil in high-risk glaucoma filtering surgery. Extended follow-up. Ophthalmology. 1995;102:1263–9. doi: 10.1016/s0161-6420(95)30875-5. [DOI] [PubMed] [Google Scholar]
- 12.Greenfield DS, Suner IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW., Jr Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114:943–9. doi: 10.1001/archopht.1996.01100140151007. [DOI] [PubMed] [Google Scholar]
- 13.Higginbotham EJ, Stevens RK, Musch DC, Karp KO, Lichter PR, Bergstrom TJ, et al. Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology. 1996;103:650–6. doi: 10.1016/s0161-6420(96)30639-8. [DOI] [PubMed] [Google Scholar]
- 14.Jampel HD, Pasquale LR, Dibernardo C. Hypotony maculopathy following trabeculectomy with mitomycin C. Arch Ophthalmol. 1992;110:1049–50. doi: 10.1001/archopht.1992.01080200029011. [DOI] [PubMed] [Google Scholar]
- 15.Chen HS, Ritch R, Krupin T, Hsu WC. Control of filtering bleb structure through tissue bioengineering: An animal model. Invest Ophthalmol Vis Sci. 2006;47:5310–4. doi: 10.1167/iovs.06-0378. [DOI] [PubMed] [Google Scholar]
- 16.Hsu WC, Ritch R, Krupin T, Chen HS. Tissue bioengineering for surgical bleb defects: An animal study. Graefes Arch Clin Exp Ophthalmol. 2008;246:709–17. doi: 10.1007/s00417-007-0744-9. [DOI] [PubMed] [Google Scholar]
- 17.Shaarawy T, Nguyen C, Schnyder C, Mermoud A. Comparative study between deep sclerectomy with and without collagen implant: Long term follow up. Br J Ophthalmol. 2004;88:95–8. doi: 10.1136/bjo.88.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaarawy T, Mermoud A. Deep sclerectomy in one eye vs deep sclerectomy with collagen implant in the contralateral eye of the same patient: Long-term follow-up. Eye (Lond) 2005;19:298–302. doi: 10.1038/sj.eye.6701469. [DOI] [PubMed] [Google Scholar]
- 19.Boey PY, Narayanaswamy A, Zheng C, Perera SA, Htoon HM, Tun TA, et al. Imaging of blebs after phacotrabeculectomy with Ologen collagen matrix implants. Br J Ophthalmol. 2011;95:340–4. doi: 10.1136/bjo.2009.177758. [DOI] [PubMed] [Google Scholar]
- 20.Papaconstantinou D, Georgalas I, Karmiris E, Diagourtas A, Koutsandrea C, Ladas I, et al. Trabeculectomy with OloGen versus trabeculectomy for the treatment of glaucoma: A pilot study. Acta Ophthalmol. 2010;88:80–5. doi: 10.1111/j.1755-3768.2009.01753.x. [DOI] [PubMed] [Google Scholar]
- 21.Rosentreter A, Schild AM, Jordan JF, Krieglstein GK, Dietlein TS. A prospective randomised trial of trabeculectomy using mitomycin C vs an ologen implant in open angle glaucoma. Eye (Lond) 2010;24:1449–57. doi: 10.1038/eye.2010.106. [DOI] [PubMed] [Google Scholar]
- 22.Wong TT, Khaw PT, Aung T, Foster PJ, Htoon HM, Oen FT, et al. The singapore 5-Fluorouracil trabeculectomy study: Effects on intraocular pressure control and disease progression at 3 years. Ophthalmology. 2009;116:175–84. doi: 10.1016/j.ophtha.2008.09.049. [DOI] [PubMed] [Google Scholar]
- 23.Rosentreter A, Mellein AC, Konen WW, Dietlein TS. Capsule excision and Ologen implantation for revision after glaucoma drainage device surgery. Graefes Arch Clin Exp Ophthalmol. 2010;248:1319–24. doi: 10.1007/s00417-010-1385-y. [DOI] [PubMed] [Google Scholar]
- 24.Petter-Puchner AH, Fortelny RH, Walder N, Mittermayr R, Ohlinger W, van Griensven M, et al. Adverse effects associated with the use of porcine cross-linked collagen implants in an experimental model of incisional hernia repair. J Surg Res. 2008;145:105–10. doi: 10.1016/j.jss.2007.03.090. [DOI] [PubMed] [Google Scholar]


