Abstract
We describe an innovative program at the University of California, Davis for students to engage in clinical needs finding. Using a team-based approach, students participated in clinical rotations to observe firsthand the needs of clinicians at the university affiliated medical center. The teams were asked to develop documentary-style videos to capture key experiences that would allow future viewers to use the videos as “virtual” clinical rotations. This was conceived as a strategy to allow students in prohibitively large classes, or students in programs at institutions without associated medical or veterinary school programs, to experience clinical rotations and perform needs assessments. The students' perspectives on the experience as well as instructor analysis of best practices for this type of activity are presented and discussed. We found that the internship experience was valuable to the students participating, by not only introducing the practice of needs finding but for increasing the students' confidence in the practice of engineering design and their ability to work independently. The videos produced were of such high quality that instructors from other institutions have requested copies for instructional use. Virtual clinical rotations through video experiences may provide a reasonable substitute for students who do not have the ability to participate in rotations in person.
Keywords: Design Education, Biomedical Engineering, Clinical Rotation, Biomedical Design
Introduction
Design education is a critical component of the undergraduate engineering curriculum and a major assessment factor in the accreditation process. All accredited engineering programs require a design component in which students must design a solution to a real world problem. Most engineering design training requires a cycle of DESIGN-IMPLEMENT-TEST(1, 2). In biomedical engineering, our students are further challenged in that they are asked to complete interdisciplinary projects with clear medical or biological applications. Traditionally, the Biomedical Engineering (BME) course instructors have solicited and received project ideas from biomedical companies, clinicians at the medical and veterinary schools, other faculty, and local organizations (e.g. Easter Seals requests projects for persons with disabilities). Prospective “clients” are asked to describe problems that require an engineering solution, but leave the problem statement open ended. Requests typically should not include a suggested solution, unless the need is for refinement or improvement of an existing device or process. The students, thus, are required to generate new concepts as part of the design process. However, the use of client-submitted project ideas excludes students from an important first step in the process of product design and innovation: identifying needs. Clinical needs finding is the process of examining current clinical practices, typically through observation and interview, in order to understand the daily challenges faced by medical practitioners (3, 4). The observer can then make an informed diagnosis of sources of clinical difficulties in order to formulate a clear problem statement. The identified needs will ultimately be translated to a set of product specifications that must be met by the proposed solution.
There are many examples of products that were designed without adequate consideration of the end user's needs (4, 5). For example, Tom Kelley, author of The Art of Innovation, discusses the development of the children's toothbrush, and points out how observation was key to designing the children's toothbrush with the fat handle and larger heads that we are familiar with today. Early children's toothbrushes were scaled down versions of the adult toothbrush. But through observation it was clear that a miniature toothbrush was difficult for children, who have limited hand dexterity compared to adults, to operate, and actually a larger handle was easier for a child to manipulate (6). Observation of children attempting to brush their teeth with the miniature brushes was key to identifying the design changes that needed to be made.
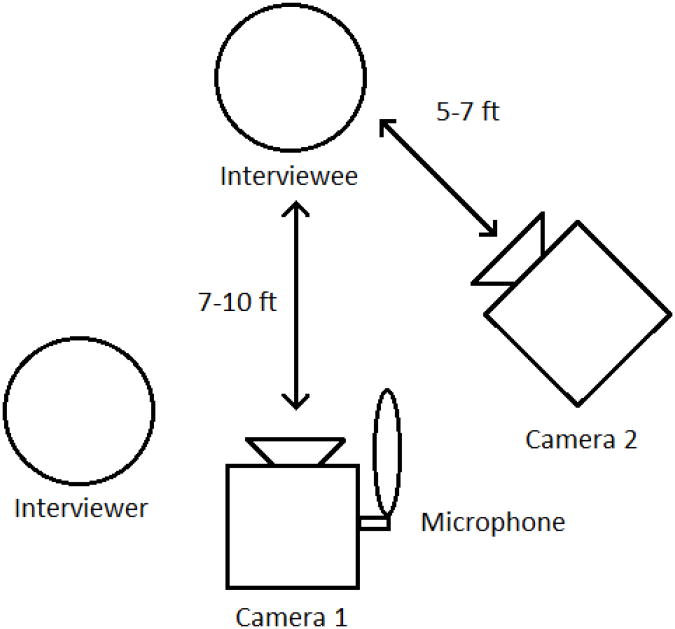
Along these lines, the “fresh eyes” of engineers can bring a new perspective to clinical problems, and an engineer may assess upon observation that the actual source of a problem differs from the clinician client's perceived source. This exemplifies one of the great benefits of interdisciplinary approaches to problem solving. Needs finding is also an approach to identifying opportunities and new markets for innovation efforts; thus, needs finding has come to be recognized as an important part of the design process. We felt that the improved process of NEEDS-DESIGN-IMPLEMENT-TEST would result in more robust solutions and product designs. An engineering design cycle that incorporates needs finding is illustrated in Figure 1. The process of design and prototyping is a cycle that feeds back for refinements until the cycle is exited with a final product. From an educational perspective, the experience of needs finding develops students' ability to communicate across disciplinary boundaries and helps them to understand why designs must meet multiple realistic constraints.
Figure 1. The Engineering Design Cycle.

The engineering design process begins with the identification of a need, leading into the development of a design and eventual implementation.
 Design cycle,
Design cycle,
 Input components
Input components
We have developed an interdisciplinary design program that will guide undergraduate students at the senior level through all the steps of the translational product design process from needs finding to commercialization. This is a campus-wide, integrative, interdisciplinary experience involving participants from the College of Engineering, Graduate School of Management, School of Medicine, School of Veterinary Medicine, Technology Transfer Office, and Design department. Clinical needs finding was added to the senior design experience by incorporating clinical rotations as an option for students in design. However, the growing number of biomedical engineering students may soon make it impractical for every student to participate in clinical rotations. Furthermore, it is also sometimes difficult for students to make time in their course schedule for a clinical rotation at the UC Davis Medical Center, located in Sacramento, some distance away from the main UC Davis campus. With this in mind, we created a novel Clinical Needs Finding Video Internship that is offered to all undergraduates, specifically targeting the students entering their senior year. The students, working in teams, participate in a clinical immersion, needs finding experience and are charged with producing a documentarystyle video that captures the key observations/conversations that allow for the identification of unmet needs. In the future, students could engage in “virtual rotations”, using these videos to identify potential problems that could be used to create their own senior design projects. Furthermore, these videos could be of use to programs at institutions that do not have affiliated medical schools or veterinary programs. The Clinical Needs Finding Video Internship is an effective tool to teach interns how to identify clinical needs as a preliminary step in the engineering design process and could be a useful alternative to an in-person clinical rotation for viewers of the resulting videos. In this paper we describe the internship experience, discuss effective practices, and include extensive coverage of the students' direct perspective of the rotation experience.
Internship Logistics
A Biomedical Engineering faculty member administered the internship, supervised the interns, and was responsible for organizing the clinical rotations. Three clinicians from the Emergency Medicine, Intensive Care Unit, and Pathology departments at the UC Davis Medical Center (UCDMC) were recruited as lead clinical contacts for the rotations; they were responsible for orienting the students to the clinics and securing required paperwork to allow the students to work in the hospitals. The students started in the departments of these lead contacts, and then rotated through other departments as more contacts were made. Many clinicians in other departments permitted the students to rotate through their units, allowing the students to experience a variety of departments throughout the internship.
Small teams of 4 to 5 interns were selected to participate in this seven-week, fulltime internship. Two groups have rotated through this program to date. Initially, two weeks were spent on-site in the UCDMC where the students were allowed to freely observe medical processes and procedures. The next two weeks were spent filming, and the final three weeks were devoted to editing the acquired footage. The project specifications called for two 15-minute, unbiased videos detailing general clinical needs. In response to this, the two teams visited a total of 20 different departments, observed nearly 30 procedures, and interviewed 31 hospital affiliates. The two teams collected a total of 30 hours of interview footage with medical students, first-year residents, physicians, surgeons, physician assistants, nurses, and technicians. In addition to interviews, the intern teams also filmed procedures, simulations, and general footage of the medical center to include in their videos.
Following the initial observation period, the teams compiled lists of potential needs topics and logically categorized these into ideas for prospective video segments. After an extensive editing process, each intern group produced 4-5 videos, each approximately 14 minutes in length. In the next section, the students' provide their firsthand view of this internship, thus references to “we” are pertaining to the student voice.
The Clinical Rotation Experience: The Student Perspective
In order to gain the most from this experience, we took the initiative to explore many departments, including those outside of our provided contacts. The first two weeks were spent in the observation phase, where we investigated different departments and absorbed as much knowledge of the hospital environment as possible. Within three weeks we began to select areas of focus for our video concept and contacted clinicians and other personnel for formal interviews and permission to film demonstrations of their work. Each week we met with the supervising faculty member from the Biomedical Engineering Department to receive feedback as to how we, as engineers, could gain more practical knowledge of clinical needs finding and to discuss strategies for developing our video concepts.
In the observation phase, we took an investigative approach towards clinical needs finding. This process involved interviews with hospital personnel using open-ended questions, and direct observation of procedures and techniques commonly utilized in the hospital. One successful method by which we explored clinical needs was by prompting physicians and hospital employees to identify any situations within their work environment where they are forced to improvise due to lack of adequate equipment or protocols. We also asked the clinicians for what they viewed as difficulties, bottlenecks, or complications typically encountered in the hospital, and noted these as areas for potential innovation. For example, a common procedure performed in the emergency department uses a needle to drain fluid from the neck of a patient. In this situation, emergency doctors have become accustomed to employing a work-around to prevent inserting the needle too deeply into the neck of patients and inadvertently puncturing a major artery or vein. Because the needles themselves do not possess any safety catch or limiting guide, the doctors use surgical scissors to cut a portion of the tip of the plastic needle cover (the sleeve around unused needles) and replace the partial case over the needle, effectively creating a failsafe guard around the needle. As another example, health professionals often have to improvise while working with obese patients. Increasing numbers of patients within the hospital suffer from obesity, a nationwide epidemic(7). Compared to patients within a healthy weight range, clinicians working with obese patients face a variety of additional challenges, from needing to penetrate thicker skin during injections or accessing vessels under the overlapping skin-folds, to added difficulties in moving and positioning the patient. Unfortunately, many of the tools available have not been designed for use on obese patients. As one physician noted, ideally, equipment should be made for each specific purpose rather than forcing doctors to improvise. By asking health professionals open-ended questions and observing them as they worked, we were able to identify these potential areas of need.
One primary goal throughout the internship was to maintain objectivity both in the interactions with hospital personnel and in the selection of clinical needs to highlight in the videos. Our team strived to provide a well-informed yet unbiased perspective that incorporated direct input from physicians and staff. Input from physicians came in many forms. Some physicians offered direct suggestions and requests for equipment changes, while others discussed existing equipment that was impractical or too expensive for common use. There were also instances in which the team recognized inefficiencies that had been overlooked. However, while editing the final video we put forth an extensive effort to avoid adding our own interpretations.
The videos were designed to provide the critical observations and interactions of the rotation experience without leading the viewers to specific needs, thus allowing the viewers to formulate their own needs statements after viewing.
Filming and Video Production
The equipment used included a Canon Rebel T2i, a Sony Handycam HDR-CX560, an Audio-Technica ATR6550 shotgun microphone, and two collapsible Sony tripods. We selected Final Cut Pro X for video editing software because of its broader editing capabilities, compared to other editing software, which would allow for more creativity in the video editing process. Several group members had previous editing experience with earlier Final Cut Pro versions and felt that it was suitable to their needs. Final Cut was designed to be used with Apple operating systems; the specific computers utilized were a Mac Pro with 6 GB ram, 1 TB hard drive, 2.8 GHz Intel Xeon processor and a 27in IMAC with a 3.1 GHz Quad-core Intel core i5 processor with 4GB ram and 1TB hard drive. These were the least expensive Apple computers available with a minimum of 4 GB ram and 1TB memory.
For the filming portion, we found it useful to carry our film equipment early on in the observation phase as the hospital is a dynamic environment with many procedures occurring spontaneously. While filming, there were a number of concerns that had to be addressed. Foremost among these was the concern for respecting HIPAA regulations (Health Insurance Portability and Accountability Act). Due to this restriction, patient filming was limited to patients who had signed a HIPAA waiver and we used only footage in which faces or other identifying features were not disclosed. We became proficient in communicating the goals of our project to patients and their loved ones in order to attain patient consents for live footage when appropriate. Another limitation was stringent hospital regulations on where filming was permitted. To overcome these boundaries that had the potential to severely limit the amount and quality of procedural footage, we turned to alternative solutions such as filming simulators at the Center for Virtual Care (CVC). We were allowed full access to the CVC, giving us the opportunity to request demonstrations of specific procedures such as intubations and surgical simulations, which would be difficult to capture during live procedures. In addition, when filming mannequins we were able to explicitly show detailed aspects of the procedures.
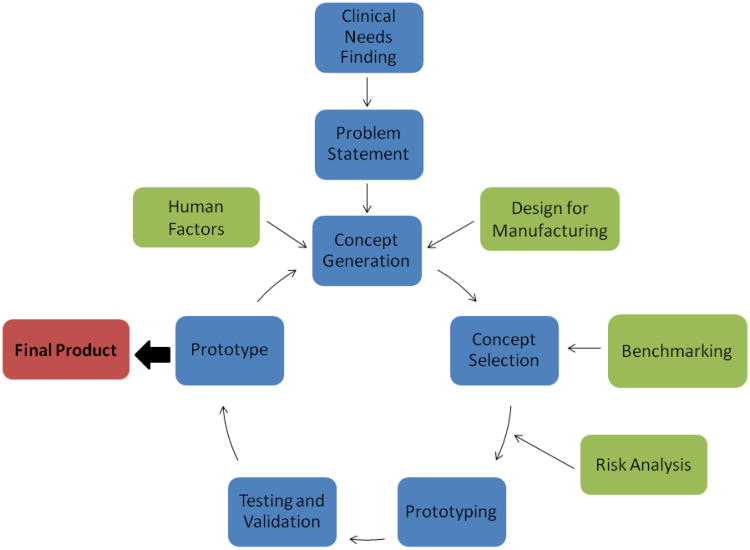
We acquired a number of types of footage to vary the complexity and interest of the material. The general types of shots included procedures on mannequins (Fig 2A), procedures on live subjects (Fig 2B), interviews (Fig 2C) and shots of scenery from the medical center (Fig 2D). In order to make the videos more professional and engaging, we used two cameras to capture the video footage from multiple angles. Figure 3 is a blocking diagram that shows the general set up that was used for interviewing subjects. The main camera was set directly in front of the interviewee and provided a wide-angle shot of his or her body from the waist up. The second camera was used to capture a shot of the interviewee's upper torso and head. There were two main advantages to using two different cameras. The first was that it allowed us to mask when portions of interviews were removed without creating a distracting gap that would result in the single camera method. By switching to the second camera, the transition was seamless. In addition, a general technique used in video editing is to remain on a single static shot for 10 seconds at most; otherwise, the viewer can lose interest. Therefore, having two cameras allowed us to switch shots back and forth between them to create a more interesting scene.
Figure 2. Screenshots illustrating types of footage acquired.
A. A mannequin demonstration
B. A procedural demonstration on a patient, with identifying features excluded from the shot.
C. An interview
D. Typical scenery/atmosphere
Figure 3.
Blocking.
Diagram illustrating typical camera placement relative to interviewee and interviewer
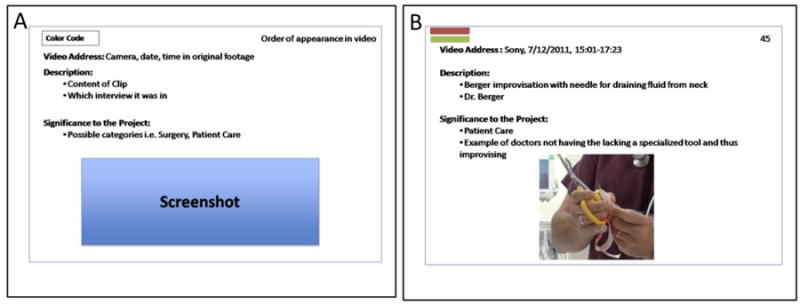
Once sufficient footage was acquired, we began the video editing process. Though typically storyboarding is completed before filming, we waited until the footage was gathered because it was very uncertain what type of footage could be acquired given the dynamic nature of medicine on a day-to-day basis. In general, a storyboard is a visual representation of how the desired shot in the final video will appear, displaying the people in the shot, the background, the overall content of the frame and the camera angle. Storyboards look very similar to graphic novels in layout, with a series of panels showing the action for each scene. However, due to the large number of ideas for clinical needs and the extensive amount of footage, typical storyboarding was unrealistic. As such, the first team developed an innovative method for streamlined storyboarding. In this method, the footage was broken down into a series of important clips. For each clip, a detailed summary card was created describing the clip, video address, and its significance to the project. A general summary card and a completed summary card are illustrated in Figure 4. The 2011 team compiled over 400 of these summary cards for all four videos. All of the clips were then analyzed critically to form categories. Final categories included surgery, imaging, patient care, and procedures. Only after this sorting process was completed were any cuts made to the raw footage. This prevented material overlap and tied clips together cohesively. Thus, raw footage dissection only required one person, yet included the input of all other team members. Through this organization, editing was consolidated.
Figure 4. Storyboarding Cards.

A. General format for summary card used in storyboarding.
B. An example of a completed summary card used for patient care video. The color-coding at the top left was for easy reference and categorization of the subject matter.
After familiarization with Final Cut Pro X and organization of the summary cards into a coherent composition, we began formal editing. Many built-in functions in Final Cut Pro X were utilized in order to bring the raw footage up to professional quality. For example, the footage collected with each camera differed in their color compositions. There was also a great deal of background noise picked up by the shotgun microphone in many of the interviews. Thus, production tools available in the video editing software were used to balance the color composition between both cameras, remove background noise, and align audio and video. Assembling fluid transitions between interviews was crucial to the quality of the final video. We accomplished this by using title blocks for each interview subject and topic segment and by incorporating transition elements to maintain the flow of the filmed material. Supplementary materials, such as videos or graphics of equipment and processes, were integrated to enhance audience comprehension. In Figure 5 we illustrate some of the aesthetic enhancements that were added. The picture-in-picture feature was added to complement descriptions of procedures that were described during interviews (Fig 5a), graphics-enhanced menus were added to facilitate navigation between the topics (Fig 5b), alignment of audio and video is shown in a screenshot from the FinalCut Pro program (Fig 5c), and titles were used strategically to organize video content (Fig 5d).
Figure 5. Video editing techniques.
A. A screenshot example of the picture-in-a-picture feature used in the surgery segment
B. Screenshot example of the imaging menu, illustrating graphics and submenus for content navigation.
C. A screenshot example of the FinalCut Pro X video editing software showing the audio and video alignment bars
D. A screenshot from the patient care segment illustrating use of floating text over the image.
One of the biggest challenges we faced when using Final Cut Pro X was frequent data loss. Like other video editing programs, Final Cut Pro X was sometimes unable to process the nearly 1 TB of high-quality video, resulting in repeated program failure. Among other shortcomings, this failure would cause Final Cut's autosave feature to malfunction, with no manual save substitute available to the user (a known and unresolved bug). To circumvent this issue, edited footage was duplicated and backed up every day for storage on external hard drives. Also, after every 30 minutes of editing the footage was rendered and the program was exited to ensure no editing was lost.
Results: The Student Perspective
The Clinical Needs Finding Experience was beneficial to us on a personal and professional level. It provided many opportunities to apply classroom skills in a real-world context and to develop new skills. We were given nearly unrestricted access to the UCDMC, with the exception of sterile or hazardous environments, but with a defined project focus. We found it most effective to rotate in pairs, which allowed us to effectively cover all of the departments and prevent overcrowding of the small rooms and hallways within the medical center. The project required teamwork and constant communication between team members, a vital skill for future careers as engineers or professionals in any industry. Similarly, constant interaction with medical professionals, students, and technicians taught us invaluable lessons in professionalism, networking, effective communication skills, and confidence. We learned to be conscious not to interfere with the work of the clinicians or disrespect the patients, as observers can leave a fairly significant footprint. It is paramount to be in tune with social cues and know when it is appropriate to ask questions. Furthermore, the project revealed insight into being a care provider in a hospital. This greater understanding highlighted the importance of the role that a biomedical engineer plays within doctor-patient dynamics. When designing a device to meet a clinical need it is extremely important to consider not only the patient who needs the therapy or diagnostic, but also the doctor who administers. In order to convey these findings to our peers, we had to effectively communicate the hospital setting to students who typically have limited exposure to this atmosphere. The video project demanded presentation skills and awareness of our audience, which are valuable assets in any professional setting. For these reasons, we believe we are better prepared for the senior design experience and ready to apply these newly acquired skills to our own projects and our future careers.
Throughout this internship, we learned how to effectively implement an engineering mindset in a clinical setting while keeping an open mind. We found that the perceived need of the clinician is not always the same as the actual need. As an engineer in a clinical setting, it is important to filter out any bias from the clinician, which may lead to a proposed solution that is not actually the best solution. In alignment with this mindset, the virtual rotation documentary was edited to provide information without an inherent bias towards a particular solution to allow the viewer to deduce needs based on their own viewing experience. Many of our team members did not have previous video editing experience, but we did not find this to be an obstacle. However, learning to edit in an educational documentary style added to the professionalism of our video. We were provided with rudimentary training and were able to deduce the rest from experimenting with the software. This notes the end of the Student Perspective section.
Virtual Clinical Needs Finding: The Videos
As mentioned earlier, each team produced 4-5 video segments of approximately 15 minutes in duration, each covering a different department of the hospital. Summaries of the content and organization of the videos from year one and year two of the internship are provided in Tables 1 and 2, respectively. The 2011 video covers 4 clinical areas (Imaging, Patient Care, Surgery, Procedures) each covering 5-6 subtopics. The 2012 video covers 5 clinical areas (Radiology, Physical Medicine and Rehabilitation, Pathology, Intensive Care, and Center for Virtual Care) each covering 2-7 subtopics. Copies of the videos can be made available to readers upon request to the corresponding author.
Table 1.
Description of video breakdown from 2011 DVD detailing the four segments: Imaging, Patient Care, Surgery, and Procedures.
| 2011 Video Distribution | |||
|---|---|---|---|
|
| |||
| Segment | Length | Components | Summary |
| Imaging | 14:18 |
|
A variety of scopes were discussed, including laryngoscopes and bronchoscopes. Inherent flaws in the equipment such as image quality and image processing and cases of the equipment failing to meet needs of the environment, including portability, robustness, and ease of use were displayed. The portable equipment frequently was difficult to transport and fit in confined spaces in patient rooms. Cost of the equipment married with equipment lacking in durability was also discussed. Technician exposure to radiation was a significant risk with the radioactive glucose used in positron emission tomography (PET). |
|
| |||
| Patient Care | 14:57 |
|
A recurring concern was equipment and procedures poorly suited to incorporate the growing number of obese patients. Difficulties arose with transporting patients, regularly rotating patients to prevent skin breakdown, and preventing the muscle loss associated with immobility. Size complicated normal concerns, as typically functional equipment frequently adapted poorly to patients who were either very large or very small, indicating not enough specialization for infants and obese patients. Other primary concerns included creating a consistently sterile environment and difficulties involved with intravenous exertions. |
|
| |||
| Surgery | 13:38 |
|
The surgery segment includes interviews with team members from Center for Virtual Care (CVC) displaying laparoscopic equipment and discussing the shortcomings of current tools used for teaching and performing surgery. Furthermore, examples of how the physicians interact with the CVC equipment demonstrate an area for further development in medical training tools. This section explores some of the drawbacks of using the mannequins to model human patients. Additionally, the physicians talk about the direction that medical training is heading. Online footage is included to highlight topics discussed in this section with regards to surgical training. |
|
| |||
| Procedures | 14:26 |
|
The major focuses of the procedural section were patient safety and procedural efficiency. Intubation and chest tubes provided both immediate and long-term concerns such as tube movement and infection. Bronchoscope maneuverability and tube access and placements were also difficulties. Safe and efficient IV placement posed additional problems. Access was complicated in special cases including in obese patients. |
Table 2.
Description of video breakdown from 2012 DVD detailing the five segments: Radiology, PM&R, Pathology, ICU, CVC.
| 2012 Video Distribution | |||
|---|---|---|---|
|
| |||
| Segments | Length | Components | Summary |
| Radiology | 13:04 |
|
The major modalities in the Radiology Department are X-Ray, Computed Tomography, Ultrasound, and Magnetic Resonance Imaging. Sometimes transferring a patient into the MRI room can be difficult with regards to patient size and equipment attached to the patient. Claustrophobia is also a concern. Protocols in place to get around these difficulties often lead to subpar images. Constraints with dealing with children also lead to poor radiographs. The use of fluoroscopy to correct intussusception, the telescoping of intestine around itself, can cause detrimental effects to the patient, while ultrasound can be safer and more efficient. |
|
| |||
| PM & R | 13:52 |
|
Physical Medicine and Rehabilitation focuses on improving mobility for many patients in the hospital, especially those with traumatic brain injuries, strokes, or spinal cord injuries. There are a variety of devices to assist walking, standing up, or sitting down, but these devices have inherent constraints and storage space is limited. Some patients are so immobile they require bedside physical therapy. This poses complications because of the many lines Intensive Care patients are hooked up to. Physical and Occupational Therapists in the Burn Unit have an additional concern because burn wounds around the neck and arms contract as they heal if not properly addressed. |
|
| |||
| Pathology | 20:16 |
|
A variety of laboratory testing occurs within the Pathology Department, including the testing of live and expired specimens. Checking for clots is one bottleneck because the test is performed manually. The Frozen Section deals with samples taken from a patient in the Operating Room, placing a large time constraint on making a diagnosis because surgeons are waiting to hear back. One of the rate-limiting steps is the staining of slides for better viewing. In gross anatomy, people are the rate-limiting step of sample processing, from the time of cutting up the tissue sample to placing it on a slide. |
|
| |||
| ICU | 15:14 |
|
The ICU is a place for people that need continuous monitoring and/or suffer from organ failure. The placement of the bed and monitoring systems is not optimal for doctors or patients' health. There are limitations in using nasogastric and orogastric tubes. When a patient is intubated in the hospital, an endotracheal tube is inflated in their airway, which can lead to complications if it is not properly inflated. Most patients have catheters in their arteries, but patient movement can cause them to lose functionality. The Emergency Medical Record system in place at the UCDMC is not an intuitive program and prevents communication between the hospital staff. |
|
| |||
| CVC | 15:30 |
|
The goal of the Center for Virtual Care is to provide clinicians with a virtual environment for learning to enhance patient care. Mannequins simulate a variety of biologically correct functions, such as blinking, pulses, breath sounds, and heart sounds. Mannequins can hook up to real patient equipment, allowing clinicians to practice both simple and more complicated procedures such as a Percutaneous Tracheostomy. As complex as these mannequins are, they are nowhere near replacing people. Many advances are needed to make the mannequins more realistic. |
Outcomes and Best Practices: Instructor Perspective
The completed videos were premiered for an audience of clinicians, students, and biomedical engineering faculty. The resulting videos were professional in quality and valued as a teaching tool by both senior design instructors and clinicians. The production quality of the videos was excellent and the team made outstanding use of intercut procedural footage and interviews to provide an engaging documentary. It was difficult to completely remove suggestions of problems from the videos; thus, clinicians discussing their perceptions of problems were also included. The students gained skills in many areas including interdisciplinary communications, teamwork, oral presentation, and time management. The schedule and pace of the seven week full-time experience was rated highly by both the students and participating clinical faculty. The division of the segments focusing on individual departments was viewed as a strength of the films. The videos can be dry when viewed in a continuous hour-long reel, and were much more digestible in 15 minute segments.
Besides benefiting the students who will be viewing these videos to obtain project ideas, the video internship directly benefited the participating interns. Aside from project management and communication skills highlighted by the students, the internship was also valuable training for their own design projects. For example, based upon exposure to clinical problems they observed through the internship, two students were inspired to pursue an independent design project. During the internship they identified a need for a gastric bypass surgical simulator to aid in medical education, to teach surgeons of all levels how to perform complicated laparoscopic procedures. They organized a team and contacted the general surgeon that they had interviewed during video filming to act as a mentor. Medical school students practice procedures such as intubation on mannequins and the student team aimed to create a similar experience for surgical residents. Simulation training has been observed to greatly improve surgical skills and proficiency exam pass rates (8-12). Virtual systems for laparoscopic training have been explored, but virtual reality can only provide limited sense of the real experience (13-17). Although simulated tissue does exist which allows surgeons to practice suturing and tissue handling, there are few existing models that replicate internal organs in a manner that provides realistic training; surgeons have expressed that learning to recognize the “feel” of tissue is important to learning how to successfully complete surgeries. The students identified the need for more realistic surgical simulation, and created a synthetic, physical model for intestinal tissue that replicated the feel and texture of live tissue. To fund the project, the student team applied for and received seed funding through the UC Davis Clinical and Translational Science Center (NIH funded). The team was invited to present their project in the form of a poster and oral presentation at the Rice 360 Beyond Traditional Borders Engineering Design Competition at Rice University in Houston, Texas (March 2012, Houston, Texas).
We are making efforts to broadly disseminate the internship experience to benefit a larger student base. The Clinical Needs Finding experience was presented at the BMES (Biomedical Engineering Society) national conference in 2012 to share this innovative approach to incorporating needs finding into the engineering design process. Instructors from other institutions expressed interest in the findings. Some asked for and were provided with copies of the films to show in their own classes. We will be following up with these programs to evaluate the effectiveness of the videos in delivering a clinical rotation experience and to determine whether students are able to formulate problems to address in their design projects.
To use the videos for a needs finding experience for students we recommend that at minimum the instructor discusses the process of needs finding, what it means and how to do it, in the same way that they would prepare students to enter the clinic for this type of activity. Without proper context, students may not mine for underlying needs and be unduly influenced by clinicians' suggestions for solutions. In our class, for clinical rotations as well as video viewing, we first define needs finding and discuss the importance of observation and needs identification in the development of the problem statement. Students are instructed on topics including:
How to be an active observer. We discuss a number of concepts including conducting interviews and listening without bias.
Keeping detailed documentation. Students are instructed to take notes throughout, jotting down ideas to follow up on. It is emphasized that keeping track of who said what, and logging contact information is critical in the process of organizing the large amount of information they will receive.
Keeping an eye out for workarounds. Students are alerted to watch for activities in which clinicians are not using a device or process as it was meant to be, where there are clearly deficiencies that cause the user to go “off protocol” to make things work for their needs.
Identifying the actual “need” versus the clinician's idea for a solution. This is perhaps one of the most important prompts for in person rotations and a problem we were able to avoid in the virtual experience by keeping bias out of the videos. Clinicians are educated individuals who can be quite inventive themselves, and getting to the root need versus potential solutions they have identified is a challenge we point out to our students. Before we emphasized this difference, students would often return from client interviews with descriptions of desired devices, but not a clear understanding for the underlying reason the clinician requested a device to be built a particular way. For example, in an interview a client may express that a device's handle is too small. If the students simply record that the need is for a bigger handle without digging deeper they miss the root of the problem, which can range from poor comfort, difficulty handling, slipperiness etc. which could be addressed by other solutions besides a bigger handle. Students are also counseled to research background and consult the appropriate literature as they begin to identify needs they wish to address in their design projects, so they can return to the clinic each day better informed. To paraphrase a famous quote, a prepared mind is better able to observe needs.
How needs are translated to project ideas. Observations in the clinic are translated to problem statements and these are the jumping off points for senior design projects. With these problem statements, the student teams begin the process of concept generation and concept selection leading to their design solution.
As an example of how the videos may be used for a class, we assigned the video segment on Surgery to a senior design class of students for viewing. The students were given the following prompt as a prelude to viewing the films: “Watch the video with an open mind, and keep an eye out for problems and needs that you observe. Some problems might be clearly stated by the clinicians who are interviewed, but many others you will get a feeling for as you watch procedures in progress or listen to what the clinicians are saying about challenges they face in their practices. The idea behind the videos was to present an unbiased observation experience, that does not indicate clearly what problems or needs there are. Therefore, project ideas may not be identified by people in the video, it is up to you as a viewer to find them. Make a list of as many “needs” that could be developed into design projects as you can identify.” We offered a prize for the largest number of legitimate needs listed.
The actual video viewing experience varied with the watcher, much as a clinical rotation would. The survey of 59 students produced 102 unique needs identified, averaging 11.2 ± 5.8 problems identified per student with a high of 32, and a low of 3. Of the 59 students, forty-three provided lists of 7-15 needs. The needs identified spanned a wide range, demonstrating different degrees of subtlety in their interpretation of observations, however most students identified the following classes of needs/potential projects:
Realistic simulated tissues that bleed, change color, etc
More maneuverable laparoscopic devices
Reusable laparoscopic device
Suturing device modifications with wider range of functionality (to accommodate smaller needles, use curved needles etc)
Different size robotic systems for different tasks
We provide a sample list of the most frequently identified needs (raw) identified by students in Table 3. Many of these have distilled the information from the video to a statement of a need that a design project could be built around. The most frequently identified needs tending to be topics that were spoken about more extensively by clinicians during interviews. Although an effort was made to avoid bias, clinician's sometimes highlighted particular needs in their interviews and these showed up more often in the students' lists. However, the diversity and number of needs identified support, anecdotally, that the observation experience clearly influenced the ability to find needs. This is much like the in person experience.
Table 3. Sample of Needs Identified by Students in the “Surgery” video segment.
| 2012 Surgery Video: Identified Needs | |||
|---|---|---|---|
| 1 | Simulate the bleeding response of tissue to prepare surgeons for the operating room | ||
| 2 | Tools are used only once and thrown away—need reusable devices | ||
| 3 | Current robotic systems are bulky and need more refinement, smaller in size, more portable | ||
| 4 | More flexible laparoscopic tools with greater articulation and degrees of freedom | ||
| 5 | Need realistic complex feedback and inputs, e.g. tactile feedback | ||
| 6 | Ability to simulate changes that real skin shows, such as pallor, rashes, etc | ||
| 7 | Blend between mannequin and virtual reality systems to give both tactile feedback and visual realism | ||
| 8 | Improve suturing device to accommodate different size needles and be more comparable to 5mm suturing device | ||
| 9 | Mannequins that are more dynamic and responsive | ||
| 10 | Improved texture of simulated tissues in elasticity and response to handling (e.g. bruising) | ||
| 11 | Improve training process to include many simulations before working on real patient | ||
| 12 | Decrease wound infection rates | ||
| 13 | Suturing device that can accommodate curved needles | ||
| 14 | Create simple devices, but with more complex functions (more intuitive to use, one hand use) | ||
| 15 | Suturing device that produces results more like hand suturing (e.g. variable stitch size, maneuverability) | ||
| 16 | Reduce surgical failure rate | ||
| 17 | Cameras with greater field of view and illumination | ||
| 18 | One hand device with camera built in, instead of separate device requiring two handed operation | ||
| 19 | More tactile feedback from laparoscopic tools | ||
| 20 | Standardized annual test for surgeons | ||
| 21 | Dynamic models that change in physical properties during surgical simulation (e.g. bowels stretch) | ||
| 22 | Simulation tools that more accurately reflect the procedure rather than simply training the mechanics (e.g. moving beans from place to place) | ||
An important addendum to firsthand clinical rotation as well as the video experience would be to follow up with clinicians for more detailed interviews and to gather more detail to set target specifications. In the absence of a nearby clinic, the video viewer could conduct phone interviews with remote subjects. We generally recommend to our students to interview many potential end users, to formulate the most useful design. Focusing on a single user can create a niche, ‘one-off” solution that is custom made for a particular use as opposed to a marketable product with wider appeal.
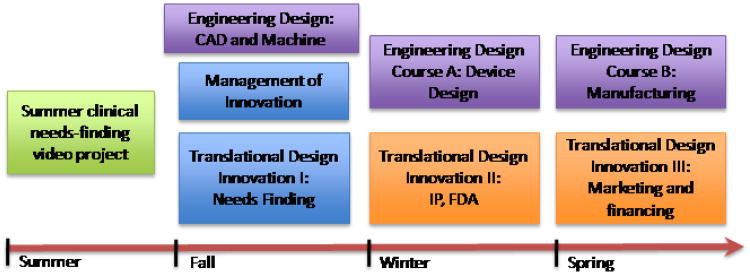
Training of biomedical engineers is an ever-increasing concern as the nation's healthcare system is growing and changing (18). The Clinical Needs Finding project sought to fill the critical gap between clinical practice and engineering solutions in the Biomedical Engineering senior design experience. In the past, students provided with predetermined problems often did not understand the “bigger picture” for their designs, leaving the students with an incomplete experience of real world needs. This can be remedied by actively exploring areas of need and interacting with medical professionals. We thus sought to integrate needs finding into the senior design experience. As shown in Figure 6, needs finding experiences are part of a larger effort to integrate real world experiences into the senior design experience at UC Davis. The existing set of design courses (purple) are being supplemented with exposure to not only clinical needs finding (orange/blue), but also other concepts essential to innovation and design (orange/blue).
Figure 6.
The Senior Design Experience at UC Davis.
The Clinical Needs Finding Internship was added to the summer before senior year to complement the yearlong senior design sequence at UC Davis. Aspects of commercialization are also being added to the program to provide a more complete experience of the engineering design process. Existing, new, and future courses are represented as shown:
 Needs Finding Internship,
Needs Finding Internship,
 Optional courses,
Optional courses,
 Senior Design series courses,
Senior Design series courses,
 Courses in Development.
Courses in Development.
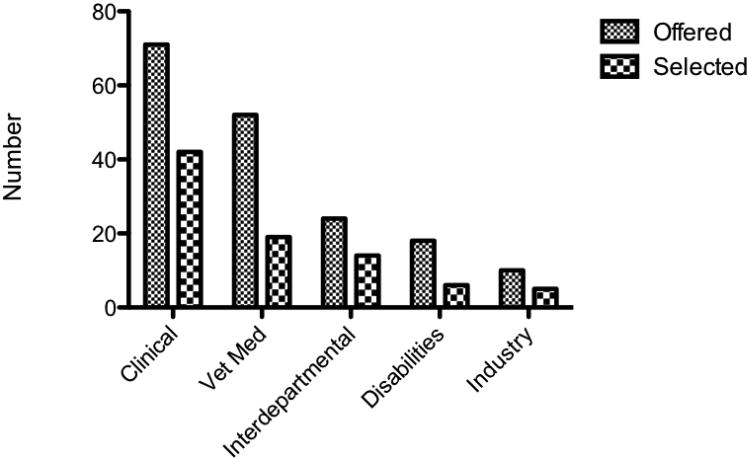
As the number of seniors grows, class sizes will soon be prohibitively large for in-person clinical experiences for every student (19). As shown in Figure 7, clinical projects are very popular with students and projects from the medical and veterinary schools have constituted the majority of past senior design projects for our 272 graduating seniors to date. Note that the numbers reflected in Figure 7 refer to numbers reflect numbers of projects, with students typically working in teams of four. We are expanding clinical needs finding into the School of Veterinary Medicine, the second largest supplier of projects for senior design. Two clinicians from the School of Veterinary Medicine (from the Departments of Surgery and Radiological Sciences and Clinical Neurology/Neurosurgery) have been recruited as lead contacts for rotations through the veterinary school departments. An added benefit to veterinary projects is that, compared to devices for human use, there are significantly fewer regulatory barriers and veterinary projects can progress from conception to implementation in the field within the time frame of the design experience. The requirement for FDA approval makes most human patient testing out of reach for the short time scale of senior design. But veterinary products do not need to undergo rigorous FDA testing in order to be used, nor are they subject to regulations governing laboratory animal use. Therefore, working on projects designed for animal use provides the additional benefit of allowing students to experience the entire project, from the initial need identification to the final implementation of the product.
Figure 7.
Sources for projects from 2006-2012.
The distribution of areas from which senior projects were offered and selected each year since program inception. Clinical applications were the most popular, with twice as many projects selected as the next most popular area. Needs finding will be a valuable experience for these types of projects.
Conclusion
The Clinical Needs Finding Video Internship provided interns with many skills required to recognize needs that lead to engineering innovation. Further, the resulting videos offer an alternate method to engage in a needs finding experience when clinical visits are not practical. The videos have already begun to be implemented both internally within the institution, and externally. Further offerings of the Clinical Needs Finding Video Internship will incorporate additional clinical departments at both the medical and veterinary hospitals to provide a library of rotation experiences for students.
Acknowledgments
We thank the National Institutes of Health for funding (1R25 EB012963). We thank Dr. Nicholas Kenyon, Dr. Aaron Bair, and Dr. Nam Tran for leading the clinical internships. In addition, we thank the following clinical personnel for their participation in the videos: Dr. Jonathan Pierce, Dr. Yasmeen Shaw, Dr. Nisha Gidwani, Dr. Nicholas Stollenwerk, Larry Baker, P.A, Ted Cohen, Cattuong Cooter, Ramsey Badawi, Chris Jarvinen, Marcus Christian, George Gonzales, Leana Aston, Leonid Krainov, Jeanne Kim, David Price, Kevin Murphy, Naomi Ross, Kyle Davis, Rocky Cervantez. We thank the following internship team members for participation in creating the videos: Eric Foo, Christopher Sanchez, Joanna Quach.
References
- 1.Dutson AJ, Todd RH, Magleby SP, Sorensen CD. A review of literature on teaching engineering design through project-oriented capstone courses. Journal of Engineering Education. 1997:17–28. [Google Scholar]
- 2.Todd RH, Magleby SP, Sorensen CD, Swan BR, Anthony DK. A Survey of capstone engineering courses in north america. Journal of Engineering Education. 1995 Apr;:165–74. [Google Scholar]
- 3.Ulrich K, Eppinger S. Product design and development. fifth. NY: McGraw Hill; 2011. [Google Scholar]
- 4.Zenios S, Makower J, Yock P. Biodesign. NY: Cambridge University Press; 2010. [Google Scholar]
- 5.Anthony S. The little black book of innovation: How it works, how to do it. Boston, MA: Harvard Business Review Press; p. 2011. [Google Scholar]
- 6.Kelley T. Field observations with fresh eyes 2008 [updated 2008; cited] Available from: http://ecorner.stanford.edu/authorMaterialInfo.html?mid=2100, http://www.youtube.com/watch?v=XrpAveg7ZIg.
- 7.Zinn A. Unconventional wisdom about the obesity epidemic. Am J Med Sci. 2010;340(6):481–91. doi: 10.1097/MAJ.0b013e3181ccb980. [DOI] [PubMed] [Google Scholar]
- 8.Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM. Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surgical Endoscopy and Other Interventional Techniques. 2008;22(8):1887–93. doi: 10.1007/s00464-008-9745-y. [DOI] [PubMed] [Google Scholar]
- 9.Bittner JG, Coverdill JE, Imam T, Deladisma AM, Edwards MA, Mellinger JD. Do increased training requirements in gastrointestinal endoscopy and advanced laparoscopy necessitate a paradigm shift? A survey of program directors in surgery. Journal of Surgical Education. 2008;65(6):418–30. doi: 10.1016/j.jsurg.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Gillen S, Grone J, Knodgen F, Wolf P, Meyer M, Friess H, et al. Educational and training aspects of new surgical techniques: experience with the endoscopic-laparoscopic interdisciplinary training entity (ELITE) model in training for a natural orifice translumenal endoscopic surgery (NOTES) approach to appendectomy. Surgical Endoscopy and Other Interventional Techniques. 2012;26(8):2376–82. doi: 10.1007/s00464-012-2165-z. [DOI] [PubMed] [Google Scholar]
- 11.Al-Kadi AS, Donnon T, Paolucci EO, Mitchell P, Debru E, Church N. The effect of simulation in improving students' performance in laparoscopic surgery: a meta-analysis. Surgical Endoscopy and Other Interventional Techniques. 2012;26(11):3215–24. doi: 10.1007/s00464-012-2327-z. [DOI] [PubMed] [Google Scholar]
- 12.Haycock AV, Youd P, Bassett P, Saunders BP, Tekkis P, Thomas-Gibson S. Simulator training improves practical skills in therapeutic GI endoscopy: results from a randomized, blinded, controlled study. Gastrointestinal Endoscopy. 2009;70(5):835–45. doi: 10.1016/j.gie.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal R, Gantert WA, Hamel C, Hahnloser D, Metzger J, Kocher T, et al. Assessment of construct validity of a virtual reality laparoscopy simulator. Journal of Laparo endoscopic & Advanced Surgical Techniques. 2007;17(4):407–13. doi: 10.1089/lap.2006.0221. [DOI] [PubMed] [Google Scholar]
- 14.Carter FJ, Schijven MP, Aggarwal R, Grantcharov T, Francis NK, Hanna GB, et al. Consensus guidelines for validation of virtual reality surgical simulators. Surgical Endoscopy and Other Interventional Techniques. 2005;19(12):1523–32. doi: 10.1007/s00464-005-0384-2. [DOI] [PubMed] [Google Scholar]
- 15.Kruglikova I, Grantcharov TP, Drewes AM, Funch-Jensen P. The impact of constructive feedback on training in gastrointestinal endoscopy using high-fidelity virtual-reality simulation: a randomised controlled trial. Gut. 2010;59(2):181–5. doi: 10.1136/gut.2009.191825. [DOI] [PubMed] [Google Scholar]
- 16.Walsh CM, Sherlock ME, Ling SC, Carnahan H. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database of Systematic Reviews. 2012;(6) doi: 10.1002/14651858.CD008237.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Satava RM, Sherk HH. Virtual reality surgical simulator - The first steps. Clinical Orthopaedics and Related Research. 2006;(442):2–4. [PubMed] [Google Scholar]
- 18.Grimes SL. The future of clinical engineering: The challenge of change. IEE Engineering in Medicine and Biology Magazine. 2003 Mar-Apr;:91–9. doi: 10.1109/memb.2003.1195702. [DOI] [PubMed] [Google Scholar]
- 19.Lukasik SJ. System, systems of systems, and the eduation of engineers. Artificial intellience for engineering design Analysis and manufacturing. 1998;(12):55–60. [Google Scholar]