Abstract
PURPOSE
To describe characteristics of systemic lupus erythematosus (SLE) patients who are frequent users of the emergency department (ED) and to identify predictors of frequent ED use.
METHODS
Data for this study were derived from the University of California, San Francisco (UCSF) Lupus Outcomes Study (LOS), a large a cohort persons with SLE who undergo annual structured interviews. Participants were categorized into one of three levels of ED utilization: non-users, if they had no visits in the preceding year, occasional users, if they had 1–2 visits and frequent users if they had 3 or more visits. We compared characteristics of the three groups and determined predictors of frequent ED use (≥3 visits) using multivariate logistic regression, adjusting for a variety of potential confounding covariates.
RESULTS
Of 807 study participants, 499 (62%) had no ED visits; 230 (28%) had occasional ED visits (1–2 visits); and 78 (10%) had frequent (≥3 visits) ED visits. Frequent ED users were younger, less likely to be employed, and less likely to have completed college. They also had greater disease activity, worse general health status, and more depressive symptoms. Frequent ED users were more likely to have Medicaid as their principal insurance. In multivariate logistic regression, older age predicted a lower likelihood of frequent ED visits whereas greater disease activity and having Medicaid insurance predicted a higher likelihood of frequent ED visits.
CONCLUSION
In persons with SLE, greater disease activity and Medicaid insurance are associated with more frequent ED use.
Introduction
Frequently relying on the Emergency Department (ED) for medical care may indicate poor access to primary care1–3, inadequate coordination among health care providers4, 5, and non-adherence to prescribed treatment plans6. Persons with systemic lupus erythematosus (SLE) may be at particular risk of over-relying on the ED; their disease is chronic and complex and often requires coordinated care from primary care physicians, rheumatologists, and various other specialists and health care providers. The disease will often be severe enough that frequent visits to the ED are inevitable. However, certain individuals, unable to sufficiently coordinate the complex care required to manage this condition, may miss the opportunity to receive appropriate preventive care, and seek medical attention only when their disease becomes acute and active. Others simply have inadequate access to primary or specialty care, and may perceive the ED as a more convenient and accessible resource for routine care.
Management of SLE presents several challenges. Persons with SLE are often required to take numerous medications that are costly, difficult to take, and require frequent monitoring. The rate of non-adherence to prescribed treatments is high, particularly among certain ethnic and economically disadvantaged groups7, 8. Furthermore, inadequate access to appropriate preventive care may exacerbate the already difficult issues inherent in SLE care. For example, using the same data source as the current study, Yazdany et al.9 showed that older individuals with SLE and those with lower incomes were less likely to visit a rheumatologist. Ward10 also showed that persons with SLE having these same characteristics (i.e., older and lower income) were more likely to have had avoidable hospitalizations, suggesting that these individuals may have more difficulty accessing care.
An understanding of the characteristics of frequent ED users may help define a vulnerable subgroup of persons with SLE. To our knowledge, frequent use of the ED has not been examined in the rheumatic diseases. A number of studies have assessed frequent ED use in the general population11–21 and in populations with certain chronic conditions, such as asthma22, 23, psychiatric illness24, and illicit drug use11, 25, 26. Many of these studies suggest that frequent users of the ED tend to be both socio-economically disadvantaged and less healthy. A better understanding of frequent ED use among persons with SLE may lead to improvements in the quality of the care they receive, both in the ED and in the outpatient setting, and may help policymakers in the allocation of resources for improved access to needed health care.
In this analysis, we sought to identify persons with SLE who are frequent users of the ED and explore how they differ from non-users and occasional users. Do frequent users differ in demographic or disease characteristics? Do they differ in type of insurance coverage? Are they more or less likely to use other healthcare resources? We analyzed data from the University of California, San Francisco (UCSF) Lupus Outcomes Study (LOS), a large and heterogeneous cohort of individuals with SLE from the United States. Participants were surveyed on various socio-demographic characteristics, health status, SLE history and activity, insurance coverage, as well as ED and other health resource utilization. Predictors of frequent ED use were determined using multivariate analysis.
Methods
Subjects
The UCSF LOS is a large cohort of individuals with SLE from the United States enrolled in an ongoing longitudinal study. Criteria for eligibility and enrollment have been described in detail previously27 and are summarized below. All participants were required to meet American College of Rheumatology (ACR) criteria28, 29 for SLE after chart review by a rheumatologist or a nurse working under a the supervision of a rheumatologist. Participants of the LOS reside in 41 different states, with the majority residing in California (75%), and were recruited from a variety of clinic and community based sources, such as support groups, conferences, and newsletters. Of the original 982 participants enrolled in the first wave of interviews, it was recently determined that 25 did not meet full ACR criteria for SLE. These subjects were excluded from the study, resulting in an original cohort of 957 participants. Data for this study were derived from the second wave of annual interviews, in which 885 (92%) of the original 957 subjects participated. Gender and race are the only variables that derive from the first wave of interviews. In order to avoid potential estimation bias that might arise because of insurance status changes resulting from a visit to the ED (e.g., participant is enrolled in Medicaid while being treated in the ED), the analysis was restricted to participants who had reported the same type of insurance coverage in the baseline and follow-up interviews. This exclusion criterion eliminated 75 of the survey respondents. The 75 subjects that were dropped from the analysis differed from the remaining 810. They were less likely to be employed (17.3% vs. 48.1%) , less likely to be Caucasian (38.7% vs. 60.2%), had higher disease activity, and were more likely to have depressive symptoms. Three subjects were excluded because they did not provide complete ED utilization data, resulting in a final sample of 807 participants. Interviews were conducted between January 2004 and January 2006.
Institutional Review Board Approval
The study protocol was approved by the UCSF Committee on Human Research.
Data
Data were collected by trained survey workers via structured, one-hour telephone interviews. Interviews consist of validated items pertaining to demographic and socioeconomic characteristics, SLE disease activity and manifestations, medications, general health, mental health, cognitive function, employment, health care utilization, and health insurance coverage27.
Measures
Demographic variables
Demographic information collected included age, gender, race/ethnicity, marital status, and education. Race/ethnicity was dichotomized into Caucasian or non-Caucasian (includes African-American, Hispanic/Latino, Asian/Pacific Islander, or other). Marital status was categorized as being currently married or living with a partner versus other. Education was reported as follows: Less than high school, high school graduate, some college, trade or vocational school, college graduate, or post graduate degree.
Disease and general health status
Disease duration was calculated as the number of years since reported diagnosis of SLE. Disease activity was measured using the Systemic Lupus Activity Questionnaire (SLAQ)30, 31, a validated, patient-reported assessment of disease activity in SLE that has been found to correlate with the Systemic Lupus Activity Measure-Revised (SLAM-R)30. Additionally, participants reported on organ system involvement (including renal, pulmonary, and central nervous system) over the preceding year, and on the presence of a SLE flare over the preceding three months. Medical Outcomes Study Short Form-1232 Physical (PCS) and Mental Component Summary (MCS) scores were used to assess physical and mental health status, respectively, and depressive symptoms were assessed by the Center for Epidemiologic Studies – Depression (CESD) scale33.
Health care resource utilization
Participants were queried about their health care resource utilization over the preceding 12 months including number of visits to physicians, by specialty; number of visits to other health care professionals; number and length of acute and long-term care hospitalizations; use of ED services (total visits and visits specifically for SLE); number and type of outpatient surgical procedures; dialysis; and medications. For this report, we chose to include total ED visits, not just visits that the participant attributed to SLE. Given the complexity of the disease, it is often difficult for patients, and even clinicians, to distinguish symptoms that results from SLE versus other conditions.
Insurance Coverage
In the US, most citizens have private insurance to cover medical expenses, most often purchased by employers or acquired independently. Publicly funded insurance is provided to certain individuals, such as the elderly and the disabled (Medicare) and the poor (Medicaid); however, a proportion of the general population (15%) remains uninsured34. Almost all LOS participants (>99%) had some form of health insurance coverage. Participants were queried on the type of their primary insurance coverage and their coverage was categorized as 1) Employer-based (including Veterans Affairs and privately purchased), 2) Medicare, or 3) Medicaid. If a participant had double-coverage with Medicare and Medicaid, they were included in the Medicare group.
Data analysis
Based on the total number of ED visits, we categorized participants into one of three levels of ED use: non-ED users (those with no visits), occasional ED users (1–2 visits), and frequent ED users (≥3ED visits). We then compared the socio-demographic, disease, and health resource utilization characteristics of the three groups. Demographic, disease, and utilization characteristics were expressed using means, standard deviations (SD) and proportions, as appropriate, and one-way ANOVA was employed to identify differences among the three groups. We used univariate and multivariate logistic regression to identify predictors of frequent ED use. Given that only 6 subjects were uninsured, the multivariate analyses were limited to individuals with health insurance. Variables in the multivariate logistic regression models included age, gender, ethnicity (Caucasian versus non-Caucasian), marital status (currently married or living with a partner), education (college degree or higher versus no college), employment status, disease activity (SLAQ score), disease duration, and health status (SF-12 PCS and MCS scores). Certain health care utilization variables, including whether a rheumatologist was the patient’s primary SLE physician, were not included in the final multivariate analysis. Separate analyses (not shown) demonstrated that these variables were not significant predictors and the results of the analyses remained largely unchanged. A variable for hospitalization, which may indicate appropriateness of ED visits, was also not included. Our data did not allow us to identify hospitalizations that were preceded by an ED visit, i.e., a temporal association could not be established. Furthermore, despite a strong and not unexpected correlation between hospitalizations and ED visits, we did not feel that including this variable as a predictor would be appropriate. We assumed that hospitalizations would result from ED visits, rather than ED visits from hospitalizations.
All statistical analyses were performed using SPSS version 16.0 ©.
Results
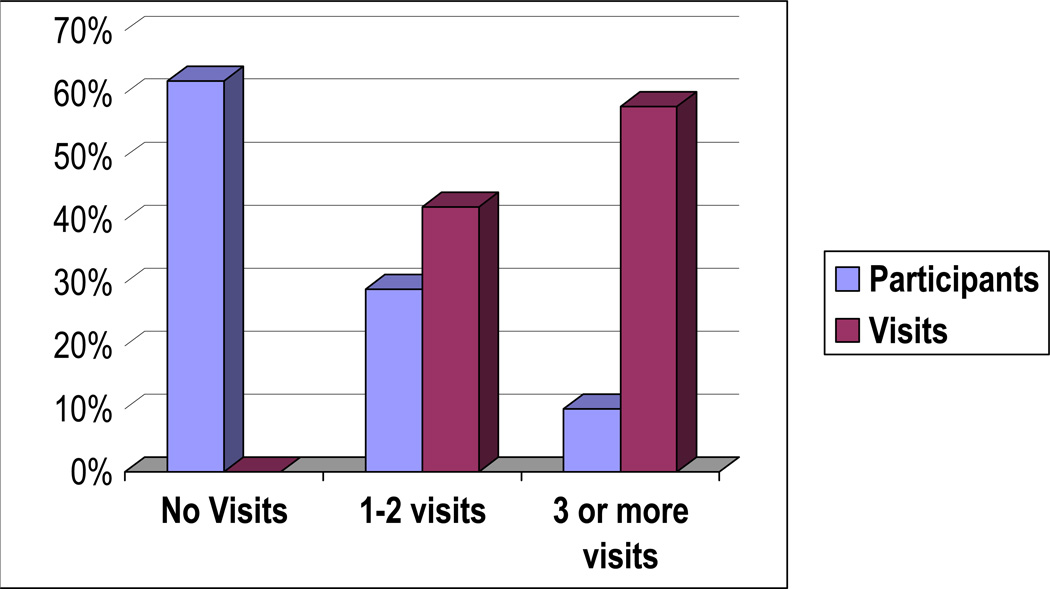
Of a total sample of 807 participants, 61.7% were non-users of the ED, 28.5% were occasional users, and 9.7% were frequent users (Table 1). The 9.7% of the total sample who represented the frequent users accounted for the majority of all ED visits (58.1%). Frequent ED users were younger, with a mean age of 44.5 versus 47.6 (non-users) and 49.0 (occasional users). Frequent ED users were less likely to be married, less likely to be employed and more likely to have incomes below the poverty level than both non users and occasional users. Frequent ED users were also more likely to have higher disease activity (as measured by the SLAQ score) and were more likely to report a disease flare in the three months preceding the interview compared to non users and occasional users. Frequent users had worse general health status (i.e., lower scores on the SF-12 MCS and PCS) and were more likely to have organ system involvement (Table 1). They were also considerably more likely to have scored 16 or higher on the CESD, which suggests possible major depression. Of the frequent users, 65.4% had a CESD score ≥ 16 compared to 30.9% of the non-users and 45.9% of the occasional users.
Table 1.
Demographic and disease characteristics of study participants by ED utilization.
| ED utilization (number of visits) |
||||
|---|---|---|---|---|
| Variables | None (n=499) |
1–2 (n=230) |
≥3 (n=78) |
P Value |
| Percent of total sample | 61.7% | 28.5% | 9.7% | |
| Percent of total ED visits | 0 | 41.9% | 58.% | |
| Demographics | ||||
| Age, mean years (SD) | 47.6 (13.1) | 49.0 (12.5) | 44.5 (11.5) | 0.028 |
| Female, % | 91.6 | 91.3 | 94.9 | 0.581 |
| Caucasian, % | 74.8 | 76.1 | 65.8 | 0.201 |
| Married or living with partner, % | 63.1 | 57.4 | 48.7 | 0.033 |
| Education | ||||
| Less than high school, % | 2.0 | 3.9 | 5.1 | |
| High school graduate, % | 10.6 | 14.8 | 10.3 | |
| Some college, no degree, % | 24.6 | 23.6 | 41.0 | |
| Associate degree/trade or vocational school | 19.4 | 21.4 | 21.8 | 0.009 |
| College graduate, % | 25.3 | 20.1 | 10.3 | |
| Master’s/PhD/Professional degree | 18.0 | 16.2 | 11.5 | |
| Employed, % | 54.1 | 43.0 | 25.6 | <0.001 |
| Below poverty level, % | 9.1 | 14.0 | 27.3 | <0.001 |
| Disease Characteristics | ||||
| Disease duration, mean years (SD) | 13.8 (8.9) | 13.4 (7.7) | 13.8 (8.0) | 0.869 |
| Disease activity (SLAQ), mean score (SD) | 10.9 (7.8) | 13.6 (7.5) | 16.9 (8.8) | <0.001 |
| Flare in last 3 months, % | 42.4 | 51.8 | 54.5 | 0.021 |
| SF-12 | ||||
| MCS-12, mean score (SD) | 49.8 (13.0) | 45.7 (13.0) | 41.2 (14.5) | <0.001 |
| PCS-12, mean score (SD) | 38.0 (6.0) | 36.5 (6.8) | 36.1 (6.2) | 0.002 |
| Renal involvement, % | 15.8 | 24.5 | 43.7 | <0.001 |
| Ever been on dialysis, % | 6 | 8 | 13 | 0.129 |
| Lung involvement, % | 16.2 | 23.5 | 37.3 | <0.001 |
| Pleurisy, % | 22.9 | 32.3 | 48.1 | <0.001 |
| Pericarditis, % | 2.8 | 6.1 | 13.2 | <0.001 |
| Hemoptysis, % | 3.2 | 7.0 | 5.1 | 0.073 |
| CESD, mean score (SD) | 12.9 (12.0) | 16.7 (11.6) | 23.7 (16.2) | <0.001 |
| CESD score 16 or higher, % | 30.9 | 45.9 | 65.4 | <0.001 |
| Medication use | ||||
| Hydroxychloroquine | 56.4 | 55.2 | 60.3 | 0.740 |
| Any DMARD | 29.5 | 29.1 | 41.0 | 0.103 |
| Corticosteroids | 54.2 | 60.7 | 73.1 | 0.004 |
SD: Standard Deviation; DMARD: Disease Modifying Anti-rheumatic Drug; CESD:Center for Epidemiologic Studies Depression Scale; SF-12: Medical Outcomes Study Short Form-12; MCS-12: Mental Component Summary; PCS Physical Component Summary;
Almost all participants had some form of health insurance coverage (Table 2). Frequent users of the ED were less likely to have employer-based insurance (49.3%) compared to 77.1% of the non-users and 65.1% of the occasional users. Frequent ED users were also much more likely to have Medicaid insurance as their primary insurance coverage than their counterparts: 21.3% compared to 3.0% among the non-users and 6.1% among the occasional users. Frequent users of the ED had greater utilization rates of other healthcare resources as well. They were more likely to have visited a general physician than the non-users (but not the occasional users) at least once in the previous year. They also made a greater number of visits to a general physician in the preceding year (8.3 visits versus 3.3 for the non-users and 5.2 for the occasional users). There was no significant difference among the groups either in the proportion having visited a rheumatologist at least once in the preceding year or in the proportion having a rheumatologist as the main doctor for their SLE; however, frequent users made more visits to rheumatologists over the preceding year (5.2) than either non-users (3.5) or occasional users (3.7). Frequent users were much more likely than non-users and occasional users to have been hospitalized in the preceding year (61.0%) compared to 8.8% of non-users and 33.9% of occasional users (Table 3).
Table 2.
Insurance coverage of non-users, occasional users, and frequent users of the ED.
| ED utilization (number of visits) |
||||
|---|---|---|---|---|
| Variables | None (n=499) |
1–2 (n=230) |
≥3 (n=78) |
p Value |
| Have any type of coverage, % | 98.8 | 99.6 | 100 | 0.402 |
| Employer based (including VA and Independent), % | 77.1 | 65.1 | 49.3 | |
| Medicare, % | 19.9 | 28.8 | 29.3 | <0.001 |
| Medicaid, % | 3.0 | 6.1 | 21.3 | |
| HMO, % | 37.0 | 32.0 | 30.1 | 0.290 |
Table 3.
A comparison of health resource utilization in subjects with various degrees of emergency department utilization.
| ED utilization (number of visits) |
||||
|---|---|---|---|---|
| Variables | None (n=499) |
1–2 (n=230) |
≥3 (n=78) |
p Value |
| Outpatient | ||||
| Visited a general MD at least once in past yr, % | 76.2 | 84.8 | 82.1 | 0.023 |
| Visited a rheumatologist at least once in past yr, % | 80.1 | 77.7 | 80.8 | 0.728 |
| Rheumatologist was main doctor managing SLE,% | 74.9 | 71.7 | 70.5 | 0.532 |
| Number of visits to a general MD in past yr | 3.3 (3.7) | 5.2 (8.0) | 8.3 (9.8) | <0.001 |
| Number of visits to a rheumatologist in past yr | 3.5 (3.5) | 3.7 (3.7) | 5.2 (6.9) | 0.002 |
| Number of visits to any specialist in past yr | 10.8 (9.1) | 14.0 (12.5) | 18.7 (17.7) | <0.001 |
| Inpatient | ||||
| Hospitalized at least once in past yr , % | 8.8 | 33.9 | 61.0 | <0.001 |
| Total number of hospital admissions in past yr | 0.1 (0.3) | 0.4 (0.7) | 1.4 (1.7) | <0.001 |
| Total number of nights is hospital in past yr | 0.4 (2.0) | 2.9 (8.3) | 7.5 (15.4) | <0.001 |
Before multivariate adjustment, logistic regression results showed that older age, being married, having a college degree, and having better mental health (i.e., higher MCS-12 scores) predicted a lower likelihood of frequent ED use (Table 4); a higher likelihood of frequent ED use was predicted by greater disease activity (as assessed by the SLAQ), increased depressive symptomatology (as assessed by a score of 16 or higher on the CESD), and having either Medicaid or Medicare insurance. In multivariate analyses, older age still predicted a lower likelihood of frequent ED use, whereas only disease activity (SLAQ score) and having Medicaid insurance remained significant predictors of frequent ED use (Table 4).
Table 4.
Factors associated with ≥3 ED visits in the past year.
| Variables | Unadjusted odds ratios (95% CI) |
Adjusted odds ratios1 (95% CI) |
|---|---|---|
| Demographic | ||
| Age, yr | 0.98 (0.96 1.00) | 0.97 (0.94 0.99) |
| Female | 1.72 (0.61, 4.86) | 0.93 (0.29, 2.92) |
| Caucasian | 0.63 (0.38, 1.06) | 0.83 (0.44, 1.53) |
| Currently married or living with partner | 0.60 (0.38, 0.96) | 0.93 (0.53, 1.65) |
| Education2 | 0.40 (0.23, 0.70) | 0.72 (0.38, 1.36) |
| Employed | 0.34 (0.20, 0.57) | 0.71 (0.37, 1.36) |
| Principal Insurance type | ||
| Employer based | Referent | Referent |
| Medicare insurance | 1.92 (1.10, 3.34) | 1.63 (0.82, 3.24) |
| Medicaid insurance | 7.89 (3.94, 15.81) | 4.37 (1.79, 10.71) |
| Disease characteristics | ||
| Disease activity (SLAQ) | 1.08 (1.05, 1.10) | 1.06 (1.01, 1.10) |
| Disease duration, yr | 1.00 (0.98, 1.03) | 1.03 (0.99,1.06) |
| Depressive symptoms3 | 3.41 (2.09, 5.57) | 1.95 (0.93, 4.09) |
| SF-12 | ||
| MCS-12 | 0.96 (0.95, 0.98) | 1.01 (0.97, 1.04) |
| PCS-12 | 0.97 (0.93, 1.00) | 0.99 (0.94, 1.03) |
CI: Confidence interval, SLAQ: Systemic Lupus Activity Questionnaire
Odds ratio from logistic regression, adjusted for age, gender, race/ethnicity, marital status, education, employment status, poverty status, insurance status, disease activity, disease duration, depressive symptoms, and health status;
College graduate or higher;
Scored 16 or higher on the Center for Epidemiologic Studies Depression Scale (CESD)
Discussion
To our knowledge, this is the first study that characterizes SLE patients who are frequent users of the ED. Individuals with three or more visits to the ED per year were more likely to be younger, unemployed, and living below the poverty level. Frequent ED users also had greater disease activity, were more likely to have had a recent flare, had more SLE organ system involvement, worse health status as measured by the SF-12 and were more likely to have scored high on a depression questionnaire. Frequent ED users also tended to use other healthcare resources more frequently, including general and specialist physician services and, especially, inpatient hospitalizations. When accounting for a variety of factors in a multivariate analysis, only greater disease activity and being on Medicaid independently predicted higher ED utilization. Older age predicted less frequent use.
There is limited data regarding ED utilization among persons with SLE. In a Mexican study6 of 180 SLE patients seen in the ED, Rojas-Serrano showed that the most frequent causes for ED consultation were fever, polyarthralgia, and abdominal pain. Of these 180 patients, 49 required inpatient hospitalization. Hospitalized patients were more likely to be less educated, were less adherent with treatment, had more severe disease, and had higher levels of depressive symptoms. That study excluded repeat visits to the ED and thus did not specifically assess characteristics of frequent ED users. Interestingly, however, those characteristics that were associated with hospitalization (i.e., level of education, severity of disease, and the presence of depressive symptoms) were similar to those that were associated with frequent ED use in our study. Our study also differs in that we used data from a large cohort of persons with a wide spectrum of SLE disease severity, and we included patients who did not visit the ED as well as those who did, allowing us to make comparisons between users and non-users.
Many of the findings in our study are corroborated by findings of frequent ED use in the general population that have shown various socio-demographic characteristics, such as poverty, marital status (being single or living alone), and lower educational level to be associated with frequent ED use19, 20, 35–39. One study, using data from the Community Tracking Study Household Survey19, a nationally representative, population-based study, assessed characteristics of frequent ED users (defined as four or more ED visits) among 45.2 million adults who had visited the ED at least once. Characteristics that were independently associated with frequent use included family income below the poverty threshold and poor physical and mental health. In another study20 of 2,333 ED users, predictors of frequent ED use included being a single parent, being single or divorced, having a high school education or less, and having an income of less than $10,000. Frequent ED users in that study also scored higher on measures of illness severity and tended to be higher users of other healthcare resources. In contrast, older age, which has been shown to predict increased ED use in the general population36 was not a predictor of frequent use in our study; in fact, we found that older age predicted a decreased likelihood of being a frequent ED user. This may reflect greater disease activity among younger participants and/or a greater use of the ED early in the disease course.
A number of studies have assessed frequent ED use among persons with asthma. Asthma and SLE share the propensity to be chronic conditions with unpredictable exacerbations often severe enough to necessitate a visit to the ED. Studies of frequent ED use in persons with asthma have also shown that various socio-demographic factors, in addition to markers of disease severity, are important predictors of frequent ED use. In a large retrospective cohort study of 1,799 asthmatics40, factors associated with frequent ED use included less education and Medicaid insurance. In another multicenter study41, independent predictors of high ED use included non-Caucasian race, Medicaid or other public insurance, being uninsured, and markers of chronic asthma severity. Thus, the characteristics of frequent ED users in the general population, as well as in persons with specific conditions such as asthma, are largely consistent with those found in our study of persons with SLE. These differences in ED use, however, may be amplified in SLE, which disproportionately affects certain socio-economically disadvantaged ethnic minorities. Although comparisons with other patient populations are difficult to make, our finding that frequent ED users, who made up 9.7% of the total sample, accounted for 58% of all ED visits was quite striking. In contrast, in the large population based study described above19, frequent users made up 8% of the study sample, yet accounted for 28% of all ED visits.
It has been suggested that frequent ED use may result from lack of access to primary or specialist care1. In our study, however, we found that frequent ED users with SLE were just as likely or more likely to have seen a primary care physician or a rheumatologist in the previous year and to have made more visits to these physicians. Similar findings have also been reported in several studies of frequent ED users in the general population12, 17, 19, 21. Higher utilization rates should be expected given the greater severity of disease seen in frequent ED users. However, although it appears that this group may have adequate access to care based on frequency of outpatient physician visits, it is important to note that we were not able to assess the timing of these visits with relation to the ED visit. Greater outpatient utilization may simply reflect arrangements made by the ED upon patient discharge rather than the timely, prevention-oriented, outpatient SLE care ideally needed to manage this condition.
Moreover, the number of visits made to a physician only represents one of several factors related to access to care, and may not fully reflect obstacles faced by certain individuals. For example, the persistent finding, in our study and others, of frequent ED use among individuals with Medicaid insurance suggests barriers to care for individuals with this type of coverage. Many providers will simply decline to see Medicaid-insured individuals, while others will not provide appointments in a timely manner or will refuse after-hours visits without a cash copayment42, 43. Using the same data source as this study, Gillis et al.44 showed that Medicaid-insured individuals with SLE traveled longer distances to see a rheumatologist, suggesting barriers to care. Given these difficulties, it is conceivable that persons on Medicaid may forego preventive outpatient visits, see physicians only after it is ‘too late’, or find it preferable to seek care at the ED, which may be perceived as more accessible and less inconvenient.
As with all studies that rely on patient-reported data, recall bias may be a potential limitation. Given that participants in the LOS have had disease of several years duration, survivorship bias may have also influenced the results of our study. Persons with more active and severe disease, who may be expected to be more frequent users of the ED, may not survive long enough to be entered into longitudinal cohorts such as the LOS. Thus, the frequency of ED visits in SLE may have been underestimated due to survivorship bias. Our study would have been strengthened by incorporating more information regarding the ED visit, such as reason for visit, acuity of diagnosis, and disposition. This type of information would give us greater insight into why certain individuals use the ED more frequently than others and should be included in future studies. More information regarding the quality of outpatient preventive care received by participants would also strengthen this study. Furthermore, although we demonstrated a difference in ED utilization in persons with various types of insurance coverage, the LOS does not include enough uninsured individuals to draw conclusions regarding this particularly vulnerable group. In order to better understand how health insurance coverage may influence ED utilization, future studies should also include uninsured individuals. The LOS in general is predominantly Caucasian, relatively well educated, and essentially insured, which may limit generalizability. Inclusion of more minority groups and individuals from across the socioeconomic spectrum would also strengthen this study.
Persons with SLE who are frequent users of the ED represent a vulnerable group of individuals who are socioeconomically disadvantaged and in poorer health. Although the finding of increased ED utilization among those with more severe disease is to be expected, the finding of increased utilization among Medicaid-insured individuals raises important questions regarding access and the provision of adequate outpatient care to these individuals. Addressing the needs of this patient population might help close the gaps in SLE care disparities.
Figure 1.
Proportion of participants in each ED utilization group and corresponding proportion of total ED visits.
Acknowledgement
We would like to acknowledge the following agencies for their support: Canadian Institutes of Health Research Fellowship to Dr. Panopalis; State of California Lupus Fund, Arthritis Foundation, AHRQ/NIAMS 1 RO1 HS013893 and NIAMS P60 ARO53308 to Dr. Yelin; NIH K24 AR02175 and RO1 AR44804 to Dr. Criswell and the Rosalind Russell Medical Research Center for Arthritis. The study was carried out in part in the General Clinical Research Center, Moffitt Hospital, University of California, San Francisco, with funds provided by the National Center for Research Resources, 5 M01 RR-00079, U.S. Public Health Service.
Reference List
- 1.Richardson LD, Hwang U. Access to care: a review of the emergency medicine literature. Acad Emerg Med. 2001;8(11):1030–1036. doi: 10.1111/j.1553-2712.2001.tb01111.x. [DOI] [PubMed] [Google Scholar]
- 2.Petersen LA, Burstin HR, O'Neil AC, Orav EJ, Brennan TA. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998;36(8):1249–1255. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. Jama. 1994;271(24):1909–1912. [PubMed] [Google Scholar]
- 4.Gill JM, Mainous AG, 3rd, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med. 2000;9(4):333–338. doi: 10.1001/archfami.9.4.333. [DOI] [PubMed] [Google Scholar]
- 5.Ionescu-Ittu R, McCusker J, Ciampi A, et al. Continuity of primary care and emergency department utilization among elderly people. Cmaj. 2007;177(11):1362–1368. doi: 10.1503/cmaj.061615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rojas-Serrano J, Cardiel MH. Lupus patients in an emergency unit. Causes of consultation, hospitalization and outcome. A cohort study. Lupus. 2000;9(8):601–606. doi: 10.1191/096120300678828785. [DOI] [PubMed] [Google Scholar]
- 7.Garcia Popa-Lisseanu MG, Greisinger A, Richardson M, et al. Determinants of treatment adherence in ethnically diverse, economically disadvantaged patients with rheumatic disease. J Rheumatol. 2005;32(5):913–919. [PubMed] [Google Scholar]
- 8.Garcia-Gonzalez A, Richardson M, Garcia Popa-Lisseanu M, et al. Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol. 2008 doi: 10.1007/s10067-007-0816-6. [DOI] [PubMed] [Google Scholar]
- 9.Yazdany J, Gillis JZ, Trupin L, et al. Association of socioeconomic and demographic factors with utilization of rheumatology subspecialty care in systemic lupus erythematosus. Arthritis Rheum. 2007;57(4):593–600. doi: 10.1002/art.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward MM. Avoidable hospitalizations in patients with systemic lupus erythematosus. Arthritis Rheum. 2008;59(2):162–168. doi: 10.1002/art.23346. [DOI] [PubMed] [Google Scholar]
- 11.Baker DW, Stevens CD, Brook RH. Determinants of emergency department use: are race and ethnicity important? Ann Emerg Med. 1996;28(6):677–682. doi: 10.1016/s0196-0644(96)70093-8. [DOI] [PubMed] [Google Scholar]
- 12.Blank FS, Li H, Henneman PL, et al. A descriptive study of heavy emergency department users at an academic emergency department reveals heavy ED users have better access to care than average users. J Emerg Nurs. 2005;31(2):139–144. doi: 10.1016/j.jen.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Byrne M, Murphy AW, Plunkett PK, McGee HM, Murray A, Bury G. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med. 2003;41(3):309–318. doi: 10.1067/mem.2003.68. [DOI] [PubMed] [Google Scholar]
- 14.Chan BT, Ovens HJ. Frequent users of emergency departments. Do they also use family physicians' services? Can Fam Physician. 2002;48:1654–1660. [PMC free article] [PubMed] [Google Scholar]
- 15.Fernandes C. Frequent users of emergency department services. Acad Emerg Med. 2005;12(6):575. doi: 10.1197/j.aem.2005.02.002. author reply 6. [DOI] [PubMed] [Google Scholar]
- 16.Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med. 2006;48(1):9–16. doi: 10.1016/j.annemergmed.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Hansagi H, Olsson M, Sjoberg S, Tomson Y, Goransson S. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001;37(6):561–567. doi: 10.1067/mem.2001.111762. [DOI] [PubMed] [Google Scholar]
- 18.Huang JA, Weng RH, Tsai WC, Hu WH, Yang DY. Analysis of emergency department utilization by elderly patients under National Health Insurance. Kaohsiung J Med Sci. 2003;19(3):113–120. doi: 10.1016/S1607-551X(09)70458-9. [DOI] [PubMed] [Google Scholar]
- 19.Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48(1):1–8. doi: 10.1016/j.annemergmed.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 20.Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users. Acad Emerg Med. 2003;10(4):320–328. doi: 10.1111/j.1553-2712.2003.tb01344.x. [DOI] [PubMed] [Google Scholar]
- 21.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 22.Castro M, Zimmermann NA, Crocker S, Bradley J, Leven C, Schechtman KB. Asthma intervention program prevents readmissions in high healthcare users. Am J Respir Crit Care Med. 2003;168(9):1095–1099. doi: 10.1164/rccm.200208-877OC. [DOI] [PubMed] [Google Scholar]
- 23.Ford JG, Meyer IH, Sternfels P, et al. Patterns and predictors of asthma-related emergency department use in Harlem. Chest. 2001;120(4):1129–1135. doi: 10.1378/chest.120.4.1129. [DOI] [PubMed] [Google Scholar]
- 24.Chaput YJ, Lebel MJ. Demographic and clinical profiles of patients who make multiple visits to psychiatric emergency services. Psychiatr Serv. 2007;58(3):335–341. doi: 10.1176/ps.2007.58.3.335. [DOI] [PubMed] [Google Scholar]
- 25.Kerr T, Wood E, Grafstein E, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health (Oxf) 2005;27(1):62–66. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- 26.Ottaway CA, Erickson PG. Frequent medical visits by cocaine-using subjects in a Canadian community: an invisible problem for health practitioners? J Subst Abuse Treat. 1997;14(5):423–429. doi: 10.1016/s0740-5472(97)00017-2. [DOI] [PubMed] [Google Scholar]
- 27.Yelin E, Trupin L, Katz P, et al. Work dynamics among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57(1):56–63. doi: 10.1002/art.22481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 29.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25(11):1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 30.Karlson EW, Daltroy LH, Rivest C, et al. Validation of a Systemic Lupus Activity Questionnaire (SLAQ) for population studies. Lupus. 2003;12(4):280–286. doi: 10.1191/0961203303lu332oa. [DOI] [PubMed] [Google Scholar]
- 31.Yazdany J, Yelin EH, Panopalis P, Trupin L, Julian L, Katz PP. Validation of the systemic lupus erythematosus activity questionnaire in a large observational cohort. Arthritis Rheum. 2007;59(1):136–143. doi: 10.1002/art.23238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Measurement. 1977;1:385–401. [Google Scholar]
- 34.Dubay L, Holahan J, Cook A. The uninsured and the affordability of health insurance coverage. Health Aff (Millwood) 2007;26(1):w22–w30. doi: 10.1377/hlthaff.26.1.w22. [DOI] [PubMed] [Google Scholar]
- 35.Okuyemi KS, Frey B. Describing and predicting frequent users of an emergency department. J Assoc Acad Minor Phys. 2001;12(1–2):119–23. [PubMed] [Google Scholar]
- 36.Murphy AW, Leonard C, Plunkett PK, et al. Characteristics of attenders and their attendances at an urban accident and emergency department over a one year period. J Accid Emerg Med. 1999;16(6):425–427. doi: 10.1136/emj.16.6.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rask KJ, Williams MV, McNagny SE, Parker RM, Baker DW. Ambulatory health care use by patients in a public hospital emergency department. J Gen Intern Med. 1998;13(9):614–620. doi: 10.1046/j.1525-1497.1998.00184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCusker J, Healey E, Bellavance F, Connolly B. Predictors of repeat emergency department visits by elders. Acad Emerg Med. 1997;4(6):581–588. doi: 10.1111/j.1553-2712.1997.tb03582.x. [DOI] [PubMed] [Google Scholar]
- 39.Lucas RH, Sanford SM. An analysis of frequent users of emergency care at an urban university hospital. Ann Emerg Med. 1998;32(5):563–568. doi: 10.1016/s0196-0644(98)70033-2. [DOI] [PubMed] [Google Scholar]
- 40.Pines JM, Buford K. Predictors of frequent emergency department utilization in Southeastern Pennsylvania. J Asthma. 2006;43(3):219–223. doi: 10.1080/02770900600567015. [DOI] [PubMed] [Google Scholar]
- 41.Griswold SK, Nordstrom CR, Clark S, Gaeta TJ, Price ML, Camargo CA., Jr Asthma exacerbations in North American adults: who are the"frequent fliers" in the emergency department? Chest. 2005;127(5):1579–1586. doi: 10.1378/chest.127.5.1579. [DOI] [PubMed] [Google Scholar]
- 42.Skaggs DL, Clemens SM, Vitale MG, Femino JD, Kay RM. Access to orthopedic care for children with medicaid versus private insurance in California. Pediatrics. 2001;107(6):1405–1408. doi: 10.1542/peds.107.6.1405. [DOI] [PubMed] [Google Scholar]
- 43.Access of Medicaid recipients to outpatient care. N Engl J Med. 1994;330(20):1426–1430. doi: 10.1056/NEJM199405193302007. [DOI] [PubMed] [Google Scholar]
- 44.Gillis JZ, Yazdany J, Trupin L, et al. Medicaid and access to care among persons with systemic lupus erythematosus. Arthritis Rheum. 2007;57(4):601–607. doi: 10.1002/art.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]