Abstract
We report three patients with deposition of pseudoexfoliation (PXF) material on intraocular lens years after uneventful cataract surgery. PXF was not present before the cataract surgery. The PXF material was found on the anterior surface of the intraocular lens in the first patient and on the posterior surface as well in the other two patients. All the patients had a polymethylmethacrylate intraocular lens placed in the sulcus. The fellow eyes did not have PXF. All the patients had open angle glaucoma in both eyes.
Keywords: Glaucoma, intraocular lens, pseudoexfoliation, pseudophakos
First demonstrated in 1917 by Lindberg, pseudoexfoliation (PXF) is diagnosed clinically by the appearance of grayish white flaky material on the anterior lens capsule and/or pupillary margin.[1] Various zones of PXF distribution on lens have been described in detail by Sugar.[2] In addition, PXF has been found to be deposited in the zonules, ciliary body, iris, corneal endothelium, angle, anterior vitreous face, and even extraocular sites such as stroma of conjunctiva and blood vessels.[1]
With relation to intraocular lenses (IOL), spontaneous dislocation, anterior capsular contraction with decentration, and tilt of IOL have been reported in patients with PXF.[3,4] Though of rare occurrence, deposition of PXF material on the intraocular lens has been reported.[5,6,7,8,9] We report similar deposition of PXF material on polymethylmethacrylate intraocular lens years after uneventful cataract surgery in three Indian patients.
Case Reports
Case 1
A 70-year-old man presented in January 2011 to our OPD with poor vision in both eyes (BE). He had extracapsular cataract extraction with implantation of a polymethylmethacrylate intraocular lens (PMMA IOL) in left eye (LE) in June 2007 for nuclear cataract. There was no record of PXF noted on the lens surface or pupillary ruff before cataract surgery. On examination, the best-corrected visual acuity (BCVA) was 20/200 in right eye (RE) and no perception of light in LE. The intraocular pressure (IOP) was 42 and 17 mm Hg in RE and LE, respectively. Examination of RE revealed dense nuclear cataract with no PXF and a cup/disc ratio of 0.9. Gonioscopy showed open angles with patchy peripheral anterior synechiae (PAS). In LE, the pupil was dilated and fixed with frosted granular material similar to PXF over the anterior surface of IOL and new vessels on iris were present [Fig. 1]. Fundus examination revealed ischemic central retinal vein occlusion and a total cup. Gonioscopy revealed open angles with no new vessels but heavy pigmentation.
Figure 1.
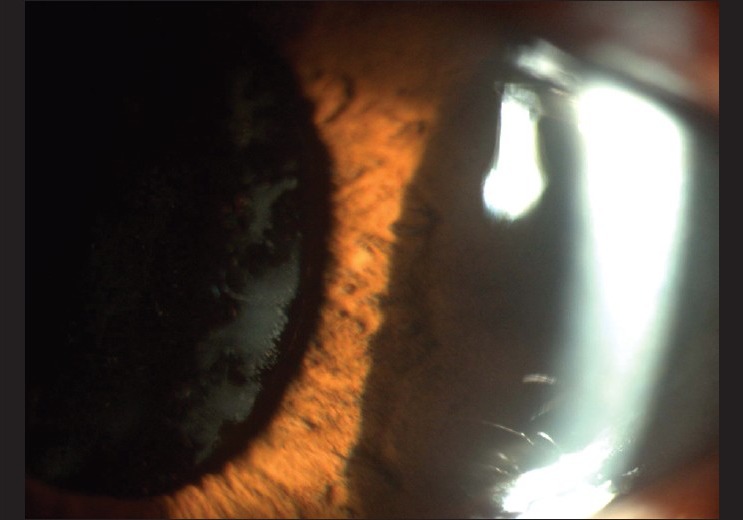
Magnified view showing frosted appearance of PXF on the anterior surface of IOL in Case 1
Case 2
A 65-year-old male presented in May 2008 with a 1-year history of decreased vision in BE. He had primary open angle glaucoma (POAG) and dense cataract. There was no PXF in either eye. Patient had manual small incision surgery with trabeculectomy in BE the same year. The posterior capsules were intact, and rigid PMMA IOL was placed in sulcus. He next turned up in May 2011 for decreased vision in BE. Following dilatation, PXF material was seen on the IOL in LE. This was distributed in a concentric ring as radial striations and on the posterior surface of the IOL where it appeared as multiple granular spots [Figs. 2a and b]. Gonioscopy of LE showed open angles with patchy PAS in the inferior angle and darkly pigmented trabecular meshwork. The IOP was 18 mmHg and the cupping was 0.8. RE had edematous cornea, visual acuity of light perception, and the IOP was 28 mmHg. No other details could be made out.
Figure 2.
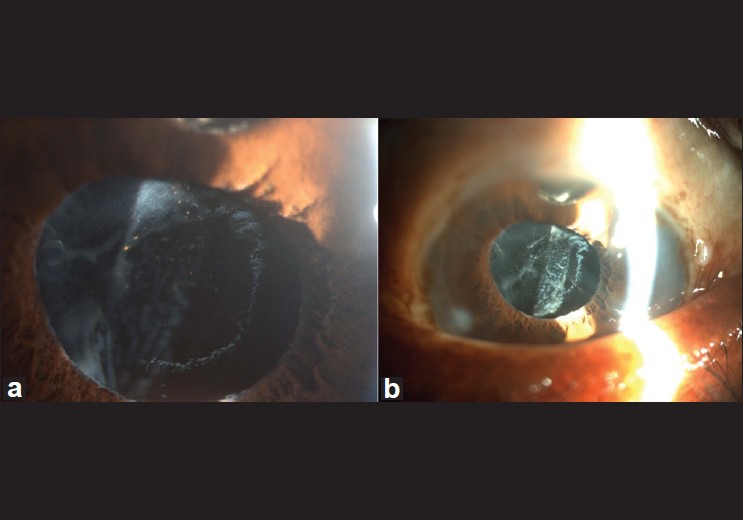
(a) Radial distribution of PXF on the anterior surface of IOL in Case 2. (b) Granular deposits of PXF on posterior surface of IOL in Case 2
Case 3
A 62-year-old male with air-borne contact dermatitis had cataract surgery 10 years ago in BE in our hospital. There was no PXF noted at the time of extracapsular cataract extraction in BE. On examination, BCVA was 20/30 in BE, PXF was noted in LE in pupillary ruff, and on IOL placed in sulcus. PXF was radially distributed nasally on the IOL and as granular dots on the posterior surface [Figs. 3a and b]. RE did not show PXF on pupillary ruff or IOL surface. The IOP in BE were 14 and 12 mmHg, respectively. Fundus examination revealed a cupping of 0.8 and 0.6 in RE and LE, respectively.
Figure 3.
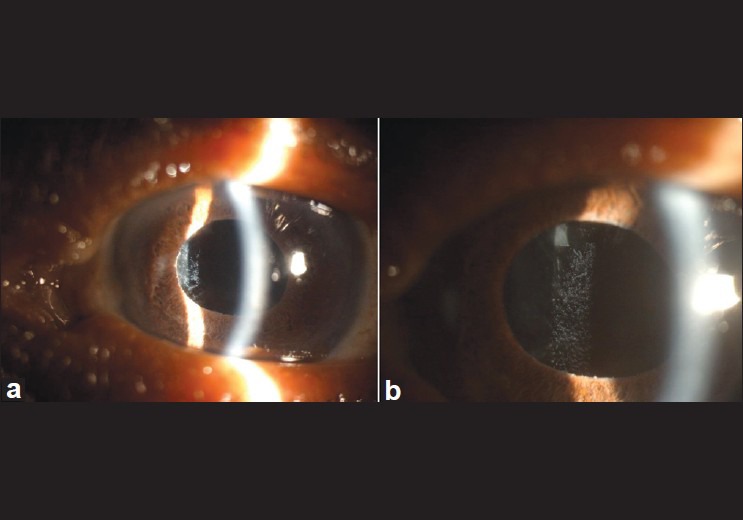
(a) PXF on anterior nasal surface of IOL in Case 3. (b) Dot-like deposits of PXF on posterior surface of IOL in Case 3
Discussion
In the three patients that we report, PXF was not noted before the cataract surgery. Nor did the fellow eyes of the patients have PXF. In Case 1, PXF was noted on the anterior surface of the IOL whereas in Cases 2 and 3, on the anterior and posterior surfaces. Though a rare finding, there are at least five published reports of PXF on IOL in the literature.[5,6,7,8,9] The number may be much more as this entity is generally not looked for in a pseudophakic eye or it could be under-reported. Chen et al. described three cases in which exfoliative material was noted on the posterior surface of IOL.[7] All three cases had an open posterior capsule before PXF was first seen. In all our patients, posterior capsule was intact.
In Case 1, the PXF had a frosted appearance with little granularity but Cases 2 and 3 showed radial distribution on IOL similar to that seen on the crystalline lens. PXF on posterior surface of IOL in two cases appeared as granular dots as described by Park et al. in two of their cases.[8]
All cases had bilateral glaucoma. Incidence of glaucoma in eyes with PXF in Indian patients has been shown to range between 22.6% and 24.1%.[10] In our patients, there was unilateral PXF but bilateral glaucoma which is not uncommon. These are typical presentations of PXF superimposed on POAG. The first two patients were already known cases of POAG on irregular treatment. The third patient however had normal pressures but with moderate cupping. PXF can be clinically evident some years after cataract surgery; it is unknown if a subclinical form could have contributed to the development of the glaucoma.
Stewart et al. reported deposition of PXF on the anterior surface of an acrylic IOL.[5] In our patients, PXF was deposited on PMMA lens. Park et al. had hypothesized that IOL placed in the sulcus stimulates ciliary body surface and production of PXF.[8]
Pseudoexfoliative material produced by one intraocular tissue can be deposited on other structures including a PMMA IOL. The presence of PXF anywhere in only one eye should alert the ophthalmologist in the aggressive management of the glaucoma. To conclude, this case series suggest that PXF could have a role in many more cases of presumed POAG without obvious PXF material on lens surface or pupillary ruff. Follow-up of patients of POAG should include slit-lamp examination even in a pseudophakic eye to look for PXF as it can clinically make its appearance later.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rao VA, Kaliaperumal S. Pseudoexfoliation syndrome-A review. Karnataka J Ophthalmol. 2004;21:11–8. [Google Scholar]
- 2.Sugar HS. The exfoliation syndrome, source of the fibrillar material on the capsule. Surv Ophthalmol. 1976;21:59–64. doi: 10.1016/0039-6257(76)90049-7. [DOI] [PubMed] [Google Scholar]
- 3.Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108:1727–31. doi: 10.1016/s0161-6420(01)00710-2. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi H, Hayashi K, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Br J Ophthalmol. 1998;82:1429–32. doi: 10.1136/bjo.82.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart JF, Jay JL. Pseudoexfoliation material on an intraocular lens. Br J Ophthalmol. 1995;79:1050–2. doi: 10.1136/bjo.79.11.1050-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts MA, Hawksworth NR. Pseudophakic pseudoexfoliation of an AkreosFit intraocular lens. Eur J Ophthalmol. 2009;19:1082–3. doi: 10.1177/112067210901900632. [DOI] [PubMed] [Google Scholar]
- 7.Chen V, Blumenthal M. Exfoliation syndrome after cataract extraction. Ophthalmology. 1992;99:445–7. doi: 10.1016/s0161-6420(92)31955-4. [DOI] [PubMed] [Google Scholar]
- 8.Park K, Kee C. Pseudoexfolaitive material on the IOL surface and development of glaucoma after cataract surgery in patients with pseudoexfolaition syndrome. J Cataract Refract Surg. 2007;33:1815–8. doi: 10.1016/j.jcrs.2007.05.045. [DOI] [PubMed] [Google Scholar]
- 9.Bahadur GG, Masket S. Pseudophakia with pseudo-pseudoexfoliation. J Cataract Refract Surg. 2007;33:1827–8. doi: 10.1016/j.jcrs.2007.06.032. [DOI] [PubMed] [Google Scholar]
- 10.Arvind H, Raju P, Paul PG, Baskaran M, Ramesh SV, George RJ, et al. Pseudexfoliation in South India. Br J Ophthalmol. 2003;87:1321–3. doi: 10.1136/bjo.87.11.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]


