Abstract
Herein, we report a case of micronodular thymoma with lymphoid stroma in a previously healthy 73-year-old male. Thymectomy was performed. The solid and macrocystic masses were encapsulated with focal invasion. The solid portion consisted of nodules of bland-looking spindle or round epithelial cells in lymphoid stroma containing prominent germinal centers. The epithelial cells had moderate amount of cytoplasm and occasional mucin production. The cystic portion was lined with cuboidal epithelium. According to World Health Organization (WHO) classification, the mass was diagnosed as a micronodular thymoma with lymphoid stroma accompanied by a pre-existing multilocular thymic cyst. Micronodular thymoma with lymphoid stroma, a possible variant of type A thymoma, is an extremely rare tumor. This so-called "unusual" variant may imply the schematic weakness of the current WHO classification that cannot cover all morphologic types. Further study is recommended for clarification of this variant and its incorporation into the current classification.
Keywords: Thymoma, Thymic cyst, Lymphoid tissue, Germinal center
Micronodular thymoma with lymphoid stroma, also known as micronodular thymoma with lymphoid B-cell hyperplasia, is an extremely rare tumor. Microscopically, the tumor is characterized by numerous epithelial nodules of spindle morphology, mixed in rich lymphoid stroma with lymphoid follicles and prominent germinal centers. Therefore, the tumor was initially regarded as a variant of spindle cell thymoma, i.e., type A thymoma.1 The nodules are composed of spindle cells with bland-looking oval nuclei which are currently categorized as an unusual variant in the latest World Health Organization (WHO) classification.2
To our best knowledge, only a single case of micronodular thymoma with lymphoid stroma has been reported in Korea.3 In this study, we report an additional case along with a brief review.
CASE REPORT
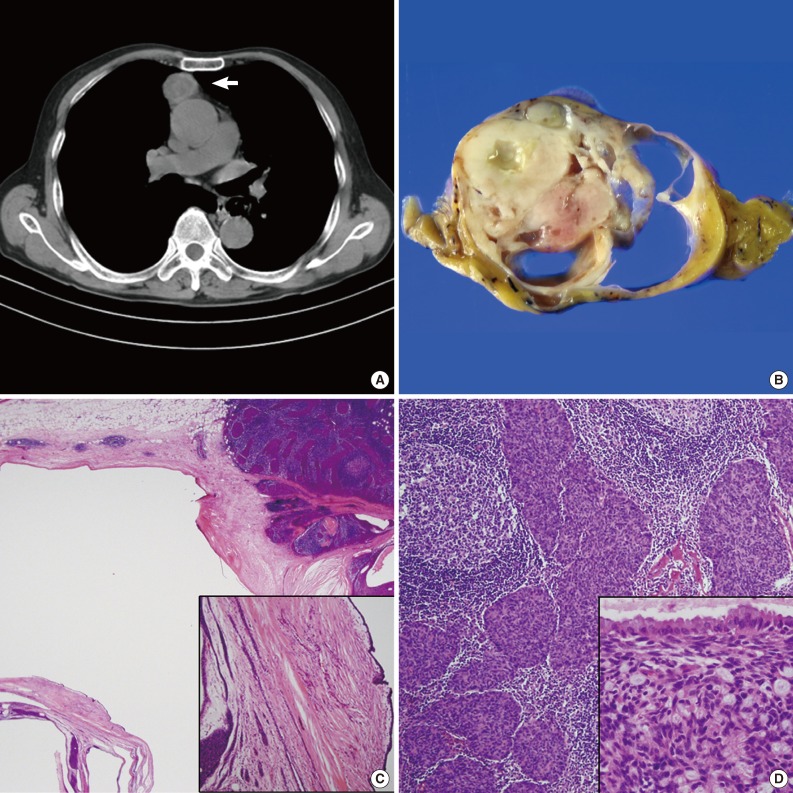
A previously healthy 73-year-old male presented with an acute onset of chest pain for one month in duration. Chest computed tomography showed a heterogeneously enhancing mass in the right anterior mediastinum approximately 5.1 cm in size, most likely representing an intermediate-grade thymic epithelial tumor (Fig. 1A). Trans-sternal extended thymectomy was performed. Upon gross examination, the external surface of the thymus was smooth and micronodular in appearance (Fig. 1B). Upon opening, the thymus was completely replaced by a yellowish brown ovoid mass that was solid and cystic in appearance, and yellowish turbid fluid was expelled from the cystic portions. The largest cyst measured 2.5×2.0×2.0 cm (Fig. 1C). Prominent macro- and microcystic changes were observed, and the cystic spaces were lined by flattened cuboidal cells (Fig. 1C, inset) with occasional mucinous epithelium (Fig. 1D, inset). Microscopically, the mass consisted of two components: a nodular epithelial component and mature lymphoid cells with prominent germinal centers (Fig. 1D). Of the nodular structures, the epithelial cells had a spindle to round appearance, with bland euchromatic nuclei and plump cytoplasm. Occasional bluish mucin was observed in the tumor. At the subepithelial area, accumulation of foamy macrophages was also observed as well as infiltrating spindle- to round-shaped epithelial cells. Some areas of the cyst wall showed extensive fibrosis. The patient was diagnosed as having a micronodular thymoma with lymphoid stroma accompanied by a pre-existing multilocular thymic cyst.
Fig. 1.
(A) Chest computed tomography shows a heterogeneously-enhancing ovoid-shaped mass (arrow) at the anterior mediastinum. (B) Gross picture of the resected thymic mass shows a homogeneously grayish tan firm cut surface with multilocular cystic changes. (C) Low power view shows a solid thymoma (right) and a macrocystic thymic cyst. Note the micronodules in the lymphoid-rich stroma. Inset shows a single layer of flattened lining cells along the multilocular cysts. (D) Multiple nodules of epithelial cells are scattered in the lymphoid-rich stroma containing prominent germinal centers. Inset shows epithelial cells having intracytoplasmic mucin and cyst-lined ciliated cuboidal epithelium with mucin.
Preoperatively, the patient showed an uneventful course for twelve months. Symptoms such as myasthenia gravis were not observed before or after removal of the mass.
DISCUSSION
The morphologic classification of thymoma has been revised and remains in much debates.1,4 According to the latest WHO classification, if the neoplastic epithelial cells and their nuclei show a bland-looking spindle or oval shape, the tumor is classified as type A thymoma, and if the cells show a round epithelioid appearance, the tumor is classified as type B thymoma. Tumors showing combined morphology of these two cell types are classified as type AB thymomas.5 Type C thymoma shows frankly malignant cytologic features like thymic carcinoma. An important feature of any morphologic classification of human neoplasia should be its ability to be easily reproduced among different observers. The new WHO classification categorized unusual morphologic variants of thymoma which do not fit into the current WHO categories as so-called "unusual" types of thymoma, which have been separated into distinctive categories in the updated edition.2 Micronodular thymoma with lymphoid stroma as in the present case, metaplastic thymoma, microscopic thymoma, sclerosing thymoma and pigmented thymoma belong to this category.1,5,6 According to the WHO classification, they present as an "unusual" type of thymoma and most are categorized as a possible type A thymoma, which take a benign clinical course, with no reported deaths.2 However, combined types or development of B-cell lymphoma have rarely been reported.7 The micronodular thymoma with lymphoid stroma, according to the WHO classification, is infrequently associated with myasthenia gravis or other paraneoplastic syndromes. Due to the relatively thin capsule and focal microinvasion to the perithymic fat, because of the limited number of reported cases, long-term follow-up is needed. Micronodular thymic carcinoma with lymphoid hyperplasia is a malignant counterpart of micronodular thymoma with lymphoid stroma, and is also categorized as unusual type of thymic carcinoma.7 The epithelial components show frankly malignant histology such as pleomorphism and increased mitotic activity. The present case was a micronodular thymoma with lymphoid stroma accompanied by a multilocular thymic cyst. Most micronodular thymomas with lymphoid stroma commonly contain cystic areas that may manifest as thymic cyst.8 This type of thymic cyst in the current case may belong to neoplastic thymic cysts, probably the acquired type.9 Contrary to congenital thymic cysts originating from sequestrated embryonal nests, acquired multilocular thymic cysts result from cystic transformation of medullary duct epithelium-derived structures as well as Hassal corpuscles by inflammation or neoplasm. Histologically, thymic tissue with or without Hassal's bodies is found within the fibrous wall of the cyst and variable lining epithelium such as epidermoid, cuboidal, or pseudostratified respiratory epithelium. Distinguishing a thymic cyst from a cystic degenerated thymoma is necessary. The perivascular cystic changes and lacking epithelial lining within the cyst wall are important pathological findings in cystic thymoma that can be differentiated from acquired thymic cyst coexisting thymoma.10
Herein, we report a case of micronodular thymoma with lymphoid stroma that is also called an "unusual" variant. Accumulation of these unusual variant cases may further expose the weakness of the WHO schema because the current classification does not encompass all morphological types. Further study is required using additional variant cases for these variant cases to be incorporated into the current classification, and not to undermine the usage of the WHO schema.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Suster S, Rosai J. Multilocular thymic cyst: an acquired reactive process. Study of 18 cases. Am J Surg Pathol. 1991;15:388–398. [PubMed] [Google Scholar]
- 2.Müller-Hermelink HK, Engel P, Harris N. Tumours of the thymus. In: Travis WD, Brambilla E, Müller-Hermelink HK, Harris CC, editors. World Health Organization classification of tumours: pathology and genetics of tumours of the lung, pleura, thymus and heart. Lyon: IARC Press; 2004. pp. 145–247. [Google Scholar]
- 3.Song HJ, Han J, Kim TS. Micronodular thymoma with lymphoid stroma: a case report. J Lung Cancer. 2011;10:56–58. [Google Scholar]
- 4.Rieker RJ, Aulmann S, Schnabel PA, et al. Cystic thymoma. Pathol Oncol Res. 2005;11:57–60. doi: 10.1007/BF03032408. [DOI] [PubMed] [Google Scholar]
- 5.Suster S, Moran CA. Problem areas and inconsistencies in the WHO classification of thymoma. Semin Diagn Pathol. 2005;22:188–197. doi: 10.1053/j.semdp.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Moran CA, Koss MN. Rhabdomyomatous thymoma. Am J Surg Pathol. 1993;17:633–636. doi: 10.1097/00000478-199306000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Weissferdt A, Moran CA. Micronodular thymic carcinoma with lymphoid hyperplasia: a clinicopathological and immunohistochemical study of five cases. Mod Pathol. 2012;25:993–999. doi: 10.1038/modpathol.2012.40. [DOI] [PubMed] [Google Scholar]
- 8.El MF, Braham E, Ayadi A, Ismail O, Kilani T. Micronodular thymoma with lymphoid stroma: report of two cases and particular association with thymic lymphoid hyperplasia in one case. Pathology. 2006;38:586–588. doi: 10.1080/00313020601027642. [DOI] [PubMed] [Google Scholar]
- 9.Nakamura S, Tateyama H, Taniguchi T, et al. Multilocular thymic cyst associated with thymoma: a clinicopathologic study of 20 cases with an emphasis on the pathogenesis of cyst formation. Am J Surg Pathol. 2012;36:1857–1864. doi: 10.1097/PAS.0b013e31826320c4. [DOI] [PubMed] [Google Scholar]
- 10.Sugio K, Ondo K, Yamaguchi M, et al. Thymoma arising in a thymic cyst. Ann Thorac Cardiovasc Surg. 2000;6:329–331. [PubMed] [Google Scholar]