Abstract
Background
Thyroid and parathyroid procedures historically have been viewed as inpatient procedures. Due to advancements in surgical techniques, these procedures were transferred from the inpatient operating room (OR) to the outpatient OR at a single academic institution approximately seven years ago. The goal of this study is to determine whether this change has decreased turnover times and maximized OR utilization.
Methods
We performed a retrospective review of 707 patients undergoing thyroid (34%) and parathyroid (66%) procedures by a single surgeon at our academic institution between 2005 and 2008. Inpatient and outpatient groups were compared using student’s t-test, Chi-squared test or the Kruskal-Wallis test where appropriate. Multiple regression analysis was used to determine how patient and hospital factors influenced turnover times.
Results
Turnover times were significantly lower in the outpatient OR (mean 18 min, ± 0.7 min) when compared with the inpatient OR (mean 36 min ±1.4 min) (p<0.001). When compared by type of procedure, all turnover times remained significantly lower in the outpatient OR. Patients in both OR’s were similar in age, gender, and co-morbidities. However, inpatients had a higher mean ASA score (2.30 vs. 2.13, p<0.001) and were more likely to have an operative indication of cancer (23.1% vs. 9.2%, p<0.001). Using multiple regression, the inpatient OR remained highly significantly associated with higher turnover times when controlling for these small differences (p<0.001).
Conclusion
Endocrine procedures performed in the outpatient OR have significantly faster turnover times leading to cost savings and greater OR utilization for hospitals.
Keywords: Turnover time, Outpatient operating room, Ambulatory procedure, Thyroidectomy, Parathyroidectomy, Operating room efficiency, Resource utilization, Process measures
Introduction
Increasing operating room (OR) costs have driven efforts to improve OR utilization and efficiency. Estimates have shown that nearly three quarters of an OR’s working day are wasted each week due to inappropriately prepared patients, unavailability or insufficient OR staff, OR assignment to emergency procedures or congestion in postoperative care units1. Therefore, it is economically important for medical institutions to allocate OR resources and staff efficiently.
Turnover time, or the time required for the anesthesia staff to finish procedures on the first surgical patient and to begin procedures on the upcoming surgical patient after the surgery suite has been sterilized, is often considered an area of OR utilization that requires improvement2. Surgeons frequently assert that additional surgical cases could be added if turnover times were reduced. While this continues to be debated, the largest cost reductions associated with lower turnover times come from more predictable OR schedules, which allow more efficient staffing2,3.
A common strategy for increased OR utilization has been to develop an outpatient OR that is dedicated to less complex cases with more predictable case times. Many surgeries that were previously performed as inpatient procedures, including tonsillectomies and cholecystectomies, are now routinely performed on an outpatient basis4. Outpatient ORs can increase operative time efficiency and therefore increase OR utilization by good patient selection and more efficient staffing5.
Thyroid and parathyroid procedures have historically been viewed as inpatient procedures because of possible complications including hematoma, laryngeal nerve damage and airway compromise6,7. However, with advancements in surgical techniques outpatient thyroid surgery has been shown to be effective and safe8–11. Consequently, thyroid and parathyroid procedures were transferred from the inpatient OR to the outpatient OR at our academic institution approximately seven years ago. The goal of this study was to determine if this change has decreased turnover times, and hence maximized OR utilization.
Methods
We performed a retrospective review of all patients who underwent thyroidectomy or parathyroidectomy procedures by a single surgeon at the University of Wisconsin Hospital between 2005 and 2008. During this time period the surgeon operated one day per week in the outpatient OR and one day per week in the inpatient OR. There was a similar case mix in each location. The anesthesia staffing was the same in both the inpatient and outpatient ORs. The team consists of a mixture of CRNAs and residents that rotate through both ORs. Over the study period, a total of 1355 procedures during our study period. Of these, 707 met the inclusion criteria (Figure 1). Dates with three or more thyroid and/or parathyroid procedures were included in the study to provide sufficient turnover times. Dates with adrenal procedures were excluded due to lack of comparability between the groups. Additionally, surgery dates that included various general surgery procedures (appendectomy, etc.) between endocrine procedures were excluded.
Figure 1.
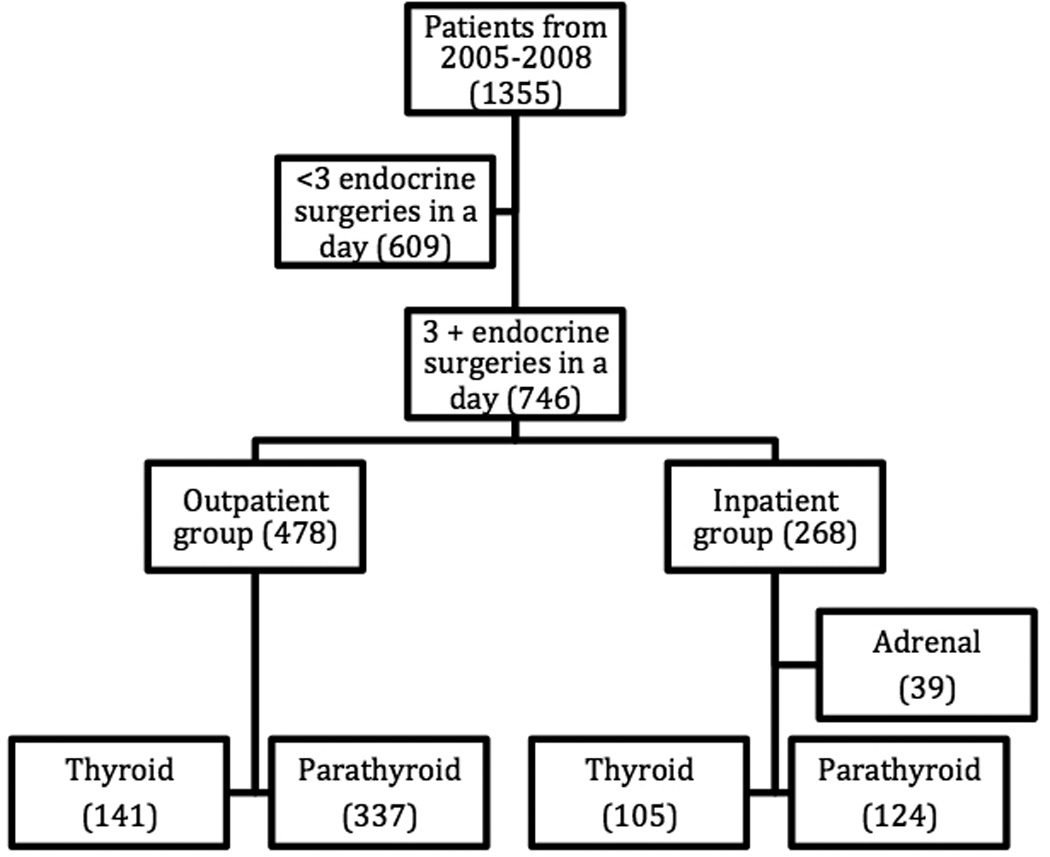
shows the exclusion criteria for the study. Days with less than 3 endocrine surgeries that ran consecutively were excluded from the study due to insufficient turnover times. Adrenal procedures were only performed in the inpatient OR over the study time period, so these procedures were excluded due to no comparative group in the outpatient OR.
Patient demographics, operative procedure performed, final pathology, and postoperative complications were obtained from our prospectively maintained Endocrine Surgery database. Electronic anesthesia reports were reviewed for American Society of Anesthesiologists (ASA) physical status classification. Additionally, time data were recorded from these records including: anesthesia start, procedure start, procedure finish, and anesthesia end times. These time data were used to calculate the following: anesthesia time before incision, operative procedure time, anesthesia time after closing, total anesthesia time, and turnover times.
The data for the inpatient and outpatient surgery groups that underwent thyroid and parathyroid procedures were analyzed using SPSS statistical software. All time data were measured in minutes. Continuous variables were compared using an independent student t-test using Levene’s test for equality of variability. Continuous variables in a non-normal distribution were analyzed using the Kruskal-Wallis test. Categorical variables were cross tabulated and analyzed using the chi-squared test. Multiple regression analysis was used to determine how patient and hospital factors influenced turnover times. P values <0.05 were considered significant.
Results
Patients treated in the outpatient and inpatient ORs were similar in age, gender, BMI, and co-morbidities such as hypertension, diabetes mellitus, and coronary artery disease (Table 1). However, there were several factors that were significantly different between the two groups. Inpatients had a slightly higher mean ASA score (2.30 vs. 2.13, p<0.001), were more likely to have an operative indication of cancer, were more likely to have a reoperative procedure and more likely to have renal failure/insufficiency (Table 1).
Table 1.
Patient demographics
| Variable | Inpatient | Outpatient | p-Value |
|---|---|---|---|
| N | 229 | 478 | - |
| Age | 57.1 ± 1.1 | 57.2 ± 0.7 | 0.97 |
| Female | 74.7% (171) | 75.3% (375) | 0.29 |
| BMI | 30.6 ± 0.5 | 29.8 ± 0.4 | 0.18 |
| Indication of cancer | 23.1% (53) | 9.2% (44) | <0.01 |
| Reoperative procedure | 17.9% (41) | 10.3% (49) | 0.005 |
| Hypertension | 59.0% (135) | 55.2% (264) | 0.37 |
| Diabetes mellitus | 18.3% (42) | 15.5% (74) | 0.33 |
| Coronary artery disease | 8.7% (20) | 7.3% (35) | 0.55 |
| Smoking | 34.9% (80) | 35.4% (169) | 0.93 |
| Alcohol consumption | 42.4% (97) | 46.0% (220) | 0.38 |
| Sleep apnea | 14.0% (32) | 15.7% (75) | 0.58 |
| Renal failure | 18.8% (43) | 6.7 % (32) | <0.01 |
The turnover times were significantly lower in the outpatient OR when compared with the inpatient OR (Table 2). The overall outpatient OR turnover times were nearly twice as fast when compared to the inpatient OR turnover times (mean 18.5 min ± 0.5 vs 36.5 min ± 1.3) (p<0.001). When compared by type of procedure performed, all turnover times remained significantly lower in the outpatient OR, with reductions of over 20 minutes recorded (Table 2).
Table 2.
Turnover Times
| Inpatient (min ± SEM) |
Outpatient (min ± SEM) |
Difference (min) |
p- value |
|
|---|---|---|---|---|
| Overall | 36.5 ± 1.3 (n = 164) | 18.5 ± 0.5 (n = 348) | 18.0 | <0.001 |
| Thyroid/thyroid | 34.0 ± 2.5 (n = 29) | 17.0 ± 1.2 (n = 26) | 17.0 | <0.001 |
| Parathyroid/parathyroid | 35.6 ± 2.0 (n = 56) | 19 ± 1.0 (n = 205) | 16.6 | <0.001 |
| Different neck procedure | 38.1 ± 3.1 (n = 79) | 17.8 ± 1.4 (n = 117) | 20.3 | <0.001 |
In addition to the out of room turnover time, we also analyzed the in room anesthesia times. The anesthesia times before incision time were four minutes shorter in the outpatient OR (mean 18.5 min ± 0.3 min) than in the inpatient OR (mean 22.8 min ± 1.0 min) (p=0.005). Similarly, anesthesia times after conclusion of the surgical procedure were one minute shorter when comparing the outpatient OR (mean 9.7 min ± 0.2 min) to the inpatient OR (mean 10.8 min ± 0.5 min). Case times were longer in the inpatient OR (mean 87 min ± 2.0 min) when compared to the outpatient OR (mean 70 min ± 2.5 min) (p<0.001).
After determining the binary significance of each variable when comparing the inpatient and outpatient ORs, those variables that were significant were analyzed together using multiple regression. The variables analyzed included: patient age, ASA classification, reoperative procedures, operative indication for cancer, renal failure and whether the procedure was performed in the inpatient or outpatient OR. When analyzed using multiple regression, the inpatient OR was significantly associated with higher turnover times (Table 3). In this model, ASA classification (p = 0.032) and an operative indication for cancer (p = 0.007) were also associated with higher turnover times. However, the inpatient/outpatient OR status was the dominant factor influencing turnover times.
Table 3.
Multiple regression analysis
| Variable | Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Age | −0.02 | 0.57 | [−0.10, 0.06] |
| Inpatient/Outpatient | 17.0 | <0.01 | [14.4, 19.6] |
| ASA Classification | 2.5 | 0.03 | [0.22, 4.85] |
| Reoperative | 1.6 | 0.37 | [−1.93, 5.22] |
| Cancer | 5.5 | <0.01 | [1.48, 9.46] |
| Renal Failure | −0.8 | 0.66 | [−4.56, 2.89] |
Overall p-value for this model <0.001
Discussion
This study compared turnover times of endocrine procedures performed in an inpatient and outpatient OR. We showed that turnover times decrease significantly when comparing the inpatient and outpatient ORs, with reductions of nearly 20 minutes between cases. Turnover times were significantly lower when comparing each individual procedure turnover times, and were greatest when transitioning from a thyroid to a parathyroid procedure, or vice versa (Table 2). Additionally, the anesthesia time before the incision and the anesthesia time after incision closure were both significantly lower, which further accentuates the difference in turnover times.
Our data supports others that have found reduced anesthesia in-room time in an outpatient OR when compared to an inpatient OR12. Our study showed a reduction in turnover times of nearly 20 minutes when comparing the inpatient to outpatient OR’s, which is similar to other studies, but the magnitude of reduction was greater. Kenyon et al previously reported a reduction in turnover times of 7.1 minutes when changing from a standard OR to a minimally invasive suite13. Though our data shows a greater reduction, this correlation between studies supports a universal reduction in turnover times when changing from an inpatient OR to an outpatient OR. These reductions in turnover times are often attributed to decreased case complexity and lower patient acuity. However, our study design showed that case mix, patient demographics and co-morbidities were similar between the inpatient and outpatient OR’s. Therefore, decreased case complexity and lower patient acuity are not the only factors contributing to the decreased turnover times. While our study focused only on parathyroid and thyroid procedures, so that we could control for case mix and complexity, we feel that these findings are likely generalizable to any procedure that could be performed in either an inpatient or outpatient setting (i.e laparoscopic cases, breast cases, skin cases, etc).
The total time difference of 23 minutes between the two groups in this study indicates significantly higher OR utilization in the outpatient OR. It is estimated that the cost of a single OR to a patient or health insurance provider is approximately $20 per minute14. Therefore, a cost savings of $460 per procedure can be saved through overall time reductions when comparing the outpatient and inpatient ORs in this study. With an average of 3 to 4 endocrine cases performed per day in the outpatient OR during the study period, there could be a cost reduction between $1,380 and $1,840 per day through reductions in turnover times. Costs of additional medications, beds and additional staff should be added to the above1, and can lead to an even greater cost savings.
While the costs directly associated with reduced turnover times are significant, the largest cost savings may come from reduced OR staffing15. The lower turnover times achieved in the outpatient OR require less OR workload. Consequently, OR staffing costs can be reduced. It is estimated that a reduction in turnover times of 10 to 19 minutes would reduce OR staffing costs by 2.5% to 4.0%15.
Recent studies have shown that turnover time improvement can result from a variety of factors. Turnover times were reduced by maintaining a fixed OR staff with dedicated manual tasks as well as instituting a more defined protocol for the OR staff2,16,17. The greatest reductions in turnover times were observed when similar procedures were performed consecutively, as was the case in this study. Also, because nurses and physicians are generally employed by different entities, their motivation for shorter turnover times might not be the same16. Turnover times can be reduced through OR staffing changes aimed at greater efficiency. At our institution the inpatient OR staff are on shifts. The outpatient OR uses a different staffing model that requires the staff only be present until the OR has been sterilized and prepared for the next day’s procedures. We believe that this difference in incentive has driven faster turnover times and improved OR efficiency at our institution, and should be researched in the future to determine if a similar staffing model in the inpatient OR could improve turnover times.
Whether reduced turnover time can lead to additional surgical cases remains a controversial topic. In a recent study, turnover times were reduced by 16 minutes after implementing a new staffing model. This resulted in one additional 90-minute procedure during the study16. However, prior research showed that decreasing turnover time would only predictably allow an additional case if all procedures were consistently less than 75 minutes3,18. The average case time of procedures performed in the outpatient OR for this study was 70 minutes. This indicates that another case could be added reliably in the outpatient OR.
Limitations of our study include the retrospective nature, the single institution, as well as the statistical differences between the groups at baseline. The inpatient OR group had a statistically higher ASA classification, was more likely to have an operative indication of cancer, to be a reoperative procedure and to have renal failure/insufficiency. These differences were likely due to selection bias, as the more complex cases were electively performed in the inpatient OR during the study period. While cancer and reoperative procedures likely impacted actual operative time, they should not have had a major impact on equipment needs or turnover time. Renal failure patients were done in the main operating room due to the need for dialysis in the immediate perioperative period. To try to control for these differences we did a multivariate analysis, which showed only ASA classification and indication of cancer remained significant. However, the inpatient/outpatient OR status showed a much stronger correlation to longer turnover times than either of these factors.
In conclusion, we found that thyroid and parathyroid procedures performed in an outpatient OR have shorter turnover times when compared to an inpatient OR. This improvement leads to decreased costs through reduced OR time and reduced staffing.
Acknowledgments
I would like to thank the Department of Surgery and the Shapiro Summer Research Program provided funding for this research
References
- 1.Weinbroum Aa, Ekstein P, Ezri T. Efficiency of the operating room suite. Am J Surg. 2003;185(3):244–250. doi: 10.1016/s0002-9610(02)01362-4. [DOI] [PubMed] [Google Scholar]
- 2.Stepaniak PS, Vrijland WW, de Quelerij M, de Vries G, Heij C. Working with a fixed operating room team on consecutive similar cases and the effect on case duration and turnover time. Arch Surg. 2010;145(12):1165–1170. doi: 10.1001/archsurg.2010.255. [DOI] [PubMed] [Google Scholar]
- 3.Dexter F, Coffin S, Tinker JH. Decreases in anesthesia-controlled time cannot permit one additional surgical operation to be reliably scheduled during the workday. Anesth Analg. 1995;81(6):1263–1268. doi: 10.1097/00000539-199512000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Terris DJ, Moister B, Seybt MW, Gourin CG, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg. 2007;136(4):556–559. doi: 10.1016/j.otohns.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Brenn BR, Reilly JS, Deutsch ES, Hetrick MH, Cook SC. Analysis of Efficiency of Common Otolaryngology Operations. 2012;129:435–437. doi: 10.1001/archotol.129.4.435. [DOI] [PubMed] [Google Scholar]
- 6.Vashishta R, Mahalingam-Dhingra A, Lander L, Shin EJ, Shah RK. Thyroidectomy Outcomes: A National Perspective. Otolaryngol Head Neck Surg. 2012 doi: 10.1177/0194599812454401. [DOI] [PubMed] [Google Scholar]
- 7.Youngwirth L, Benavidez J, Sippel R, Chen H. Postoperative parathyroid hormone testing decreases symptomatic hypocalcemia and associated emergency room visits after total thyroidectomy. Surg. 2010;148(4):841–844. doi: 10.1016/j.surg.2010.07.038. discussion 844–6. [DOI] [PubMed] [Google Scholar]
- 8.Hessman C, Fields J, Schuman E. Outpatient thyroidectomy: is it a safe and reasonable option? Am J Surg. 2011;201(5):565–568. doi: 10.1016/j.amjsurg.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 9.Hall BL, Hirbe M, Yan Y, et al. Thyroid and parathyroid operations in veterans affairs and selected university medical centers: results of the patient safety in surgery study. J Am Coll Surg. 2007;204(6):1222–1234. doi: 10.1016/j.jamcollsurg.2007.02.073. [DOI] [PubMed] [Google Scholar]
- 10.Mazeh H, Khan Q, Schneider DF, et al. Same-day thyroidectomy program: Eligibility and safety evaluation. Surg. 2012;152(6):1133–1141. doi: 10.1016/j.surg.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 11.Tuggle CT, Roman S, Udelsman R, Sosa JA. Same-day thyroidectomy: a review of practice patterns and outcomes for 1,168 procedures in New York State. Ann Surg Oncol. 2011;18(4):1035–1040. doi: 10.1245/s10434-010-1398-0. [DOI] [PubMed] [Google Scholar]
- 12.Hsiao KC, Machaidze Z, Pattaras JG. Time management in the operating room: an analysis of the dedicated minimally invasive surgery suite. JSLS : Journal of the Society of Laparoendoscopic Surgeons / Society of Laparoendoscopic Surgeons. 2004;8(4):300–303. [PMC free article] [PubMed] [Google Scholar]
- 13.Kenyon TA, Urbach DR, Speer JB, et al. Dedicated minimally invasive surgery suites increase operating room efficiency. Surg Endosc. 2001;15(10):1140–1143. doi: 10.1007/s004640080092. [DOI] [PubMed] [Google Scholar]
- 14.Park KW, Dickerson C. Can efficient supply management in the operating room save millions? Curr Opin Anesth. 2009;22(2):242–248. doi: 10.1097/ACO.0b013e32832798ef. [DOI] [PubMed] [Google Scholar]
- 15.Dexter F, Abouleish AE, Epstein RH, Whitten CW, Lubarsky Da. Use of Operating Room Information System Data to Predict the Impact of Reducing Turnover Times on Staffing Costs. Anesth Analg. 2003:1119–1126. doi: 10.1213/01.ANE.0000082520.68800.79. [DOI] [PubMed] [Google Scholar]
- 16.Cendán JC, Good M. Interdisciplinary work flow assessment and redesign decreases operating room turnover time and allows for additional caseload. Arch Surg. 2006;141(1):65–69. doi: 10.1001/archsurg.141.1.65. discussion 70. [DOI] [PubMed] [Google Scholar]
- 17.van Det MJ, Meijerink WJHJ, Hoff C, Pierie JPEN. Interoperative efficiency in minimally invasive surgery suites. Surg Endosc. 2009;23(10):2332–2337. doi: 10.1007/s00464-009-0335-4. [DOI] [PubMed] [Google Scholar]
- 18.Mazzei WJ. Operating room start times and turnover times in a university hospital. Journal of clinical anesthesia. 6(5):405–408. doi: 10.1016/s0952-8180(05)80011-x. [DOI] [PubMed] [Google Scholar]


