Abstract
Contraction and relaxation of the detrusor smooth muscle (DSM), which makes up the wall of the urinary bladder, facilitates the storage and voiding of urine. Several families of K+ channels, including voltage-gated K+ (KV) channels, Ca2+-activated K+ (KCa) channels, inward-rectifying ATP-sensitive K+ (Kir, KATP) channels, and two-pore-domain K+ (K2P) channels, are expressed and functional in DSM. They control DSM excitability and contractility by maintaining the resting membrane potential and shaping the action potentials that determine the phasic nature of contractility in this tissue. Defects in DSM K+ channel proteins or in the molecules involved in their regulatory pathways may underlie certain forms of bladder dysfunction, such as overactive bladder. K+ channels represent an opportunity for novel pharmacological manipulation and therapeutic intervention in human DSM. Modulation of DSM K+ channels directly or indirectly by targeting their regulatory mechanisms has the potential to control urinary bladder function. This Review summarizes our current state of knowledge of the functional role of K+ channels in DSM in health and disease, with special emphasis on current advancements in the field.
Introduction
The physiological functions of the urinary bladder are to store and periodically release urine, facilitated by the contraction and relaxation of the detrusor smooth muscle (DSM) that comprises the urinary bladder wall.1 DSM expresses a variety of K+ channels that determine DSM excitability and contractility.1–4 The fundamental purpose of the DSM K+ channels is to precisely regulate and fine-tune Ca2+ entry via voltage-gated Ca2+ (CaV) channels, and thus the intracellular Ca2+ concentration that controls DSM contraction and relaxation. Some studies suggest that K+ channels expressed in interstitial cells may also have a role in determining the pattern of DSM spontaneous electrical and contractile activity; however, their particular role in the urinary bladder is less clear compared to in the gut.5–8 This Review focuses on the role of K+ channels expressed in the DSM cell membrane under normal and pathophysiological conditions, and the function of K+ channels at a molecular, single-channel and whole-cell current level, and within isolated DSM tissues, animal models of bladder disease and patients with bladder dysfunction.
K+ channels are integral membrane proteins that span DSM cell membranes to form a pore that can be penetrated selectively by K+ ions. The K+ channels are the largest and most diverse group of ion channels, represented by about 80 different genes encoding the pore-forming channel subunits as well as many additional genes encoding regulatory subunits.9,10 Several families of K+ channels, including voltage-gated K+(KV) channels, Ca2+-activated K+ (KCa) channels, inward-rectifying ATP-sensitive K+ (Kir, KATP) channels, and two-pore-domain K+ (K2P) channels, are expressed and functional in DSM cells (Figure 1). The K+ channels have a critical role in maintaining the DSM cell resting membrane potential, illustrated by the negative equilibrium potential for K+. In general, the opening of K+ channels causes cell membrane hyperpolarization, limits Ca2+ entry via L-type CaV channels and causes DSM relaxation. By contrast, inhibition of DSM K+ channels leads to membrane depolarization and activation and opening of L-type CaV channels, causing DSM contraction. DSM exhibits spontaneous action potentials,2,5,11–16 which determine the phasic (rhythmic) nature of the spontaneous contractions in this tissue.5,16–24 Ca2+ entry via L-type CaV channels is responsible for the initial depolarization phase of the DSM action potential (Figure 2) and leads to an increase in global intracellular Ca2+, which activates DSM phasic contractions.14,25,26 The K+ channels shape the DSM cell’s action potential by delivering repolarization after the initial episode of depolarization. Figure 2 illustrates the specific role of various K+ channels in shaping the DSM resting and action potentials, and, subsequently, DSM phasic contractions. The DSM phasic contractions can be abnormally increased under pathophysiological conditions of detrusor overactivity (DO), overactive bladder (OAB), and related urinary incontinence.1,2,24,27–34 The importance of K+ channels in DSM excitability and contractility suggests that K+ channel defects, alterations or mutations, also known as channelopathies,9,10 may cause certain forms of bladder pathologies.
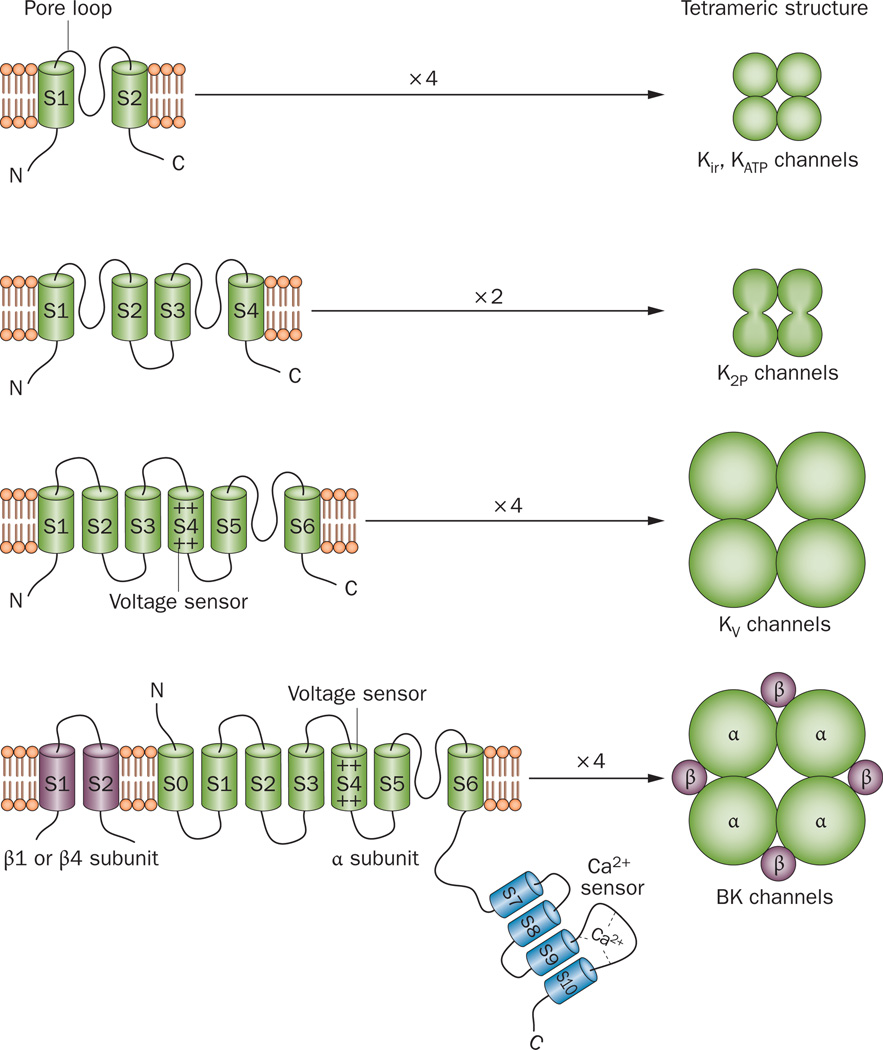
Figure 1.
Illustration of the transmembrane architecture and subunit stoichiometry of the K+ channel types expressed in detrusor smooth muscle cells. Kir channels (represented by the KATP channel) have the simplest K+ channel structure, with two transmembrane segments (S) connected by a pore loop. Four such subunits form a functional tetrameric channel pore. K2P channels form a tetrameric pore structure from two subunits each containing two pore loops. KV channel subunits have six transmembrane segments with a voltage sensor in the S4 transmembrane domain. BK channels consist of four pore-forming α-subunits and the four regulatory β1 or β4 subunits. Abbreviations: BK channels, large-conductance voltage-activated and Ca2+-activated K+ channels; K2P channels, two-pore-domain K+ channels; KATP channels, inward-rectifying ATP-sensitive K+ channels; Kir channels, inward-rectifying K+ channels; KV channels, voltage-gated K+ channels.
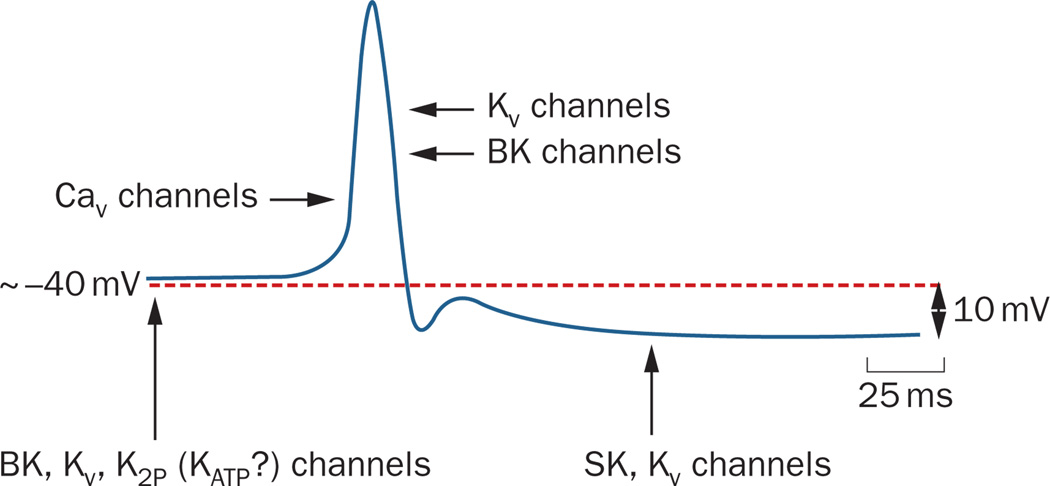
Figure 2.
Schematic illustration of the detrusor smooth muscle action potential and the roles of various K+ channels in determining resting membrane potential and action potential. BK, KV, K2P, and probably KATP channels determine the resting membrane potential. BK and KV channels contribute to the initial repolarization phase of the action potential. SK and KV channels contribute to the prolonged after-hyperpolarization phase of the action potential. Abbreviations: BK channels, large-conductance voltage-activated and Ca2+-activated K+ channels; CaV channels, voltage-gated Ca2+ channels; K2P channels, two-pore-domain K+ channels; KATP channels, inward-rectifying ATP-sensitive K+ channels; KV channels, voltage-gated K+ channels; SK channel, small-conductance Ca2+-activated K+ channel.
Methods for studying DSM K+ channels
The methods for the study of DSM K+ channels range from the measurement of K+ current flow through a single K+ channel to investigation of K+ channel function in whole-animal experiments, including the use of animal models of bladder disease as well as genetically engineered mouse models with either altered K+ channel structure, or a lack or overexpression of a particular K+ channel subtype. In general, most standard molecular and cell biology techniques have been applied to study K+ channels in DSM. Currently, an established procedure exists to develop and utilize K+-channel-specific antibodies for immunocytochemistry and western or northern blot analyses, or to perform reverse transcription PCR (RT-PCR). A recent advancement in DSM K+ channel research is the application of a single-cell RT-PCR technique to identify K+ channel gene transcripts in single, freshly isolated DSM cells while avoiding contamination with non-DSM cells.18,22,35–37 However, truly direct assessment of K+ channel activity can only be achieved via patch-clamp electrophysiology;38 all other approaches and methods of studying DSM K+ channel activity are indirect.
Erwin Neher and Bert Sakmann received the Nobel Prize in Physiology or Medicine in 1991 for their discoveries concerning the function of single ion channels in cells using the patch-clamp technique. The patch-clamp method allows the recording of single K+ channel currents as well as K+ currents from a whole cell.10,38 The first patch-clamp recordings of K+ channels in freshly isolated DSM cells were conducted by Gerrit Isenberg’s group in the mid-1980s,39 followed by a series of studies by several laboratories, including my group at the University of South Carolina.17,22,23,30,36,37,40,41 The development of the perforated patch-clamp technique42 has allowed us to study K+ channel function and regulation while maintaining the native environment of the DSM cells, thereby preserving the regulatory and signal transduction pathways.17,22,23,43 The electrophysiological techniques, as well as functional studies on whole animals or isolated DSM strips and whole bladders, can be combined with pharmacological approaches when the K+ channel is tested by various K+ channel inhibitors or activators. The latter are often referred to as ‘K+ channel openers’. Figure 3 illustrates hypothetical pharmacological dissection of DSM whole-cell K+ currents recorded by the perforated patch-clamp technique in response to a voltage-step depolarization similar to the depolarization that occurs during an action potential (Figure 2). Another common technique for studying the role of K+ channels uses isometric DSM tension recordings (contractility) of isolated DSM strips in combination with K+ channel pharmacological modulators.16–18,22–24
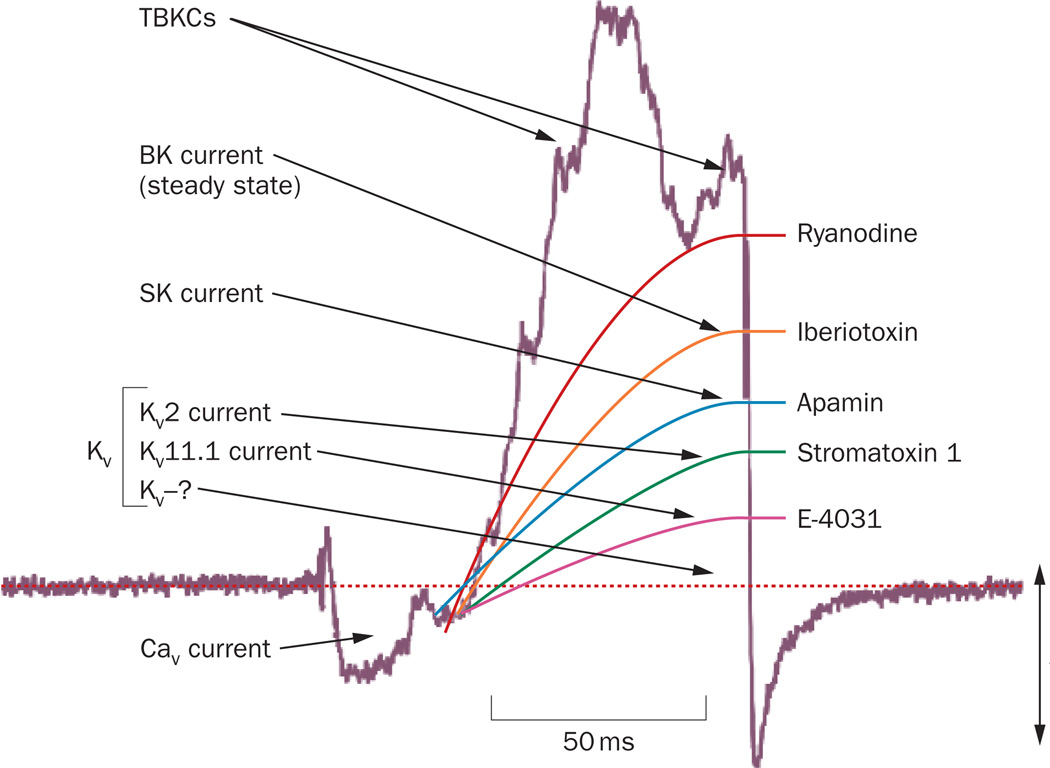
Figure 3.
Hypothetical pharmacological dissection of KCa and KV currents in detrusor smooth muscle cells using various K+ channel-selective inhibitors. The current trace is an original patch-clamp recording of a whole-cell current from a guinea pig detrusor smooth muscle cell elicited in response to depolarization voltage-step. The initial inward L-type CaV current provides Ca2+ for the activation of the KCa currents. Ryanodine is an inhibitor of the ryanodine receptor, iberiotoxin is a BK channel inhibitor, apamin is an SK channel inhibitor, stromatoxin 1 is a KV2 channel inhibitor, and E-4031 is a KV11.1 channel inhibitor. Abbreviations: BK, large-conductance voltage-activated and Ca2+-activated K+ channel; CaV, voltage-gated Ca2+ channels; KCa, Ca2+-activated K+ channel; KV, voltage-gated K+ channel; SK, small-conductance Ca2+-activated K+ channel; TBKCs, transient BK currents.
The ability to genetically manipulate the mouse genome by deleting or overexpressing specific genes encoding K+ channel subunits allows us to evaluate the significance of certain K+ channel gene products and to study their functional effects from the cellular level to the whole-animal level. The mouse has become the model of choice for genetic engineering, due to its short gestation cycle, low maintenance costs, the relative ease of introducing foreign genetic material into their genomes, and the extensive literature on mouse genetics. One limitation to the K+ channel genetic ablation approach, however, is the problem of developmental compensation, in which protein products of other (usually closely related) genes functionally substitute for a deleted gene, resulting in the absence of obvious phenotypic abnormalities. For example, genetic deletion of the BK channel (also known as the Maxi-K channel, KCa1.1, KCNMA1, or slo) causes protein kinase A (PKA) overexpression to compensate for the channel loss.17,44 One interesting transgenic animal model possesses a tetracycline-based genetic switch and can either overexpress or suppress a particular K+ channel, the SK3 channel, depending on orally administered doxycycline.21 The effects of K+ channel modulators can also be examined at the whole-organ level by conducting urodynamic measurements in animal models of bladder disease.21,28,45,46
DSM K+ channel families
Structurally, all DSM K+ channels form a pore-loop and can have a 2, 4, 6, or 7 transmembrane segment (S) architecture (Figure 1). Functionally, the K+ channels form four major families: KV channels with 6S transmembrane architecture; KCa channels with 6S or 7S transmembrane architecture; Kir, KATP channels with 2S trans-membrane architecture; and K2P channel family with 4S transmembrane architecture.
Voltage-gated K+ channels
Of all the K+ channels that control DSM excitability and contractility, the KV channel family is the most diverse, with pronounced variations in their mechanisms of activation and inactivation. In DSM cells, KV channels work to repolarize the membrane potential to end an action potential, and also have a role in setting the resting membrane potential.13,25,36,37,47 In the human genome, the KV channel family is represented by 40 genes classified into 12 subfamilies based on their amino acid sequence homology (Table 1); each KV gene encodes a pore-forming α-subunit, four of which form a functional KV channel tetramer (Figure 1).10,48,49 The KV channels use a unique nomenclature in which the number after the KV indicates the gene subfamily (KV1–KV12) and the number after the dot indicates the individual K+ channel member (KV1.1, KV1.2, and so on). Splice variant isoforms are indicated by lowercase letters at the end (KV1.1a, KV1.1b, and so on).48,49 The Ca2+-activated (KCa1–KCa5), inwardly rectifying (Kir1–Kir7), and K2P (K2P1–K2P15) channels, described below, use the same classification system.48
Table 1.
Nomenclature and commercially available pharmacological inhibitors and activators of functional KV channels
| Channel | Human gene | Inhibitors (antagonists or blockers) | Activators (agonists or openers) |
|---|---|---|---|
| Kv1.1 | KCNA1 | Dendrotoxin K, dendrotoxin I, resiniferatoxin, kaliotoxin 1, margatoxin, hongotoxin 1, agitoxin 2, mast cell degranulating peptide, maurotoxin, stichodactyla toxin, flecainide | None |
| Kv1.2 | KCNA2 | Tityustoxin Kα, hongotoxin 1, maurotoxin, noxiustoxin, resiniferatoxin, dendrotoxin K, dendrotoxin I, charybdotoxin, flecainide | None |
| Kv1.3 | KCNA3 | Agitoxin 1, agitoxin 2, OSK1 (α-KTx3.7), margatoxin, kaliotoxin 1, hongotoxin 1, maurotoxin, noxiustoxin, charybdotoxin, resiniferatoxin, stichodactyla toxin, CP339818, UK78282, Psora-4, cromakalim, flecainide | None |
| Kv1.4 | KCNA4 | UK78282, CP339818, riluzole, quinidine | None |
| Kv1.5 | KCNA5 | Mephetyl tetrazole, DPO-1, riluzole, S9947, resiniferatoxin, flecainide, clofilium, bupivacaine, propafenone, quinidine | None |
| Kv1.6 | KCNA6 | Agitoxin 2, α-dendrotoxin, hongotoxin 1, charybdotoxin, mast cell degranulating peptide, stichodactyla toxin | None |
| Kv1.7 | KCNA7 | Margatoxin, resiniferatoxin, noxiustoxin, stichodactyla toxin, flecainide, amiodarone, quinidine, CP339818 | None |
| Kv1.8 | KCNA10 | Charybdotoxin, ketoconazole, pimozide | cGMP |
| Kv2.1 | KCNB1 | Hanatoxin, stromatoxin 1, heteroscodratoxin 1, heteroscodratoxin 2, 2,3-butanedione monoxime | Linoleic acid |
| Kv2.2 | KCNB2 | Stromatoxin 1, quinine | None |
| Kv3.1 | KCNC1 | BDS-I, BDS-II, resiniferatoxin, flecainide, riluzole, fluoxetine, cromakalim | None |
| Kv3.2 | KCNC2 | BDS-I, BDS-II, stichodactyla toxin | None |
| Kv3.3 | KCNC3 | Tetraethylammonium (nonselective), 4-aminopyridine (nonselective) | None |
| Kv3.4 | KCNC4 | BDS-I, BDS-II | None |
| Kv4.1 | KCND1 | Heteroscodratoxin 1 | None |
| Kv4.2 | KCND2 | Phrixotoxin 1, phrixotoxin 2, stromatoxin 1, heteroscodratoxin 1, heteropodatoxin 2, quinidine | None |
| Kv4.3 | KCND3 | Phrixotoxin 1, phrixotoxin 2, bupivacaine, heteroscodratoxin 1 | NS5806 |
| Kv7.1 | KCNQ1 | Chromanol 293B, JNJ303, mefloquine, XE991, linopiridine | L-364373, mefenamic acid, niflumic acid |
| Kv7.2 | KCNQ2 | XE991, linopiridine, DMP543 | Retigabine, BMS204352, flupirtine, diclofenac |
| Kv7.3 | KCNQ3 | XE991, linopiridine, DMP543 | Retigabine, BMS204352, flupirtine, diclofenac |
| Kv7.4 | KCNQ4 | XE991, linopiridine, DMP543, bepridil | Retigabine, BMS204352, flupirtine, diclofenac |
| Kv7.5 | KCNQ5 | XE991, linopiridine, DMP543 | Retigabine, BMS204352, flupirtine |
| Kv10.1 | KCNH1 | E4031, clofilium, terfenadine, astemizole, cisapride, dofetilide, quinidine | None |
| Kv10.2 | KCNH5 | Quinidine | None |
| Kv11.1 | KCNH2 | BeKm-1, ergtoxin, dofetilide, cisapride, terfenadine, halofantrine, E-4031, astemizole | NS1643, PD118057, ICA-105574 |
| Kv11.2 | KCNH6 | Ergtoxin, BeKm-1 | None |
| Kv11.3 | KCNH7 | Ergtoxin, BeKm-1, sertindole, pimozide | None |
| Kv12.1 | KCNH8 | Ba2+ (nonselective) | None |
| Kv12.2 | KCNH3 | CX4, Cs+ (nonselective) | None |
| Kv12.3 | KCNH4 | Ba2+ (nonselective) | None |
KV5, KV6, KV8, and KV9 are not listed in the table because they are electrically silent and do not form their own homotetramers. Instead, they combine with the KV2 channel family to form new heteromultimeric KV channels. Abbreviations: BDS, blood depressing substance; KV, voltage-gated K+ channel.
KV1–KV4, KV7, and KV10–KV12 form homotetrameric KV channels (Figure 1), whereas KV5, KV6, KV8, and KV9 do not make their own homotetramers but rather form heterotetrameric KV channels with the KV2 subunits. Splice variance, post-translational modification, and a large variety of accessory KV subunits further diversify the KV channel family.10,50 Expression of KV1.3 and KV1.6 channels has been shown in human DSM,51 and low expression of KV1.2 and KV1.5 has been reported in rat DSM.52 Expression of KV2.1 and KV2.2 channels has been demonstrated in rat DSM; KV2.1 seems to be the predominant channel subtype.18,52,53 In mouse DSM, the KV2.1 subunit associates with electrically silent subunits (KV5.1, KV6.1, KV6.2 or KV6.3), forming ‘KV2.1/X’ hetero-tetramers.47 Similar to rat DSM,18 human DSM cells express KV2.1 and KV2.2 channels along with the electrically silent KV9.1 subunit.36 Guinea pig DSM expresses KV2.1 (but not KV2.2) and the electrically silent subunits KV6.2, KV6.3, KV8.2, and KV9.1–KV9.3, indicating marked species differences.37 Human, rat and guinea pig DSM does not express the KV4.2 channel, which mediates the fast A-type KV current.18,36,37
The functional role of KV channels in DSM remains controversial.13 The reason for this controversy has been the lack of subtype-specific KV channel inhibitors, which has hampered the study of these channels in DSM cells. All KV channels are inhibited nonselectively by tetra-ethylammonium (TEA), and most of them by 4-amino-pyridine,10,12,25,47 but these inhibitors do not allow dissection of individual KV channel subtypes. In the past decade, emerging highly specific KV channel inhibitors, most of them toxins isolated from venomous species, have enabled researchers to selectively isolate KV channel subtypes and determine their contribution to complex physiological processes in different tissues (Table 1).10 We can now use these same pharmacological tools to identify individual KV channel subtypes and determine their functional role in DSM. One such example is the spider venom peptide stromatoxin 1, which is a highly specific inhibitor of the KV2.1, KV2.2 and KV4.2 homotetramers, as well as KV2.1/6.3 and KV2.1/9.3 hetero-tetramers.54,55 This toxin has allowed us to reveal that KV2 homotetrameric and hetertetrameric channels contribute to the electrical and contractile activity of rat, guinea pig and human DSM.18,36,37 Studies from Karl-Erik Andersson’s group showed that retigabine, an activator of KV7 channels (also known as KCNQ channels), increased micturition volume and voiding intervals and, when given intravesically, decreased capsaicin-induced DO.46 In rat isolated DSM strips, retigabine reduced both pharmacologically induced and nerve-evoked DSM contractions, effects that were reversed by XE991, a KV7 channel inhibitor.56 McCloskey’s group also identified KV7 channels in cells isolated from DSM wall.8 Data for guinea pig DSM,26 along with data from our group for rat DSM (G. V. Petkov, unpublished data), show that E4031, a specific inhibitor of the Kv11.1 channel (also known as ERG1, hERG, or KCNH2), increases DSM contractility, indicating a functional role for this K+ channel. The role of KV channels in DSM pathophysiology remains largely unexplored. Decreased mRNA expression of the KV2.1 channel in a rat model of DSM hyper-reflexia induced by spinal cord injury has been reported,53 but this study lacked sufficient quantitative evaluation to support such a finding.
The structural diversity of the KV channels contributes to the variety of their pharmacological properties and makes them potentially attractive targets for pharmacological treatment in bladder diseases.18,27,50 However, substantial gaps in our knowledge exist regarding the cellular and functional roles, expression, and regulation of different subtypes of KV channels in DSM. Thus, further molecular, patch-clamp, and functional studies characterizing the KV channels, particularly in human DSM, are urgently needed. Future investigations in this area may lead to the development of selective pharmacological or genetic therapies for OAB.4,50
Ca2+-activated K+ channels
In DSM, the KCa channel family is represented by three major groups, which are classified based on their single channel conductance: large-conductance voltage-activated and Ca2+-activated K+ (BK) channels; small-conductance Ca2+-activated K+ channels (SK1–SK3); and intermediate-conductance Ca2+-activated K+ (IK) channels. SK and IK channels are Ca2+-activated but voltage-insensitive.
BK channels
The BK channel is highly expressed in DSM,22,24,35 and is arguably the most important physiologically relevant K+ channel that regulates DSM function.13,14,17,19,20,22,24,32,34,43,44,57,58 This importance arises from the fact that the BK channel is the only member of the K+ channel family that is activated by both voltage and Ca2+, so is uniquely suited to serve as a Ca2+–voltage signal integrator in the modulation of membrane excitability.10 These channels have a single-channel conductance of 100–250 pS, hence the names ‘big K+’ or ‘Maxi-K’ channel. BK channels are selectively blocked with high affinity by the scorpion venoms iberiotoxin and charybdotoxin59 and the Penicillium mycotoxin paxilline.60
Depending on the experimental conditions, DSM single BK channel conductance varies from 122 pS to 244 pS in guinea pigs,14,61 170–200 pS in rats and humans,62 214 pS in mice24 and 136 pS in humans.22 The BK channels are highly dense in guinea pig DSM cells (~21 channels per µm2).63 The BK channel’s pore-forming α-subunit has the structure of the KV channel’s α-subunit with the addition of an S0 transmembrane segment (providing a 7S transmembrane architecture) and a long intracellular domain (S7–S10) at the C-terminus containing the Ca2+ sensor (Figure 1). In addition to the pore-forming α-subunits, the BK channels may also contain one of the four known tissue-specific regulatory subunits (BKβ1–BKβ4), with BKβ1 being smooth-muscle-specific and BKβ4 neuron-specific. Although BKβ1 is the primary auxiliary subunit in DSM,24 recent studies at both mRNA and protein levels have also identified the presence of BKβ4 in rat, mouse and human DSM22,35,64 and confirmed the absence of BKβ2 and BKβ3 subunits.22,35 Data obtained from BKβ1-knockout mice indicate that the BKβ1 subunit increases the apparent Ca2+ and voltage sensitivities of BK channels.24 Genetic deletion of the BKβ1 subunit significantly decreases single BK channel open probability, causing DO.24
Whereas the BKβ1 subunit has a key physiological role in bladder function,24 the function of the recently discovered BKβ4 subunit in DSM is less clear.22,35,64 In DSM from a rat model with partial urethral obstruction (PUO), BKβ4 subunit expression decreases gradually with increasing PUO severity.64 Under the pathological conditions of PUO, DSM exhibits increased phasic contractions as BKβ4 subunit expression decreases.64 Pharmacological blockade of BK channels increases the amplitude and duration of spontaneous action potentials, indicating that the repolarization phase of the DSM action potential is mediated by BK channel activity.13,14,65 Blocking the BK channel with iberiotoxin depolarizes the resting membrane potential in both isolated DSM cells and intact DSM tissue.14,22,23 Genetic deletion of the BK α-subunit in mice causes sustained membrane depolarization in DSM cells.17,44 Collectively, these findings indicate that BK channels control the resting membrane potential in both rodent and human DSM (Figure 2).
In DSM of humans and various other species, pharmacological inhibition of DSM BK channels also increases the amplitude, duration and force of the spontaneous phasic contractions, as well as DSM tone.19,22,24,26,33,59,66 Pharmacological inhibition or genetic deletion of the BK channel enhances the nerve-evoked contractions in mouse, rat, guinea pig, and human DSM isolated strips.22,34,44,67,68 On the other hand, well established (such as NS1608, NS8 and NS1619) and novel (such as NS11021) BK channel openers increase BK channel open probability and whole-cell BK currents, causing DSM hyperpolarization and relaxation in various species.26,29,33,58,61,62,69,70
Ca2+ is an important regulator not only of DSM contractility, but also of the BK channels. In DSM, BK channel activation depends on both Ca2+ entry through L-type CaV channels and Ca2+ release from the ryanodine receptors (RyRs) of the sarcoplasmic reticulum (SR).20,22,23,43,57 BK channels are under the local control of so-called ‘Ca2+ sparks’, caused by highly localized Ca2+ releases from the RyRs (Figure 4). The suggestion that Ca2+ sparks have a role in smooth muscle relaxation through local BK channel activation, causing transient BK currents (TBKCs; also known as spontaneous transient outward currents [STOCs]) (Figure 3), was first proposed by Mark Nelson’s group in 1995.71 In guinea pig DSM, BK channels and RyRs co-localize at junctional areas of the cell membrane and SR, where Ca2+ sparks originate to trigger TBKCs.57,63 In DSM cells, the Ca2+ sparks and related TBKCs are effectively inhibited by ryanodine (Figures 3 and 4).17,20,22,43,57 The physiological role of Ca2+ sparks and related TBKCs, which contribute to setting the resting membrane potential, has been revealed in DSM of various animal species20,23,43,57,63 and more recently in human DSM.22
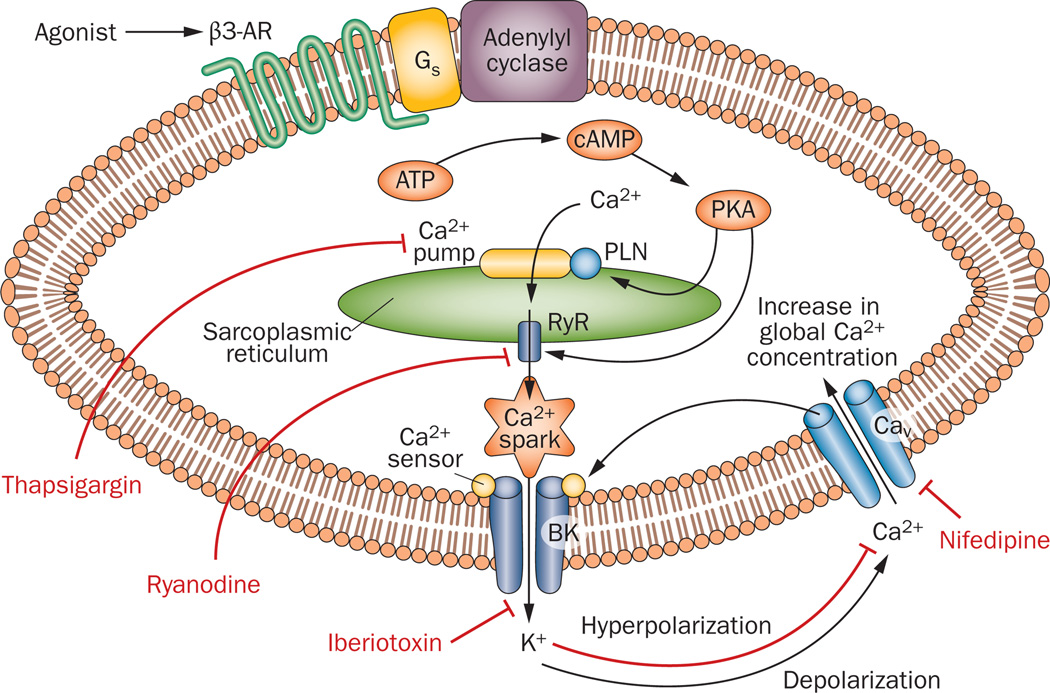
Figure 4.
Schematic illustration of the functional coupling between the β3-AR and the BK channel in a detrusor smooth muscle cell. The BK channels control the opening and closing of the L-type CaV channels by depolarizing or hyperpolarizing the cell membrane, thus regulating the global Ca2+ influx and spontaneous phasic contractions. BK channels are activated by localized Ca2+ signals (‘Ca2+ sparks’) caused by Ca2+ release from the RyRs of the SR, adjacent to the cell membrane. Stimulation of the β3-AR with selective agonists leads to PKA activation, PLN phosphorylation, and activation of the SR Ca2+-pump and RyRs, which causes an increase in Ca2+ spark and TBKC activity. The increased TBKC frequency results in a sustained membrane hyperpolarization, closure of the L-type CaV channels, reduction in the global Ca2+ concentration, and detrusor smooth muscle relaxation. When Ca2+ sparks are blocked with ryanodine and/or thapsigargin (an SR Ca2+-pump inhibitor), the functional coupling between β3-ARs and BK channels is disrupted. Abbreviations: β3-AR, β3 adrenergic receptor; BK channel, large-conductance voltage-activated and Ca2+-activated K+ channel; PKA, protein kinase A; PLN, phospholamban; RyR, ryanodine receptor; SR, sarcoplasmic reticulum; TBKC, transient BK current.
Not long ago, our knowledge about the presence and function of the BK channel in human DSM was very limited and based on several scattered studies.25,62,66,72 A large, multidisciplinary approach, including both single-channel and whole-cell patch-clamp recordings on freshly isolated human DSM cells from 53 patients without history of OAB, has now provided the first systematic identification and characterization of the BK channel in native human DSM.22
In DSM, stimulation of β-adrenergic receptors (β-ARs) increases intracellular cAMP concentration, which activates PKA that, in turn, phosphorylates specific proteins resulting in DSM relaxation (Figure 4).1,5,17,15 Compelling evidence suggests that BK channels are activated by stimulation of β-ARs to promote relaxation of guinea pig, rat and mouse DSM.17,23,43,73 PKA stimulation has been shown to activate Ca2+ sparks in guinea pig DSM.43 PKA-induced phosphorylation of phospholamban (PLN) activates the SR Ca2+-pump and elevates SR Ca2+ load; thus, RyRs and Ca2+ spark activity in DSM cells (Figure 4). Inhibition of the BK channel with iberiotoxin in wild-type mouse DSM significantly reduces β-AR-mediated and PKA-mediated DSM relaxations in response to isoprenaline and forskolin, respectively.17 Paradoxically, DSM from BK α-subunit knock-out mice showed enhanced sensitivity to isoprenaline and forskolin,17 indicating that compensatory mechanisms in the β-AR– cAMP–PKA signal transduction pathway might partially overcome the permanent loss of BK channels in β-AR-mediated relaxation, even though the BK channel is a critical element of DSM excitability and contractility. These findings are also supported by a follow-up study in which an alternative BK α-subunit knock-out mouse model was used.44 β-AR agonists can also modulate K+ conductance in human DSM.72 As β3-AR and BK channels are functionally coupled at the RyR level to mediate relaxation of rat DSM (Figure 4),23 alterations in this functional coupling might be involved in the pathophysiology of OAB. These findings support the concept that selective β3-AR agonists might be effective drugs for controlling urinary bladder function.23
The overall physiological function of the BK channel is to reduce membrane excitability and oppose both myogenic and neurogenic human DSM contractions.22 Disrupting this function would lead to increased DSM contractility and DO. Indeed, increasing evidence collected during the past decade suggests that alterations in BK channel expression, regulation or function have very important implications for normal and abnormal bladder physiology. Also, the BK channel seems to be the most likely candidate involved in DO etiology. BK channel inhibition with iberiotoxin increases DSM excitability,14 and analogous increases in DSM excitability are caused by experimental PUO.74 In addition, BK channel inhibition with iberiotoxin leads to increased DSM contractility,17,19,22,23,26,33,59 which resembles DSM behavior after PUO. One study showed that DSM strips, isolated from 38 patients with neurogenic DO, consistently showed no response to iberiotoxin or the BK channel opener NS1619, indicating BK channel dysfunction in these patients.33 Furthermore, BK channel activity is reduced in patients with neurogenic OAB, leading to increased DO in combination with reduced iberiotoxin-sensitive currents, as shown by combined patch-clamp and DSM contractility studies.30 DSM cells from rats with experimental PUO also show decreased BK channel expression and reduced iberiotoxin-sensitive currents, indicating decreased BK channel activity.75
Expression of RyR, which provides negative feedback regulation of the BK channel to control normal DSM contractility (Figure 4), is decreased in DSM from rats with experimental PUO.31 DSM cells of RyR2 knockout mice have decreased TBKC frequency, resulting in a depolarized membrane potential and DO.76 Thus, changes in BK channel regulatory mechanisms, such as RyR, might be implicated in the pathogenesis of DO and OAB.31,76 OAB prevalence is well known to increase with age,27 and our unpublished observations indicate that BK channel expression decreases with age (G. V. Petkov, unpublished data), consistent with findings that aging reduces membrane BK channel density in coronary and corporal smooth muscle.77,78 Decreased BK channel expression has been reported in patients with benign prostatic hyperplasia and associated DO, as well as in rabbits with PUO-induced DO.29 Genetic deletion of the BKβ1 or pore-forming BK α-subunits also leads to DO.17,24,32,34,44 In rats, overexpression of the BK α-subunit using gene transfer techniques eliminated DO caused by PUO,79 consistent with the opposite phenomenon (increased DSM contractility) observed in knock-out mice lacking BK channel subunits.17,24,32,34,44 BK channel gene transfer is in a phase I clinical trial for treatment of erectile dysfunction, and a similar trial is planned for OAB.80–83 Thus, the BK channel represents a novel opportunity for therapeutic intervention in human DSM.
SK channels
The SK channels (also known as KCa2 channels) have a single-channel conductance of 5–20 pS,10 and structurally resemble the KV channels but are voltage-insensitive. SK channels, regulated by Ca2+ and calmodulin,84 contribute to the DSM action potential after the hyperpolarization phase.11,12,25 These channels have a low density in guinea pig DSM cells (~0.01 SK channels per µm2 or ~50 SK channels per cell).20 The low SK channel density, along with their pronounced Ca2+ sensitivity, uniquely suits these channels as sensors for changes in global Ca2+ induced by activation of L-type CaV channels during the DSM action potential. Apamin, a peptide from bee venom, blocks all of the three known SK channel subtypes (SK1–SK3 [also known as KCa2.1–KCa2.3]) with high potency (Figure 3), and increases DSM contractility.12,19–21,26,40,41,66,67,85 In a conditional knock-out mouse model, overexpression of the SK3 channel elevated SK currents, which increased bladder capacity and decreased the frequency of DSM phasic contractions in vitro, whereas suppression of SK3 channel expression significantly increased the frequency of DSM phasic contractions in vitro and nonvoiding contractions in vivo.21 Studies in SK2 knock-out mice suggest that SK2 channels are another essential contributor to DSM function.85
Pharmacological activation of SK channels with specific openers might be a novel approach to restoring normal DSM function. Urodynamic studies in rats showed that NS309, a potent SK/IK channel activator, increases bladder capacity and decreases voiding frequency.45 NS4591, another SK/IK channel activator, inhibits carbachol-induced DSM contractions in vitro86 and bladder overactivity in vivo.87 In 2009, Heike Wulff ‘s group at the University of California at Davis designed SKA-31, a new SK/IK channel opener, which is the most potent and selective activator of SK and IK channels known to date.88 A recent study using a combined experimental approach involving single-cell RT-PCR, western blot, perforated whole-cell patch-clamp and DSM contractility recordings indicated that pharmacological activation of SK channels with SKA-31 can reduce the excitability and contractility of guinea pig DSM.41 Moreover, the study established that SK channels, but not IK channels, mediate SKA-31 effects in DSM.41
In essence, SK channels have fundamental roles in regulating DSM action potentials, related phasic contractions and, therefore, bladder function. However, many aspects of the regulatory mechanisms of DSM SK channels remain unknown, and knowledge about the role of SK channels in human DSM function remains limited.25,66,89 Thus, it is necessary to obtain such information directly from human DSM using the patch-clamp technique.
IK channels
IK channels (also known as SK4 or KCa3.1 channels) have single-channel conductance of 20–80 pS,10 and, like SK channels, structurally resemble the KV channels but are also voltage-insensitive. IK channels have been shown to be expressed at the mRNA level in mouse DSM.90 We have also shown mRNA expression of IK channels in native guinea pig DSM using single-cell RT-PCR, and further confirmed IK channel protein expression with western blot analysis.41 Studies using charybdotoxin suggest that IK channels may have a functional role in mouse DSM;13,90 however, such claims require further evidence, as charybdotoxin inhibits both IK and BK channels.59 The discovery of the selective IK channel inhibitor, TRAM-34,91 enabled us to study the functional role of this channel in the DSM. Even at high concentrations (1–30 µmol/l), TRAM-34 does not affect the myogenic and neurogenic contractions of DSM strips isolated from rats, guinea pigs and humans.40,41 Although the IK channel is expressed at the mRNA and protein levels, patch-clamp and functional studies did not confirm a role for IK channels in guinea pig and rat DSM excitability and contractility.40,41
Inward-rectifying ATP-sensitive K+ channels
The Kir channels have inward rectification properties, which refers to the fact that the inward K+ current, under hyperpolarizing conditions (below the K+ equilibrium potential) has a higher amplitude compared to the outward K+ current elicited under equivalent depolarizing conditions.10 In DSM, the Kir channel family is represented by the ATP-sensitive K+ channels (KATP; also known as Kir6 channels), which are composed of four inwardly rectifying K+ channel subunits (Kir6) and four regulatory sulphonylurea receptor subunits, and have single-channel conductance of 11–12 pS.92,93 KATP channels are inhibited by intracellular ATP and by sulphonylurea agents. They are activated when the intracellular ATP concentration is low and the ADP concentration is high, thus linking the cell’s metabolic state with its membrane excitability. The specific KATP channel inhibitor, glibenclamide,16,94,95 does not affect DSM excitability or contractility in the absence of KATP channel stimulation, a finding that questions whether or not KATP channels contribute to DSM resting membrane potential under normal physiological conditions;12,26,93 however, pharmacological activation of KATP channels causes membrane hyperpolarization, which closes the L-type CaV channels, thereby reducing DSM contractility.16 Various chemically unrelated compounds, known as KATP channel openers (such as cromakalim, levcromakalim, pinacidil, diazoxide, ZD6169, P1075 and A-312110) activate DSM KATP channels directly, causing decreased membrane excitability and contractility.4,5,12,16,92–97
The concept of increasing KATP channel opening pharmacologically for the treatment of OAB was first proposed by Karl-Erik Andersson’s group as early as 1988.98 However, the actual discovery of the KATP channel in guinea pig DSM using the patch-clamp technique was first achieved in 1993 by Nelson’s group,99 and, more recently, KATP channels were also identified at a single channel level in pig and human DSM cells.92,93 To date, there is no clear evidence that KATP channelopathies are involved in DO etiology. Indeed, it is doubtful that the KATP channels are involved in bladder pathologies, as DSM strips isolated from various knock-out mouse models lacking different KATP channel subunits show no differences in contractility when compared with DSM strips from mice with functional KATP channels (G. V. Petkov, unpublished data). Thus, it is unlikely that mutations in KATP channels in particular are the cause of DO and OAB. In addition, the pharmaceutical industry has failed to develop bladder-selective KATP channel openers, owing to a lack of DSM specificity.4 Interestingly, the density of KATP channels is significantly higher in DSM compared to other tissues;16,92,95 therefore, one way to achieve bladder-selective effects could be to apply lower doses of KATP channel openers that theoretically would not affect other tissues with lower KATP channel density. Indeed, studies have shown that KATP channels can be significant modulators of the membrane potential in DSM, and that ~1% of the functional KATP channels need to be activated in order to inhibit DSM action potentials and related phasic contractions.16
Two-pore-domain channels
The K2P channels, also known as ‘leak K+ channels’, consist of a pair of 4S transmembrane subunits linked in a tandem dimer that forms a functional channel (Figure 1). In addition to setting the cell’s resting membrane potential (Figure 2), these channels facilitate many other functions, such as stretch, oxygen, pH and temperature sensing.100 A major obstacle in studying the K2P channels has been the lack of selective channel inhibitors. Studies by Sang-Don Koh’s group at the University of Nevada have characterized the functional role of some DSM K2P channels under normal and pathological conditions.28,101,102 pH-sensitive K2P channels of the TASK-1 and TASK-2 subtypes were shown to be expressed and functional in mouse DSM.102 These channels have an important role in stabilizing the DSM cell’s resting membrane potential.102
DSM relaxes during the bladder filling phase to accommodate high bladder capacity while maintaining low intravesical pressure.1 However, the mechanisms responsible for the stabilization of bladder excitability during stretch have been subject to debate. Mouse DSM expresses functional K2P, stretch-dependent K+ channels of the TREK-1 subtype101 that have also been identified in cultured human DSM cells, which show 12-fold higher expression levels compared to cultured aortic myocites.103 BL-1249, a putative TREK-1 channel opener, produces a concentration-dependent membrane hyperpolarization in cultured human DSM cells, inhibits the KCl-induced contractions of rat DSM isolated strips, and decreases the frequency of isovolumic contractions in vivo, without significantly affecting blood pressure in rats.103 These channels may, therefore, have a physiological role in suppressing DSM excitability and contractility in response to stretch during bladder filling. TREK-1 channels are implicated in some bladder pathologies. Systemic administration of l-methioninol, a TREK-1 channel inhibitor, induces nonvoiding contractions during bladder filling.28 In a mouse model of PUO, the DSM TREK-1 channel is downregulated, leading to DO.28 In the future, K2P channels might become important therapeutic targets in bladder dysfunction.
Conclusions
K+ channels control DSM cell excitability by maintaining the resting membrane potential and shaping the action potentials that trigger DSM phasic contractions. Altering DSM K+ channel properties can, therefore, have profound effects on urinary bladder function. Among all K+ channels, the BK, SK and KV channels are the most important physiological regulators of DSM excitability and contractility. As the KV channel family is represented by 40 genes, forming different KV channel homo-multimers or heteromultimers, many new KV channel subtypes with unique roles in DSM function are likely to be discovered. Moreover, such DSM-specific KV channels will represent tissue-selective drug targets.
Evidence collected during the past decade suggests that BK channel dysfunction leads to some forms of DO. A clinical trial is currently underway to examine the effects of infusing a BK channel plasmid as a treatment for OAB, further underscoring the potential utility of BK channel manipulation. Increasing BK channel expression levels can reduce DO; alternatively, targeting the BK, SK or KV channels with synthetic channel-opening agents represents a novel opportunity for pharmacological manipulation of the bladder to reduce DO. Genetic manipulation of K+ channels or the use of channel openers could, in the future, replace the commonly prescribed therapy for OAB—antimuscarinic agents, which currently have limited effectiveness and numerous adverse effects. To facilitate these novel therapeutic approaches, however, we first need to better understand K+ channel functions and regulatory mechanisms in human DSM. Thus, it is necessary for us to obtain further evidence regarding the role of K+ channels in DSM function directly from native human DSM cells in health and disease using a multidisciplinary approach, including the patch-clamp technique, and correlate the electrophysiological findings with patients’ clinical profiles.
Key points.
K+ channels control the excitability and contractility of detrusor smooth muscle (DSM)
Large-conductance voltage-activated and Ca2+-activated (BK) channels, small-conductance Ca2+-activated K+ (SK) channels, two-pore-domain K+ (K2P) channels and voltage-gated K+ (Kv) channels are important regulators of DSM function
BK channelopathy is implicated in some forms of detrusor overactivity and related overactive bladder
BK, SK, K2P and KV channels represent novel targets for pharmacological or gene-therapy-mediated control of DSM function
The Kv channel family is the most diverse; therefore, it is likely that many new DSM KV channels, some of them bladder-specific, are yet to be discovered
Acknowledgments
The author thanks the members of his research group (Drs J. Malysz, K. Hristov, S. Parajuli, W. Xin, Ms A. Smith, Ms R. Soder, Mr S. Afeli and Mr Q. Cheng), as well as Dr J. Schnellmann for the critical evaluation of the manuscript. This work was supported by grants from the NIH (DK084284 and DK083687).
Footnotes
Competing interests
The author declares no competing interests.
References
- 1.Andersson KE, Arner A. Urinary bladder contraction and relaxation: physiology and pathophysiology. Physiol. Rev. 2004;84:935–986. doi: 10.1152/physrev.00038.2003. [DOI] [PubMed] [Google Scholar]
- 2.Brading AF. Spontaneous activity of lower urinary tract smooth muscles: correlation between ion channels and tissue function. J. Physiol. 2006;570:13–22. doi: 10.1113/jphysiol.2005.097311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christ GJ, Hodges S. Molecular mechanisms of detrusor and corporal myocyte contraction: identifying targets for pharmacotherapy of bladder and erectile dysfunction. Br. J. Pharmacol. 2006;147(Suppl. 2):S41–S55. doi: 10.1038/sj.bjp.0706627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gopalakrishnan M, Shieh CC. Potassium channel subtypes as molecular targets for overactive bladder and other urological disorders. Expert Opin. Ther. Targets. 2004;8:437–458. doi: 10.1517/14728222.8.5.437. [DOI] [PubMed] [Google Scholar]
- 5.Hashitani H, Brading AF, Suzuki H. Correlation between spontaneous electrical, calcium and mechanical activity in detrusor smooth muscle of the guinea-pig bladder. Br. J. Pharmacol. 2004;141:183–193. doi: 10.1038/sj.bjp.0705602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCloskey KD. Characterization of outward currents in interstitial cells from the guinea pig bladder. J. Urol. 2005;173:296–301. doi: 10.1097/01.ju.0000141581.00922.f4. [DOI] [PubMed] [Google Scholar]
- 7.McCloskey KD. Interstitial cells in the urinary bladder—localization and function. Neurourol. Urodyn. 2010;29:82–87. doi: 10.1002/nau.20739. [DOI] [PubMed] [Google Scholar]
- 8.McCloskey KD, Anderson UA, Carson C. KCNQ currents and their contribution to resting membrane potential and the excitability of interstitial cells of cajal from the guinea pig bladder. J. Urol. 2009;182:330–336. doi: 10.1016/j.juro.2009.02.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashcroft FM. From molecule to malady. Nature. 2006;440:440–447. doi: 10.1038/nature04707. [DOI] [PubMed] [Google Scholar]
- 10.Petkov GVin. In: Pharmacology: Principles and Practice. Hacker M, Messer WS, Bachmann KA, editors. Academic Press; 2009. pp. 387–427. [Google Scholar]
- 11.Creed KE, Ishikawa S, Ito Y. Electrical and mechanical activity recorded from rabbit urinary bladder in response to nerve stimulation. J. Physiol. 1983;338:149–164. doi: 10.1113/jphysiol.1983.sp014666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujii K, Foster CD, Brading AF, Parekh AB. Potassium channel blockers and the effects of cromakalim on the smooth muscle of the guinea-pig bladder. Br. J. Pharmacol. 1990;99:779–785. doi: 10.1111/j.1476-5381.1990.tb13006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayase M, Hashitani H, Kohri K, Suzuki H. Role of K+ channels in regulating spontaneous activity in detrusor smooth muscle in situ in the mouse bladder. J. Urol. 2009;181:2355–2365. doi: 10.1016/j.juro.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Heppner TJ, Bonev AD, Nelson MT. Ca2+-activated K+ channels regulate action potential repolarization in urinary bladder smooth muscle. Am. J. Physiol. 1997;273:C110–C117. doi: 10.1152/ajpcell.1997.273.1.C110. [DOI] [PubMed] [Google Scholar]
- 15.Nakahira Y;, et al. Effects of isoproterenol on spontaneous excitations in detrusor smooth muscle cells of the guinea pig. J. Urol. 2001;166:335–340. [PubMed] [Google Scholar]
- 16.Petkov GV, Heppner TJ, Bonev AD, Herrera GM, Nelson MT. Low levels of KATP channel activation decrease excitability and contractility of urinary bladder. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;280:R1427–R1433. doi: 10.1152/ajpregu.2001.280.5.R1427. [DOI] [PubMed] [Google Scholar]
- 17.Brown SM;, et al. Beta-adrenergic relaxation of mouse urinary bladder smooth muscle in the absence of large-conductance Ca2+-activated K+ channel. Am. J. Physiol. Renal Physiol. 2008;295:F1149–F1157. doi: 10.1152/ajprenal.00440.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen M, Kellett WF, Petkov GV. Voltage-gated K+ channels sensitive to stromatoxin-1 regulate myogenic and neurogenic contractions of rat urinary bladder smooth muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;299:R177–R184. doi: 10.1152/ajpregu.00036.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrera GM, Heppner TJ, Nelson MT. Regulation of urinary bladder smooth muscle contractions by ryanodine receptors and BK and SK channels. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000;279:R60–R68. doi: 10.1152/ajpregu.2000.279.1.R60. [DOI] [PubMed] [Google Scholar]
- 20.Herrera GM, Nelson MT. Differential regulation of SK and BK channels by Ca2+ signals from Ca2+ channels and ryanodine receptors in guinea-pig urinary bladder myocytes. J. Physiol. 2002;541:483–492. doi: 10.1113/jphysiol.2002.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herrera GM;, et al. Urinary bladder instability induced by selective suppression of the murine small conductance calcium-activated potassium (SK3) channel. J. Physiol. 2003;551:893–903. doi: 10.1113/jphysiol.2003.045914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hristov KL, Chen M, Kellett WF, Rovner ES, Petkov GV. Large conductance voltage- and Ca2+-activated K+ channels regulate human detrusor smooth muscle function. Am. J. Physiol. Cell Physiol. 2011;301:C903–C912. doi: 10.1152/ajpcell.00495.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hristov KL;, et al. Stimulation of β3-adrenoceptors relaxes rat urinary bladder smooth muscle via activation of the large-conductance Ca2+-activated K+ channels. Am. J. Physiol. Cell Physiol. 2008;295:C1344–C1353. doi: 10.1152/ajpcell.00001.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petkov GV;, et al. β1-subunit of the Ca2+-activated K+ channel regulates contractile activity of mouse urinary bladder smooth muscle. J. Physiol. 2001;537:443–452. doi: 10.1111/j.1469-7793.2001.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hashitani H, Brading AF. Electrical properties of detrusor smooth muscles from the pig and human urinary bladder. Br. J. Pharmacol. 2003;140:146–158. doi: 10.1038/sj.bjp.0705319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imai T;, et al. Effects of different types of K+ channel modulators on the spontaneous myogenic contraction of guinea-pig urinary bladder smooth muscle. Acta Physiol. Scand. 2001;173:323–333. doi: 10.1046/j.1365-201X.2001.00908.x. [DOI] [PubMed] [Google Scholar]
- 27.Andersson KE, Wein AJ. Pharmacology of the lower urinary tract: basis for current and future treatments of urinary incontinence. Pharmacol. Rev. 2004;56:581–631. doi: 10.1124/pr.56.4.4. [DOI] [PubMed] [Google Scholar]
- 28.Baker SA;, et al. Role of TREK-1 potassium channel in bladder overactivity after partial bladder outlet obstruction in mouse. J. Urol. 2010;183:793–800. doi: 10.1016/j.juro.2009.09.079. [DOI] [PubMed] [Google Scholar]
- 29.Chang S;, et al. Detrusor overactivity is associated with downregulation of large-conductance calcium- and voltage-activated potassium channel protein. Am. J. Physiol. Renal Physiol. 2010;298:F1416–F1423. doi: 10.1152/ajprenal.00595.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hristov K, Afeli S, Kellett WF, Rovner E, Petkov GV. Neurogenic detrusor overactivity is associated with decreased BK channel activity: electrophysiological and functional studies on human detrusor smooth muscle. J. Urol. 2010;183:e73–e74. [Google Scholar]
- 31.Jiang HH, Song B, Lu GS, Wen QJ, Jin XY. Loss of ryanodine receptor calcium-release channel expression associated with overactive urinary bladder smooth muscle contractions in a detrusor instability model. BJU Int. 2005;96:428–433. doi: 10.1111/j.1464-410X.2005.05644.x. [DOI] [PubMed] [Google Scholar]
- 32.Meredith AL, Thorneloe KS, Werner ME, Nelson MT, Aldrich RW. Overactive bladder and incontinence in the absence of the BK large conductance Ca2+-activated K+ channel. J. Biol. Chem. 2004;279:36746–36752. doi: 10.1074/jbc.M405621200. [DOI] [PubMed] [Google Scholar]
- 33.Oger S;, et al. Effects of potassium channel modulators on myogenic spontaneous phasic contractile activity in human detrusor from neurogenic patients. BJU Int. 2011;108:604–611. doi: 10.1111/j.1464-410X.2010.09935.x. [DOI] [PubMed] [Google Scholar]
- 34.Thorneloe KS, Meredith AL, Knorn AM, Aldrich RW, Nelson MT. Urodynamic properties and neurotransmitter dependence of urinary bladder contractility in the BK channel deletion model of overactive bladder. Am. J. Physiol. Renal Physiol. 2005;289:F604–F610. doi: 10.1152/ajprenal.00060.2005. [DOI] [PubMed] [Google Scholar]
- 35.Chen M, Petkov GV. Identification of large conductance calcium activated potassium channel accessory beta4 subunit in rat and mouse bladder smooth muscle. J. Urol. 2009;182:374–381. doi: 10.1016/j.juro.2009.02.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hristov K, Chen M, Afeli S, Rovner E, Petkov GV. Expression and function of voltage-gated K+ channels sensitive to stromatoxin-1 in human detrusor smooth muscle. J. Urol. 2011;185:e91. [Google Scholar]
- 37.Hristov KL;, et al. KV2.1 and electrically silent KV channel subunits control excitability and contractility of Guinea pig detrusor smooth muscle. Am. J. Physiol. Cell Physiol. 2010 doi: 10.1152/ajpcell.00303.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamill OP, Marty A, Neher E, Sakmann B, Sigworth FJ. Improved patch-clamp techniques for high-resolution current recording from cells and cell-free membrane patches. Pflugers Arch. 1981;391:85–100. doi: 10.1007/BF00656997. [DOI] [PubMed] [Google Scholar]
- 39.Klockner U, Isenberg G. Action potentials and net membrane currents of isolated smooth muscle cells (urinary bladder of the guinea-pig) Pflugers Arch. 1985;405:329–339. doi: 10.1007/BF00595685. [DOI] [PubMed] [Google Scholar]
- 40.Kellett WF, Cui X, Hristov KL, Petkov GV. SK and IK Ca2+-activated K+ channels as novel pharmacological targets to control urinary bladder smooth muscle excitability and contractility. FASEB J. 2008;22:1201–1219. [Google Scholar]
- 41.Parajuli SP, Soder RP, Hristov KL, Petkov GV. Pharmacological activation of SK channels with SKA-31 decreases Guinea pig detrusor smooth muscle excitability and contractility. J. Pharmacol. Exp. Ther. 2011 doi: 10.1124/jpet.111.186213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horn R, Marty A. Muscarinic activation of ionic currents measured by a new whole-cell recording method. J. Gen. Physiol. 1988;92:145–159. doi: 10.1085/jgp.92.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Petkov GV, Nelson MT. Differential regulation of Ca2+-activated K+ channels by β-adrenoceptors in guinea pig urinary bladder smooth muscle. Am. J. Physiol. Cell Physiol. 2005;288:C1255–C1263. doi: 10.1152/ajpcell.00381.2004. [DOI] [PubMed] [Google Scholar]
- 44.Sprossmann F;, et al. Inducible knockout mutagenesis reveals compensatory mechanisms elicited by constitutive BK channel deficiency in overactive murine bladder. FEBS J. 2009;276:1680–1697. doi: 10.1111/j.1742-4658.2009.06900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pandita RK, Ronn LC, Jensen BS, Andersson KE. Urodynamic effects of intravesical administration of the new small/ intermediate conductance calcium activated potassium channel activator NS309 in freely moving, conscious rats. J. Urol. 2006;176:1220–1224. doi: 10.1016/j.juro.2006.04.081. [DOI] [PubMed] [Google Scholar]
- 46.Streng T, Christoph T, Andersson KE. Urodynamic effects of the K+ channel (KCNQ) opener retigabine in freely moving, conscious rats. J. Urol. 2004;172:2054–2058. doi: 10.1097/01.ju.0000138155.33749.f4. [DOI] [PubMed] [Google Scholar]
- 47.Thorneloe KS, Nelson MT. Properties and molecular basis of the mouse urinary bladder voltage-gated K+ current. J. Physiol. 2003;549:65–74. doi: 10.1113/jphysiol.2003.039859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gutman GA, et al. International Union of Pharmacology. XLI. Compendium of voltage-gated ion channels: potassium channels. Pharmacol. Rev. 2003;55:583–586. doi: 10.1124/pr.55.4.9. [DOI] [PubMed] [Google Scholar]
- 49.Gutman GA, et al. International Union of Pharmacology. LIII. Nomenclature and molecular relationships of voltage-gated potassium channels. Pharmacol. Rev. 2005;57:473–508. doi: 10.1124/pr.57.4.10. [DOI] [PubMed] [Google Scholar]
- 50.Wulff H, Castle NA, Pardo LA. Voltage-gated potassium channels as therapeutic targets. Nat. Rev. Drug Discov. 2009;8:982–1001. doi: 10.1038/nrd2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davies AM, Batchelor TJ, Eardley I, Beech DJ. Potassium channel KVα1 subunit expression and function in human detrusor muscle. J. Urol. 2002;167:1881–1886. [PubMed] [Google Scholar]
- 52.Ohya S, Tanaka M, Watanabe M, Maizumi Y. Diverse expression of delayed rectifier K+ channel subtype transcripts in several types of smooth muscles of the rat. J. Smooth Muscle Res. 2000;36:101–115. doi: 10.1540/jsmr.36.101. [DOI] [PubMed] [Google Scholar]
- 53.Gan XG, An RH, Bai YF, Zong DB. Expressions of voltage-gated K+ channel 2.1 and 2.2 in rat bladder with detrusor hyperreflexia. Chin. Med. J. (Engl.) 2008;121:1574–1577. [PubMed] [Google Scholar]
- 54.Escoubas P, Diochot S, Celerier ML, Nakajima T, Lazdunski M. Novel tarantula toxins for subtypes of voltage-dependent potassium channels in the Kv2 and Kv4 subfamilies. Mol. Pharmacol. 2002;62:48–57. doi: 10.1124/mol.62.1.48. [DOI] [PubMed] [Google Scholar]
- 55.Moreno-Dominguez A, Cidad P, Miguel-Velado E, Lopez-Lopez JR, Perez- Garcia MT. De novo expression of Kv6.3 contributes to changes in vascular smooth muscle cell excitability in a hypertensive mice strain. J. Physiol. 2009;587:625–640. doi: 10.1113/jphysiol.2008.165217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rode F, Svalo J, Sheykhzade M, Ronn LC. Functional effects of the KCNQ modulators retigabine and XE991 in the rat urinary bladder. Eur. J. Pharmacol. 2010;638:121–127. doi: 10.1016/j.ejphar.2010.03.050. [DOI] [PubMed] [Google Scholar]
- 57.Herrera GM, Heppner TJ, Nelson MT. Voltage dependence of the coupling of Ca2+ sparks to BKCa channels in urinary bladder smooth muscle. Am. J. Physiol. Cell Physiol. 2001;280:C481–C490. doi: 10.1152/ajpcell.2001.280.3.C481. [DOI] [PubMed] [Google Scholar]
- 58.Soder RP, Petkov GV. Large conductance Ca2+-activated K+ channel activation with NS1619 decreases myogenic and neurogenic contractions of rat detrusor smooth muscle. Eur. J. Pharmacol. 2011;670:252–259. doi: 10.1016/j.ejphar.2011.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Suarez-Kurtz G, Garcia ML, Kaczorowski GJ. Effects of charybdotoxin and iberiotoxin on the spontaneous motility and tonus of different guinea pig smooth muscle tissues. J. Pharmacol. Exp. Ther. 1991;259:439–443. [PubMed] [Google Scholar]
- 60.Knaus HG;, et al. Tremorgenic indole alkaloids potently inhibit smooth muscle high-conductance calcium-activated potassium channels. Biochemistry. 1994;33:5819–5828. doi: 10.1021/bi00185a021. [DOI] [PubMed] [Google Scholar]
- 61.Layne JJ, Nausch B, Olesen SP, Nelson MT. BK channel activation by NS11021 decreases excitability and contractility of urinary bladder smooth muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;298:R378–R384. doi: 10.1152/ajpregu.00458.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Siemer C, Bushfield M, Newgreen D, Grissmer S. Effects of NS1608 on MaxiK channels in smooth muscle cells from urinary bladder. J. Membr. Biol. 2000;173:57–66. doi: 10.1007/s002320001007. [DOI] [PubMed] [Google Scholar]
- 63.Ohi Y, et al. Local Ca2+ transients and distribution of BK channels and ryanodine receptors in smooth muscle cells of guinea-pig vas deferens and urinary bladder. J. Physiol. 2001;534:313–326. doi: 10.1111/j.1469-7793.2001.t01-3-00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kita M;, et al. Effects of bladder outlet obstruction on properties of Ca2+-activated K+ channels in rat bladder. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;298:R1310–R1319. doi: 10.1152/ajpregu.00523.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hashitani H, Brading AF. Ionic basis for the regulation of spontaneous excitation in detrusor smooth muscle cells of the guinea-pig urinary bladder. Br. J. Pharmacol. 2003;140:159–169. doi: 10.1038/sj.bjp.0705320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Darblade B;, et al. Effects of potassium channel modulators on human detrusor smooth muscle myogenic phasic contractile activity: potential therapeutic targets for overactive bladder. Urology. 2006;68:442–448. doi: 10.1016/j.urology.2006.03.039. [DOI] [PubMed] [Google Scholar]
- 67.Herrera GM, Etherton B, Nausch B, Nelson MT. Negative feedback regulation of nerve-mediated contractions by KCa channels in mouse urinary bladder smooth muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;289:R402–R409. doi: 10.1152/ajpregu.00488.2004. [DOI] [PubMed] [Google Scholar]
- 68.Kellett WF, Petkov GV. Role of Ca2+-activated K+ channel in the neurogenic contractions induced by electrical field stimulation in detrusor smooth muscle isolated from rats and guinea pigs. Biophys. J. 2010;98:125a–126a. [Google Scholar]
- 69.Malysz J;, et al. Functional characterization of large conductance calcium-activated K+ channel openers in bladder and vascular smooth muscle. Naunyn Schmiedebergs Arch. Pharmacol. 2004;369:481–489. doi: 10.1007/s00210-004-0920-y. [DOI] [PubMed] [Google Scholar]
- 70.Parajuli SP, Hristov K, Pandey R, Rovner ES, Petkov GV. BK channel activation with NS1619 decreases excitability and contractility of human urinary bladder smooth muscle. FASEB J. 2011;25 1115.14. [Google Scholar]
- 71.Nelson MT;, et al. Relaxation of arterial smooth muscle by calcium sparks. Science. 1995;270:633–637. doi: 10.1126/science.270.5236.633. [DOI] [PubMed] [Google Scholar]
- 72.Takemoto J, et al. Potentiation of potassium currents by β-adrenoceptor agonists in human urinary bladder smooth muscle cells: a possible electrical mechanism of relaxation. Pharmacology. 2008;81:251–258. doi: 10.1159/000114719. [DOI] [PubMed] [Google Scholar]
- 73.Kobayashi H, Adachi-Akahane S, Nagao T. Involvement of BKCa channels in the relaxation of detrusor muscle via β-adrenoceptors. Eur. J. Pharmacol. 2000;404:231–238. doi: 10.1016/s0014-2999(00)00606-3. [DOI] [PubMed] [Google Scholar]
- 74.Li L;, et al. Changes in T-type calcium channel and its subtypes in overactive detrusor of the rats with partial bladder outflow obstruction. Neurourol. Urodyn. 2007;26:870–878. doi: 10.1002/nau.20392. [DOI] [PubMed] [Google Scholar]
- 75.Aydin M, Wang H-Z, Melman A, DiSanto ME. Large conductance calcium-activated potassium channel activity, as determined by whole cell patch clamp recording, is decreased in urinary bladder smooth muscle cells from male rats with partial urethral obstruction. J. Urol. 2009;181(Suppl.):542. doi: 10.1111/j.1464-410X.2012.11137.x. [DOI] [PubMed] [Google Scholar]
- 76.Hotta S;, et al. Ryanodine receptor type 2 deficiency changes excitation-contraction coupling and membrane potential in urinary bladder smooth muscle. J. Physiol. 2007;582:489–506. doi: 10.1113/jphysiol.2007.130302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Davies KP;, et al. Ageing causes cytoplasmic retention of MaxiK channels in rat corporal smooth muscle cells. Int. J. Impot. Res. 2007;19:371–377. doi: 10.1038/sj.ijir.3901541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toro L;, et al. Aging, ion channel expression, and vascular function. Vascul. Pharmacol. 2002;38:73–80. doi: 10.1016/s0306-3623(02)00128-3. [DOI] [PubMed] [Google Scholar]
- 79.Christ GJ, et al. Bladder injection of “naked” hSlo/pcDNA3 ameliorates detrusor hyperactivity in obstructed rats in vivo . Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;281:R1699–R1709. doi: 10.1152/ajpregu.2001.281.5.R1699. [DOI] [PubMed] [Google Scholar]
- 80.Christ GJ. Potential applications of gene therapy/transfer to the treatment of lower urinary tract diseases/disorders. Handb. Exp. Pharmacol. 2011;202:255–265. doi: 10.1007/978-3-642-16499-6_12. [DOI] [PubMed] [Google Scholar]
- 81.Melman A, Bar-Chama N, McCullough A, Davies K, Christ G. Plasmid-based gene transfer for treatment of erectile dysfunction and overactive bladder: results of a phase I trial. Isr. Med. Assoc. J. 2007;9:143–146. [PubMed] [Google Scholar]
- 82.Melman A, Feder M. Gene therapy for the treatment of erectile dysfunction. Nat. Clin. Pract. Urol. 2008;5:60–61. doi: 10.1038/ncpuro1014. [DOI] [PubMed] [Google Scholar]
- 83.Melman A, Rojas L. Christ, G. Gene transfer for erectile dysfunction: will this novel therapy be accepted by urologists? Curr. Opin. Urol. 2009;19:595–600. doi: 10.1097/MOU.0b013e3283314985. [DOI] [PubMed] [Google Scholar]
- 84.Maylie J, Bond CT, Herson PS, Lee WS, Adelman JP. Small conductance Ca2+-activated K+ channels and calmodulin. J. Physiol. 2004;554:255–261. doi: 10.1113/jphysiol.2003.049072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thorneloe KS;, et al. Small-conductance, Ca2+-activated K+ channel 2 is the key functional component of SK channels in mouse urinary bladder. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;294:R1737–R1743. doi: 10.1152/ajpregu.00840.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nielsen JS;, et al. Effect of the SK/IK channel modulator 4,5-dichloro-1,3-diethyl-1,3-dihydro-benzoimidazol-2-one (NS4591) on contractile force in rat, pig and human detrusor smooth muscle. BJU Int. 2011;108:771–777. doi: 10.1111/j.1464-410X.2010.10019.x. [DOI] [PubMed] [Google Scholar]
- 87.Hougaard C;, et al. A positive modulator of KCa2 and KCa3 channels, 4,5-dichloro-1,3-diethyl-1,3-dihydro-benzoimidazol-2-one (NS4591), inhibits bladder afferent firing in vitro and bladder overactivity in vivo . J. Pharmacol. Exp. Ther. 2009;328:28–39. doi: 10.1124/jpet.108.143123. [DOI] [PubMed] [Google Scholar]
- 88.Sankaranarayanan A;, et al. Naphtho[1,2-d] thiazol-2-ylamine (SKA-31), a new activator of KCa2 and KCa3.1 potassium channels, potentiates the endothelium-derived hyperpolarizing factor response and lowers blood pressure. Mol. Pharmacol. 2009;75:281–295. doi: 10.1124/mol.108.051425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen MX;, et al. Small and intermediate conductance Ca2+-activated K+ channels confer distinctive patterns of distribution in human tissues and differential cellular localisation in the colon and corpus cavernosum. Naunyn Schmiedebergs Arch. Pharmacol. 2004;369:602–615. doi: 10.1007/s00210-004-0934-5. [DOI] [PubMed] [Google Scholar]
- 90.Ohya S;, et al. SK4 encodes intermediate conductance Ca2+-activated K+ channels in mouse urinary bladder smooth muscle cells. Jpn J. Pharmacol. 2000;84:97–100. doi: 10.1254/jjp.84.97. [DOI] [PubMed] [Google Scholar]
- 91.Wulff H;, et al. Design of a potent and selective inhibitor of the intermediate-conductance Ca2+-activated K+ channel, IKCa1: a potential immunosuppressant. Proc. Natl Acad. Sci. USA. 2000;97:8151–8156. doi: 10.1073/pnas.97.14.8151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kajioka S;, et al. Levcromakalim and MgGDP activate small conductance ATP-sensitive K+ channels of K+ channel pore 6.1/sulfonylurea receptor 2A in pig detrusor smooth muscle cells: uncoupling of cAMP signal pathways. J. Pharmacol. Exp. Ther. 2008;327:114–123. doi: 10.1124/jpet.108.140269. [DOI] [PubMed] [Google Scholar]
- 93.Kajioka S;, et al. Diphosphate regulation of adenosine triphosphate sensitive potassium channel in human bladder smooth muscle cells. J. Urol. 2011;186:736–744. doi: 10.1016/j.juro.2011.03.153. [DOI] [PubMed] [Google Scholar]
- 94.Davis-Taber R;, et al. [125I]A-312110, a novel high-affinity 1,4-dihydropyridine ATP-sensitive K+ channel opener: characterization and pharmacology of binding. Mol. Pharmacol. 2003;64:143–153. doi: 10.1124/mol.64.1.143. [DOI] [PubMed] [Google Scholar]
- 95.Shieh CC;, et al. Functional implication of spare ATP-sensitive K+ channels in bladder smooth muscle cells. J. Pharmacol. Exp. Ther. 2001;296:669–675. [PubMed] [Google Scholar]
- 96.Foster CD, Fujii K, Kingdon J, Brading AF. The effect of cromakalim on the smooth muscle of the guinea-pig urinary bladder. Br. J. Pharmacol. 1989;97:281–291. doi: 10.1111/j.1476-5381.1989.tb11952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Heppner TJ, Bonev A, Li JH, Kau ST, Nelson MT. Zeneca ZD6169 activates ATP-sensitive K+ channels in the urinary bladder of the guinea pig. Pharmacology. 1996;53:170–179. doi: 10.1159/000139428. [DOI] [PubMed] [Google Scholar]
- 98.Andersson KE;, et al. Effects of pinacidil on bladder muscle. Drugs. 1988;36(Suppl. 7):41–49. doi: 10.2165/00003495-198800367-00007. [DOI] [PubMed] [Google Scholar]
- 99.Bonev AD, Nelson MT. ATP-sensitive potassium channels in smooth muscle cells from guinea pig urinary bladder. Am. J. Physiol. 1993;264:C1190–C1200. doi: 10.1152/ajpcell.1993.264.5.C1190. [DOI] [PubMed] [Google Scholar]
- 100.Sanders KM, Koh SD. Two-pore-domain potassium channels in smooth muscles: new components of myogenic regulation. J. Physiol. 2006;570:37–43. doi: 10.1113/jphysiol.2005.098897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Baker SA;, et al. Methionine and its derivatives increase bladder excitability by inhibiting stretch-dependent K+ channels. Br. J. Pharmacol. 2008;153:1259–1271. doi: 10.1038/sj.bjp.0707690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Beckett EA;, et al. Functional and molecular identification of pH-sensitive K+ channels in murine urinary bladder smooth muscle. BJU Int. 2008;102:113–124. doi: 10.1111/j.1464-410X.2008.07541.x. [DOI] [PubMed] [Google Scholar]
- 103.Tertyshnikova S;, et al. BL-1249 [(5,6,7,8-tetrahy dro-naphthalen-1-yl)-[2-(1H–tetrazol-5-yl)-phenyl]-amine]: a putative potassium channel opener with bladder-relaxant properties. J. Pharmacol. Exp. Ther. 2005;313:250–259. doi: 10.1124/jpet.104.078592. [DOI] [PubMed] [Google Scholar]