Abstract
The purpose of this study was to develop and validate a brief, clinically relevant, multidimensional interview to assess pain burden among children and adolescents with sickle cell disease (SCD). The Sickle Cell Disease Pain Burden Interview-Youth (SCPBI-Y) was developed using a panel of experts, patients and caregivers. Validation was undertaken with youth with SCD, ages 7 to 21 years (N=129), recruited from four urban children’s hospitals. Youth were recruited from inpatient (N=62) and outpatient (N=67) settings. The SCPBI-Y demonstrated strong internal consistency reliability, cross-informant concordance (child-caregiver), and test-retest reliability (outpatient setting). Moderate construct validity was found with validated measures of functional ability, pain, and quality of life. The SCPBI-Y demonstrated construct validity using a contrasted group approach between youth in inpatient versus outpatient settings and by severity of SCD symptoms, suggesting that youth in inpatient settings and with higher disease severity exhibited greater pain burden. Discriminant validity was found between SCPBI-Y and mood. Our preliminary findings suggest that the SCPBI-Y is a valid and reliable multidimensional interview that can be utilized in different clinical settings to evaluate pain burden among children and adolescents with SCD.
Keywords: sickle cell disease, SCD, pain, functional assessment, adolescents
Introduction
Sickle cell disease is a genetically transmitted disease that in the U.S, predominately affects African Americans. SCD is characterized by acute, severe, painful vaso-occlusive episodes. Pain is the hallmark of sickle cell disease and the dominant feature of children’s medical lives;1,29 about 60–70% of hospitalizations in patients with sickle cell disease are for uncontrolled pain.2 Pain becomes chronic in some adolescents with SCD, in fact there is evidence to suggest that chronic pain occurs in children and adolescents more often than previously acknowledged.31 Currently, little is understood about the impact of pain on the lives of children with sickle cell disease. Number of hospitalizations or emergency department visits have been used as a proxy for pain impact or phenotype; however, a majority of pain episodes in children with sickle cell disease are treated at home and do not reach medical attention.5–7,14,20,30,32,37
A simple disease-specific measure of the impact of pain on physical, social, and emotional function in youth with sickle cell disease would be a valuable tool to enhance understanding of the burden of pain on the lives of children with sickle cell disease. Core outcome domains recommended by the Pediatric division of the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (Ped-IMMPACT) group for evaluation in pediatric chronic and recurrent pain include assessment of pain impact on physical, social, and emotional function.22 As such, a measure of pain burden would allow for assessment of changes in pain impact over time in response to interventions or natural progression of disease, allow stratification of children into different risk groups based on their pain burden, and allow for evaluation of factors which might determine pain impact. Currently available measures of pain impact have had limited use in youth with sickle cell disease and it is unknown whether the same areas of physical, emotional, and social impact are relevant in this population for understanding pain burden.
While daily diaries measuring pain and pain impact have been employed in a number of studies,6,11 compliance with diaries is difficult and interpretation relies on summarizing extant data, and thus diaries are not used for clinical assessment for most patients. Measures of functional disability or impairment can assess the impact of persistent pain. For example, functional disability tools target issues such as sleep, activity, and communication, as well as mood and well being.9,10,23 Functional assessment and quality of life scales for chronic and recurrent pain in children have been validated and include the Functional Disability Inventory (FDI), 36 the Child Activities Limitation Interview (CALI-21),24 and the Pediatric Quality of Life Inventory (PedsQL).33,34 The FDI, CALI-21, and PedsQL have all be utilized among pediatric SCD populations. Previous research has supported validity of the PedsQL within pediatric SCD;21,28 however, the FDI and CALI-21 have not been well-validated in SCD exclusively. For example, validation has been established for the CALI-21 among chronic pain populations that included SCD along with youth with chronic headaches and juvenile rheumatoid arthritis.26 Although available HRQOL and functional assessment tools are valuable for providing measurement of health impact, they may not include specific areas of pain impact most affected in SCD. For some clinicians they also may be considered too lengthy to utilize in a busy clinical setting.
The purpose of this study was to develop and then assess the psychometric properties of a brief multidimensional interview, the Sickle Cell Disease Pain Burden Interview-Youth (SCPBI-Y) to assess pain burden. We conceptualized pain burden as encompassing pain, and the impact of pain on physical function, social/community participation, and the emotional aspects of daily living. We hypothesized that the SCPBI-Y would demonstrate strong reliability as defined by internal consistency and test-retest reliability, and cross-informant concordance (caregiver-child). Caregiver-child concordance analyses have been used in several evidence-based pediatric pain assessment validation studies.2,4 We also hypothesized that the SCPBI-Y would demonstrate strong validity as defined by face and construct validity (concurrent validity and contrasted groups approach). Convergent validity using validated measures of pain interference, function, quality of life, and mood was expected to be moderate. Specifically, we expected moderate relationships whereby higher scores on the SCPBI-Y (indicating high pain burden) would be associated with more days in pain, poorer quality of life, more activity limitations, and more negative mood. Using a contrasted group approach, we expected that pain burden would be greater in patients who were hospitalized for acute pain, when compared with outpatients at baseline status, and that pain burden would be greater in patients with more severe disease compared to patients with milder disease.
Materials and Methods
Tool Development
The SCPBI-Y was developed through review of pediatric functional assessment and pain impact tools in the literature. These impact tools included the PedsQL, the CALI-21, the FDI and PedsMIDAS.17 Experts, which included physicians, nurses, psychologists, and researchers in the fields of sickle cell disease, pain and functional assessment reviewed an initial draft of the SCPBI-Y. The original draft of this brief interview included six items. Subsequently, several modifications were made and the draft was again reviewed by the expert panel, as well by parents and patients with sickle cell disease, for face validity. The SCPBI-Y initially included 6 items to allow for a measure that could be easily utilized in the clinical setting. The time period for the SCPBI-Y assessment, “over the past month,” was chosen in order to be consistent with other multidimensional measures (e.g., PedsQL, CALI-21).
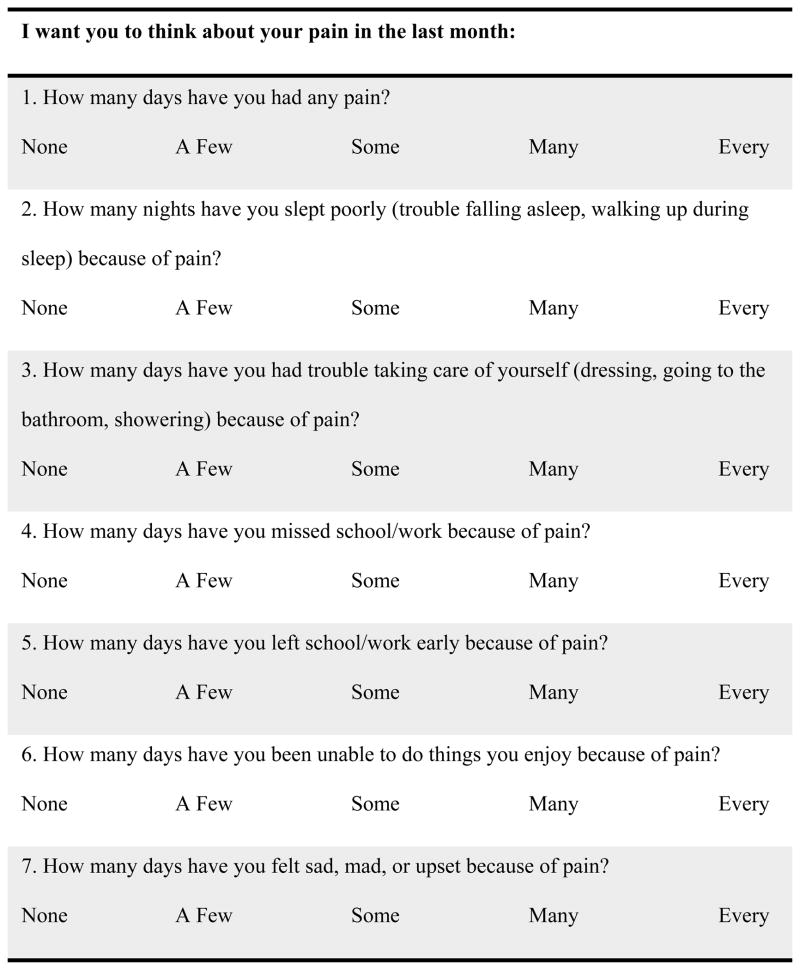
The measure was sent to members of a Sickle Cell Disease parent advisory board for review and comment at which time a seventh item that was added to the interview. The SCPBI-Y was piloted in patients with sickle cell disease presenting to the Hematology/Oncology clinic at the PI’s institution and final changes were made (Figure 1).
Figure 1.
Items of the Sickle Cell Pain Burden Inventory.
Participants and Procedures
Participants were English-speaking subjects with sickle cell disease ages 7–21 who were recruited from four urban children’s medical centers in the eastern United States. These centers include Connecticut Children’s Medical Center (CCMC), Johns Hopkins Hospital, Children’s Hospital of Philadelphia (CHOP), and Children’s Hospital of Atlanta (CHOA). The study was approved by the Institutional Review Boards at these 4 institutions. Written informed consent was obtained from all adults (parents and subjects age 18 and older) in this study and written assent was obtained from children and adolescents (<18 years of age). Participants were recruited from two care settings, one group of patients was recruited in the outpatient sickle cell clinic at routine visits at their baseline health status (outpatient group), and the second group of patients was recruited in the inpatient setting during hospitalization for an acute pain episode (inpatient group).
Outpatient Group
For the outpatient group, we excluded patients who were currently experiencing an acute pain episode at the time of enrollment, however those with chronic pain were included as long as their pain was not above baseline levels. Outpatient participants completed measures and were contacted via phone to complete the SCPBI-Y at week one to determine test-retest reliability. Patients with SCD were approached for the study by a research assistant during their routine medical appointment for the outpatient group. After consent was obtained, participants in the outpatient group were asked to complete six baseline measures and their caregivers (for subjects ≤ 17 years of age), were asked to complete three measures. Parents and children were interviewed in separate rooms. Research personnel contacted outpatient clinic participants one week post-baseline via phone to complete follow-up SCPBI-Y.
Inpatient Group
Inpatients were recruited as part of a larger acute pain study. These participants completed the measures once during their acute hospitalization. For the inpatient group, patients were asked to complete four measures within 72 hours of hospital admission and no follow-up data were collected. See Table 1 for complete demographic information
Table 1.
Demographic Information
| Inpatient Group | Outpatient Group | |
|---|---|---|
| Age M(SD) | 15.70 (3.85) | 15.30 (3.75) |
| Gender % (N) | ||
| Male | 43.3% (29) | 33.9% (31) |
| Female | 56.7% (38) | 66.1% (41) |
| Ethnicity | ||
| Black or African-American | 89.7% (29) | 80.6% (50) |
| Hispanic | 6.1% (4) | 11.5% (7) |
| SCD type | ||
| HbSS | 72.7% (48) | 72.1% (44) |
| HbSC | 21.2% (14) | 18.0% (11) |
| HbSBeta+-thalasemia | 4.5% (3) | 4.9% (3) |
| HbSBeta0 | 1.5% (1) | 4.9% (3) |
| Disease Severity | ||
| Not Severe | -- | 50.8% (30) |
| Severe | -- | 49.2% (29) |
Outpatient N = 62
Inpatient N = 67
Measures
General Information Form
Participants completed a general information form that asked patients to describe disease history, pain experience within the last month (i.e., number of days in pain), treatment interventions and medication use. Both patient groups completed this form.
Sickle Cell Disease Pain Burden Interview-Youth (SCPBI-Y)
The SCPBI-Y is a 7-item measure designed to assess the impact of pain on physical, social/community, and emotional aspects of daily function. The interview administered verbally can be completed by patients and their caregiver(s) in approximately one minute. The seven questions use a Likert scale (none, a few, some, many, and every). The SCPBI yields a numeric score, with a higher number indicating higher pain burden. The following scoring system was utilized: “none” = 0, “a few” = 1, “some” = 2, “many” = 3, “every” = 4. Scores range from 0=no pain burden to 28= severe pain burden. Both patient groups were administered this interview. A parent version of the interview was also administered to parents in the outpatient group with identical items directed to obtain information from the caregiver.
Sickle Cell Disease Assessment Instrument: Disease Severity Classification
The Sickle Cell Disease Assessment Instrument: Disease Severity Classification8 is a measure used to assess disease characteristics among patients with SCD. This classification system collects tabulates number of acute chest syndrome diagnoses, as well as pain episodes requiring an emergency department evaluation or hospitalization over the previous two years. A score of two or greater indicates severe disease. Interrater reliability was evaluated among six nurses completing the measure for 18 patients, ages 18 months to 5 years, resulting in a strong level of reliability (r = 0.94). Test-retest reliability was strong for this measure (r = 1.00).8 This information was collected from the outpatient group only as medical records were not uniformly available for the inpatient group.
Children’s Activity Limitations Interview-21 (parent and child report)
The Children’s Activity Limitations Interview – 21 (CALI-21) is a self-report instrument designed to assess pain-related activity limitations in children and adolescents (ages 8–18) via caregiver and child written report.24 The measure asks participants to report on pain-related limitations in 21 daily activities over the previous 4 weeks, rating the difficulty in completing each activity on a 5-point rating scale, ranging from 0 ‘not difficult’ to 4 ‘extremely difficult’. The score is calculated by summing ratings for all 21 items, (possible range from 0 to 84), with higher scores indicating greater activity limitations or more impairment. Two factors representing limitation in Active and Routine activities can also be computed. The CALI-21 has shown good internal consistency, high cross-informant reliability, and demonstrated construct validity. Both groups were administered the CALI-21.
Positive and Negative Affect Schedule—Child Version (PANAS-C)
The PANAS-C is a 27-item assessment of mood.18 The PANAS-C asks the child to rate the degree to which different words (i.e. sad, active, joyful) describe how they feel on a scale of 1 (very slightly or not at all) to 5 (extremely). This measure has been validated among 4th to 8th grade children and has been shown to a reliable and valid measure within this population. The PANAS-C has been validated among pediatric populations, yielding strong convergent and discriminant validity.17 Both inpatient and outpatient groups were administered this scale that yields a Positive Affect and Negative Affect score.
Pediatric Quality of Life Inventory (PedsQL) Generic 4.0
The PedsQL Generic 4.0 is a measure of health-related quality of life developed for children.33,34 The generic module has physical, emotional, social and school domains. Two versions of the measure was used: the child version (ages 8–12) and teen version (ages 13–17). Scores are calculated on a 0–100 scale, with higher scores representing better health-related quality of life. The PedsQL generic core scales have been previously used in youth with SCD and has established reliability and validity properties.21,27,36 Both groups were administered the PedsQL, according to the age of the patient.
Statistical Analysis
Test-retest reliability using Pearson correlation coefficients was examined through re-administration of the SCPBI-Y by phone 1 week after the initial visit for the outpatient group. Because the temporal stability of functional limitations for vaso-occlusive pain is unknown, data on test-retest reliability of the SCPBI-Y provided useful information about variability in children’s functioning and pain burden. Cross-informant concordance (association between patient and caregiver SCPBI-Y scores) was determined using Pearson correlation coefficients for the outpatient group. Within both patient groups, evidence for construct validity was assessed by evaluating the relationship of SCPBI-Y with measures of frequency of pain, function, and quality of life using Pearson correlation coefficients. Contrasted group validity, a form of construct validity, was determined using independent samples t-tests on SCPBI-Y scores, comparing the outpatient group to the inpatient group; separate t-tests compared SCPBI-Y scores in patients with severe disease vs milder disease. We expect that there would be higher pain burden among those with more severe disease as determined by the Sickle Cell Disease Assessment Instrument. Convergent and discriminant validity was determined by using Pearson correlation coefficients between the SCPBI-Y scores and mood measures.
The total score for the PANAS-Negative had significantly positive kurtosis and a logarithmic transformation was performed to yield a normal distribution. Preliminary analyses also explored potential confounding variables, such as age and gender using Pearson correlation coefficient and Independent Samples t-test analyses, respectively.
Results
Of the 64 patients approached for the outpatient group, 59 (92.2%) enrolled in the study. Three patients refused to participate due to time constraints, disinterest, or discomfort about follow-up data collection via phone. Two additional patients were consented, but did not have time to complete the measures at baseline and therefore, did not enroll in the study. Of the 59 enrolled, two patients were excluded due to inability to adequately complete the measures. As a result, 57 participants were included in the outpatient group recruited at CCMC for this study and an additional 5 participants were recruited from Johns Hopkins Hospital (total outpatient n=62).
Of the 73 patients approached for the inpatient group, six patients were excluded due to experiencing acute chest syndrome (N=3) or were outside the age criteria (N=3). As a result, there were 67 participants recruited in the inpatient group: 17 participants from CCMC, 20 from Johns Hopkins, 15 from CHOA, and 15 from CHOP.
Descriptive statistics for the SCPBI-Y, CALI-21, PANAS, and PedsQL for the outpatient, inpatient, and combined groups are summarized in Table 2. The results of these analyses indicated that there were no significant differences between males and females among each of the measure total scores. In addition, age was unrelated to outcome or validation measures. Thus, these confounding variables were not controlled for in any subsequent analyses.
Table 2.
Descriptive statistics
| Outpatient M (SD) |
Inpatient M (SD) |
Combined M (SD) |
|
|---|---|---|---|
| SCPBI-Y | 6.79 (5.94) | 11.77 (5.09) | 9.38 (6.03) |
| Week 1 | 6.66 (5.39) | -- | -- |
| CALI | 16.84 (15.58) | 25.05 (17.13) | 21.58 (17.20) |
| PANAS | |||
| Positive Affect | 36.35 (10.16) | 25.89 (12.02) | 30.87 (12.31) |
| Negative Affect | 24.71 (9.09) | -- | -- |
| PedsQL (Total) | 69.39 (17.59) | 59.33 (17.41) | 64.07 (18.14) |
Outpatient N = 62
Inpatient N = 67
Combined Group N= 129
Reliability
Internal consistency reliability was determined using a Cronbach’s alpha among the seven items of the SCPBI-Y. The SCPBI-Y demonstrated strong internal consistency reliability among the outpatient group (α=0.909; N=62), inpatient group (α=0.821; N=67), and both participant groups combined (α=0.891; N=129). Test-retest reliability was determined by assessing the relationship between SCPBI-Y scores from enrollment and one-week later using Pearson’s correlation coefficient (outpatient group only). Of the 62 patients in the outpatient group, there were 15 patients who were contacted by phone, but could not be reached within one week. As hypothesized, the SCPBI-Y demonstrated strong test-retest reliability after one week (n=47, r=0.80, p<0.001). Cross-informant concordance (caregiver-child agreement) was analyzed by assessing the relationship between SCPBI-Y scores of youth participants and their caregivers at study enrollment (in the outpatient clinic group only). As expected, the SCPBI-Y demonstrated strong cross-informant concordance (n=40, r=0.78, p<0.001). Since the sample included young adults, there was a portion of our sample who did not have parents available for the study.
Validity
Findings that provide empirical support for construct validity were determined by comparing SCPBI-Y scores to summary scores of measures of similar constructs and these findings are summarized in Table 3. As hypothesized, there were significantly moderate to strong relationships, in which higher scores on the SCPBI-Y (indicating higher pain burden) were related to increased activity limitations and poorer health-related quality of life for the outpatient, inpatient, and combined groups. These analyses provided support for the convergent validity of the SCPBI. Discriminant validity was determined by a significant and weak, inverse relationship, in which higher pain burden on the SCPBI-Y was associated with less positive affect on the PANAS-Positive Affect for the outpatient and combined group and no relationship between these two measures for the inpatient group.
Table 3.
Correlations between SCPBI-Y and CALI, PANAS, and PedsQL
| CALI | PANAS-Positive | PANAS-Negative | PedsQL | |
|---|---|---|---|---|
| SCPBI-Y | ||||
| Outpatient | 0.64*** | −0.28* | 0.49*** | −0.65*** |
| Inpatient | 0.41** | −0.08 | -- | −0.61*** |
| Combined | 0.54*** | −0.31** | -- | −0.66*** |
Note.
p< .05,
p< .01,
p< .001
Strong construct validity was also demonstrated by a positive relationship between higher pain burden and increased number of reported days of pain over the last four weeks for the outpatient group (n=56, r=0.73, p<.001).
Construct validity using a contrasted groups approach was determined on SCPBI-Y scores for the outpatient compared to the inpatient group. As hypothesized, patients in the inpatient group had significantly greater pain burden than patients in the outpatient group (t(127 = −5.12, p<.001); moreover, there were significant differences between patients who exhibited severe symptoms of SCD and patients who exhibited non-severe symptoms (t(57)= −3.52, p=.001) according to the SCD disease classification,8 suggesting that patients with severe SCD reported significantly greater pain burden.
Discussion
This study presents preliminary evidence of reliability and validity of the SCPBI-Y, a brief clinical interview designed to assess pain burden for children and adolescents with SCD. The SCPBI-Y has strong internal consistency and test-retest reliability, supporting our hypothesis; moreover, there was strong concordance between caregiver and child SCPBI-Y total scores. Moderate to strong evidence of construct validity was found with validated measures of mood, functional ability, pain, and quality of life. The SCPBI-Y also discriminated between youth in inpatient versus outpatient settings and those with severe versus less severe SCD symptoms.
Construct validity was demonstrated, in that the SCPBI-Y score strongly correlated with days of reported pain, indicating that patients who experienced more days of reported pain were more likely to experience greater pain burden in both outpatient and inpatient settings. The SCPBI-Y also demonstrated moderate to strong construct validity when compared to functional ability and quality of life measures across outpatient and inpatient groups. Other studies have demonstrated strong relationships between pain and function, and pain and quality of life in patients with chronic pain in general15,19,38 and SCD specifically.16,24 Pain characteristics are associated with significant limitations in daily activities, including school participation.16 In addition, pain may be predictive of physical function within this population.24
Regarding quality of life, there was evidence to suggest that children with SCD experience lower levels of quality of life compared to healthy peers.12 Other studies have found differences between children with mild and severe disease characteristics using PedsQL parent report, suggesting lower quality of life among children with greater severity.28 Also, pain-related hospitalizations have also predicted lower parental reported quality of life scores.25 Thus, the relationship between higher pain burden on the SCPBI-Y and lower quality of life via both parent and child reports is consistent with previous literature.
Negative affect exhibited a moderate to strong relationship with the SCPBI-Y, indicating that higher pain burden was associated with greater negative affect in the baseline (outpatient) group; however, the relationship between the SCPBI-Y score and positive affect was weak for the outpatient group and not significant for the inpatient group. Thus, it is difficult to interpret the relationship between mood and pain burden on the SCPBI-Y. It may be that the SCPBI-Y is more likely to tap into changes in negative rather than positive affect, or that youth with SCD may have elevated levels of depressed affect that contribute to the observed relationship. Previous research in outpatient settings has supported a relationship between negative mood and pediatric SCD pain.13 Our previous study of hospitalized youth with sickle cell disease demonstrated that positive affect was significantly associated over time with youth’s physical function scores but not with their pain scores. In contrast, as in the present study, negative affect was positively associated with pain and inversely associated with youth’s physical function scores.39
Construct validity using contrasted groups approach was determined by comparing SCPBI-Y scores between outpatient and inpatient groups, with the expected finding that youth hospitalized for vaso-occlusive pain had higher pain burden than youth seen in the outpatient clinic setting. Additionally, patients with more severe SCD reported greater levels of pain burden than patients with less severe disease. The findings of this study support strong construct validity for SCPBI-Y, indicating that the SCPBI-Y is sensitive to differences in pain burden by severity for SCD-related symptoms. Youth who require medical care (emergency department visits, hospitalizations) more frequently than others may also have greater pain burden scores.
There were limitations of our study. The mean age for our sample was 15.31 years, reflecting the fact that the majority of our sample consisted of adolescent and young adults with SCD; thus, these results may not generalize to all age groups. Also, since the SCPBI-Y assessed pain burden over the last month, there was potential recall bias among participants. In addition we collected only a limited number of caregiver reports. A number of young adult participants did not have a caregiver present in clinic or in the hospital to complete the study measures. Given the age spectrum of youth with SCD impacted by pain some of our measures were not validated across the age range of participants. Further validation of the SCPBI-Y in a younger SCD sample with more caregivers available will be an important next step with this measure.
While there are a number of clinical assessments that are available for medical personnel to assess the daily impact of SCD (i.e., functional ability, mood, quality of life), many of these measures are lengthy and cumbersome to use in a clinical setting. Few of these measures have been developed specifically for youth with sickle cell disease or to specifically assess pain impact or burden. The PedsQL Generic Core Scale is reliable and valid in youth with sickle cell disease and is also responsive to change during recovery for an acute painful episode; however it is not a pain specific measure.3,28 The PROMIS Pediatric Pain Interference Scale is an 8 item scale which evaluates interference by pain on physical, psychological and social functioning that was recently validated in a mixed illness population and may also be useful in this population, but this will require further study and validation in sickle cell disease.35
The SCPBI-Y is a brief disease-specific, reliable and valid interview that clinicians can use to assess the impact of pain on physical, emotional and social function. The evaluation for pain in youth with SCD usually takes place in the busy clinic or inpatient setting. This tool gives clinicians the opportunity to rapidly assess pain burden, broadening their understanding of their patients pain beyond pain intensity scores and health care utilization and allowing them to understand how pain specifically impacts their patients. Linking pain burden with interventions be they pharmacologic, behavioral or physical may lead to better care of youth with SCD.
Future research should examine the impact of the use of the SCPBI-Y on recognition and treatment of pain in individuals with sickle cell disease. Evaluation of this measure across the life span in younger children, but also into adulthood, will help understand the evolution of pain burden in individuals with SCD. Continued validation of this instrument, in particular, in younger samples and in response to intervention, is a focus of further investigation.
PERSPECTIVE.
Multifaceted pain assessments are salient in providing optimal care to children and adolescents with sickle cell disease; however, current evaluations are lengthy and cumbersome to administer clinically. The current study introduces and validates a brief, clinically useful multidimensional interview to evaluate pain burden specific to youth with sickle cell disease.
Footnotes
Disclosures
This research was made possible through funding from the National Institute of Health (K-23 HL090832) and the Patrick and Catherine Weldon Donaghue Medical Research Foundation. There are no conflicts of interest associated with any of the authors.
References
- 1.Ballas SK. Pain management of sickle cell disease. HematolOncol Clin North Am. 2005;19:785–802. doi: 10.1016/j.hoc.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Barakat LP, Simon K, Schwartz LA, Radcliffe J. Correlates of pain-rating concordance for adolescents with sickle cell disease and their caregivers. Clin J Pain. 2008;24:438–446. doi: 10.1097/AJP.0b013e3181646038. [DOI] [PubMed] [Google Scholar]
- 3.Brandow AM, Brousseau DC, Pajewski NM, Panepinto JA. Vaso-occlusive painful events in sickle cell disease: Impact on child well-being. Pediatr Blood Cancer. 2010;54:92–97. doi: 10.1002/pbc.22222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen LL, Lemanek K, Blount RL, Dahlquist LM, Lim CS, Palermo TM, McKenna KD, Weiss KE. Evidence-based assessment of pediatric pain. J Pediatr Psychol. 2008;33:939–955. doi: 10.1093/jpepsy/jsm103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conner-Warren RL. Pain intensity and home pain management of children with sickle cell disease. Issues Compr Pediatr Nurs. 1996;19:183–195. doi: 10.3109/01460869609026860. [DOI] [PubMed] [Google Scholar]
- 6.Dampier C, Ely E, Brodecki D, O’Neal P. Home Management of Pain in Sickle Cell Disease: A Daily Diary Study in Children and Adolescents. J Pediatr HematolOncol. 2002;24:643–647. doi: 10.1097/00043426-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Dampier C, Ely E, Eggleston B, Brodecki D, O’Neal P. Physical and cognitive-behavioral activities used in the home management of sickle pain: A daily diary study in children and adolescents. Pediatr Blood Cancer. 2004;43:674–678. doi: 10.1002/pbc.20162. [DOI] [PubMed] [Google Scholar]
- 8.Day SW. Development and evaluation of a sickle cell assessment instrument. Pediatr Nurs. 2004;30:451–458. [PubMed] [Google Scholar]
- 9.Eccleston C, Jordan AL, Crombez G. The impact of chronic pain on adolescents: A review of previously used measures. J Pediatr Psychol. 2006;31:684–697. doi: 10.1093/jpepsy/jsj061. [DOI] [PubMed] [Google Scholar]
- 10.Eccleston C, Jordan A, McCracken LM, Sleed M, Connell H, Clinch J. The Bath Adolescent Pain Questionnaire (BAPQ): Development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain. 2005;118:263–270. doi: 10.1016/j.pain.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 11.Ely E, Dampier C, Gilday M, O’Neal P, Brodecki D. Caregiver report of pain in infants and toddlers with sickle cell disease: Reliability and validity of a daily diary. J Pain. 2002;3:50–57. doi: 10.1054/jpai.2002.xb30064. [DOI] [PubMed] [Google Scholar]
- 12.Fuggle P, Shand PA, Gill LG, Davies SC. Pain, quality of life, and coping in sickle cell disease. Arch Dis Child. 1996;75:199–203. doi: 10.1136/adc.75.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gil KM, Carson JW, Porter LS, Ready J, Valrie C, Redding-Lallinger R, Daeschner C. Daily stress and mood and their association with pain: Health care use and school activity in adolescents with sickle cell disease. J Pediatr Psychol. 2003;28:363–373. doi: 10.1093/jpepsy/jsg026. [DOI] [PubMed] [Google Scholar]
- 14.Gil KM, Porter L, Ready J, Workman E, Sedway J, Anthony KK. Pain in children and adolescents with sickle cell disease: An analysis of daily pain diaries. Child Health Care. 2000;29:225–241. [Google Scholar]
- 15.Gold J, Mahrer N, Yee J, Palermo T. Pain, fatigue, and health-related quality of life in children and adolescents with chronic pain. Clin J Pain. 2009;25:407–412. doi: 10.1097/AJP.0b013e318192bfb1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graumlich SE, Powers SW, Byars KC, Schwarber LA, Mitchell MJ, Kalinyak KA. Multidimensional assessment of pain in pediatric sickle cell disease. J Pediatr Psychol. 2001;26:203–214. doi: 10.1093/jpepsy/26.4.203. [DOI] [PubMed] [Google Scholar]
- 17.Hershey AD, Powers SW, Vockell AL, LeCates S, Kabbouche M, Maynard MK. PedMIDAS. Development of a questionnaire to assess disability of migraines in children. Neurol. 2001;57:2034–2039. doi: 10.1212/wnl.57.11.2034. [DOI] [PubMed] [Google Scholar]
- 18.Laurent J, Catanzaro S, Joiner TE, Rudolph KD, Potter KI, Lambert S, Osborne L, Gathright T. A measure of positive and negative affect for children: Scale development and preliminary validation. Psychol Assessment. 1999;11:326–338. [Google Scholar]
- 19.Long AC, Krishnamurthy V, Palermo TM. Sleep disturbances in school-age children with chronic pain. J Pediatr Psychol. 2008;33:258–268. doi: 10.1093/jpepsy/jsm129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maikler VE, Broome ME, Bailey P, Lea G. Childrens’ and adolescents’ use of diaries for sickle cell pain. JSPN. 2001;6:161–169. doi: 10.1111/j.1744-6155.2001.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 21.McClellan CB, Schartz J, Sanchez C, Roberts CW. Validity of the Pediatric Quality of Life Inventory for youth with sickle cell disease. J Pediatr Psychol. 2008;33:1153–1162. doi: 10.1093/jpepsy/jsn036. [DOI] [PubMed] [Google Scholar]
- 22.McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, Eccleston C, Finley GA, Goldschneider K, Haverkos L, Hertz SH, Ljungman G, Palermo T, Rappaport BA, Rhodes T, Schechter N, Scott J, Sethna N, Svensson OK, Stinson J, von Baeyer CL, Walker L, Weisman S, White RE, Zajicek A, Zeltzer L. Consensus statement: Core outcomes domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J Pain. 2008;9:771–783. doi: 10.1016/j.jpain.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: A critical review of the literature. J Dev Behav Pediatr. 2000;21:58–69. doi: 10.1097/00004703-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Palermo TM, Lewandowski AS, Long AC, Burant CJ. Validation of a self-report questionnaire version of the Child Activity Limitations Interview (CALI): The CALI-21. Pain. 2008;31:644–652. doi: 10.1016/j.pain.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palermo T, Schwartz L, Drotar D, McGowan K. Parental Report of Health-Related Quality of Life in Children with Sickle Cell Disease. J Behav Med. 2002;25:269–283. doi: 10.1023/a:1015332828213. [DOI] [PubMed] [Google Scholar]
- 26.Palermo TM, Witherspoon D, Valenzuela D, Drotar D. Development and validation of the Child Activity Limitations Interview: A measure of pain-related functional impairment. Pain. 2004;109:461–470. doi: 10.1016/j.pain.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 27.Panepinto JA, Bonner M. Health-related quality of life in sickle cell disease: Past, present, and future. Pediatr Blood Cancer. 2012 Apr 22; doi: 10.1002/pbc.24176. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Panepinto JA, Pajewski NM, Foerster LM, Hoffmann RG. The performance of the PedsQL™ Generic Core Scales in children with sickle cell disease. J Pediatr HematolOncol. 2008;30:666–673. doi: 10.1097/MPH.0b013e31817e4a44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Platt OS, Thorington BD, Brambilla DJ, Milner PF, Rosse WF, Vichinsky E, Kinney TR. Pain in sickle cell disease: Rates and risk factors. N Engl J Med. 1991;325:11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- 30.Smith WR, Penberthy LT, Bovbjerg VE, McClish DK, Roberts JD, Dahman B, Aisiku IP, Levenson JL, Roseff SD. Daily Assessment of Pain in Adults with Sickle Cell Disease. Ann Intern Med. 2008;148:94–101. doi: 10.7326/0003-4819-148-2-200801150-00004. [DOI] [PubMed] [Google Scholar]
- 31.Smith WR, Scherer M. Sickle-cell pain: Advances in epidemiology and etiology. Hematol. 2010;2010:409–415. doi: 10.1182/asheducation-2010.1.409. [DOI] [PubMed] [Google Scholar]
- 32.Valrie CR, Gil KM, Redding-Lallinger R, Daeschner C. Brief report: Daily mood as a mediator or moderator of the pain-sleep relationship in children with sickle cell disease. J Pediatr Psychol. 2008;33:317–322. doi: 10.1093/jpepsy/jsm058. [DOI] [PubMed] [Google Scholar]
- 33.Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Genetic Core Scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Varni JW, Seid M, Rode CA. The PedsQL™: Measurement model for the Pediatric Quality of Life Inventory. Med Care. 1999;37:126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Varni JW, Stucky BD, Thissen D, DeWitt EM, Irwin DE, Lai J, Yeatts K, DeWalt DA. PROMIS pediatric interference scale: An item response theory analysis of the pediatric pain item bank. J Pain. 2010;11:1109–1191. doi: 10.1016/j.jpain.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walker LS, Greene JW. The Functional Disability Inventory: Measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- 37.Westerman MP, Baily K, Freels S, Schlegel R, Williamson P. Assessment of painful episode frequency in sickle-cell disease. Am J Hematol. 1997;54:183–188. doi: 10.1002/(sici)1096-8652(199703)54:3<183::aid-ajh2>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 38.Wilson A, Palermo T. Physical activity and function in adolescents with chronic pain: A controlled study using actigraphy. J Pain. 2012;13:121–130. doi: 10.1016/j.jpain.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zempsky WT, Palermo TM, Corsi JM, Lewandowski AS, Zhou C, Casella JF. Daily changes in pain, mood, and physical function in youth hospitalized for sickle cell pain. Pain Res Manag. 2013;18:33–38. doi: 10.1155/2013/487060. [DOI] [PMC free article] [PubMed] [Google Scholar]