Abstract
Endobronchial metastases from hepatocellular carcinoma are very rare. Up to date, no more than 7 cases were reported. The authors present a case of 20-year old female with metastatic hepatocellular carcinoma to superior lobar bronchus. Examination of cytological and small biopsy specimens obtained from bronchoscopy revealed characteristic microscopic features and immunohistochemical profile of hepatocellular carcinoma.
Keywords: Hepatocellular carcinoma, endobronchial carcinoma, cytology, fine-needle aspiration cytology
Introduction
Lung is the most common metastatic site of hepatocellular carcinoma; approximately 50% of secondary deposits are found in pulmonary parenchyma, nevertheless the endobronchial metastases are exceptionally rare. So far, the definition of endobronchial metastases has not been unified [1]; the criteria remains flexible: if the invasion of tracheobronchial structures by parenchymal or lymph node mass is included, an incidence amounts nearly 50%, but if the definition is confined to the direct metastasis to the tracheobronchial tree from the non-pulmonary malignancy the frequency is limited to 2% [2,3]. The latest studies have focused on “developmental modes” of endobronchial metastases complying with clinical and pathological features [4]. The most common sites of extrapulmonary primary tumors which have predilection to endobronchial metastases are colorectal and breast cancer as well as osteogenic sarcoma [2,3,5-7]. A single case descriptions of metastases from papillary [8] and follicular [9] thyroid carcinoma, prostatic carcinoma [10], giant-cell tumor of bone [11], malignant melanoma [12], renal-cell carcinoma [13], endometrial and uterine cervix carcinoma [14], soft tissue liposarcoma [15] or testis seminoma [16] were reported. Majority of patients with the diagnosis of hepatocellular carcinoma have distant metastases within the first year. The most frequent locations are: lungs, bones and adrenal glands [17]. However, an uncommon sites of dissemination i.e. skull [18], left atrium [19], orbit [20] were found. The Medline and Embase search (from 1980 to January 2013) by key words: (endobronchial metastases) and (hepatocellular carcinoma) revealed descriptions of 7 patients. The authors present following case with a brief review of literature.
Case presentation
A 20-year old female was admitted to the Maria Skłodowska-Curie Memorial Cancer Center and Institute of Oncology (Warsaw – Poland) with a suspicion of right lung metastatic tumor. The patient, never-smoker, complained of chest pain on the right side and dyspnea on exertion; she did not notified cough, sputum weight loss or other symptoms. Chest X-ray and computed tomography (Figure 1A) showed pathologic mass involving superior lobe of the right lung with an extension to superior and middle mediastinum; the total size was 120 x 76 x 80 mm. Central tumor necrosis and atelectasis of superior lobe were depicted. A bronchoscopy showed tumor mass which was closing superior lobar bronchus and was localized 12 mm from tracheal carina (Figure 1B). The brush cytology and biopsy specimens were carried out.
Figure 1.
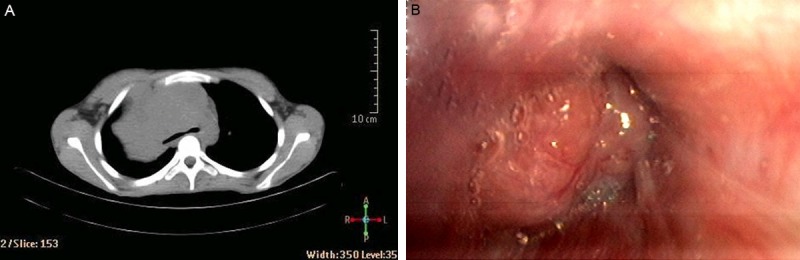
A: The computed tomography and (B) bronchoscopy imaging of the pulmonary tumor mass.
A hematoxylin-eosin staining revealed hypercellular smears with cohesive groups of malignant cells as well as numerous small groups and scattered single cells. An endothelial rimming of neoplastic cell groups was significant and characteristically CD34 (Dako Denmark, RTU, monoclonal mouse anti-human) positive. The nuclei were large and hyperchromatic without prominent nucleoli. The cytoplasm was faintly granular. Many apoptotic cells and abundant necrosis masses were noted. The tumor cells stained strongly immunohistochemically with hepatocyte (Dako Denmark, 1:25, monoclonal mouse anti-human) and alpha-1-fetoprotein (Dako Denmark, 1:400, polyclonal rabbit anti-human) antibodies. The endobronchial metastatic hepatocellular carcinoma was diagnosed. The bronchoscopic small biopsy specimen examination confirmed the cytological diagnosis (Figure 2A-D). The cytological diagnosis was made without knowledge of clinical data.
Figure 2.
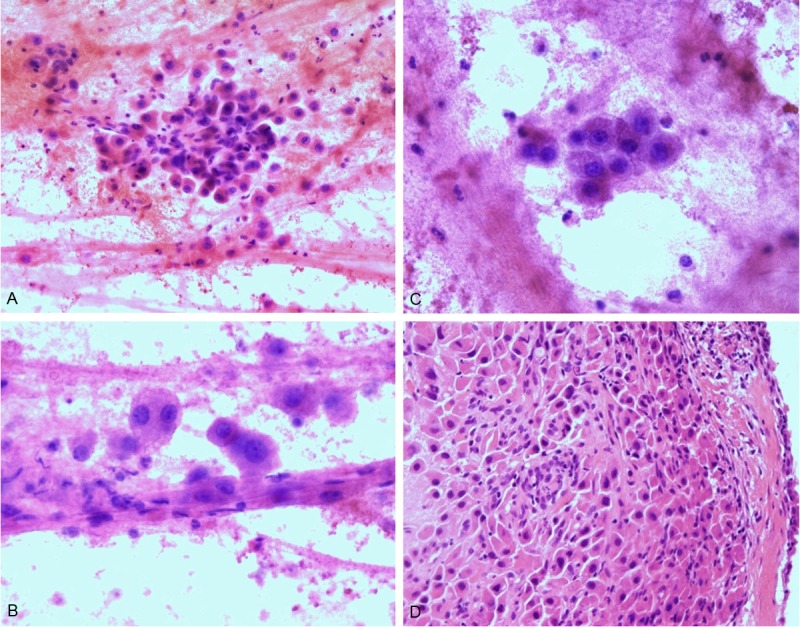
The hepatocellular carcinoma - brush cytology (A - 100x, B - 200x, C - 200x) and biopsy specimen (D - 100x).
The prior medical history revealed that two years ago patient underwent left hemihepatectomy because of left hepatic lobe tumor which was reaching an iliac ala. Microscopic examination confirmed hepatocellular carcinoma (the trabecular type). Sorafenib therapy was administrated and continued until increased toxicity appeared. The radiological imaging showed metastases to lymph nodes of vena cava region. Chemotherapy with doxorubicin, fluorouracil and cisplatin was administrated. Moreover, thermoablation of metastatic tumors was performed. Subsequently, a single renal metastasis was surgically removed. HCV status was negative and serum alpha-fetoprotein (AFP) level was not evaluated.
At present, after 6 months since the diagnosis of the endobronchial hepatocellular carcinoma metastasis, the patient is still alive and continues monotheraphy with doxorubicin.
Summary
The incidence of endobronchial metastases from extrapulmonary malignancies differs depending on the definition criteria and ranges from 2% to even 50% [1-3]. If the metastasis is limited directly to tracheobronchial tree, without its invasion by continuity from tumor mass localized in adjacent structures i.e. parenchyma or lymph nodes, the incidence rate is lower. Sorensen [21] reviewed an English language literature from 1962 to 2002 and reported 204 patients with endobronchial metastases from 20 non-pulmonary primary tumors. In majority of studies the most frequent endobronchial metastases originated from breast, colorectal and renal carcinoma [2,3,5,6].
The clinical presentation and radiological imaging of endobronchial metastases [22] are similar to primary bronchogenic carcinoma. Most patients suffer from cough, hemoptysis, chest pain, dyspnea and respiratory failure but asymptomatic cases were reported as well. The present patient complained of chest pain on the right side and dyspnea on exertion.
Kiryu et al [4] proposed four developmental modes of tracheobronchial metastases: type I – direct metastasis to the bronchus, type II – bronchial invasion by a parenchymal lesion, type III – bronchial invasion by mediastinal or hilar lymph node metastasis and type IV – peripheral lesions extended along the proximal bronchus. Type IV and I were the most frequent and amounted to 56,3% and 31,3% respectively. The authors emphasized difficulty in differentiation type II from type IV; the crucial point was the depth of invasion (mucosa/submucosa). According to above classification, case presented in following report should be classified as type III because of the superior and middle mediastinum involvement.
The radiological imaging methods as X-ray, computed tomography and magnetic resonance, are non specific for distinguishing endobronchial metastases from primary lung carcinoma. The most valuable diagnostic tool is bronchoscopy [3,23]; besides the direct visualization of tumor, the cytological and histopathological material can be obtained to specify the origin of malignancy.
The cytodiagnostic criteria of well differentiated hepatocellular carcinoma comprise: numerous stripped atypical nuclei, macronucleoli, increased mitoses and multinucleation. The architectural features include widened trabeculae, well defined capillaries transverse to tissue fragments, solid islands of hepatocytes rimmed by endothelial cells [24]. The immunohistochemistry is useful in confirmation the final diagnosis. The most specific markers of hepatocellular carcinoma are hepatocyte paraffin 1 (HepPar1) and alpha-1-fetoprotein [24].
The treatment of endobronchial metastases is difficult and should be individualized according to histopathological diagnosis, size and site of metastases and general condition of a patient.
Up to date, 8 cases of hepatocellular carcinoma endobronchial metastases were reported (4 females, 3 males, 1 lack of data). At the time of metastasis patients were from 20 to 80 years old (mean 61 years old). The only younger patient was presented in this study, the others were above 60 years old. Period between the primary tumor excision and clinically significant development of endobronchial metastasis varied from 9 to 108 months (mean 53 months). All patients were symptomatic and the most frequent manifestations included hemoptysis and cough. In majority of cases biochemical data was not available (HCV status and alpha-fetoprotein serum level). The most common developmental mode was type I and IV. The treatment options included chemotherapy, surgical treatment (pulmonectomy or lobectomy), bronchial stent placement and radiotherapy. The management depended mainly on surgical experience within particular oncology centre. At present, after 6 months since the diagnosis of the endobronchial hepatocellular carcinoma metastasis, reported patient is still alive and is receiving monotheraphy with doxorubicin. The summary of literature review was presented on Table 1.
Table 1.
Characteristics of the endobronchial metastases from hepatocellular carcinoma with literature review
| Case No | Gender | Age | Symptoms and duration | Duration of symptoms | Time from primary diagnosis | AFP level | HCV status | Lung/Lobe | Type of developmental mode | Treatment | Follow up | Author | Publication year |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 66 | Pneumonia | LD | Does not concern+ | LD | LD | Right/Upper | LD | Chemotherapy | Died 7 months | Camps C [25]# | 1988 |
| 2 | M | 61 | Hemoptysis Cough Respiratory failure | LD | 9 years | normal | LD | Right/Main | IV | LD | Died, 3 days after admission | Murayama J [26] | 1992 |
| 3 | LD | LD | LD | LD | 9 months | LD | LD | LD | LD | LD | LD | Salud A [3]## | 1996 |
| 4 | F | 61 | Hemoptysis Cough | 1 month | 16 months | 1215 ng/ml | LD | Right/Upper | I | Lobectomy | Alive, 18 months | Lee KY [27] | 2003 |
| 5 | M | 80 | Hemoptysis | LD | 2 years | 261 ng/ml | positive | Left/Lower | I | Radiation | Alive 25 months | Kido T [28] | 2005 |
| 6 | M | 65 | Hemoptysis | LD | 8 years | normal | LD | Right/Lower | I | Pulmonectomy | Alive, 6 months | Purandare NC [29] | 2009 |
| 7 | F | 71 | Progressive dyspnea Respiratory failure | 3 months | 7 years | LD | positive | Bilateral | IV | Bronchial stent placement | Died, 20 days | Uchida R [30] | 2010 |
| 8 | F | 20 | Chest pain Dyspnea on exertion | 2 months | 3 years | LD | negative | Right/Upper | III | Chemotherapy | Alive, 6 months | This case | 2013 |
LD – lack of data.
First symptoms of hepatocellular carcinoma were endobronchial metastases.
Article in Spanish.
1 case in series of 32 cases of various endobronchial metastases.
In conclusion, the endobronchial metastasis of hepatocellular carcinoma is an extremely rare phenomenon. It should be taken into consideration especially when the patient with previous history of hepatocellular carcinoma has clinical symptoms or radiological suspicion of primary lung cancer. Bronchoscopy with thorough cytological or histopathological examination remains the most useful method to limit the risk of misdiagnosis.
Disclosure of conflict of interest
None.
References
- 1.Akoglu S, Ucan ES, Celik G, Sener G, Sevinc C, Kilinc O, Itil O. Endobronchial metastases from extrathoracic malignancies. Clin Exp Metastasis. 2005;22:587–91. doi: 10.1007/s10585-005-5787-x. [DOI] [PubMed] [Google Scholar]
- 2.Katsimbri PP, Bamias AT, Froudarakis ME, Peponis IA, Constantopoulos SH, Pavlidis NA. Endobronchial metastases secondary to solid tumors: report of eight cases and review of the literature. Lung Cancer. 2000;28:163–70. doi: 10.1016/s0169-5002(99)00134-8. [DOI] [PubMed] [Google Scholar]
- 3.Salud A, Porcel JM, Rovirosa A, Bellmunt J. Endobronchial metastatic disease: analysis of 32 cases. J Surg Oncol. 1996;62:249–52. doi: 10.1002/(SICI)1096-9098(199608)62:4<249::AID-JSO4>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Kiryu T, Hoshi H, Matsui E, Iwata H, Kokubo M, Shimokawa K, Kawaguchi S. Endotracheal/endobronchial metastases: clinicopathologic study with special reference to developmental modes. Chest. 2001;119:768–75. doi: 10.1378/chest.119.3.768. [DOI] [PubMed] [Google Scholar]
- 5.Ohno T, Nakayama Y, Kurihara T, Ichikawa H, Tsuda K, Ishida T, Hirato J, Suzuki Y. Endobronchial metastasis of breast cancer 5 years after breast-conserving therapy. Int J Clin Oncol. 2001;6:101–4. doi: 10.1007/pl00012083. [DOI] [PubMed] [Google Scholar]
- 6.Mogulkoc N, Goker E, Atasever A, Veral A, Ozkok S, Bishop PW. Endobronchial metastasis from osteosarcoma of bone: treatment with intraluminal radiotherapy. Chest. 1999;116:1811–4. doi: 10.1378/chest.116.6.1811. [DOI] [PubMed] [Google Scholar]
- 7.Heitmiller RF, Marasco WJ, Hruban RH, Marsh BR. Endobronchial metastasis. J Thorac Cardiovasc Surg. 1993;106:537–42. [PubMed] [Google Scholar]
- 8.Chen WH, Wang YH, Lu YC, Huang CC, Wong SL. Endobronchial metastasis from an occult papillary thyroid carcinoma: a case report. Changgeng Yi Xue Za Zhi. 1998;21:200–5. [PubMed] [Google Scholar]
- 9.Kushwaha RA, Verma SK, Mahajan SV. Endobronchial metastasis of follicular thyroid carcinoma presenting as hemoptysis: a case report. J Cancer Res Ther. 2008;4:44–5. doi: 10.4103/0973-1482.39606. [DOI] [PubMed] [Google Scholar]
- 10.Gerogianni I, Gravas S, Papadopoulos D, Terzis A, Nakou M, Tzortzis V, Gourgoulianis K, Melekos MD. Endobronchial metastasis from prostate cancer. Int Urol Nephrol. 2008;40:961–4. doi: 10.1007/s11255-008-9369-0. [DOI] [PubMed] [Google Scholar]
- 11.Boghani A, Gayathri K, Ratnakar KS. Endobronchial metastasis from giant cell tumor of bone. Chest. 1994;106:1599–601. doi: 10.1378/chest.106.5.1599. [DOI] [PubMed] [Google Scholar]
- 12.Seam N, Khosla R. Metastatic endobronchial melanoma. Respiration. 2009;77:214. doi: 10.1159/000098403. [DOI] [PubMed] [Google Scholar]
- 13.Barthwal MS, Chatterji RS, Jawed KZ. Endobronchial metastases from renal cell carcinoma. J Assoc Physicians India. 2003;51:1027–8. [PubMed] [Google Scholar]
- 14.Kim YS, Chang J, Shin DH, Kim HS, Kim SK. Endobronchial metastasis of uterine cervix cancer: a two case reports and a review of the literature. Yonsei Med J. 2002;43:547–52. doi: 10.3349/ymj.2002.43.4.547. [DOI] [PubMed] [Google Scholar]
- 15.Nair S, Kumar P, Ladas G. Intratracheal metastasis secondary to soft tissue liposarcoma. Singapore Med J. 2007;48:e81–3. [PubMed] [Google Scholar]
- 16.Ozsu S, Erol MM, Oztuna F, Ersoz S, Kavgaci H, Aksoy HZ. Endobronchial metastasis from testicular seminoma. Med Princ Pract. 2008;17:493–5. doi: 10.1159/000151573. [DOI] [PubMed] [Google Scholar]
- 17.Herold CJ, Bankier AA, Fleischmann D. Lung metastases. Eur Radiol. 1996;6:596–606. doi: 10.1007/BF00187656. [DOI] [PubMed] [Google Scholar]
- 18.Hsieh CT, Sun JM, Tsai WC, Tsai TH, Chiang YH, Liu MY. Skull metastasis from hepatocellular carcinoma. Acta Neurochir (Wien) 2007;149:185–90. doi: 10.1007/s00701-006-1071-3. [DOI] [PubMed] [Google Scholar]
- 19.Agelopoulou P, Kapatais A, Varounis C, Grassos C, Kalkandi E, Kouris N, Pierakeas N, Babalis D. Hepatocellular carcinoma with invasion into the right atrium. Report of two cases and review of the literature. Hepatogastroenterology. 2007;54:2106–8. [PubMed] [Google Scholar]
- 20.Font RL, Maturi RK, Small RG, Garcia-Rojas M. Hepatocellular carcinoma metastatic to the orbit. Arch Ophthalmol. 1998;116:942–5. doi: 10.1001/archopht.116.7.942. [DOI] [PubMed] [Google Scholar]
- 21.Sorensen JB. Endobronchial metastases from extrapulmonary solid tumors. Acta Oncol. 2004;43:73–9. doi: 10.1080/02841860310018053. [DOI] [PubMed] [Google Scholar]
- 22.Rivera-Garcia R, White CS, Templeton PA. Lung cancer: value of various imaging modalities. Clin Lung Cancer. 1999;1:130–6. doi: 10.3816/clc.1999.n.010. discussion 137. [DOI] [PubMed] [Google Scholar]
- 23.Lossos IS. Sources of endobronchial metastases. Chest. 1990;98:1308–9. doi: 10.1378/chest.98.5.1308-b. [DOI] [PubMed] [Google Scholar]
- 24.Onofre AS, Pomjanski N, Buckstegge B, Bocking A. Immunocytochemical diagnosis of hepatocellular carcinoma and identification of carcinomas of unknown primary metastatic to the liver on fine-needle aspiration cytologies. Cancer. 2007;111:259–68. doi: 10.1002/cncr.22768. [DOI] [PubMed] [Google Scholar]
- 25.Camps C, Soler JJ, Juan G, Navarro R, Lloret J, Gonzalez G. [An unusual form of metastasis of hepatocarcinoma: endobronchial metastasis] . Rev Esp Enferm Apar Dig. 1988;74:155–7. [PubMed] [Google Scholar]
- 26.Murayama J, Naitoh T, Doi M, Yano H, Ohtsuka M, Yoshizawa Y, Hasegawa S. [A case of small liver cancer presenting as a huge mediastinal mass] . Nihon Kyobu Shikkan Gakkai Zasshi. 1992;30:708–13. [PubMed] [Google Scholar]
- 27.Lee KY, Ryu SJ, Joo M. Endobronchial metastasis of hepatocellular carcinoma. Yonsei Med J. 2003;44:544–7. doi: 10.3349/ymj.2003.44.3.544. [DOI] [PubMed] [Google Scholar]
- 28.Kido T, Iwanaga T, Takata S, Kaketa Y, Kawanami T, Kido M. [A case of solitary endobronchial metastasis of hepatocellular carcinoma] . Nihon Kokyuki Gakkai Zasshi. 2005;43:422–6. [PubMed] [Google Scholar]
- 29.Purandare NC, Pramesh CS, Rangarajan V, Shet T, Shukla PJ, Mistry RC. Hepatocellular carcinoma recurring as isolated endobronchial metastasis 8 years after primary surgery. J Thorac Imaging. 2009;24:147–9. doi: 10.1097/RTI.0b013e3181972368. [DOI] [PubMed] [Google Scholar]
- 30.Uchida R, Masugi Y, Nishizawa T, Kimura T, Yamada T. Extensive endobronchial growth of metastatic hepatocellular carcinoma resulting in respiratory failure: a case report. Pathol Res Pract. 2010;206:116–20. doi: 10.1016/j.prp.2009.03.001. [DOI] [PubMed] [Google Scholar]


