Abstract
Objective
Large-scale treatment studies suggest that effective depression treatment and reduced depression are associated with improved substance use outcomes. Yet, information is limited regarding the longitudinal association between depressive symptoms and problematic substance use and its predictors, particularly in real-world practice settings. Using latent growth modeling, we examined the: 1) longitudinal association between depressive symptoms and problematic substance use; 2) impact of depressive symptoms on problematic substance use; 3) impact of problematic substance use on depressive symptoms; and 4) role of co-occurring symptoms on depression and problematic substance use.
Methods
Participants were part of the Youth Partners in Care (YPIC) study, an effectiveness trial evaluating a quality improvement intervention for youth depression through primary care. This ethnically diverse sample included youths aged 13 - 21 years screening positive for depression from five health care organizations. Participants were followed four times over an 18-month period and assessed for both depressive symptoms and problematic substance use.
Results
Both depressive symptoms and problematic substance use declined over time. Higher baseline depressive symptoms predicted a slower decline in problematic substance use; but baseline problematic substance use did not predict changes in depressive symptoms. These prospective associations remained robust controlling for co-occurring symptoms.
Conclusions
Results support prior large-scale depression studies indicating depression burden negatively impacts substance use outcome and extends these findings to real world practice settings. Findings underscore the importance of addressing depression severity in youth with concurrent substance use problems, even in the context of comorbid symptoms of anxiety, delinquency, and aggression.
Keywords: Depression, Substance use, Youth, Comorbidity, Longitudinal
Youth who have experienced a major depressive episode within the past year compared to those who have not, report significantly higher rates of substance use (Substance Abuse and Mental Health Service Administration, 2009), with rates of diagnosable substance abuse in those with diagnosed depression being around 25 - 40% (Cohen, Cohen, Kasen & Velez, 1993). Comorbid depressive and substance use disorders are associated with more severe mood symptoms (Swendsen, Merikengas, Canino, Kessler, Rubio-Stipec & Angst, 1998), longer illness duration (Merikangas, Zhang, Avenevoli, Acharya, Neuenschwander et al., 2003), and greater health care utilization (Kessler, McGonagle, Zhao, & Nelson, 1994) than either disorder in isolation. Youth with comorbid disorders seek more treatment in general (Lewinsohn, Clark, Seeley & Rohde, 1994), and tend to be more refractory to interventions (Essau, 2009).
Given the association between adolescent depression and substance use problems, alleviation of depression has the potential to impact substance use trajectories. This question has been explored using data from two large multi-site randomized controlled trials of treatments for adolescent depression: the Treatment of Adolescent Depression Study (TADS; March, Silva, Petrycki, Curry, Wells, Fairbank et al., 2004; Curry, Silva, Rohde, Ginsburg, Kennard, Kratochvil et al., 2012); and Treatment of SSRI-Resistant Depression in Adolescents Study (TORDIA, Brent, Emslie, Clarke, Wagner, Asarnow, Keller et al., 2008; Goldstein, Shamseddeen, Spirito, Emslie, Clarke, Wagner et al., 2009). In both studies, adolescents with substance use disorders (SUDs) were excluded at baseline, but substance use was not an exclusion criterion, and some youths developed SUDs and showed substance-related impairments during the trials. In TADS, adolescents who responded positively to depression treatment had a lower likelihood of developing SUDs than did youths who benefited minimally from depression treatment. Similarly, in TORDIA, there was significant improvement in substance-related impairment among adolescents who responded to depression treatment, with the strongest depression treatment benefits evident among youths with low substance-related impairment at the end of the 12-week acute treatment period, regardless of their baseline levels of substance-related impairment. No significant differential effects of specific depression treatments (cognitive-behavior therapy (CBT) and/or pharmacological) were found in either TADS or TORDIA. In TADS, baseline levels of substance use were associated with poorer response to depression treatment (Curry et al., 2012); in TORDIA baseline substance use impairment, but not frequency of use, showed a marginal association with treatment response (Goldstein et al, 2009; Asarnow, Emsile, Clarke, Wagner, Spirito, Vitiello et al, 2009). Collectively, these findings support the view that decreases in depressive symptoms are likely to lead to reduced substance use problems.
In contrast to the TADS and TORDIA studies which were conducted under highly controlled efficacy/laboratory conditions, the Youth Partners in Care (YPIC) study is a large multi-site effectiveness trial examining the impact of increasing access to evidence-based depression treatments (CBT and/or medication) in primary care clinics under usual practice conditions. The study focused on primary care because most youths in the United States have access to primary care services, and models for improving mental health care outcomes through primary care have shown promise and are likely to be increasingly emphasized in this era of health care reform (Ziv, Boulet, & Slap, 1999; Wells, Tang, Carlson, & Asarnow, 2012; Zuckerbrot, Maxon, Pagar, Davies, Fisher & Shaffer, 2007). The Youth Partners In Care trial (YPIC; Asarnow, Jaycox, Duan, LaBorde, Rea, Murray et al., 2005; Asarnow, Jaycox, Tang, Duan, LaBorde, Zeledon et al, 2009) is among the largest depression intervention effectiveness trials, and the first and largest to be conducted in primary care. As published elsewhere (Asarnow et al, 2005; 2009), youth who received enhanced access to evidence-based interventions demonstrated improved depression outcome at the 6-month follow-up evaluation. A significant indirect path from 6-month to l12 and 18-month outcomes indicated that treatment benefits at 6-months were associated with a shift toward a healthier course at later follow-up points. The current study uses this unique dataset to conduct analyses of the longitudinal covariation of depressive symptoms and problematic substance use over the 18 months of follow-up, examining the impact of substance use problems on the course of depressive symptoms and the impact of depressive symptom severity on the course of substance use problems. One benefit of the YPIC study is that there were few exclusion criteria, and youths with substance use problems were not excluded from the sample, as they were in TORDIA and TADS. Thus, an examination of factors predicting change from baseline levels of depression and substance use is possible given that youth enrolled in the study with pre-existing symptoms and use. Previous YPIC data indicate the enhanced access intervention demonstrated improvements in depression at 6-months; however, it remains unclear as to the course of depression over the full18 month period and how depression severity impacts substance use outcome across the entire sample. Examining prospective associations between depression and substance use over time in the context of an effectiveness study targeting depression will inform our understanding of factors that promote or possibly temper change over time.
Another issue requiring resolution is the impact of comorbidity/co-occurring disorders given that depression in youth is highly comorbid (Angold, Costello, & Erkanli, 1999), and extent literature indicates that comorbidity is associated with a weaker treatment response (Curry, Rohde, Simons, Silva, Vitiello, Kratochvil et al, 2006; Essau, 2009). This issue is particularly critical given that any relationship between youth depression and substance use is likely multifactorial, and therefore, potentially impacted by the presence of other co-occurring symptoms and behaviors. Indeed, observed prospective associations between depression and substance use may be due to unexamined “third variable” factors. The most commonly co-occurring affective and behavioral symptoms in youth with depression are anxiety (25-75%) and conduct problems (21-50%) (Cohen et al., 1993; Kashani, Carlson, Beck, & Hoeper, 1987; Lewinsohn, Rohde, & Seeley, 1998). Research is mixed, however, regarding the impact of anxiety and conduct/deliquency problems on depression and substance use outcome in samples of depressed youth, despite significant associated risks such as violence and suicide in this population (Biederman, Newcorn, & Sprich, 1996; Treuting & Hinshaw, 2001). Some studies suggest that anxiety contributes uniquely to substance use course (Abraham & Fava, 1999; Kendall, Safford, Flannery-Schroeder, & Webb, 2004; Schutte, Hearst & Moos, 1997) and others indicate no effect (Bardone, Moffitt, Caspi, Dickson, Stanton & Silva, 1998; King, Iacono, & McGue, 2004). Delinquency has been associated with substance use specifically; however, studies indicate that aggression and anger, rather than delinquent behaviors, account for the association between conduct behaviors and substance use outcomes (Harty, Miller, Newcorn, & Halperin, 2009; Picardi, Morosini, Gaetano, Pasquini, & Biondi, 2004). Clarifying the role of anxiety, delinquency, and aggression in predicting substance use is important given that depression is highly comorbid with these problems and depression typically presents within the context of a multi-symptom profile (Angold et al., 1999). Because of the effectiveness design employed in YPIC, with youths enrolled regardless of comorbid presentation, this study offers a unique opportunity to examine the impact of co-occurring symptoms, and to assess whether prospective associations between depression and substance use problem outcome are observed, controlling for co-occurring symptoms.
Finally, the mixed research findings within the broader literature focusing on depression and substance use, underscore the need for additional research to clarify temporal associations between depression and substance use problems. By examining these questions in a sample identified with depression we can better understand how disorder processes relate over time. Some studies suggest that depression predicts the development of substance use (Birchwood, Mason, MacMillian, & Healy, 1993; King et al., 2004), others indicate that substance use precedes the development of depression (Brook, Brook, Zhang, Cohen, & Whiteman, 2002; Newcomb & Bentler, 1989; Rodhe, Lewinsohn, Kahler, Seeley, & Brown, 2001), and others suggest that symptoms are reciprocal over time (Brown, Lewinsohn, Seeley, & Wagner, 1996; Newcomb, Vargas-Carmona, & Galaif, 1999). The majority of studies however, are limited by methodological issues such as cross-sectional or short-term (two-wave) longitudinal designs (Chassin, Flora, & King, 2004; Cole & Maxwell, 2003; Schutte et al., 1997). Studies employing multiple time points have strong potential for clarifying prospective associations between depression and substance use (Fleming, Mason, Mazza, Abbott & Catalano, 2008).
The major aim of the current study was to examine associations between depression and substance use among youths participating in one of the largest depression treatment effectiveness trials ever conducted with youths, the YPIC study. This effectiveness trial included youths screening positive for depression, with few exclusions (e.g. acute psychosis that would interfere with ability to participate in assessments and interventions). Youths with substance use problems were included in the sample, as were youths with the full range of comorbid symptom presentations typical of depressed youths in primary care. Data were available over four waves of assessment spanning an 18-month follow-up period, allowing longitudinal analyses of associations between depression and substance use over time, as well as the impact of co-occurring symptoms of anxiety, aggression, and delinquent behaviors on prospective associations between depressive symptoms and substance use problems. We hypothesized that: 1) consistent with results of other major depression treatment trials (Goldstein et al., 2009; Curry et al., 2012), higher depression levels would be associated with less improvement in problematic substance use over the course of the 18-month follow-up, and 2) while co-occurring symptoms of anxiety, aggression, and delinquency would be predictive of longitudinal course, associations between depressive symptoms and problematic substance use would remain robust controlling for these covariates.
Method
Participants and Procedure
Participants were drawn from the YPIC study, a multi-site study that screened consecutive youth patients for depressive symptoms across six clinical sites within five diverse health care organizations. Institutional review boards of all participating organizations approved the study. As detailed descriptions of methods are available elsewhere, an overview is provided (for additional information: Asarnow et al., 2005; 2009). Participants aged 13 to 21 years were recruited during their primary-care visit and enrollment eligibility determined through in-clinic screenings using brief self-administered questionnaires. The present study included 451 youths who participated in the YPIC baseline assessment. Overall study eligibility criteria were: (1) youth endorsed “stem items” for major depression or dysthymia from the 12-month Composite International Diagnostic Interview (CIDI-12; World Health Organization, 1997) modified slightly to conform to diagnostic criteria for adolescents, 1-week or more of past-month depressive symptoms, plus a total Center for Epidemiological Studies-Depression Scale (CES-D) score ≥ 16; or (2) CES-D score ≥ 24 (Radloff, 1977). Following common adolescent medicine practices (Society for Adolescent Health and Medicine, 1995), we defined adolescence broadly extending into the transitional age period. Exclusion criteria included non-English-speaking, medical provider not in study, and the presence of a sibling in the study. Across sites, a total 4,783 youth were eligible for screening, 84% (4,002 youth) completed the screener, and 1,034 of these 4,002 youths (26%) screened positive for depressive symptom burden and were eligible for enrollment. Of those, 519 enrolled (50%), with 86% of the enrolled sample (N=451) completing baseline assessments (Time 1). Reasons for not enrolling in the study included no contact information (.03%), refused (12%), and agreed but did not consent (16%) (see Asarnow et al, 2005). As noted elsewhere (Asarnow et al, 2005), differences between those enrolled vs. not enrolled were found by site, gender, and ethnicity. We note this as a study limitation, and explore the impact of these variables on the data (see Results section). Youth were then followed at 6-, 12-, and 18-months post-baseline forming the longitudinal dataset. As noted, the larger sample (N=451) includes an additional 33 youths who were in the pilot phase and were not in the randomized trial (n=418) (Asarnow et al., 2005; 2009). At Time 1 (baseline), youth had a mean age of 17.2 years (SD = 2.06, range 13.2 – 21.10 years) were included. The sample was predominantly female (n = 355, 71%) and largely minority (Latino n = 252, 56%; Biracial n = 63, 14%; African American n = 59, 13%; Caucasian n = 55, 12%; Other n = 14, 3%, and Asian n = 6, 1%). Regarding subsequent time points in the larger sample (N=451), 86 (19%) youth dropped between Time 1 and Time 2 (Time 2 sample, N = 365, 81% retention), a further 38 (10% of Time 2 sample) dropped by Time 3 (N = 327), and another 5 (1.5% of Time 3 sample) dropped by the final time point (N = 322), with an overall retention rate of 71%.
Measures
The Composite International Diagnostic Interview (CIDI-12; World Health Organization, 1997) was used to measure depressive symptoms. This structured interview was administered by trained interviewers with ongoing quality assurance assessments to ensure reliability. A symptom count within the past 12 months (past six months between time points two and four) was used and provided a continuous measure of symptoms. Higher scores indicated more depressive symptoms. All interviewers were trained and supervised by senior staff with official CIDI and Diagnostic Interview Schedule (DIS) training and more than 10 years of experience in conducting CIDIs and the DIS. Regular quality assurance monitoring was conducted, with quality assurance ratings on a randomly selected 10% of interviews indicating strong quality (Scale range, 1-3, 1=highest quality, Mean 1.02, SD 0.06) (Asarnow et al, 2005). The Problem Oriented Screening Instrument for Teenagers (POSIT; Radhert, 1991) provided an assessment of problems associated with substance use. The use of a measure of problematic substance use versus an assessment of quantity and frequency of use was chosen as data suggest that problematic substance use as a construct may be more related to internalizing symptoms than are measures of frequency and quantities of use (Newcomb & Bentler, 1989); therefore, limiting analyses to frequency and quantities of use when examining links with internalizing symptoms may miss important relationships. POSIT questions were answered yes/no, and scores range from 0 – 13. Higher scores indicate greater problematic substance use. The substance use subscale of the POSIT demonstrated good internal consistency (Cronbach’s alpha .82) in this sample and adequate convergent validity with the Personal Experience Inventory in published studies (correlation of .60; McLaney, Del Boca, & Babor, 1994). Critically, participants were assured of confidentiality regarding their use of substances to enhance accurate reporting of behaviors.
Covariates were measured as follows: (a) Anxious symptoms were assessed using the Brief Symptom Inventory - Anxiety subscale (BSI: Derogatis & Melisaratos, 1983), and included six items rated as 0 = not at all true through 4 = extremely true within the past 30 days; higher scores indicating greater anxiety. This measure demonstrated adequate internal consistency (Cronbach’s alpha .78) in this sample and good test-retest reliability in other published studies (kappa = 0.79; Kellet, Beail, Newman, & Frankish, 2003), (b) the aggressive symptom and delinquency variables were assessed using their respective subscales of the Youth Self Report (YSR; Achenbach, 1991) and Young Adult Self Report (YASR; Achenbach, 1997). The YSR is normed on youth aged 11 - 18 years, and the YASR is normed on youth aged 18 - 30 (12 items). Both the YSR and YASR were used given the age distribution of the sample being from 13 to 21. Total scores were generated with higher scores indicating more symptoms/behaviors. Three questions regarding substance use were removed from YSR/YASR Delinquency scale to prevent confounding effects. The YSR/YASR demonstrated high internal consistency in this sample (Cronbach’s alpha .91) and adequate test-retest reliability in published studies (kappa .60; Achenbach, 1991, 1997).
Data Analytic Strategy
As we were interested in examining change over time between two factors (depressive symptoms and problem-substance use), latent growth models (LGM) with parallel-processes were used (Curran, Stice, & Chassin, 1997; Fleming et al, 2008). LGM with parallel-process allowed for an examination of change over time in the constructs of depressive symptoms and substance use problems, as well as the ability to test predictive relations between constructs and covariates. Steps in model building followed established guidelines (see Muthén & Muthén, 1998-2004 for additional information). The latent intercept and growth variables were formed by the depressive symptom and problem substance use indicators at each time point, a common methodology in parallel-process LG modeling (Curran et al., 1997; Fleming, et al., 2008). We used Mplus 3.13 (Muthén & Muthén, 1998-2004) to test LG models. Goodness of fit of the models was evaluated using the root-mean-square error of approximation (RMSEA) and its 90% confidence interval (CI), the Tucker-Lewis index (TLI), the Comparative Fit Index (CFI) and the standardized root-mean-square residual (SRMR). Acceptable model fit was defined in part by the criteria forwarded by Hu and Bentler (1999): RMSEA values close to .06 or below (90% CI limit), CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. Multiple indices were selected because they provide different information for evaluating model fit (i.e., absolute fit, fit adjusting for model parsimony, fit relative to a null model). Together, these indices provide a more conservative and reliable evaluation of model fit. Strength of effects were examined by looking at the significance of parameter estimates at the p < 0.05 level and by examination of effect size following Cohen’s d estimations where d = .20, .50, and .80 for small, medium, and large effects. Direction of effects was determined by the valence (positive indicating increasing change/growth and negative indicating decreasing change/growth) of the coefficient. We report standardized values in all models. Missing data were handled by maximum-likelihood estimation (direct ML) under the assumption of missingness at random (MAR) (Allison, 2003; Raykov, 2005). This method is more efficient and produces less biased parameter estimates than other methods such as mean/regression imputation, pairwise or listwise deletion strategies (Schafer & Graham, 2002). Although it is not possible to explicitly test the assumption of MAR (Enders, 2010), we included variables in analyses that may be associated with missingness (see Results section), thereby bolstering support for the appropriateness of the MAR assumption in this case. Prior to all LGM analysis however, we first examined initial normality, univariate and multivariate outlier assumption testing was conducted using SPSS V15.0 (SPSS Inc. 2008).
Results
Descriptive Statistics
Table 1 reports means, standard deviations, variance, and zero-order correlations among the primary clinical variables (depressive symptoms, problematic substance use) and covariates. As seen in Table 1, depressive symptoms and problematic substance use behaviors decreased over time. Consistent with prior reports on these data (Asarnow et al., 2009), declines in depressive symptoms were greatest between baseline (Time 1) and Time 2 (at the end of the 6-month intervention period). A similar pattern of more rapid declines in substance use problems between Time 1 and 2 was also observed (See Mean depression and substance use problem scores in Table 1). At Time 1, most youths were experiencing moderate levels of depressive symptoms, with roughly forty-two percent meeting diagnostic criteria for Major Depressive Disorder. At Time 1, 202 youth reported any substance use (excluding tobacco and caffeine), of which 112 (24.8%) endorsed ≥1 problem associated with substance use (see Table 2 for distribution of substances used). Regarding the covariates, on the YSR/YASR, 28% of the sample endorsed clinically significant levels of problem behavior across the delinquency or aggressive behavior scale, and 64% endorsed ≥3 items out of six on the BSI indicating a substantial subgroup with anxiety symptoms at baseline.
Table 1.
Correlations and Descriptive Statistics among Covariates, Depressive Symptoms and Problematic Substance Use at All Waves. (N=451)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | .13** | −.04 | .12* | −.08 | .17** | .14** | .05 | −.01 | −.02 | −.01 | .02 | −.21** | −.35** |
| 2. Gender | - | −.07 | .10* | .14* | .10 | −.00 | .11* | .08 | −.03 | −.12 | .03 | −.12* | −.22** | |
| 3. Ethnicity | - | .05 | .08 | .10 | .06 | .12* | .03 | −.01 | .01 | .10* | .13* | .06 | ||
| 4. Depressive Sx T1 | - | .42** | .31** | .32** | .16** | .26** | .19** | .13* | .46** | .31** | .19** | |||
| 5. Depressive Sx T2 | - | .44** | .39** | .11* | .25** | .27** | .18** | .32** | .16** | .07 | ||||
| 6. Depressive Sx T3 | - | .43** | .14* | .17* | .25** | .14* | .24 | .13* | .03 | |||||
| 7. Depressive Sx T4 | - | .12* | .22** | .20** | .23** | .21* | .12* | −.01 | ||||||
| 8. Problem Use T1 | - | .59** | .56** | .49** | .26** | .26** | .43** | |||||||
| 9. Problem Use T2 | - | .75** | .55** | .23** | .21** | .33** | ||||||||
| 10. Problem Use T3 | - | .70** | .21** | .23** | .31** | |||||||||
| 11. Problem Use T4 | - | .21** | .22** | .24** | ||||||||||
| 12. Anxiety | - | .39** | .23** | |||||||||||
| 13. Aggression | - | .63** | ||||||||||||
| 14. Delinquency | - | |||||||||||||
| Mean | 17.2 | - | - | 8.53 | 5.65 | 3.86 | 3.06 | .84 | .66 | .69 | .59 | 4.90 | 9.78 | 3.87 |
| Standard Deviation | 2.06 | - | - | 4.19 | 5.67 | 5.32 | 4.66 | 1.98 | 1.67 | 1.76 | 1.59 | 4.51 | 5.89 | 3.22 |
| Skewness | .22 | - | - | −.31 | .45 | .98 | 1.26 | 3.08 | 3.02 | 2.82 | 3.41 | 1.33 | .71 | 1.12 |
| Kurtosis | .65 | - | - | -1.22 | -1.11 | −.42 | .299 | 10.4 | 10.0 | 8.27 | 13.0 | 1.98 | .41 | 1.55 |
Note.
= p<.05.
p<.01.
Depressive Sx T1-T4 = Depression symptom count from the CIDI at Times 1-4; Posit T1-T4 = Problem Oriented Screening Inventory for Teens at Times 1-4.
Table 2.
Substance use at baseline.
| Substance Used | Total (N = 202)+ |
|---|---|
| Alcohol | 62.9% |
| Days alcohol used in past 30, mean (SD) |
1.5 (4.2) |
| Marijuana | 59.2% |
| Any other drug | 20.6% |
| Amphetamines | 12.1% |
| Barbiturates | 8.5% |
| Cocaine | 10.6% |
| Tranquilizers | 5.0% |
| Heroin | 0.7% |
| Other opioids | 1.4% |
| LSD | 9.3% |
| Other drug | 5.0% |
Preliminary Analyses and Attrition
All variables were examined for normality, linearity, and both univariate and multivariate outliers. As shown in Table 1, several variables evidenced significant skewness and kurtosis (thus, leading to the use of the MLR fitting function). Data coverage in the sample for the depressive symptom and problematic use indicators ranged from 100% to a minimum of 66% and for the covariates from 98 - 100%, suggesting adequate data coverage. Regarding attrition, logistic regression equations predicting drop out across waves were conducted including all study variables of interest as well as demographic variables of gender, age, and ethnicity. Only age emerged as a predictor of attrition, with older youths more likely to drop by Time 2 (p = 0.002; mean age of dropped out cases 17.8 vs. 17.0 years for those retained in the sample) but not Times 3 and 4. We thus included age as a covariate in study models to control for these effects. Given this was a multi-site study we examined site differences across study variables of interest. No differences were found across baseline variables by site suggesting that youths were similar regarding their level of depressive symptom severity, problematic substance use, and co-occurring symptom levels by site.
Intervention Effects
Regarding intervention condition, we examined the impact of randomization condition (quality improvement (QI) intervention vs. usual care (UC)) on the examined model. Because these analyses examined effects of intervention condition, they included only the N=418 youths in the randomized controlled trial (with the additional 33 pilot participants not included). A dummy code was created for intervention condition, with QI coded as 1 and UC coded as 0, and the LGM model was regressed onto this covariate (a suitable method for examining multiple-groups differences (Brown, 2006) in LGM). The model fit the data adequately (χ2(25) = 49.9, p = 0.002, SRMR = .04, RMSEA= .05 (90% CI[.03 - .05]), TLI = .94, CFI = .95). Results indicated that regression paths predicting initial levels and change from the randomization group covariate were not statistically significant. Thus, initial level and change in depression and substance use symptoms over time did not differ between intervention groups. Intervention condition was therefore not included in the main models reported below. However, a secondary analyses was conducted including the treatment condition covariate and all other covariates in the subsample of randomized youth to control for any potential variance accounted for by treatment condition. Results of the main model as described below were similar with no change in conclusions.
Prospective Associations and Role of Covariates
Using the larger sample of N=451 to increase power and generalizability, a LGM with parallel-process was fit to the data. As we were interested in assessing temporal associations between initial depressive symptoms and problem substance use and outcome, and whether inclusion of covariates impacted associations, we examined whether initial depressive symptoms levels predicted change in problem use, and whether initial problem substance use levels predicted change in depressive symptoms over time controlling for the covariates of interest. Regression paths were therefore specified within and between intercepts and slopes, and between intercepts and slopes and the covariates of anxiety, aggression, and delinquency (and age and gender were included to control for their effects). This model allowed us to therefore concurrently examine the longitudinal associations between depressive symptoms and problem substance use, whether any associations between depressive symptoms and problem use were significant controlling for the covariates of interest, and how the covariates of interest impacted any prospective associations.
The overall model fit the data adequately, χ2(41) = 58.39, p=0.03, SRMR = .03, RMSEA= .03 (90% CI[.01 - .04]), TLI = .96, CFI = .98. Time points 2 and 3 in both the depressive symptom and problematic substance use processes were freely estimated (with growth specified as non-linear: Time 1= 0, Time 2 = *, Time 3 = *, and Time 4 = 1, with * = freely estimated indicator with 0 = beginning of growth trajectory). This growth process was specified as our interest was in the amount of and individual differences in change between baseline and 18 months follow-up time points. Moreover, a non-linear growth trajectory provided superior fit to the data than a linear growth trajectory. Error covariances were fixed to equality within the substance use process as earlier steps in model building (not detailed here for space reasons) indicated convergence issues when the substance use error variances were freely estimated, and inadequately modeled error has been reported as a potential factor leading to improper solutions (Brown, 2006).
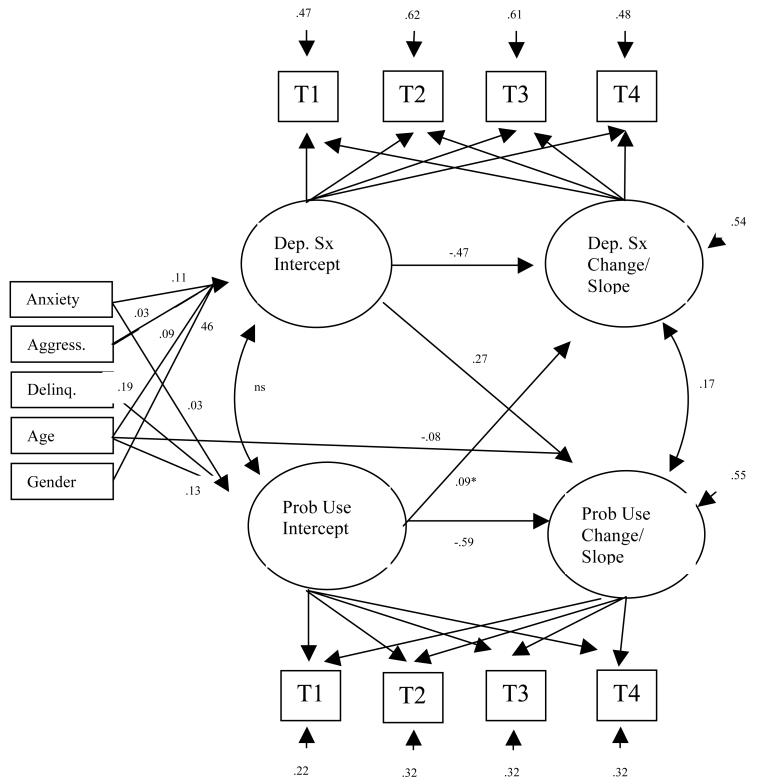
As seen in Table 3, intercept and slope factors were significant, with both slopes evidencing a negative mean change (see Mean scores for depressive symptom and problem use slopes), indicating a decrease in depressive symptoms and problematic substance use over time. Figure 1, provides details of the LGM more specifically. Thus, the slope of problematic substance use was regressed onto the intercept of depressive symptoms, and the slope of depressive symptoms was regressed onto the intercept of problem substance use. Data indicate that holding initial levels of problematic substance use and the background covariates constant, there was a significant effect of depressive symptoms predicting problem substance use change over time (standardized value: 0.27, z-value 1.96, p < 0.05, Cohen’s d = .25) (represented in Figure 1 by the arrow from depression intercept to problem use slope). Importantly, as the regression path from depressive symptom initial status to problematic substance use slope was statistically significant (p < .05) and positively signed, an interaction effect emerged with the effect of time on problematic substance use differing across levels of depression. The positive sign of this path combined with an overall negative slope mean (indicating a reduction in problematic substance use), suggests that youth who experienced higher initial levels of depressive symptoms at baseline evidenced a less steep decline in problematic substance use over time. No significant effect of initial problematic substance use predicting change in depression emerged, holding initial depression severity and background covariates constant (standardized value .09, z-value 0.84, p > 0.05, Cohen’s d = .09) (arrow in Figure 1 shown for presentational clarity). We also examined within process associations. Here, the slope of depressive symptoms was regressed on the initial level of depressive symptoms (and the slope of problematic substance use was regressed on the initial level of problematic substance use). Again, as noted in Figure 1, regression paths (arrows linking depressive symptoms intercept to depressive symptom slope, and problematic substance use intercept to problematic substance use slope) were significant and negative, indicating that youth with higher initial depressive symptoms evidenced a faster decline in depressive symptoms, and youth with greater initial problematic substance use evidenced a faster decline in problematic substance use over time. Correlations between intercepts and slopes were also specified in the model (curved arrows linking depression and problem use intercept, and depression slope and problem substance use slope). Here only slope factor correlations were significant suggesting changes over time in one process was associated with changes in the other.
Table 3.
Mean and variance coefficients for Depressive symptoms and Problem Substance Use intercept and slopes (N=451)
| Parameter | Coeff. (SE) | Coeff./SE (Z-Value, p <0.5) |
|---|---|---|
| Depressive sx: Intercept | ||
| Intercept Mean | 8.53 (.27) | 31.33 |
| Intercept Variance | 17.6 (2.8) | 6.29 |
| Depressive sx: Slope | ||
| Slope Mean | −5.49 (.32) | −17.1 |
| Slope Variance | 11.24 (4.2) | 2.66 |
| Problem Sub. Use: Intercept |
||
| Intercept Mean | .85 (0.9) | 8.97 |
| Intercept Variance | 3.03 (0.6) | 4.95 |
| Problem Sub. Use: Slope | ||
| Slope Mean | −.211 (.09) | −2.23 |
| Slope Variance | 1.78 (.62) | 2.84 |
Figure 1.
Parallel-process latent growth model of depressive symptoms and problematic substance use with arrows representing directional paths between latent variables, and between latent variables and covariates age, gender, anxiety, aggression, and delinquency (N=451). For presentational clarity, only significant standardized estimates shown (z-value > 1.96, p <.05). ns = non-significant correlation linking Dep. Sx intcept and Prob. Use. Intercept. For residual variances, unstandardized variances shown. Dep. Sx = depressive symptoms, Prob. Use = Problematic Substance use, Aggress. = aggression, and Delinq. = delinquency. T1 = Time 1/baseline, T2 = Time 2, T3 = Time 3, T4 = Time 4. All intercept factor loadings fixed to 1.0. Slope factor loadings fixed to 0.0 at T1 and 1.0 at T4, with T2 and T3 freely estimated. Freely estimated factor loadings for T2 and 3 are .32 and .54 for Depression slope and .59 and .73 for Problem Use slope. * = ns path shown completeness.
As noted previously, we sought to examine how the covariates of interest predicted any associations. Thus, the intercepts and slopes of depressive symptoms and problem substance use (as represented by arrows pointing from covariates to both intercepts and slopes in Figure 1 with only significant paths shown) were regressed onto the covariates of anxiety, aggression, and delinquency (and age and gender to control for their effects). Data indicated that higher initial depressive symptoms were predicted by greater levels of anxiety, higher aggression scores, being older, and male. Greater delinquent behaviors, higher levels of anxiety, and older age predicted higher initial problematic substance use scores. Temporal change in either depression or problem substance use was not predicted by any covariate other than age: Older youth evidenced a faster rate of decline in problematic substance use symptoms over time.
Discussion
Major findings of the present study are: 1) within the context of one of the largest extant youth depression treatment effectiveness trials, youth showed declines in depression and substance use outcomes over time; 2) higher initial depressive symptom severity predicted a slower decline in problematic substance use over time; 3) there were no effects for initial problematic substance use impacting change over time in depressive symptoms, supporting unidirectional associations between depression and substance use in this depressed sample; and 4) prospective associations remained robust controlling for the presence of comorbid/co-occurring symptoms with covariates predicting initial severity of depression and problematic substance use more so than temporal change.
Role of Intervention Condition
The present results must be viewed within the context of other results from the YPIC study. As reported elsewhere, the primary YPIC analyses demonstrated that improving access to evidence-based depression treatments through primary care was associated with improved depression outcomes at the end of the 6-month intervention period (Asarnow et al., 2005), with early improvements associated with a shift towards healthier pathways through 12 and 18-months of follow-up (Asarnow et al. 2009). Instrumental variable analyses further indicated that when youths in the YPIC trial received treatments that met at least minimum criteria for appropriate depression care given current guidelines, they had a significantly reduced likelihood of severe depression, falling from 45.2% for those without appropriate treatment, to 10.9% with appropriate treatment broadly (Wells et al., 2012). The present findings indicating that initial depressive symptom severity slowed change over time in problematic substance use underscores the notion that improved substance use outcome is related to depressive symptom severity, underscoring the adverse impact of high depression levels. Our results showing that depression severity negatively impacts substance use outcome are consistent with those for the two major adolescent depression treatment efficacy trials conducted in the United States – TADS (Curry et al., 2012) and TORDIA (Goldstein et al., 2009). We extend these findings however, by demonstrating that depression negatively impacts substance use course across a diverse range of patient groups and under real-world practice conditions. These key findings underscore the need to target depression severity to improve substance use outcome in youth. It is however, important to note that the present results differ from the primary YPIC analyses (as reported elsewhere see Asarnow et al, 2005; 2009) in that the present analyses collapsed across intervention groups and time points, and focused on the average slope of change across the 6, 12, and 18 month follow-ups. Moreover, the present analyses incorporated different depression outcome measures.
Prospective Associations and Role of Covariates
We also examined temporal associations between depressive symptoms and problematic substance use. In this sample of youth identified with and treated for elevated depressive symptoms, our data support uni-directional models of depression impacting substance use given that 1) initial levels of depression were predictive of change in substance use, and 2) initial levels of problematic substance use were not significantly associated with changes in depression level over time. The finding of uni-directional vs. reciprocal associations may be related to the fact that the sample was selected for the presence of depression and the study emphasized depression treatment. These results, nevertheless, are consistent with Affect Regulation (Cappell & Greeley, 1987) and Self-Medication (Khantzian, 1997) theories that view substance use as a self-regulation strategy for responding to the emotional distress and dysphoria present in depression. Our findings regarding within process change suggest that youth with higher initial depressive symptoms evidenced a faster decline in depressive symptoms change, and youth with higher initial problem substance use also evidenced a faster decline in problem substance use change. These findings may be related to youth with higher initial levels having greater variance to change over time. An important finding from the present study is that inclusion of the covariates of anxiety, aggression, and delinquency did not fully account for the observed relationship between depressive symptoms and problematic substance use. This has heretofore been unexamined in a sample of depressed youth. Our findings demonstrate that associations between depression and problematic substance use are robust, not accounted for by these measures of co-occurring symptoms/comorbidity effects, and underscore the importance of improving depressive symptoms even in a community sample with high levels of comorbid symptoms and behaviors. Of interest, the covariates examined contributed to depressive symptoms and problem use in different ways. Being older, male, and having a greater level of both aggression and anxiety predicted higher levels of initial depressive symptoms; whereas higher levels of initial problematic substance use was associated with higher rates of delinquent behaviors, higher anxiety levels, and older age. Aggression did not account for associations between delinquency and problematic substance use. Anxiety is relevant to both initial depressive symptom severity and problematic substance use, whereas delinquency appears to be specific to problematic substance use initial severity. The finding that older age predicted both more severe depression and problematic substance use initial levels is consistent with the developmental processes in depression and substance use whereby older adolescents experience higher rates of depression and substance use compared to younger adolescents. Temporal change in general was more difficult to predict by the current variables, although older age was predictive of a faster rate of decline in problematic substance use. This latter finding appears consistent with the tendency of youth to mature out of problematic substance use as they enter their early twenties (SAMHSA, 2009) the upper age limit in the YPIC trial. Limited prediction of temporal change has been noted in other longitudinal studies examining the impact of covariates on growth (Windle & Windle, 2001).
Limitations
The present findings need to be considered in the context of study limitations. As noted previously, while not all youths with positive depression screens enrolled in the study, the YPIC sample was large, diverse, included primary care patients sampled from six sites in five different health care organizations, supporting the view that the sample is broadly representative of the sampled population. Further, the study aimed to examine the study questions within a sample of depressed primary care youth patients; results may not generalize to non-depressed youths or to youths sampled from other settings. Further research is needed to determine whether different patterns might emerge for youth selected for the presence of primary substance abuse/misuse and/or in treatment settings were substance use is the focus. Moreover, given the emphasis on depression treatment in the YPIC study, stronger predictive effects between depressive symptom growth and problematic substance use growth might be expected. The study results indicate that changes in depressive symptoms are associated with changes in substance use problems; this change could have been due to naturally occurring change or treatment effects. Although initial level and change in depression and substance use symptoms over time did not differ significantly between intervention groups, an examination of differences between intervention groups regarding the parallel process was unable to be conducted as initial conditions appropriate for conducting multi-group comparisons were not met i.e., the model did not evidence appropriate goodness of fit in each separate treatment group. Therefore direct comparisons between the two intervention conditions cannot be made. A further limitation is that while youths were followed over 18 months, a longer observation period might have yielded different patterns. Further, the problematic use outcome variable combined both alcohol and drug use behaviors. Thus, distinctions among different substances cannot be made and under-reporting of substance use may have occurred. Indeed, data suggest differential associations with depressive symptoms and different types of substances (Fleming et al., 2008); therefore, future studies should attempt to differentiate associations by substance type. Finally, YPIC was a health services project which aimed to reduce assessment burden and maximize study feasibility with a primary care population. Therefore, we used dimensional measures of the psychopathology constructs. Future studies including more detailed diagnostic assessments could expand understanding of different diagnostic/co-occurring symptom patterns. Moreover, the variables studied were not exhaustive and it is possible that other, untested variables may be of relevance in explaining prospective associations in youth with depression and problematic substance use.
Implications for Research, Policy, and Practice
Consistent with the emphasis in the National Prevention Strategy (National Prevention Council, 2011) on developing integrated care programs to address mental health, substance abuse, and other needs within primary care settings, as well as recommendations from the US Preventive Services Task Force (2009) to screen adolescents for depression when resources are adequate for evaluation and treatment/follow-up, the present results underscore the pernicious effects of depression over time in adolescent primary care patients. Other research indicating that primary care interventions for adolescent depression as well as substance abuse are associated with improved outcomes (Asarnow et al., 2005; 2009; Cheung, Zuckerbrot, Jensen, Ghalib, Laraque, & Stein, 2007; D’Amico, Miles, Stern, & Meredith, 2008) support the value of primary care screening and treatment strategies. The co-occurrence of depression and substance use problems is associated with particularly adverse outcomes, including suicide and suicide attempts (National Prevention Council, 2011), highlighting the need to further clarify the mechanisms associated with the high co-occurrence between these behaviors, the diverse pathways through which depression and substance use problems impact later outcomes, and the need to develop strategies for interrupting cycles of continuing dysfunction.
Acknowledgments
This study was supported by Agency for Health Care Research and Quality grant HS09908 (P.I. Joan R. Asarnow, Ph.D.) and National Institute of Mental Health grant MH078596 (P.I. Joan R. Asarnow, Ph.D.) Additional support was provided by the American Psychological Association 2009 Dissertation Research Award to the first author.
References
- Abraham H, Fava M. Order of onset of substance abuse and depression in a sample of depressed outpatients. Comprehensive Psychiatry. 1999;40:44–50. doi: 10.1016/s0010-440x(99)90076-7. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. Manual for the Youth Self-Report and 1991 profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Achenbach TM. Young Adult Self Report. University of Vermont, Department of Psychiatry; Burlington, VT: 1997. [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. Journal of the American Medical Association. 2005;293:311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Emslie G, Clarke G, Wagner KD, Spirito A, Vitiello B, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, Tang L, Duan N, LaBorde AP, Zeledon LR, Anderson M, Murray P, Landon C, Rea M, Wells KB. Are there long-term benefits of short-term quality improvement interventions for depressed youth in primary care? American Journal of Psychiatry. 2009;166:1002–10. doi: 10.1176/appi.ajp.2009.08121909. [DOI] [PubMed] [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. Journal Of The American Academy Of Child and Adolescent Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. American Journal Of Psychiatry. 1996;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Mason R, MacMillan F, Healy J. Depression, demoralization and control over psychotic illness: A comparison of depressed and non-depressed patients with a chronic psychosis. Psychological Medicine. 1993;23:387–395. doi: 10.1017/s0033291700028488. [DOI] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. Journal of the American Medical Association. 2008;299:901–13. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence and substance use disorders. Archives Of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. Guilford Press; New York, NY: 2006. [Google Scholar]
- Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1602–1610. doi: 10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Cappell H, Greeley J. Alcohol and tension reduction: An update on research and theory. In: Blane HT, Leonard KE, editors. Psychological Theories of Drinking and Alcoholism. Guilford Press; New York: 1987. [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE. Guidelines for adolescent depression in primary care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120:1313–26. doi: 10.1542/peds.2006-1395. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez CN. An epidemiological study of disorders in late childhood and adolescence: I. Age- and gender-specific prevalence. Journal Of Child Psychology And Psychiatry. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Stice E, Chassin L. The relation between adolescent alcohol use and peer alcohol use: A longitudinal random coefficients model. Journal of Consulting and Clinical Psychology. 1997;65:130–140. doi: 10.1037//0022-006x.65.1.130. [DOI] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, March J. Predictors and Moderators of Acute Outcome in the Treatment for Adolescents With Depression Study (TADS) Journal Of The American Academy Of Child and Adolescent Psychiatry. 2006;45:1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Curry J, Silva S, Rohde P, Ginsburg G, Kennard B, Kratochvil C, et al. Onset of alcohol or substance use disorders following treatment for adolescent depression. Journal of Consulting and Clinical Psychology. 2012;80:299–312. doi: 10.1037/a0026929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal Of Substance Abuse Treatment. 2008;35:53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Enders CK. Applied missing data analysis. Guilford Press; New York, NY US: 2010. [Google Scholar]
- Essau CA. Progress and unresolved issues in the treatment of adolescent depression. In: Essau CA, editor. Treatments for adolescent depression: Theory and practice. Oxford University Press; New York, NY US: 2009. pp. 313–319. [Google Scholar]
- Fleming C, Mason A, Mazza J, Abbott R, Catalano R. Latent growth curve modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Goldstein BI, Shamseddeen W, Spirito A, Emslie G, Clarke G, Wagner KD, Asarnow JR, Vitiello B, Ryan N, Birmaher B, Mayes T, Onorato M, Zelazny J, Brent DA. Substance use and the treatment of resistant depression in adolescents. Journal of American Academy of Child Adolescent Psychiatry. 2009;48:1182–92. doi: 10.1097/CHI.0b013e3181bef6e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harty SC, Miller CJ, Newcorn JH, Halperin JM. Adolescents with childhood ADHD and comorbid disruptive behavior disorders: Aggression, anger, and hostility. Child Psychiatry And Human Development. 2009;40:85–97. doi: 10.1007/s10578-008-0110-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kashani JH, Carlson GA, Beck NC, Hoeper EW. Depression, depressive symptoms, and depressed mood among a community sample of adolescents. American Journal Of Psychiatry. 1987;144:931–934. doi: 10.1176/ajp.144.7.931. [DOI] [PubMed] [Google Scholar]
- Kellett S, Beail N, Newman D, Frankish P. Utility of the Brief Symptom Inventory in the assessment of psychological distress. Journal of Applied Research in Intellectual Disability. 2003;16:127–134. [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child Anxiety Treatment: Outcomes in Adolescence and Impact on Substance Use and Depression at 7.4-Year Follow-Up. Journal Of Consulting And Clinical Psychology. 2004;72:276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB. Lifetime and 12-month prevalence of DSM-III—R psychiatric disorders in the United States: Results from the National Comorbidity Study. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King S, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in prospective prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal Of The American Academy Of Child & Adolescent Psychiatry. 1994;33:809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clinical Psychology Review. 1998;18:765–794. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- McLaney M, Del Boca F, Babor T. A validation study of the Problem-Oriented Screening Instrument for Teenagers (POSIT) Journal of Mental Health. 1994;3:363–376. [Google Scholar]
- Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study. Archives of General Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus 3.1. Author; Los Angeles: 1998-2004. [Google Scholar]
- National Prevention Council . National Prevention Strategy. U.S. Department of Health and Human Services, Office of the Surgeon General; Washington, DC: 2011. [Google Scholar]
- Newcomb MD, Bentler PM. Substance use and abuse among teenagers. American Psychologist. 1989;44:242–248. doi: 10.1037//0003-066x.44.2.242. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Vargas-Carmona J, Galaif ER. Drug problems and psychological distress among a community sample of adults: Predictors, consequences, or confound? Journal of Community Psychology. 1999;27:405–429. [Google Scholar]
- Picardi A, Morosini P, Gaetano P, Pasquini M, Biondi M. Higher levels of anger and aggressiveness in major depressive disorder than in anxiety and somatoform disorders. Journal of Clinical Psychiatry. 2004;65:443–443. doi: 10.4088/jcp.v65n0322b. [DOI] [PubMed] [Google Scholar]
- Radhert E. The adolescent assessment and referral system manual. National Institute on Drug Abuse; Rockville, MD: 1991. DHHS Publication No. (ADM) 91-1735 ed. [Google Scholar]
- Radolff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Medicine. 1977;1:385–401. [Google Scholar]
- Raykov T. Analysis of Longitudinal Studies With Missing Data Using Covariance Structure Modeling With Full-Information Maximum Likelihood. Structural Equation Modeling. 2005;12:493–505. [Google Scholar]
- Rohde P, Lewinsohn PM, Kahler CW, Seeley JR, Brown RA. Natural course of alcohol use disorders from adolescence to young adulthood. Journal Of The American Academy Of Child & Adolescent Psychiatry. 2001;40:83–90. doi: 10.1097/00004583-200101000-00020. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schutte KK, Hearst J, Moos RH. Gender differences in the relations between depressive symptoms and drinking behavior among problem drinkers: A three-wave study. Journal of Consulting and Clinical Psychology. 1997;65:392–404. doi: 10.1037//0022-006x.65.3.392. [DOI] [PubMed] [Google Scholar]
- Society for Adolescent Health and Medicine Guidelines for adolescent health research: Conference proceedings. Journal of Adolescent Health. 1995;17:264. [PubMed] [Google Scholar]
- SPSS 15.0 . SPSS Base 15.0 for Windows User’s Guide. SPSS Inc.; Chicago IL: 2008. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2009 National Survey on Drug Use and Health: Summary of National Findings. U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- Swendsen JD, Merikangas KR, Canino GJ, Kessler RC, Rubio-Stipec M, Angst J. The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Comprehensive Psychiatry. 1998;39:176–184. doi: 10.1016/s0010-440x(98)90058-x. [DOI] [PubMed] [Google Scholar]
- Treuting JJ, Hinshaw SP. Depression and self-esteem in boys with attention-deficit/hyperactivity disorder: Associations with comorbid aggression and explanatory attributional mechanisms. Journal Of Abnormal Child Psychology. 2001;29:23–39. doi: 10.1023/a:1005247412221. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force Screening and Treatment for Major Depressive Disorder in Children and Adolescents: U.S. Preventive Services Task Force Recommendation Statement. Pediatrics. 2009;123:1223–28. doi: 10.1542/peds.2008-2381. [DOI] [PubMed] [Google Scholar]
- Wells KB, Tang L, Carlson GA, Asarnow J. Treatment of youth depression in primary care under usual practice conditions: Observational findings from youth partners in care. Journal Of Child And Adolescent Psychopharmacology. 2012;22:80–90. doi: 10.1089/cap.2011.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Windle R. Depressive symptoms and cigarette smoking amoung milddle adolescents: Prospective associations and intrapersonal and interpersonal influences. Journal of Consulting and Clinical Psychology. 2001;69:215–226. [PubMed] [Google Scholar]
- World Health Organization . Composite International Diagnostic Interview [CIDI]: Core Version 2.1: Interviewer’s Manual. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- Ziv A, Boulet JR, Slap GB. Utilization of physician offices by adolescents in the United States. Pediatrics. 1999;104:35–42. doi: 10.1542/peds.104.1.35. [DOI] [PubMed] [Google Scholar]
- Zuckerbrot RA, Maxon L, Pagar D, Davies M, Fisher PW, Shaffer D. Adolescent depression screening in primary care: feasibility and acceptability. Pediatrics. 2007;119:101–8. doi: 10.1542/peds.2005-2965. [DOI] [PubMed] [Google Scholar]