Abstract
There is an urgent need for new and better vaccines against tuberculosis (TB). Current vaccine design strategies are generally focused on the enhancement of cell-mediated immunity. Antibody-based approaches are not being considered, mostly due to the paradigm that humoral immunity plays little role in the protection against intracellular pathogens. Here, we reappraise and update the increasing evidence for antibody-mediated immunity against Mycobacterium tuberculosis, discuss the complexity of antibody responses to mycobacteria, and address mechanism of protection. Based on these findings and discussions, we challenge the common belief that immunity against M. tuberculosis relies solely on cellular defense mechanisms, and posit that induction of antibody-mediated immunity should be included in TB vaccine development strategies.
The Need for New TB Vaccines
Approximately one-third of the world’s population is infected with Mycobacterium tuberculosis (M.tb), leading to an asymptomatic state referred to as latent tuberculosis infection (LTBI). About 10% of people with LTBI subsequently develop the disease tuberculosis (TB), a risk that can be up to 30 times higher in the setting of immunodeficiency such as that caused by HIV infection (World Health Organization, 2012). Consequently, an estimated 8.8 million new TB cases are currently reported annually, with ~1.1 million TB-associated deaths among HIV-uninfected and ~0.35 million among HIV coinfected people (World Health Organization, 2012). The available vaccine in the form of an attenuated Mycobacterium bovis Bacillus Calmette-Guérin (BCG) strain is clearly inadequate, and a more effective vaccine against active TB is urgently needed.
An “ideal” antituberculous vaccine would protect against both infection with M.tb in exposed persons and the development of disease in those who have already been infected. The current BCG vaccine has limited protective capacity. Its main effect is partial protection against disseminated TB during early childhood with little or no impact on the development of “reactivation” TB later in life (reviewed in Colditz et al., 1994). Furthermore, this vaccine appears to have variable effectiveness due to considerable batch-to-batch variations as well as differences in BCG strains utilized for vaccination (Keyser et al., 2011). In addition, the BCG vaccine does not prevent infection with M.tb. Nevertheless, this vaccine has been in use for almost a century and remains the only approved vaccine against TB.
Historically the most effective antimicrobial vaccines protect the host by generating antibody responses that neutralize the initial inoculum to prevent the establishment of infections (Robbins et al., 1995). In fact, all approved vaccines against bacterial pathogens, except for M.tb, are believed to mediate protection by generating an antibody response that neutralizes the infecting inoculum (Robbins et al., 1995). Unfortunately, it has been difficult to apply this successful formula for protection against TB because infection fails to consistently elicit protective Abs to M.tb (Glatman-Freedman, 2006). A clinically highly relevant alternative would be a vaccine that would not protect against infection but would prevent disease. The association of TB with granuloma progression to caseous necrosis suggests that a vaccine that could promote and enhance local containment might prevent both disease and transmission. In this regard, the fact that humoral immunity is a potent mediator of inflammation, and that some antibodies downregulate inflammation (Buccheri et al., 2007), suggests that vaccines eliciting inflammation-modulating antibodies could protect by preventing granulomas from progressing to caseous necrosis. Such a vaccine is theoretically possible even though there is no precedent for this among licensed products. In this strategy the protective effect would be mediated by better control of mycobacteria in the granuloma through the addition of antibody effector mechanisms and/or better-organized granulomas.
Several new TB vaccines and vaccination approaches are in development, and many of those are presently at various stages in clinical trials. These have been extensively reviewed elsewhere (Checkley and McShane, 2011; Kaufmann, 2011) and will not be discussed in detail here. Most of the new vaccination strategies focus on either improving the current BCG vaccine or boosting it with a second dose of BCG or a different TB vaccine. However, all of these strategies have in common the goal of targeting the enhancement of cell-mediated immunity against M.tb. While there is no doubt that cell-mediated immunity is a major component in the control of mycobacterial infection, there are now compelling data showing that protective Abs against mycobacteria exist as discussed here and previously described (Abebe and Bjune, 2009; Glatman-Freedman, 2006;Glatman-Freedman and Casadevall, 1998). Such data suggest that enhanced TB vaccine effectiveness could be achieved by including approaches that, in addition to cell-mediated immunity, also induce humoral immunity. In this regard, vaccines that elicit responses from both arms of the adaptive immunity may work synergistically, given the interconnectedness between humoral and cellular immunity. However, antibody-based vaccine approaches are still not being considered in the design of vaccines against TB. This is due to several factors that range from inadequate understanding of the efficacy of antibody-mediated immunity against intracellular pathogens, to the notion that, given that Th1-type responses are critical for containment of intracellular infection, a vaccine must work through that mechanism for efficacy. This Perspective will reappraise and update the increasing evidence of antibody-mediated immunity against M.tb, explore potential mechanism of protection, and challenge the common belief that immunity against M.tb relies solely on cellular defense mechanisms. Due to the wealth of literature and prior reviews, we focus predominantly on studies published more recently. For a summary of earlier studies, we refer the reader to an earlier review (Glatman-Freedman and Casadevall, 1998). At the end of this Perspective, we propose a paradigm shift and propose that induction of antibody-mediated immunity should be included in TB vaccine development strategies.
The Human Humoral Immune Response to TB
The field of TB serology provides abundant data showing that M.tb induces a humoral immune response to a wide variety of mycobacterial antigens in humans despite being an intracellular pathogen (reviewed in Steingart et al., 2009). Furthermore, several studies have demonstrated that intradermal BCG vaccination elicits IgG and IgM responses to several mycobacterial antigens, and especially to the glycolipid lipoarabinomannan, a major cell wall antigen (Beyazova et al., 1995; Brown et al., 2003; de Vallière et al., 2005). Some of these antibody responses were also shown to enhance both innate and cell-mediated immune responses against mycobacteria (de Vallière et al., 2005).
The humoral immune response to mycobacterial antigens differs depending on the state of infection (reviewed in Kunnath-Velayudhan and Gennaro, 2011). For example, individuals with LTBI, considered to not have active TB, have Abs to a much smaller and partially different repertoire of M.tb antigens than those with TB. Furthermore, data in both animals and humans indicate that the height of antibody titers correlates with the degree of mycobacterial burden (Achkar et al., 2010;Kunnath-Velayudhan et al., 2010; Yu et al., 2012). The observation of high antibody titers against mycobacterial antigens in patients with the disease has historically supported the argument that these antibodies must be nonprotective. Paradoxically, the same type of reasoning is not used to challenge the currently established concept that immunity against TB is mostly cell and cytokine mediated (i.e., INF-γ), since the majority of patients develop TB despite having normal T cell function and high INF-γ levels. In fact, just as certain antibody titers can serve as markers for TB, INF-γ levels can indicate progression from infection to disease (Diel et al., 2011; Lin et al., 2009). Although we concur that many antibodies elicited by M.tb might not be functional or could even enhance an inflammatory response, various studies show or suggest that certain antibodies have protective function against TB.
Antibody-Mediated Protection against Intracellular Pathogens
The efficacy of antibody-mediated immunity against a microbe is established by three general approaches singly or in combination (Casadevall, 2004):
Establish that passive administration of a microbe-specific antibody modifies the course of infection to the benefit of the host.
Document an inverse relationship between the presence of microbe specific antibody in a host and susceptibility to infection and disease.
Establish increased susceptibility to disease in hosts with deficits in humoral immunity and/or B cell function.
Until relatively recently it was not possible to consistently establish any of these criteria for a role of antibody-mediated immunity in protection against TB. The inability to obtain positive evidence combined with the overwhelming evidence for a strong role for cell-mediated protection set up a false dichotomy which posited no role for humoral immunity while assigning all protective function to cell-mediated immunity. It is noteworthy that this belief also represented a logical error in assuming that the absence of experimental evidence for antibody-mediated immunity implied no role for antibody in host defense. Further obscuring the analysis was the notion that since M.tb was an intracellular pathogen it was outside the reach of antibody efficacy because immunoglobulins are extracellular molecules. However, this relatively simplistic view missed the numerous mechanisms by which antibody-mediated immunity could modify the outcome of bacterial intracellular pathogenesis through effects ranging from opsonization to activation of FcR (Casadevall, 2003).
Like mycobacteria, many of the medically relevant fungi such as C. neoformans and Histoplasma capsulatum are facultative intracellular pathogens, and control of infection requires vigorous granuloma formation indicative of cell-mediated immunity. Like the field of TB, the field of mycology once regarded humoral immunity to have no role in protection against fungi, but this dogma was unraveled by the application of hybridoma technology, which revealed the existence of protective monoclonal antibodies (mAbs; reviewed in Casadevall, 1995). Two decades later, humoral immunity had been shown to be protective against numerous fungi (reviewed in Casadevall and Pirofski, 2012a), and two vaccines against C. albicans are currently in clinical trials, both of which are believed to mediate protection by eliciting protective humoral immunity (reviewed in Cassone and Casadevall, 2012). Furthermore, similar debates had gone on in other fields involving intracellular pathogens such as Salmonella spp., and yet vaccines were ultimately developed and licensed that protected through antibody-mediated immunity (Collins, 1974).
The precedents with medically relevant fungi and Salmonella spp. are relevant to the mycobacterial field because they establish that failure to elicit a protective antibody response and an inability to demonstrate the efficacy of antibody-mediated protection by the conventional methodology do not negate the absence of protective antibodies and the possibility of designing vaccines that mediate protection by eliciting protective antibody responses. We believe that sufficient information for the protective efficacy of antibodies against mycobacteria has now accumulated such that the field has reached a tipping point with regards to reassessing the mechanisms of immunity against TB.
The Complexity of Humoral Immunity against TB
The efficacy of humoral immunity against TB has now been studied for over 100 years, but for most of this time conclusive evidence has been lacking because animal and human studies have provided inconsistent and sometimes contradictory data (reviewed in Glatman-Freedman and Casadevall, 1998). However, even though the evidence for the efficacy of humoral immunity was inconsistent, the majority of studies in the literature ranging from the era of serum therapy to immunization with defined antigens suggested a protective role for antibody (Glatman-Freedman and Casadevall, 1998). The problem was not the absence of studies showing efficacy for antibody but the inconsistency in experimental results. When interpreting early studies, one must also take into consideration that serum therapy was typically performed with antibody preparations obtained from a different species than the one studied (Glatman-Freedman and Casadevall, 1998). In recent years, serological studies in animals have shown species-specific antibody responses to TB (Lyashchenko et al., 2008). Thus, transfer of antibody preparations between different species might be less effective than within the same species, and it is difficult to conclude much about the efficacy of antibodies from negative studies.
Following the fungal experience where the antibody response is complex and includes the generation of both protective and nonprotective antibodies, it is possible that the interstudy inconsistencies in the early studies reflected the types and amounts of antibodies found in the polyclonal preparations. Indirect evidence to support this notion comes from the observation that protective and nonprotective mAbs to TB exist (Teitelbaum et al., 1998). Heterogeneity of antibody responses has been documented in human TB (Lyashchenko et al., 1998; Steingart et al., 2009; Yu et al., 2012), and there is evidence that only a minority of TB patients produce antibodies with the specificity of a protective antibody to the mycobacterial polysaccharide arabinomannan (AM) (Navoa et al., 2003). Furthermore, a recent study demonstrated that sera from some TB contacts with high IgG titers against tuberculin can block proliferation of PBMC cultures with tuberculin, while sera from a few other contacts with high titers stimulated proliferation (Encinales et al., 2010). In contrast, no influence was observed with low-titer sera. These observations highlight the complexity and heterogeneity of the human humoral immune response against TB and emphasize that studies have to be meticulously well-designed and elaborate to identify and investigate protective functions of antibodies against TB.
The Evidence that Humoral Immunity Contributes to Protection against TB
In the past two decades, numerous studies have provided evidence for the three criteria used to establish the efficacy of humoral immunity against TB (Table 1). Eight independent laboratories have now reported that mAbs to mycobacterial antigens, ranging from surface proteins to polysaccharides, modify the course of experimental mycobacterial infection in mice to the benefit of the host (Balu et al., 2011; Buccheri et al., 2009; Chambers et al., 2004; Hamasur et al., 2004; López et al., 2009; Pethe et al., 2001; Teitelbaum et al., 1998; Williams et al., 2004; Table 1 and Table 2). Furthermore, three recent passive polyclonal IgG or serum transfer studies within the same species (mice) or from humans to mice have shown protection against TB (Guirado et al., 2006; Olivares et al., 2006; Roy et al., 2005). Depending on the study design and the types and targets of mAbs evaluated, the measures of protection used were significantly increased survival times (Chambers et al., 2004; Hamasur et al., 2004; Teitelbaum et al., 1998), reduction of disease dissemination (Pethe et al., 2001), reduction of organ pathology (Balu et al., 2011; Chambers et al., 2004; López et al., 2009), and/or reduced organ CFU (Balu et al., 2011; Buccheri et al., 2009; Hamasur et al., 2004; López et al., 2009; Williams et al., 2004). One study evaluated the effects of either mAb (2E9IgA1) plus IFN-γ treatment, mAb alone, or IFN-γ alone compared to PBS controls (Balu et al., 2011). Compared to controls, the combined mAb plus IFN-γ treatment reduced lung CFU counts 4 weeks post-M.tb infection the most (>1 log[10]; p < 0.05). In contrast, there was no significant CFU reduction by IFN-γ alone (p = 0.23), while reduction due to mAb was borderline significant (p = 0.06). This study suggests a greater protective effect of an IgA mAb compared to IFN-γ but most of all demonstrates the potential synergism between antibody and cytokine treatment in the protection against TB. None of the mAb studies included a comparison group of BCG-vaccinated mice, hindering the direct comparison of quantitative effects of TB vaccines enhancing the cell-mediated immunity. When comparing mAb transfer studies to vaccination studies with BCG substrains which induce variable organ CFU reduction ranging from 1/2 to 1 1/2 mean log(10) 30 days after experimental M.tb infection in mice (Keyser et al., 2011), some of the quantitative effects of mAbs were less, some were similar, and some were superior to those described for BCG vaccines (Table 2). We note that the existence of protective mAbs does not in itself prove that humoral immunity has a role in the host defense against TB. For example, protective mAbs have been described against antigens in both Listeria monocytogenes and Histoplasma capsulatum that do not appear to contribute to natural immunity against those pathogens (Edelson et al., 1999; Nosanchuk et al., 2003). Nevertheless, the fact that such antibodies exist, together with further data discussed below, provides strong evidence for the notion that antibodies can be protective against TB.
Table 1.
Evidence of Antibody-Mediated Protection against TB
| Criterion | Evidence | References |
|---|---|---|
| Passive antibody transfer studies | Eight independent groups have shown protection and/or modification of the course of mycobacterial infection in mice with passive transfer of mAbs to mycobacterial antigens (Table 2) |
Balu et al., 2011; Buccheri et al., 2009; Chambers et al., 2004; Hamasur et al., 2004; López et al., 2009; Pethe et al., 2001; Teitelbaum et al., 1998; Williams et al., 2004 |
| Three independent groups have recently shown protection in mice with passive transfer of immune polyclonal sera |
Guirado et al., 2006; Olivares et al., 2006; Roy et al., 2005 |
|
| Antibody titer associated with reduced susceptibility |
AM-containing conjugate vaccine elicits antibody response that reduces susceptibility to infection (Table 3) |
Glatman-Freedman et al., 2004; Hamasur et al., 2003 |
| BCG as well as M.tb antigen-containing conjugate and DNA/RNA vaccines elicit cellular and humoral immune responses and improve outcome of infection (Table 3) |
Chang-hong et al., 2008; de Vallière et al., 2005; Giri et al., 2006; Glatman-Freedman et al., 2004; Grover et al., 2006; Hamasur et al., 2003; Huygen et al., 1996; Kohama et al., 2008; Niu et al., 2011; Palma et al., 2008; Teixeira et al., 2006; Xue et al., 2004 |
|
| Increased susceptibility in hosts with antibody deficits |
Peak of childhood TB is temporally correlated with nadir in maternal antibody |
Beyazova et al., 1995; Cruz and Starke, 2007; Donald et al., 2010 |
| Lack of antibodies against certain mycobacterial antigens is associated with TB dissemination in children and adults |
Boggian et al., 1996; Costello et al., 1992; Dayal et al., 2008; Gupta et al., 1997; Sada et al., 1990 |
|
| Lack of early humoral immune response in M.tb-infected nonhuman primates predicts high likelihood for reactivation disease |
Kunnath-Velayudhan et al., 2012 | |
| B cell-deficient mice are more susceptible to TB |
Maglione et al., 2008; Maglione et al., 2007; Vordermeier et al., 1996 |
|
| Polymeric IgR-deficient mice lose mycobacterial antigen-specific IgA response in saliva and are more susceptible to respiratory BCG infection |
Tjärnlund et al., 2006 | |
| IgA deficiency increases susceptibility to mycobacterial infection in mice |
Buccheri et al., 2007; Rodríguez et al., 2005 | |
| Other | Existence of mycobactericidal antibodies | Conti et al., 1998 |
| FcR-mediated phagocytosis promotes phagolysosomal fusion |
Armstrong and Hart, 1975 | |
| FcR-mediated phagocytosis increases macrophage Ca2+ signaling and intracellular killing |
Malik et al., 2000 | |
| IgG bound to BCG enhances oxygen release in phagosomes and antimycobacterial activity of alveolar macrophages |
Suga et al., 1996 |
mAb, monoclonal antibody; AM, arabinomannan; M.tb, M. tuberculosis.
Table 2.
Studies Demonstrating Protective Function of Monoclonal Antibodies against Experimental TB in Mice
| mAb (Isotype) | Target Antigen (Type) |
Model | Organism/Antigen Challenge (Route) |
mAb Administration (Timing to Infection) |
Change in CFU | Biological Effect | Quantitative Effect | References |
|---|---|---|---|---|---|---|---|---|
| 9d8 (IgG3) | AM (capsular polysaccharide) |
Mouse (BALB/c and C57BL/6) |
M.tb (ae and i.t.) | i.t. (simultaneous/ preincubated mAb with M.tb) |
↔ Lungs, spleen, and liver |
Prolonged survival and enhanced containment of M.tb within granuloma centers |
30%–60% of mAb-treated mice survived >75 days (33% over 220 days) versus death in control mice within 30 days (p < 0.01) |
Teitelbaum et al., 1998 |
| 4057 (IgG3) | HBHA (surface-exposed protein) | Mouse (BALB/c) | BCG (i.n.) | i.n. (simultaneous/ preincubated mAb with BCG) |
↔ Lungs | Reduction of disease dissemination |
Reduced spleen colonization by ~3 log(10) CFUs 3 weeks postinfection in mAb-treated mice compared to controls (p value not stated) |
Pethe et al., 2001 |
| ↓ Spleen |
||||||||
| TBA61 (IgA) | 16 kDa α-crystalin (intracellular and cell-wall protein) |
Mouse (BALB/c) | M.tb (ae and i.n.) | i.n. (3 hr before and 3 or 6 days after) |
↓ Lungs | CFU reduction in early disease |
Reduced lung colonization by ~1 log(10) CFUs 9 days postinfection in mAb-treated mice compared to controls (p < 0.01) |
Williams et al., 2004 |
| SMITH14 (IgG1) | AM portion of LAM (cell-wall glycolipid) |
Mouse (BALB/c) | M.tb (i.v.) | i.v. (simultaneous/ preincubated mAb with M.tb or 1 hr prior) |
↓ Lungs | CFU reduction and prolonged survival |
Reduced lung, liver, and spleen colonization by ~1–2 log(10) CFUs 14 days postinfection in mAb-treated mice 1 hr prior to infection compared to controls (p < 0.05 lungs and p < 0.01 liver and spleen) and survival of 7–8/10 (75%) mAb-treated mice versus 4/10 (40%) controls at 70 days (p < 0.01) |
Hamasur et al., 2004 |
| ↓Liver | ||||||||
| ↓Spleen | ||||||||
| MBS43 (IgG2b) | MPB83 (cell- wall and CF protein) |
Mouse (BALB/c) | M. bovis (i.v.) | i.n. (simultaneous/ preincubated mAb with M. bovis) |
↔ Lungs | Reduced lung pathology and prolonged survival |
Twice the estimated amount of normal lung tissue in mAb- treated mice compared to controls (p < 0.05) and 8/8 (100%) of mAb-treated mice survived >38 days (end of experiment) versus 0/8 (0%) of control mice (death within 30–34 days) (p < 0.005) |
Chambers et al., 2004 |
| ↔Liver | ||||||||
| ↔Spleen | ||||||||
| TBA61 (IgA) and TBA84 (IgA) |
16 kDa α-crystalin (intracellular and cell-wall protein) and 38 kDa PstS-1 (Cr protein) |
Mouse (BALB/c) | M.tb (i.t.) | i.t. (mAb given 30 min prior to infection) |
↓ Lungs (only for TBA61) |
Reduced lung pathology (only for TBA61) |
Reduced lung colonization by ~200 × 103 CFUs 21 days postinfection in mAb TBA61- treated mice compared to controls and TBA84-treated mice (p < 0.05) and reduced peribronchial inflammation in TBA61-treated mice compared to controls 21 days postinfection (p < 0.05) |
López et al., 2009 |
| TBA61 (IgA) | 16 kDa α-crystalin (intracellular and cell-wall protein) |
Mouse (BALB/c, C57BL/6,and C3H/HeJ) |
M.tb (i.v.) | i.n. and i.v. given at 3, 5, or 7 weeks as CIT with INF-γ, polyclonal Ab against IL-4, and mAbTBA61 in mice treated for 4 weeks with INH/R |
↓ Lungs in CIT- treated mice |
Prevention of TB relapse in mice treated with CIT together with ↑[ granuloma formation and ↑ cyto- and chemokine levels |
Reduced lung colonization by ~3–4 log(10) CFUs 8 weeks postinfection in CIT-treated mice compared to controls; strongest protection when CIT given 5 weeks postinfection (p = 0.001) |
Buccheri et al., 2009 |
| 2E9 (IgA1) | 16 kDa α-crystalin (intracellular and cell-wall protein) |
Mouse (CD89tg) | M.tb (i.n.) | i.n. with and without INF-γ (2 hr prior and 1 or 21 days post) |
↓ Lungs | Reduced lung pathology |
Reduced lung colonization by <1 log(10) CFUs 4 weeks postinfection in mAb plus INF-γ-treated mice compared to controls (p < 0.05) and significantly reduced lung granuloma formation in mAb- treated mice (<10%) compared to controls (~45%, p < 0.001) |
Balu et al., 2011 |
| ↓Spleen |
mAb, monoclonal antibody, CFU, colony-forming units, INF-γ, interferon-gamma, IL, interleukin; Antigens, AM, arabinomannan; LAM, lipoarabinomannan; HBHA, heparin-binding haemaglutinin; M.tb, M. tuberculosis, CF, culture filtrate, CIT, combined immunotherapy, INH/R, Isoniazid and Rifampin, ae, aerosol, i.n., intranasal, i.v., intravenous, i.t., intratracheal.
The criterion of associating the presence and absence of antibody with resistance and susceptibility to TB, respectively, has also been met. Regarding the presence of antibody, mice immunized with AM conjugate vaccines develop high IgG titers against AM and are more TB resistant than control mice (Glatman-Freedman et al., 2004; Hamasur et al., 2003; Table 1 and Table 3). In fact, one of these AM conjugate vaccines demonstrated prolonged survival and reduced histopathological findings comparable to BCG vaccine (Hamasur et al., 2003). Furthermore, BCG, many other mycobacterial antigen-based conjugate vaccines, as well as DNA/RNA vaccines, elicit humoral immune responses and improve the outcome of TB infection (Table 3). Although most of these vaccine studies conclude that protection against TB was based solely on cell-mediated immunity, they did not evaluate antibody function. Only the study by de Vallière et al. investigated the role of antibodies. This showed that BCG-induced antibodies promote critically enhancing effects on both the innate and cell-mediated immune responses to mycobacteria, providing further evidence of protective antibody functions against TB (de Vallière et al., 2005).
Table 3.
TB Vaccination Studies Documenting Induction of Ab Responses
| Organism or Antigen (Adjuvant) |
Vaccination Route |
Vaccination Time Points |
Experimental Model |
Organism Challenge (Route) |
Timing of Infection | Immune Response | CFU | Biological Effect | References |
|---|---|---|---|---|---|---|---|---|---|
| DNA encoding Ag 85A (none) |
i.m. | 0, 3, 6 weeks | Mice (BALB/c and C57BL/6) |
BCG and M.tb (i.v. [BCG] and ae [M.tb]) |
3–10 weeks after last immunization |
↑ Ag 85A-specific IgG1, IgG2a, and IgG2b, TNF-α and GM-CSF; ↔ IL-4, IL-6, and IL-10 |
↓ Lungs | Reduction in bacterial load (comparable to BCG) |
Huygen et al., 1996 |
| AM (TT and Ag85B) |
s.c. (mice); s.c. followed by i.n. (guinea pigs) |
0 (mice) | Mice (C57BL/6) and guinea pigs |
M.tb (i.n. or i.v. for mice; respiratory for guinea pigs) |
3–10 weeks after last immunization |
↑ AM-specific IgG, and T cell proliferation |
↔ Lungs | Prolonged survival and reduced pathology in lungs and spleen (comparable to BCG) |
Hamasur et al., 2003 |
| 0, 24 days (guinea pigs) |
→ Spleen | ||||||||
| AM (rEPA) | s.c. | 0, 2, 4 weeks | Mice (BALB/c) | BCG and M.tb (i.v.) |
Not stated | ↑ AM-specific IgG | ↓ Lungs | Reduction in bacterial load (1 week after infection) |
Glatman-Freedman et al., 2004 |
| ↓ Spleen ↓ Liver |
|||||||||
| RNA/DNA encoding MPT83 (none) |
i.m. | 0, 3, 6, 9 weeks | Mice (BALB/c) | M.tb (i.v.) | 4 weeks after last immunization |
↑ MPT83-specific IgG, IFN-γ, and IL-2 |
↓ Lungs | Protection against disease (inferior to BCG) |
Xue et al., 2004 |
| BCG | i.d. | 0, 6 months | Humans | NA | NA | ↑ LAM-specific IgG | NA | Postvaccination Abs enhanced the capacity of neutrophils and monocytes/macrophages to (1) internalize BCG, and (2) inhibit mycobacterial growth in vitro |
de Vallière et al., 2005 |
| Ag 85A, 85B, and 85AB (DDA) |
i.n. and s.c. | 0, 2, 4 weeks | Mice (BALB/c) | M.tb (ae) | 30 days after last immunization |
↑ Ag 85A- and 85B -specific IgA, IgG, IgG2, IFN-γ, IL-12, and IL-4 |
↓ Lungs | Protection against disease (comparable to BCG), strongest response with i.n. Ag85AB |
Giri et al., 2006 |
| ↓ Spleen | |||||||||
| DNA encoding Ag 85B (none) |
i.m. | 0, 15, 30, 45 days |
Mice (BALB/c) | M. bovis | 2 weeks after last immunization |
↑ Ag 85B-specific IgG, IgG1, and IgG2a, IFN-γ and TNF-α; ↔ IL-4 |
↔ Lungs | Partial reduction in bacterial load |
Teixeira et al., 2006 |
| ↓ Spleen | |||||||||
| DNA encoding CFP10 and CFP21 combined with Ag85B |
i.m. | 0, 3, 6 | Mice (C57BL/6) | M.tb (i.v.) | 4 weeks after last immunization |
↑ IgG1 and IgG2a (not indicated to which antigens), ↑IFN-γ, IL-12, and CTL response |
↓ Lungs | Reduction in bacterial load (comparable to BCG) |
Grover et al., 2006 |
| ↓Spleen | |||||||||
| DNA encoding Ag 85B (LTK63) |
i.m. | 0, 2 weeks | Mice (C57BL/6) | M.tb (i.v.) | 4 weeks after last immunization |
↑ Ag 85B-specific IgG, mostly IgG2b, ↓ IFN-γ, IL-10, and TNF-α compared to non-LTK 85B vaccine |
↓ Lungs | Partial reduction in bacterial load |
Palma et al., 2008 |
| rHBHA (cholera toxin) |
i.n. | 0, 2, 3, 4, 5 weeks | Mice (BALB/c) | BCG (ae) | 2 weeks after last immunization |
↑ HBHA-specific IgG and IgA, and IFN-γ |
↔ Lungs | Partial reduction in bacterial load 2 weeks postinfection |
Kohama et al., 2008 |
| ↓ Spleen | |||||||||
| DNA encoding fusion protein of Ag 85B and ESAT6 |
i.m. | 0, 2, 4, 6 weeks | Mice (BALB/c) | M.tb (i.v.) | 4 weeks after last immunization |
↑ Ag 85B-specific IgG1, IgG2a, and IFN-γ; ↔ IL-2 |
↓ Lungs | Reduced pathology in lungs and spleen |
Chang-hong et al., 2008 |
| ↓ Spleen | |||||||||
| Subunit vaccine Mtb 10.4-HspX |
s.c. | 0, 3, 6 weeks | Mice (C57 BL/6) | M.tb (i.v.) | 10 weeks after last immunization |
↑ HspX-specific IgG1, IgG2b, IgG2c, IFN-γ, and Il-17 |
↓ Lungs | Reduced pathology in lungs and spleen |
Niu et al., 2011 |
CFU, colony-forming units; INF-γ, interferon-gamma; IL, interleukin; TNF-α, tumor necrosis factor-alpha; rHBHA, recombinant heparin-binding haemaglutinin (surface-exposed protein); Ag, antigen; BCG, Mycobacterium bovis bacillus Calmette-Guerin; DDA, dimethyldioctadecylammonium bromide; i.m., intramuscular; s.c., subcutaneous; i.n., intranasal; i.d., intradermal; i.v., intravenous; ae, aerosol; AM, arabinomannan; rEPA, recombinant Pseudomonas aeruginosa exotoxin A; TT, tetanus toxoid; CTL, cytotoxic T lymphocyte.
Regarding the absence of antibody, the peak age of vulnerability for children coincides with a nadir in antibody to TB (Beyazova et al., 1995; Cruz and Starke, 2007; Donald et al., 2010). This relationship is further supported by a study demonstrating an association between the lack of antibody to the mycobacterial cell wall glycolipid lipoarabinomanna (LAM) with disseminated TB in age-matched children (Costello et al., 1992) (Table 1). Although these correlations do not necessarily establish causality, it is noteworthy that patients with HIV-associated TB, which tends to progress faster and frequently disseminates, also lack antibodies to LAM (Boggian et al., 1996). Furthermore, serological studies have found lower antibody levels against mycobacterial antigens in both children and adults with miliary, meningeal, and pleural TB in contrast to localized pulmonary TB (Dayal et al., 2008; Gupta et al., 1997; Sada et al., 1990). These findings suggest that low-antibody titers could increase the risk of TB dissemination.
There is also increasing evidence that mice with defective humoral immunity are more susceptible to TB. There are four studies with B cell-deficient mice in the literature. Two of them report that such mice are more susceptible to experimental infection (Maglione et al., 2007; Vordermeier et al., 1996). Another study involving mouse challenge with M.tb followed by isoniazid therapy and then rechallenge found no difference between B cell-deficient and wild-type mice (CDC, 2012). In contrast, one study found that the pulmonary histopathology was more pronounced in B cell knockout compared to wild-type mice after low-dose M.tb infection (Bosio et al., 2000). Despite comparable bacterial loads early after infection, B cell-deficient mice had reduced pulmonary granuloma formation and delayed dissemination of bacteria from lungs to peripheral organs compared to wild-type mice. These effects could be reconstituted with naive B cells, but not with serum from M.tb-infected wild-type mice. When interpreting such contradictory data, one has to keep in mind that for many components of the immune system, such as B cells, antibodies, and T cells and macrophages, good, bad, or neutral effects can be demonstrated, depending on many factors including the immune competency of the host. In that respect, although a lack of granuloma formation, especially in humans, is typically associated with increased numbers of mycobacteria, decreased containment of disease, and a higher likelihood of TB dissemination (Achkar and Jenny-Avital, 2011; Di Perri et al., 1996; Saunders and Cooper, 2000), granulomas may also help to promote infection in some animal models, such as the zebrafish (Davis and Ramakrishnan, 2009; Rubin, 2009). The investigators of the latter two studies concluded that humoral immunity had no role in the defense against TB, although, when evaluating negative studies, it is important to consider that an inability in measuring a difference does not necessarily imply that there is no difference.
We note that although antibodies are the products of B cells, these cells in themselves can contribute to host defense against mycobacterial disease through their numerous effects on the inflammatory response (Almeida et al., 2011; Bosio et al., 2000;Maglione and Chan, 2009; Maglione et al., 2007; Russo and Mariano, 2010; Zhang et al., 2012). In this regard, we note that whereas antibody-independent B cell effects are largely accepted by the field, the historical controversy involves the role of antibodies as B cell products, not B cells in themselves. Another study indicating a role of antibodies showed that IgA-deficient mice are more susceptible to infection with BCG (Rodríguez et al., 2005). Similarly, polymeric IgR-deficient mice that were vaccinated with the mycobacterial antigen PstS-1 had lower PstS-1 specific IgA levels in their saliva and were more susceptible to BCG infection then vaccinated wild-type mice (Tjärnlund et al., 2006). Also providing supportive evidence for a role of antibody protection in mucosal surfaces was the observation that IgA administration in the setting of IL-4 neutralization and IFN-γ administration conferred protection against M.tb in mice (Buccheri et al., 2007). The observation that mice lacking the γ-chain of an activating receptor for the Fc portion of Abs (FcγR) are more susceptible to M.tb infection and advanced pulmonary disease than wild-type mice (Maglione et al., 2008) provides further strong supportive evidence for a role of humoral immunity in host defense against mycobacteria.
Mechanisms of Antibody-Mediated Protection against M.tb
Despite being a facultative intracellular pathogen, M.tb is potentially susceptible to various mechanisms of antibody-mediated immunity. Opsonization through FcγR was shown to promote phagolysosomal fusion (Armstrong and Hart, 1975) and to increase macrophage Ca2+ signaling and intracellular killing (Malik et al., 2000). IgG bound to BCG increased the release of oxygen in the phagosomes of alveolar macrophages, suggesting the enhancement of antimycobacterial macrophage activity by antibody (Suga et al., 1996). Immune complexes that stimulate FcεRII-CD23 receptors trigger cellular changes that promote the killing of Toxoplasma gondii, another intracellular pathogen (Vouldoukis et al., 2011), and stimulation of the same receptor has been associated with antimycobaterial activity (Mossalayi et al., 2009). Furthermore, the existence of potentially synergistic functions between humoral and cell-mediated immunity against TB is suggested by the observation that anti-mycobacterial antibodies in BCG-vaccinated persons enhance both innate and cell-mediated immune responses against mycobacteria (de Vallière et al., 2005), and that sera from TB contacts with high but not low IgG titers against tuberculin can block proliferation of PBMC cultures with tuberculin (Encinales et al., 2010). Moreover, a robust T cell response against intracellular pathogens such as Chlamydia spp. and mycobacteria is enhanced by specific antibody responses that can augment Th1 activation via FcR by facilitating rapid uptake, processing, and presentation of antigens (Igietseme et al., 2004).
Antibody can also contribute to the host defense against M.tb by promoting the clearance of immunomodulatory antigens such as LAM (Glatman-Freedman et al., 2000). In addition, there are mechanisms shown in other intracellular pathogens that could also apply to M.tb. Protective and nonprotective mAbs mediate differences in gene expression for Cryptococcus neoformans (McClelland et al., 2010), and agglutinating nonopsonic antibodies have been shown to mediate bactericidal effects against Streptococcus pneumoniae through quorum-sensing-related mechanisms (Yano et al., 2011). Finally, antibodies that mimic the action of fungal killer toxin have been shown to be bactericidal to M.tb (Conti et al., 1998). Although such antibodies are unlikely to be present in M.tb infection, the fact that mycobacteria can be killed directly by certain antibodies provides a precedent for such a mechanism of antibody-mediated protection.
In addition to these direct mechanisms, antibodies can influence the outcome of mycobacterial infection through their ability to modulate inflammation. Some antibodies, such as IgM, can demonstrate proinflammatory properties through their ability to activate complement (Ciurana et al., 2004), while other antibodies, such as IgG, can demonstrate pro- or anti-inflammatory properties depending on the antigen and FcR receptor engaged (Ballow, 2011; Lux et al., 2010). Antibody-mediated activation of complement in mycobacterial infection has been demonstrated in several studies by various groups. Human IgG, and to a lesser extent, IgM, was found to enhance complement binding to BCG (Carroll et al., 2009). In TB patients, levels of serum IgG2 but not IgM against LAM correlated positively with classical complement activation induced by BCG (Hetland et al., 1998). Furthermore, human IgG against mycobacterial antigens in bacterial sonicates enhanced complement activation by M.tb and increased phagocytosis of M.tb by macrophages (Manivannan et al., 2012).
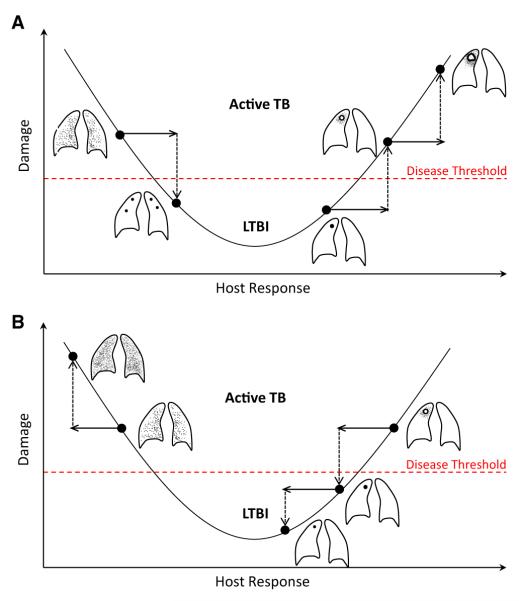
When the action of antibodies is analyzed from the context of the damage-response framework, it is apparent how the pro- or anti-inflammatory properties can be protective or deleterious depending on the immune status of the host (Figure 1). M.tb is pathogenic in hosts with either too much or too little inflammatory response, as evidenced by disease states characterized by caseous necrosis or widespread dissemination, such as miliary TB, respectively (Achkar and Jenny-Avital, 2011; Casadevall and Pirofski, 2003). In contrast, hosts that mount an intermediate response can presumably control infection through granuloma formation. From this synthesis it is apparent that antibodies that are proinflammatory could help hosts that respond with too little inflammation, while those that are anti-inflammatory could help hosts with exuberant inflammatory responses that result in tissue destructions.
Figure 1. Interpretation of the Potential Function of Pro- and Anti-Inflammatory Antibodies against M.tb in the Context of the Damage-Response Framework by Casadevall and Pirofski.
(A) Potential effects of a proinflammatory antibody with enhanced inflammation leading on the one hand to the improvement from disseminated/miliary TB in an immunocompromised host (left) to localized granuloma formation, and on the other hand to progression from granuloma to caseous necrosis in the more immunocompetent host (right).
(B) Potential effects of an anti-inflammatory antibody leading to worsening TB dissemination in the immunocompromised host who has already reduced inflammation (left), but improved containment of local disease from caseous necrosis to granuloma formation in the more immunocompetent host with a strong inflammatory response (right). LTBI, latent TB infection.
Characteristics of Protective Antibodies to M.tb
The major antibody characteristics that contribute to protection are specificity, affinity, and isotype. At this time relatively few mAbs have been studied in detail, and it is not possible to draw broad conclusions on the characteristics of protective antibodies to M.tb. However, some themes are beginning to emerge. At least six different antigenic determinants have been shown to be targeted by protective antibodies (Table 2). Murine mAbs of the IgM, IgG1, IgG3, and IgA isotype have each been shown to protect against TB, implying that these constant regions can mediate protection (Table 2). Evidence that the constant region has an important role in protection comes from the observation that an IgG3 to AM lost protective efficacy when switched to IgG2a, although there were no side-by-side comparisons of the parent and switched isotypes in the same experiment (Schwebach, 2002). In addition, Williams et al. showed that an IgA against the 16 kDa α-cristalin (TBA61) mediated some protection against TB, as evidenced by reduced mycobacterial burden in the lungs, while an IgG1 mAb (TB68) against the same epitope had no effect (Williams et al., 2004). The finding that some IgAs are protective against M.tb in pulmonary infection is interesting given the importance of this isotype in mucosal immunity. In this regard, Balu et al. reported that intranasal administration of IgA1 mAb 2E9 and recombinant mouse IFN-γ significantly inhibited pulmonary H37Rv infection in mice transgenic for human CD89, but not in CD89-negative littermate controls, suggesting that binding to CD89 was necessary for the IgA-mediated protection (Balu et al., 2011). At this time there is no information on the role of affinity in antibody efficacy. Furthermore, given that studies of antibody-mediated immunity against M.tb using defined reagents such as mAbs are at their infancy, the role of complement and type of FcR activation necessary for protection has not yet been investigated.
Antibody-Mediated Immunity against TB Could Enhance Vaccine Efficacy
When one considers the older data (Glatman-Freedman, 2006;Glatman-Freedman and Casadevall, 1998), the experience with other pathogens such as fungi and Salmonella spp., the complexity of antibody responses to mycobacteria, and other recent studies as summarized in Table 1, the preponderance of evidence indicates a role for humoral immunity in protection against TB. Given that protective and nonprotective antibodies exist, and that the antibody response to TB is heterogeneous, positive studies are much more significant than negative studies. In fact, negative studies are best interpreted to mean that the particular serum or vaccine used did not result in antibody-mediated protection in a specific setting, and such studies do not necessarily speak to the general question of antibody efficacy against TB. In contrast, positive studies provide evidence for the ability of humoral immunity to contribute to the host defense against TB. We therefore interpret the existing data to indicate that induction of antibody-mediated immunity could enhance protective effects of TB vaccine approaches.
We propose that antibody-mediated immunity can have a protective role against M. tb at various stages of infection. Based on the published observation in the field, we note that several mechanisms have already been established. Early in the course of infection, protective antibodies could promote ingestion by phagocytic cells and increased intracellular killing through FcR-mediated phagocytosis, which can also enhance cellular response through rapid uptake and processing of mycobacterial antigens. Such antibodies could also activate complement, which in turn can promote phagocytosis and inflammation. Antibodies to cell-surface polysaccharides and lipopolysaccharides could further mediate their clearance, and thus reduce their capacity for detrimental effects on the immune response. Finally, antibodies can modify the intensity of the inflammatory response, and here their dual nature as pro- and anti-inflammatory molecules could promote a bactericidal inflammatory response and/or reduce the tissue-destroying effects of runaway granuloma formation. In fact, antibodies could have different roles in protecting immunologically naive hosts during initial infection and in the setting of vaccination to protect against infection. Naturally occurring antibody, in particular IgM, has been shown to be critical against many infectious diseases (Casadevall and Pirofski, 2012b) and is likely to have an important role in protection by facilitating an early inflammatory response. In contrast, vaccine-induced IgG could be expected to function differently through the engagement of FcR. Although the relative importance of these effects is currently uncertain and may differ from host to host, the fact that antibodies have the capacity to powerfully affect all aspects of the interaction between mycobacteria and other components of the immune system suggests that this arm of the adaptive immune response can make a decisive contribution to the outcome of M.tb infection and should not be ignored.
ACKNOWLEDGMENTS
This work was supported by funds from the National Institutes of Health (NIH)/National Institute of Allergy and Infectious Diseases (NIAID; AI-067665 to J.M.A. and AI-033774, AI-052733, AI-033142 to A.C.); the National Heart, Lung, and Blood Institute (NHLBI; HL-059842 to A.C.); the Center for AIDS Research (CFAR) at the Albert Einstein College of Medicine (AI-51519; J.M.A.); the Aeras TB Vaccine Foundation (J.M.A. and A.C.); and the Food and Drug Administration (FDA; 1U18 FD004012/01 to J.M.A.). A.C. is also the recipient of a Bill and Melinda Gates Grand Challenge award and a TB Vaccine Accelerator Program award. We thank Anke Ziegenbalg for her graphic assistance with the figure.
REFERENCES
- Abebe F, Bjune G. The protective role of antibody responses during Mycobacterium tuberculosis infection. Clin. Exp. Immunol. 2009;157:235–243. doi: 10.1111/j.1365-2249.2009.03967.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achkar JM, Jenny-Avital ER. Incipient and subclinical tuberculosis: defining early disease states in the context of host immune response. J. Infect. Dis. 2011;204(Suppl 4):S1179–S1186. doi: 10.1093/infdis/jir451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achkar JM, Jenny-Avital E, Yu X, Burger S, Leibert E, Bilder PW, Almo SC, Casadevall A, Laal S. Antibodies against immunodominant antigens of Mycobacterium tuberculosis in subjects with suspected tuberculosis in the United States compared by HIV status. Clin. Vaccine Immunol. 2010;17:384–392. doi: 10.1128/CVI.00503-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida LP, Trombone AP, Lorenzi JC, Rocha CD, Malardo T, Fontoura IC, Gembre AF, Silva RL, Silva CL, Castelo AP, Coelho-Castelo AA. B cells can modulate the CD8 memory T cell after DNA vaccination against experimental tuberculosis. Genet. Vaccines Ther. 2011;9:5. doi: 10.1186/1479-0556-9-5. http://dx.doi.org/10.1186/1479-0556-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong JA, Hart PD. Phagosome-lysosome interactions in cultured macrophages infected with virulent tubercle bacilli. Reversal of the usual nonfusion pattern and observations on bacterial survival. J. Exp. Med. 1975;142:1–16. doi: 10.1084/jem.142.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballow M. The IgG molecule as a biological immune response modifier: mechanisms of action of intravenous immune serum globulin in autoimmune and inflammatory disorders. J. Allergy Clin. Immunol. 2011;127:315–323. doi: 10.1016/j.jaci.2010.10.030. [DOI] [PubMed] [Google Scholar]
- Balu S, Reljic R, Lewis MJ, Pleass RJ, McIntosh R, van Kooten C, van Egmond M, Challacombe S, Woof JM, Ivanyi J. A novel human IgA monoclonal antibody protects against tuberculosis. J. Immunol. 2011;186:3113–3119. doi: 10.4049/jimmunol.1003189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyazova U, Rota S, Cevheroğlu C, Karsligil T. Humoral immune response in infants after BCG vaccination. Tuber. Lung Dis. 1995;76:248–253. doi: 10.1016/s0962-8479(05)80013-9. [DOI] [PubMed] [Google Scholar]
- Boggian K, Fierz W, Vernazza PL. Infrequent detection of lipoarabinomannan antibodies in human immunodeficiency virus-associated mycobacterial disease. Swiss HIV Cohort Study. J. Clin. Microbiol. 1996;34:1854–1855. doi: 10.1128/jcm.34.7.1854-1855.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosio CM, Gardner D, Elkins KL. Infection of B cell-deficient mice with CDC 1551, a clinical isolate of Mycobacterium tuberculosis: delay in dissemination and development of lung pathology. J. Immunol. 2000;164:6417–6425. doi: 10.4049/jimmunol.164.12.6417. [DOI] [PubMed] [Google Scholar]
- Brown RM, Cruz O, Brennan M, Gennaro ML, Schlesinger L, Skeiky YA, Hoft DF. Lipoarabinomannan-reactive human secretory immunoglobulin A responses induced by mucosal bacille Calmette-Guérin vaccination. J. Infect. Dis. 2003;187:513–517. doi: 10.1086/368096. [DOI] [PubMed] [Google Scholar]
- Buccheri S, Reljic R, Caccamo N, Ivanyi J, Singh M, Salerno A, Dieli F. IL-4 depletion enhances host resistance and passive IgA protection against tuberculosis infection in BALB/c mice. Eur. J. Immunol. 2007;37:729–737. doi: 10.1002/eji.200636764. [DOI] [PubMed] [Google Scholar]
- Buccheri S, Reljic R, Caccamo N, Meraviglia S, Ivanyi J, Salerno A, Dieli F. Prevention of the post-chemotherapy relapse of tuberculous infection by combined immunotherapy. Tuberculosis (Edinb.) 2009;89:91–94. doi: 10.1016/j.tube.2008.09.001. [DOI] [PubMed] [Google Scholar]
- Carroll MV, Lack N, Sim E, Krarup A, Sim RB. Multiple routes of complement activation by Mycobacterium bovis BCG. Mol. Immunol. 2009;46:3367–3378. doi: 10.1016/j.molimm.2009.07.015. [DOI] [PubMed] [Google Scholar]
- Casadevall A. Antibody immunity and invasive fungal infections. Infect. Immun. 1995;63:4211–4218. doi: 10.1128/iai.63.11.4211-4218.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A. Antibody-mediated immunity against intracellular pathogens: two-dimensional thinking comes full circle. Infect. Immun. 2003;71:4225–4228. doi: 10.1128/IAI.71.8.4225-4228.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A. The methodology for determining the efficacy of antibody-mediated immunity. J. Immunol. Methods. 2004;291:1–10. doi: 10.1016/j.jim.2004.04.027. [DOI] [PubMed] [Google Scholar]
- Casadevall A, Pirofski LA. The damage-response framework of microbial pathogenesis. Nat. Rev. Microbiol. 2003;1:17–24. doi: 10.1038/nrmicro732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A, Pirofski LA. Immunoglobulins in defense, pathogenesis, and therapy of fungal diseases. Cell Host Microbe. 2012a;11:447–456. doi: 10.1016/j.chom.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A, Pirofski LA. A new synthesis for antibody-mediated immunity. Nat. Immunol. 2012b;13:21–28. doi: 10.1038/ni.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassone A, Casadevall A. Recent progress in vaccines against fungal diseases. Curr. Opin. Microbiol. 2012;15:427–433. doi: 10.1016/j.mib.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Vaccines and immunizations: rubella. 2012 http://www.cdc.gov/vaccines/pubs/pinkbook/rubella.html#.
- Chambers MA, Gavier-Widén D, Hewinson RG. Antibody bound to the surface antigen MPB83 of Mycobacterium bovis enhances survival against high dose and low dose challenge. FEMS Immunol. Med. Microbiol. 2004;41:93–100. doi: 10.1016/j.femsim.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Chang-hong S, Xiao-wu W, Hai Z, Ting-fen Z, Li-Mei W, Zhi-kai X. Immune responses and protective efficacy of the gene vaccine expressing Ag85B and ESAT6 fusion protein from Mycobacterium tuberculosis. DNA Cell Biol. 2008;27:199–207. doi: 10.1089/dna.2007.0648. [DOI] [PubMed] [Google Scholar]
- Checkley AM, McShane H. Tuberculosis vaccines: progress and challenges. Trends Pharmacol. Sci. 2011;32:601–606. doi: 10.1016/j.tips.2011.06.003. [DOI] [PubMed] [Google Scholar]
- Ciurana CL, Zwart B, van Mierlo G, Hack CE. Complement activation by necrotic cells in normal plasma environment compares to that by late apoptotic cells and involves predominantly IgM. Eur. J. Immunol. 2004;34:2609–2619. doi: 10.1002/eji.200425045. [DOI] [PubMed] [Google Scholar]
- Colditz GA, Brewer TF, Berkey CS, Wilson ME, Burdick E, Fineberg HV, Mosteller F. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA. 1994;271:698–702. [PubMed] [Google Scholar]
- Collins FM. Vaccines and cell-mediated immunity. Bacteriol. Rev. 1974;38:371–402. doi: 10.1128/br.38.4.371-402.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti S, Fanti F, Magliani W, Gerloni M, Bertolotti D, Salati A, Cassone A, Polonelli L. Mycobactericidal activity of human natural, monoclonal, and recombinant yeast killer toxin-like antibodies. J. Infect. Dis. 1998;177:807–811. doi: 10.1086/517815. [DOI] [PubMed] [Google Scholar]
- Costello AM, Kumar A, Narayan V, Akbar MS, Ahmed S, Abou-Zeid C, Rook GA, Stanford J, Moreno C. Does antibody to mycobacterial antigens, including lipoarabinomannan, limit dissemination in childhood tuberculosis? Trans. R. Soc. Trop. Med. Hyg. 1992;86:686–692. doi: 10.1016/0035-9203(92)90192-f. [DOI] [PubMed] [Google Scholar]
- Cruz AT, Starke JR. Clinical manifestations of tuberculosis in children. Paediatr. Respir. Rev. 2007;8:107–117. doi: 10.1016/j.prrv.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Davis JM, Ramakrishnan L. The role of the granuloma in expansion and dissemination of early tuberculous infection. Cell. 2009;136:37–49. doi: 10.1016/j.cell.2008.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayal R, Singh A, Katoch VM, Joshi B, Chauhan DS, Singh P, Kumar G, Sharma VD. Serological diagnosis of tuberculosis. Indian J. Pediatr. 2008;75:1219–1221. doi: 10.1007/s12098-008-0222-3. [DOI] [PubMed] [Google Scholar]
- de Vallière S, Abate G, Blazevic A, Heuertz RM, Hoft DF. Enhancement of innate and cell-mediated immunity by antimycobacterial antibodies. Infect. Immun. 2005;73:6711–6720. doi: 10.1128/IAI.73.10.6711-6720.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Perri G, Cazzadori A, Vento S, Bonora S, Malena M, Bontempini L, Lanzafame M, Allegranzi B, Concia E. Comparative histopathological study of pulmonary tuberculosis in human immunodeficiency virus-infected and non-infected patients. Tuber. Lung Dis. 1996;77:244–249. doi: 10.1016/s0962-8479(96)90008-8. [DOI] [PubMed] [Google Scholar]
- Diel R, Loddenkemper R, Niemann S, Meywald-Walter K, Nienhaus A. Negative and positive predictive value of a whole-blood interferon-γ release assay for developing active tuberculosis: an update. Am. J. Respir. Crit. Care Med. 2011;183:88–95. doi: 10.1164/rccm.201006-0974OC. [DOI] [PubMed] [Google Scholar]
- Donald PR, Marais BJ, Barry CE., 3rd Age and the epidemiology and pathogenesis of tuberculosis. Lancet. 2010;375:1852–1854. doi: 10.1016/S0140-6736(10)60580-6. [DOI] [PubMed] [Google Scholar]
- Edelson BT, Cossart P, Unanue ER. Cutting edge: paradigm revisited: antibody provides resistance to Listeria infection. J. Immunol. 1999;163:4087–4090. [PubMed] [Google Scholar]
- Encinales L, Zuñiga J, Granados-Montiel J, Yunis M, Granados J, Almeciga I, Clavijo O, Awad C, Collazos V, Vargas-Rojas MI, et al. Humoral immunity in tuberculin skin test anergy and its role in high-risk persons exposed to active tuberculosis. Mol. Immunol. 2010;47:1066–1073. doi: 10.1016/j.molimm.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giri PK, Verma I, Khuller GK. Enhanced immunoprotective potential of Mycobacterium tuberculosis Ag85 complex protein based vaccine against airway Mycobacterium tuberculosis challenge following intranasal administration. FEMS Immunol. Med. Microbiol. 2006;47:233–241. doi: 10.1111/j.1574-695X.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- Glatman-Freedman A. The role of antibody-mediated immunity in defense against Mycobacterium tuberculosis: advances toward a novel vaccine strategy. Tuberculosis (Edinb.) 2006;86:191–197. doi: 10.1016/j.tube.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Glatman-Freedman A, Casadevall A. Serum therapy for tuberculosis revisited: reappraisal of the role of antibody-mediated immunity against Mycobacterium tuberculosis. Clin. Microbiol. Rev. 1998;11:514–532. doi: 10.1128/cmr.11.3.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glatman-Freedman A, Mednick AJ, Lendvai N, Casadevall A. Clearance and organ distribution of Mycobacterium tuberculosis lipoarabinomannan (LAM) in the presence and absence of LAM-binding immunoglobulin M. Infect. Immun. 2000;68:335–341. doi: 10.1128/iai.68.1.335-341.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glatman-Freedman A, Casadevall A, Dai Z, Jacobs WR, Jr., Li A, Morris SL, Navoa JA, Piperdi S, Robbins JB, Schneerson R, et al. Antigenic evidence of prevalence and diversity of Mycobacterium tuberculosis arabinomannan. J. Clin. Microbiol. 2004;42:3225–3231. doi: 10.1128/JCM.42.7.3225-3231.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover A, Ahmed MF, Singh B, Verma I, Sharma P, Khuller GK. A multivalent combination of experimental antituberculosis DNA vaccines based on Ag85B and regions of difference antigens. Microbes Infect. 2006;8:2390–2399. doi: 10.1016/j.micinf.2006.04.025. [DOI] [PubMed] [Google Scholar]
- Guirado E, Amat I, Gil O, Díaz J, Arcos V, Caceres N, Ausina V, Cardona PJ. Passive serum therapy with polyclonal antibodies against Mycobacterium tuberculosis protects against post-chemotherapy relapse of tuberculosis infection in SCID mice. Microbes Infect. 2006;8:1252–1259. doi: 10.1016/j.micinf.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Gupta S, Bhatia R, Datta KK. Serological diagnosis of childhood tuberculosis by estimation of mycobacterial antigen 60-specific immunoglobulins in the serum. Tuber. Lung Dis. 1997;78:21–27. doi: 10.1016/s0962-8479(97)90012-5. [DOI] [PubMed] [Google Scholar]
- Hamasur B, Haile M, Pawlowski A, Schröder U, Williams A, Hatch G, Hall G, Marsh P, Källenius G, Svenson SB. Mycobacterium tuberculosis arabinomannan-protein conjugates protect against tuberculosis. Vaccine. 2003;21:4081–4093. doi: 10.1016/s0264-410x(03)00274-3. [DOI] [PubMed] [Google Scholar]
- Hamasur B, Haile M, Pawlowski A, Schroder U, Kallenius G, Svenson SB. A mycobacterial lipoarabinomannan specific monoclonal antibody and its F(ab’) fragment prolong survival of mice infected with Mycobacterium tuberculosis. Clin. Exp. Immunol. 2004;138:30–38. doi: 10.1111/j.1365-2249.2004.02593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetland G, Wiker HG, Høga̋sen K, Hamasur B, Svenson SB, Harboe M. Involvement of antilipoarabinomannan antibodies in classical complement activation in tuberculosis. Clin. Diagn. Lab. Immunol. 1998;5:211–218. doi: 10.1128/cdli.5.2.211-218.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huygen K, Content J, Denis O, Montgomery DL, Yawman AM, Deck RR, DeWitt CM, Orme IM, Baldwin S, D’Souza C, et al. Immunogenicity and protective efficacy of a tuberculosis DNA vaccine. Nat. Med. 1996;2:893–898. doi: 10.1038/nm0896-893. [DOI] [PubMed] [Google Scholar]
- Igietseme JU, Eko FO, He Q, Black CM. Antibody regulation of Tcell immunity: implications for vaccine strategies against intracellular pathogens. Expert Rev. Vaccines. 2004;3:23–34. doi: 10.1586/14760584.3.1.23. [DOI] [PubMed] [Google Scholar]
- Kaufmann SH. Fact and fiction in tuberculosis vaccine research: 10 years later. Lancet Infect. Dis. 2011;11:633–640. doi: 10.1016/S1473-3099(11)70146-3. [DOI] [PubMed] [Google Scholar]
- Keyser A, Troudt JM, Taylor JL, Izzo AA. BCG sub-strains induce variable protection against virulent pulmonary Mycobacterium tuberculosis infection, with the capacity to drive Th2 immunity. Vaccine. 2011;29:9308–9315. doi: 10.1016/j.vaccine.2011.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohama H, Umemura M, Okamoto Y, Yahagi A, Goga H, Harakuni T, Matsuzaki G, Arakawa T. Mucosal immunization with recombinant heparin-binding haemagglutinin adhesin suppresses extrapulmonary dissemination of Mycobacterium bovis bacillus Calmette-Guérin (BCG) in infected mice. Vaccine. 2008;26:924–932. doi: 10.1016/j.vaccine.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Kunnath-Velayudhan S, Gennaro ML. Immunodiagnosis of tuberculosis: a dynamic view of biomarker discovery. Clin. Microbiol. Rev. 2011;24:792–805. doi: 10.1128/CMR.00014-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunnath-Velayudhan S, Salamon H, Wang HY, Davidow AL, Molina DM, Huynh VT, Cirillo DM, Michel G, Talbot EA, Perkins MD, et al. Dynamic antibody responses to the Mycobacterium tuberculosis proteome. Proc. Natl. Acad. Sci. USA. 2010;107:14703–14708. doi: 10.1073/pnas.1009080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunnath-Velayudhan S, Davidow AL, Wang HY, Molina DM, Huynh VT, Salamon H, Pine R, Michel G, Perkins MD, Xiaowu L, et al. Proteome-scale antibody responses and outcome of Mycobacterium tuberculosis infection in nonhuman primates and in tuberculosis patients. J. Infect. Dis. 2012;206:697–705. doi: 10.1093/infdis/jis421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin PL, Rodgers M, Smith L, Bigbee M, Myers A, Bigbee C, Chiosea I, Capuano SV, Fuhrman C, Klein E, Flynn JL. Quantitative comparison of active and latent tuberculosis in the cynomolgus macaque model. Infect. Immun. 2009;77:4631–4642. doi: 10.1128/IAI.00592-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Y, Yero D, Falero-Diaz G, Olivares N, Sarmiento ME, Sifontes S, Solis RL, Barrios JA, Aguilar D, Hernández-Pando R, Acosta A. Induction of a protective response with an IgA monoclonal antibody against Mycobacterium tuberculosis 16kDa protein in a model of progressive pulmonary infection. Int. J. Med. Microbiol. 2009;299:447–452. doi: 10.1016/j.ijmm.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Lux A, Aschermann S, Biburger M, Nimmerjahn F. The pro and anti-inflammatory activities of immunoglobulin G. Ann. Rheum. Dis. 2010;69(Suppl 1):i92–i96. doi: 10.1136/ard.2009.117101. [DOI] [PubMed] [Google Scholar]
- Lyashchenko K, Colangeli R, Houde M, Al Jahdali H, Menzies D, Gennaro ML. Heterogeneous antibody responses in tuberculosis. Infect. Immun. 1998;66:3936–3940. doi: 10.1128/iai.66.8.3936-3940.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyashchenko KP, Greenwald R, Esfandiari J, Chambers MA, Vicente J, Gortazar C, Santos N, Correia-Neves M, Buddle BM, Jackson R, et al. Animal-side serologic assay for rapid detection of Mycobacterium bovis infection in multiple species of free-ranging wildlife. Vet. Microbiol. 2008;132:283–292. doi: 10.1016/j.vetmic.2008.05.029. [DOI] [PubMed] [Google Scholar]
- Maglione PJ, Chan J. How B cells shape the immune response against Mycobacterium tuberculosis. Eur. J. Immunol. 2009;39:676–686. doi: 10.1002/eji.200839148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maglione PJ, Xu J, Chan J. B cells moderate inflammatory progression and enhance bacterial containment upon pulmonary challenge with Mycobacterium tuberculosis. J. Immunol. 2007;178:7222–7234. doi: 10.4049/jimmunol.178.11.7222. [DOI] [PubMed] [Google Scholar]
- Maglione PJ, Xu J, Casadevall A, Chan J. Fc gamma receptors regulate immune activation and susceptibility during Mycobacterium tuberculosis infection. J. Immunol. 2008;180:3329–3338. doi: 10.4049/jimmunol.180.5.3329. [DOI] [PubMed] [Google Scholar]
- Malik ZA, Denning GM, Kusner DJ. Inhibition of Ca(2+) signaling by Mycobacterium tuberculosis is associated with reduced phagosome-lysosome fusion and increased survival within human macrophages. J. Exp. Med. 2000;191:287–302. doi: 10.1084/jem.191.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manivannan S, Rao NV, Ramanathan VD. Role of complement activation and antibody in the interaction between Mycobacterium tuberculosis and human macrophages. Indian J. Exp. Biol. 2012;50:542–550. [PubMed] [Google Scholar]
- McClelland EE, Nicola AM, Prados-Rosales R, Casadevall A. Ab binding alters gene expression in Cryptococcus neoformans and directly modulates fungal metabolism. J. Clin. Invest. 2010;120:1355–1361. doi: 10.1172/JCI38322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossalayi MD, Vouldoukis I, Mamani-Matsuda M, Kauss T, Guillon J, Maugein J, Moynet D, Rambert J, Desplat V, Mazier D, et al. CD23 mediates antimycobacterial activity of human macrophages. Infect. Immun. 2009;77:5537–5542. doi: 10.1128/IAI.01457-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navoa JA, Laal S, Pirofski LA, McLean GR, Dai Z, Robbins JB, Schneerson R, Casadevall A, Glatman-Freedman A. Specificity and diversity of antibodies to Mycobacterium tuberculosis arabinomannan. Clin. Diagn. Lab. Immunol. 2003;10:88–94. doi: 10.1128/CDLI.10.1.88-94.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu H, Hu L, Li Q, Da Z, Wang B, Tang K, Xin Q, Yu H, Zhang Y, Wang Y, et al. Construction and evaluation of a multistage Mycobacterium tuberculosis subunit vaccine candidate Mtb10.4-HspX. Vaccine. 2011;29:9451–9458. doi: 10.1016/j.vaccine.2011.10.032. [DOI] [PubMed] [Google Scholar]
- Nosanchuk JD, Steenbergen JN, Shi L, Deepe GS, Jr., Casadevall A. Antibodies to a cell surface histone-like protein protect against Histoplasma capsulatum. J. Clin. Invest. 2003;112:1164–1175. doi: 10.1172/JCI19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivares N, León A, López Y, Puig A, Cádiz A, Falero G, Martínez M, Sarmiento ME, Fariñas M, Infante JF, et al. The effect of the administration of human gamma globulins in a model of BCG infection in mice. Tuberculosis (Edinb.) 2006;86:268–272. doi: 10.1016/j.tube.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Palma C, Iona E, Giannoni F, Pardini M, Brunori L, Fattorini L, Del Giudice G, Cassone A. The LTK63 adjuvant improves protection conferred by Ag85B DNA-protein prime-boosting vaccination against Mycobacterium tuberculosis infection by dampening IFN-gamma response. Vaccine. 2008;26:4237–4243. doi: 10.1016/j.vaccine.2008.05.050. [DOI] [PubMed] [Google Scholar]
- Pethe K, Alonso S, Biet F, Delogu G, Brennan MJ, Locht C, Menozzi FD. The heparin-binding haemagglutinin of M. tuberculosis is required for extrapulmonary dissemination. Nature. 2001;412:190–194. doi: 10.1038/35084083. [DOI] [PubMed] [Google Scholar]
- Robbins JB, Schneerson R, Szu SC. Perspective: hypothesis: serum IgG antibody is sufficient to confer protection against infectious diseases by inactivating the inoculum. J. Infect. Dis. 1995;171:1387–1398. doi: 10.1093/infdis/171.6.1387. [DOI] [PubMed] [Google Scholar]
- Rodríguez A, Tjärnlund A, Ivanji J, Singh M, García I, Williams A, Marsh PD, Troye-Blomberg M, Fernández C. Role of IgA in the defense against respiratory infections IgA deficient mice exhibited increased susceptibility to intranasal infection with Mycobacterium bovis BCG. Vaccine. 2005;23:2565–2572. doi: 10.1016/j.vaccine.2004.11.032. [DOI] [PubMed] [Google Scholar]
- Roy E, Stavropoulos E, Brennan J, Coade S, Grigorieva E, Walker B, Dagg B, Tascon RE, Lowrie DB, Colston MJ, Jolles S. Therapeutic efficacy of high-dose intravenous immunoglobulin in Mycobacterium tuberculosis infection in mice. Infect. Immun. 2005;73:6101–6109. doi: 10.1128/IAI.73.9.6101-6109.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin EJ. The granuloma in tuberculosis—friend or foe? N. Engl. J. Med. 2009;360:2471–2473. doi: 10.1056/NEJMcibr0902539. [DOI] [PubMed] [Google Scholar]
- Russo RT, Mariano M. B-1 cell protective role in murine primary Mycobacterium bovis bacillus Calmette-Guerin infection. Immunobiology. 2010;215:1005–1014. doi: 10.1016/j.imbio.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Sada E, Ferguson LE, Daniel TM. An ELISA for the serodiagnosis of tuberculosis using a 30,000-Da native antigen of Mycobacterium tuberculosis. J. Infect. Dis. 1990;162:928–931. doi: 10.1093/infdis/162.4.928. [DOI] [PubMed] [Google Scholar]
- Saunders BM, Cooper AM. Restraining mycobacteria: role of granulomas in mycobacterial infections. Immunol. Cell Biol. 2000;78:334–341. doi: 10.1046/j.1440-1711.2000.00933.x. [DOI] [PubMed] [Google Scholar]
- Schwebach JR. Sue Golding Graduate Division of Medical Sciences. Albert Einstein College of Medicine; Bronx, NY: 2002. The carbohydrate surface of M. tuberculosis: antigenicity and antibody immunity. [Google Scholar]
- Steingart KR, Dendukuri N, Henry M, Schiller I, Nahid P, Hopewell PC, Ramsay A, Pai M, Laal S. Performance of purified antigens for serodiagnosis of pulmonary tuberculosis: a meta-analysis. Clin. Vaccine Immunol. 2009;16:260–276. doi: 10.1128/CVI.00355-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suga M, Tanaka F, Muranaka H, Nishikawa H, Ando M. Effect of antibacterial antibody on bactericidal activities of superoxide and lysosomal enzyme from alveolar macrophages in rabbits. Respirology. 1996;1:127–132. doi: 10.1111/j.1440-1843.1996.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Teitelbaum R, Glatman-Freedman A, Chen B, Robbins JB, Unanue E, Casadevall A, Bloom BR. A mAb recognizing a surface antigen of Mycobacterium tuberculosis enhances host survival. Proc. Natl. Acad. Sci. USA. 1998;95:15688–15693. doi: 10.1073/pnas.95.26.15688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira FM, Teixeira HC, Ferreira AP, Rodrigues MF, Azevedo V, Macedo GC, Oliveira SC. DNA vaccine using Mycobacterium bovis Ag85B antigen induces partial protection against experimental infection in BALB/c mice. Clin. Vaccine Immunol. 2006;13:930–935. doi: 10.1128/CVI.00151-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjärnlund A, Rodríguez A, Cardona PJ, Guirado E, Ivanyi J, Singh M, Troye-Blomberg M, Fernández C. Polymeric IgR knockout mice are more susceptible to mycobacterial infections in the respiratory tract than wild-type mice. Int. Immunol. 2006;18:807–816. doi: 10.1093/intimm/dxl017. [DOI] [PubMed] [Google Scholar]
- Vordermeier HM, Venkataprasad N, Harris DP, Ivanyi J. Increase of tuberculous infection in the organs of B cell-deficient mice. Clin. Exp. Immunol. 1996;106:312–316. doi: 10.1046/j.1365-2249.1996.d01-845.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vouldoukis I, Mazier D, Moynet D, Thiolat D, Malvy D, Mossalayi MD. IgE mediates killing of intracellular Toxoplasma gondii by human macrophages through CD23-dependent, interleukin-10 sensitive pathway. PLoS ONE. 2011;6:e18289. doi: 10.1371/journal.pone.0018289. http://dx.doi.org/10.1371/journal.pone.0018289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams A, Reljic R, Naylor I, Clark SO, Falero-Diaz G, Singh M, Challacombe S, Marsh PD, Ivanyi J. Passive protection with immunoglobulin A antibodies against tuberculous early infection of the lungs. Immunology. 2004;111:328–333. doi: 10.1111/j.1365-2567.2004.01809.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Global tuberculosis report 2012. Geneva, Switzerland: 2012. http://www.who.int/tb/publications/global_report/ [Google Scholar]
- Xue T, Stavropoulos E, Yang M, Ragno S, Vordermeier M, Chambers M, Hewinson G, Lowrie DB, Colston MJ, Tascon RE. RNA encoding the MPT83 antigen induces protective immune responses against Mycobacterium tuberculosis infection. Infect. Immun. 2004;72:6324–6329. doi: 10.1128/IAI.72.11.6324-6329.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yano M, Gohil S, Coleman JR, Manix C, Pirofski LA. Antibodies to Streptococcus pneumoniae capsular polysaccharide enhance pneumococcal quorum sensing. mBio. 2011;2:00176–11. e00176–11. doi: 10.1128/mBio.00176-11. http://dx.doi.org/10.1128/mBio. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X, Prados-Rosales R, Jenny-Avital ER, Sosa K, Casadevall A, Achkar JM. Comparative evaluation of profiles of antibodies to mycobacterial capsular polysaccharides in tuberculosis patients and controls stratified by HIV status. Clin. Vaccine Immunol. 2012;19:198–208. doi: 10.1128/CVI.05550-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Zheng X, Zhang J, Zhu Y, Zhu X, Liu H, Zeng M, Graner MW, Zhou B, Chen X. CD19(+)CD1d(+)CD5(+) B cell frequencies are increased in patients with tuberculosis and suppress Th17 responses. Cell. Immunol. 2012;274:89–97. doi: 10.1016/j.cellimm.2012.01.007. [DOI] [PubMed] [Google Scholar]