Abstract
Purpose
To describe the development of an academic-health services partnership undertaken to improve use of evidence in clinical practice.
Approach
Academic health science schools and health service settings share common elements of their missions: to educate, participate in research, and excel in healthcare delivery, but differences in the business models, incentives, and approaches to problem-solving can lead to differences in priorities. Thus, academic and health service settings do not naturally align their leadership structures or work processes. We established a common commitment to accelerate the appropriate use of evidence in clinical practice and created an organizational structure to optimize opportunities for partnering that would leverage shared resources to achieve our goal.
Findings
A jointly governed and funded institute integrated existing activities from the academic and service sectors. Additional resources included clinical staff and student training and mentoring, a pilot research grant-funding program, and support to access existing data. Emergent developments include an appreciation for a wider range of investigative methodologies and cross-disciplinary teams with skills to integrate research in daily practice and improve patient outcomes.
Conclusions
By developing an integrated leadership structure and commitment to shared goals, we developed a framework for integrating academic and health service resources, leveraging additional resources, and forming a mutually beneficial partnership to improve clinical outcomes for patients.
Keywords: academic-service partnership, academic medical center, evidence-based practice (EBP), nursing research, healthcare delivery
Partnerships between academic and health service centers are increasingly valuable. Healthcare needs of the global population are changing, focusing more on quality and safety of care, the aging population, a limited health economy, and health policies that demand re-sizing the workforce. Academic service partnerships can contribute significantly to an effective response, as highlighted in recent reports on the future of nursing (Front Line Care, 2010; Institute of Medicine, 2010). The responsiveness of nurses to current changes in care delivery and health reforms demands science-based, validated innovations. Partnerships provide opportunities to leverage clinical, intellectual, and financial resources to generate new knowledge and translate that knowledge into innovative, real-world patient care practices. A defining characteristic of a learning healthcare system is the nimble use and creation of new knowledge such that existing, population data informs real-time, individual-level patient care in an ongoing, reiterative manner (Olsen, Aisner, & McGinnis, 2007). As learning healthcare systems develop internationally, partnerships provide opportunities to link patient and population data with care delivery to build innovative systems that contribute to improved patient safety, quality of care and quality of life across age groups.
Within nursing, research has long been used to drive clinical decision-making (Granger, 2001; Granger & Chulay, 1999; Titler & Everett, 2001) and improve patient outcomes. Reports by the Institute of Medicine and others emphasize the expanding role of the nurse in bringing new knowledge to patients in a more timely manner (Brown, Donaldson, Burnes Bolton, & Aydin, 2010; Committee on Quality of Health Care in America, 2001; Granger, 2008; Patrician, Loan, McCarthy, Brosch, & Davey, 2010; Reis et al., 2010). Nurses exert positive influence on timeliness by increasing the use of evidence at the point of care; integrating qualitative and quantitative analytic methods to evaluate care delivery and patient outcomes; and developing multidisciplinary teams of clinical staff and university-based faculty and students (Slutsky, 2007). These innovations require linkages at the senior leadership level and between research and patient care delivery structures and strategies (Institute of Medicince, 2003).
Despite recent support for collaboration between academia and service (Institute of Medicine, 2010), such partnerships continue to be difficult to cultivate and sustain in university-based health service settings (Nabavi, Vanaki, & Mohammadi, 2011). Although both academic and health service systems engage in education, research, and care delivery activities, they have distinct missions, target different audiences, and are based on different business models (De Geest et al., 2010). They vary in the financial incentives and rewards that shape performance and differ in the urgency and consequences that drive problem-solving. For example, faced with frequent readmission of patients with heart failure, the academic approach uses a conceptual framework to identify risk factors and develop interventions, but the health system needs to reduce monthly losses in reimbursement due to premature heart failure readmissions. Thus, the academic entities and service sectors have fundamental differences in orientation and culture. University health professional schools educate health professions students and develop knowledge through research. University-based hospitals deliver complex care to a broad array of patients from the local community as well as national and international settings. While continuing to serve as a major training site for health professions students, the university hospital embodies a fast-paced culture in which cost must be managed in light of benefit and value. Academic and service sectors prioritize care delivery, education, and research differently.
The research and scientific priorities of each sector also differ. In the university, the large federal grant funding mechanisms, i.e., the National Institutes of Health (NIH) and the Agency for Healthcare Research and Quality (AHRQ), drive research priorities. In the health service sector, the Center for Medicare and Medicaid Services (CMS) and individual consumers and private payers drive quality improvement priorities through reimbursement-based incentives and publicly reported quality metrics. In the university, accreditation boards such as the Commission on Collegiate Nursing Education (CCNE) and the National League for Nursing Accrediting Commission (NLNAC) monitor quality metrics; in the health care system, the Joint Commission serves as the accrediting body whose oversight is essential for reimbursement. Rewards for excellence also differ: the university strives to attain national ranking based on educational programs, grant acquisitions, faculty diversity, knowledge generation, and enrollment quotas; the health system strives to achieve recognition for quality through public reporting of outcomes and prestigious distinctions, e.g., the Baldrige Award and Magnet Recognition®. Deans and hospital executive or financial officers may favor different strategies to achieve those priorities and may have very different reward structures from their Boards for particular activities.
Against this backdrop, the National Institutes of Health (NIH) awarded the first 12 Clinical Translational Science Awards (CTSA) in 2005, effectively prioritizing a new mission for academic healthcare centers: to design and develop systems for speeding translation of scientific discoveries from concept to practice. CTSAs evolved from the NIH Roadmap initiative of 2000 and formed a new agenda for improving public access to new scientific knowledge about health. This agenda represented an effort to provide a return on the public investment in science through more rapid development of technologies and behavioral interventions and communicating research results that can be applied to patient care. At approximately the same time as the Roadmap initiative, the Institute of Medicine (IOM) published the first consensus report on quality and patient centeredness in care, entitled Crossing the Quality Chasm (Committee on Quality of Health Care in America, 2001). This report identified six quality-related metrics for improving care: safety, effectiveness, patient-centeredness, timeliness, efficiency and equity (Committee on Quality of Health Care in America, 2001).
With these new funds, initiatives, agendas, and metrics came new opportunities for academic and healthcare settings to integrate the best evidence from scientific research with care delivery to improve quality and effectiveness of care at the local unit (Figure 1) (Califf et al., 2007). The first challenge was to harness academic funding priorities with payor priorities for patient care to translate the best approaches to care into a clinical “living laboratory.” Such priority alignment would then bring its own challenge: implementation (Olsen, et al., 2007).
Figure 1.
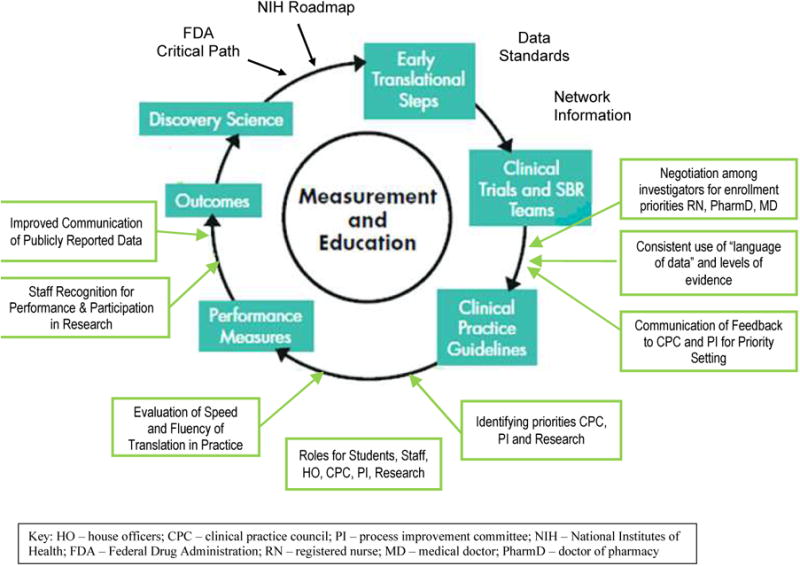
NIH Cycle of Scientific Discovery and Overlay of Clinical Application and Health Systems Role as Living Laboratory. Adapted from (Califf, et al., 2007).
Another challenge highlighted by the IOM agenda was to align the methodological approach to problem solving of academic research studies with the operational process evaluations used in the service setting. Design, analysis, and timelines all differed. Academic scientific inquiry could not be produced rapidly enough to accommodate the response times of the reimbursement-driven service setting. Producing lengthy scientific proposals every four months to obtain federal grant support for long-term project completion was not in line with operational goals that required more process and financial data, less emphasis on theory, and greater emphasis on control chart methodology (Schweikhart & Dembe, 2009). Rapid response approaches to process improvement, i.e., Plan-Do-Study-Act (PDSA) and Six Sigma (Guinane, Sikes, & Wilson, 1994; Varkey, Reller, & Resar, 2007),were often sufficient for operational questions about care delivery processes (Brown, et al., 2010; Patrician, et al., 2010). Service setting nurses – distant from the budgetary dependence of university faculty on external funding – were impatient with long academic project timelines and perceived the external funding process as a laborious waste of time, yielding impractical results available only long after the presenting clinical need. Academicians often viewed the data analyses of performance improvement to be a naïve approach to deep, underlying issues, characterized by flawed designs and failure to deal with appropriate hypothesis testing, confounding, and bias. Missing was a vision for a combined approach that improved short- and long-term patient outcomes and an analytic strategy that recognized the appropriateness of each system's respective function.
Existing literature on academic service partnerships is focused largely on partnerships between academic education and community-based clinical settings (Hunt, Bonham, & Jones, 2011; Murray, Havener, Davis, Jastremski, & Twichell, 2011). A gap remains, which describes how academic service partnerships drive innovation in healthcare delivery across all care settings, and how doing so improves both the quality of care and patient safety. More attention is needed on partnerships in complex university-based systems (De Geest, et al., 2010) as well as on the nursing role in the timely integration of research into practice (Institute of Medicine, 2010).
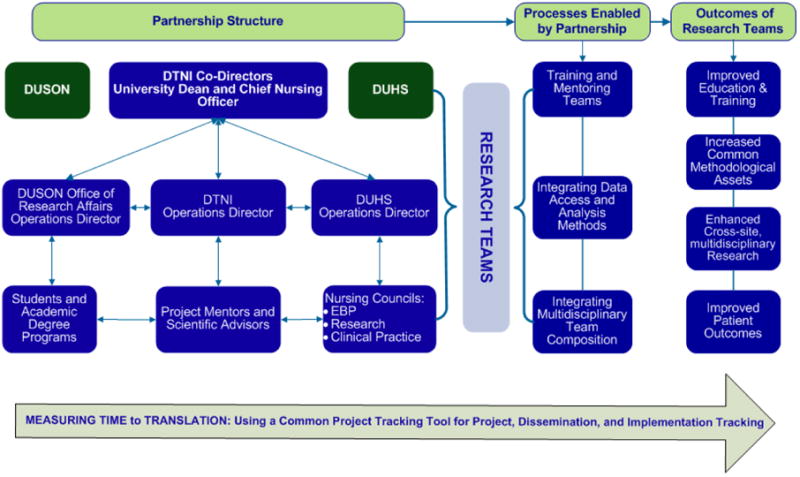
To address this gap, the Duke Translational Nursing Institute (DTNI) was established with combined funding from the Duke School of Nursing, the Duke University Health System, and an NIH-sponsored CTSA, which provided seed money for collaborative research efforts. The DTNI entails unit-based research teams, supported by a partnership structure that integrated key research and care procedures and targets defined, priority outcomes (Figure 2). Prioritization of research team projects is driven by local patient care priorities as well as national priorities for safe, quality care. The DTNI has unified the clinical, operational, and financial agendas of both academic and service settings and developed a common path for developing shared work processes, as described in detail below.
Figure 2. Structural Process and Outcomes of Academic-Health Service Partnership.
The Duke Translational Nursing Institute
Partnership Structure
DTNI directorship
An effective alignment of academic and health service goals to direct the partnership effort required a structural integration of nursing leadership from the university and the health system. The DTNI is co-directed by the Dean of the School of Nursing and the Chief Nursing and Patient Care Services Officer for the health system. Initially, the co-directors conducted a joint assessment of resources and personnel that might contribute time and expertise to the partnership, convening experts from existing research operations teams and hospital and academic councils and seeking both clinicians and faculty who were clinically engaged and committed to translational research in clinical practices of professional nurses, students of nursing, and multidisciplinary research teams.
Duke University School of Nursing's Office of Research Affairs
The Duke University School of Nursing (DUSON) Office of Research Affairs (ORA), led by a faculty member who serves as the Dean for Research Affairs and a staff-level Operations Director, supports DTNI research-related data management, data entry and cleaning, data transcription, and external grant submissions. The ORA is accountable to the Duke Medicine institutional review board and the university's Office of Grants and Contracts for compliance of all regulatory affairs involving staff, student and faculty research and for nursing quality improvement projects. The ORA also collaborates with the DTNI to oversee nursing students and advise staff nurses working on ongoing health system-based research teams.
Academic degree programs and students
Students at Duke, including nursing, medicine, physical therapy, divinity, participate in research teams to fulfill degree requirements. Students benefit from an enriched experience of collaborative research. Clinical sites experience some increased demands from student involvement, offset by support from the DTNI, faculty, and attention to real-world clinical issues.
DTNI research operations
The time dedicated by each participant to education, skills training, professional development, dissemination support, or design of research and quality improvement projects is negotiated with the setting of primary appointment, be it health system or university. Role responsibilities are designed to leverage both academic and clinical resources to facilitate student and staff development of the skills required to identify clinical research priorities and select a feasible study design for approaching these priorities. These skills include identifying existing evidence about patient care problems, identifying valid and reliable measures, and carrying out the study procedures in a clinically feasible way (Granger, 2008). Key mentors and support staff assist with these responsibilities.
Research practice management and regulatory mentor
The DTNI is staffed with an advanced practice nurse who specializes in regulatory and ethics oversight and has expertise in the regulatory process across all types of study designs. In addition, this role presupposes a working knowledge of the requirements and constraints of both funded and unfunded work, research and quality improvement programs, and facilitating applications for funding through private sponsorship, small grants programs, and local philanthropic grant mechanisms.
Design, analysis and data management mentor
One or more statisticians is available to support the research and quality improvement projects, depending on resources and programmatic volume. The statistician works with each team to ensure clear, measurable variables and a study design appropriate to the research question(s) and unit routines
Administrative support specialist
The administrative support specialist arranges team and mentor appointments, orders study supplies, compiles study packet materials, collects study materials from clinical units, trains study teams to budget, monitors budgets and budget reporting for study teams, manages room reservations and information technology (IT) capacity for internal dissemination, and uploads manuscripts for external dissemination.
Project mentors and scientific advisors
Project mentors are dually-appointed senior nurse scientists and advanced practice nurses who mentor unit-based research teams in the conduct of point of care research and quality improvement projects. They have varying amounts of salary support from the university and health service setting. Project mentors may be disease- or patient population-focused or have expertise on issues, such as preventing patient falls, decreasing nosocomial infection, or evaluating health system-wide rapid response teams.
Duke University Health System research operations and clinical councils
The health system arm of the research operations is led by a nurse scientist and supported by both centralized and specialty-based nursing councils.
Evidence-Based Practice (EBP) Council
The Evidence Based Practice Council is comprised of nurse scientists, staff from across health system sites, and research mentors from both the academic and service settings. EBP Council members evaluate existing research and make recommendations to staff nurses via the Clinical Practice Councils regarding the availability and quality of existing evidence, preparation of clinical practice guidelines and policy changes; and further research
Research Council
The Research Council includes representatives from each clinical area. It generates ideas for new research, disseminates research results, creates infrastructure to support bedside level research, and frames the implications of new science for patient care.
Clinical Practice Council (CPC)
The Clinical Practice Councils include staff nurses from each clinical division or service line and evaluate and disseminate research and quality improvement findings for patient populations, such as oncology, critical care, cardiovascular, or pediatrics. They review existing and new evidence for consideration and integration into health system patient care policies and procedures.
Research Teams
Research team members and the details of their respective roles and responsibilities have been described previously (Granger, 2001, 2008; Granger & Chulay, 1999). To summarize, teams of 5-15 clinical staff members develop and conduct a specific research project. Nursing students, house officers, or other learners may briefly affiliate with the team. The structure of the team is flexible, and responsibilities are carefully distributed among members and across shifts in order to complete the translation effectively and efficiently.
Processes Enabled by Partnership
A series of retreats and monthly group meetings focused on collaboration for training and mentoring research teams; improving methodological approaches for data collection, warehousing, access and use of data; and integrating multidisciplinary students and staff into research teams. The co-directors also convened monthly steering committee meetings to reassess clinical research priorities, evaluate the productivity of the research teams, review internal and external dissemination of project findings, and address resource allocation issues.
Training and mentoring teams for students and staff
We integrated didactic training, both academic coursework and continuing education (CE)-approved modules for staff, into the real-world point of care research. Previous work on student participation in health system-based research teams had not explicitly linked student coursework to clinical problems identified by health system members (Granger, 2008; Schwartz-Barcott, Patterson, Lusardi, & Farmer, 2002). The research course faculty member and the health system nurse scientist insured that teams included a local hospital-based expert with access to clinical data forms and data collection processes, clinical information and insight into relevant unit-specific practice patterns.
We also changed the mentoring process by matching students requiring clinical research experience with teams of nurses engaged in point of care research or quality improvement projects. Student coursework required a “deliverable” that remained for use in the clinical areas, such as short DVD recordings of how to obtain informed consent and enroll a patient in a study (Bowers, 2010), or that summarized existing evidence for a specific clinical research project (DukeTranslationalNursingInstitute, 2011). This material was used subsequently in Institutional Review Board applications and for manuscript preparation by research teams.
Integrating data access and analysis methods
A second set of process changes enabled by the partnership was the integration of data management methods across quality improvement evaluation and health science research. These process changes were accomplished in two ways. First, the health system leadership and staff nurses identified quality improvement priorities. Research teams were encouraged to address these priority clinical problems, and faculty whose research expertise was aligned with the patient population or clinical problem were paired with these teams for consultation, to facilitate development of the design, measures, and analysis for the project.
Another process change focused on integration of system support for electronic medical record access. Patient data was collected for use in real-time, to be research-ready at the point of data entry (e.g., electronically entered and coded at the point of data entry in the clinical area) to inform and support care. Real-time access to both individual-level and population-level data and the ability to compare clinical guidelines with real-time patient-reported symptoms, prove more effective and efficient (Abernethy et al., 2010; Abernethy, Wheeler, & Bull, 2011).
Integrating multi-disciplinary team composition
A third focus on process – increasing multidisciplinary involvement on research teams at the unit-level – was not a new idea: patient outcomes are known to be improved when disciplines work together to establish plans of care, particularly in chronic illness (Hobgood et al., 2010; Sochalski et al., 2009). However, because evidence also shows that multidisciplinary learning and problem-solving are difficult to develop, DTNI engaged the Institute for Healthcare Improvement (IHI), whose initiatives to increase successful multidisciplinary efforts have gained widespread attention (Berwick, 2003; Leape et al., 2009). DTNI partners worked together with the local student chapter of the IHI, and IHI partners participated in quarterly meetings with nursing students, faculty and research scientists on specific unit-based projects to integrate medical students and house staff, pharmacists, dieticians, clergy, physical therapists, and others into teams.
The Outcomes of the Research Teams
The DTNI partnership between academia and health service has resulted in an integrated structure that supports improved work processes and outcomes for education and research. Most importantly, partnering has improved patient outcomes directly and indirectly by decreasing the time for new knowledge to infiltrate direct patient care delivery systems and practices.
Improved education and training
Results of integrating formal training and mentoring of research teams across university and health service settings have been broad. Dissemination of the outcomes have increased shared educational forums in both DUSON and the health system. The partnership has co-sponsored nursing grand rounds; educational webinars on research priorities; “Research Day” seminars; and other formal and informal project presentations. The co-directorship of the DTNI has lent credibility to its training and mentoring work across settings.
Increased shared methodological approaches and assets
Integration of research methodologies has lowered the boundaries between the university focus on development of new knowledge and the health system focus on process monitoring and rapid generation of publicly reported quality metrics. We have developed tools such as the common project database, a warehouse of commonly used, well-validated questionnaires and patient-reported outcomes measures, and lists of contacts and collaborative investigators across settings. List-serves and social networks help to keep staff and students integrated by sustaining common research goals incorporating suggestions for coursework modifications, matching didactic and clinical preceptorships, producing student and staff workshops on data abstraction in the clinical setting, and distributing research enrollment reports to clinicians via web and electronic mail.
Enhanced cross-disciplinary cross-site research
The partnership has enabled multidisciplinary research teams to follow patient transitions from in-patient units to outpatient settings, the community, and the patient home. Nurse investigators are no longer isolated in or limited to the acute care setting in which they work but are partnered with nurse practitioners and students in the ambulatory clinic setting and home health and with public health nurses and certified community health workers who collaborate with the DTNI research teams. Current research teams that study care transitions for patients with heart failure, diabetes, and hypertension, for example, are therefore able to transparently cross settings of care delivery to interact with patients in locations that are more convenient, familiar and comfortable for them. Tailoring these research interactions to patients leads to better study follow up, patient satisfaction, data collection, and more reliable and valid findings. Furthermore, cross-discipline, cross-site studies have tended to be of a broader scope and amenable to wider implementation.
Improved clinical outcomes for patients
Successful collaboration and a culture of flexible problem-solving served to translate new scientific evidence more rapidly into the patient care arena. For example, our neuro-intensive care unit nurse researchers were funded by a small grant from the DTNI to study the effect of nursing care interventions such as bathing on variations in the intracranial pressure of patients with ICP monitors (Kim et al., 2011). The study began and was completed, published and evaluated by the Clinical Practice Council in less than nine months. To promote these early successes and to encourage other teams, DNTI has presents a “Time to Translation Award” and other recognitions for moving evidence rapidly into direct patient care delivery.
To date, DNTI point of care studies have improved care processes for patient and family decision making at the end of life care (Johnson et al., 2010), improved patient safety and use of prevention strategies for patients undergoing alcohol withdrawal in the setting of acute myocardial infarction (Fullwood et al., 2011), and improved the reliability of blood glucose testing and subsequent safety of intravenous insulin dosing after cardiothoracic surgery (Ellis et al., 2011). In each case, new scientific discoveries reached patients in the form of an evidence-based practice review, a new practice recommendation, or through partnered mentoring of clinicians to read new science more effectively. Additional studies in progress will evaluate the effectiveness of care transitions for patients with heart failure from acute care to home, the safety of transitions to home for patients with destination left ventricular assist devices, and the value to patients and families of connecting acute care and clinic visits with in-home follow up.
Challenges
Our experience in establishing substantive changes in organizational processes to support the academic service partnership has been challenging. Though participants explicitly endorsed common values, including the values of mutual respect, inclusion, transparency, attention to shared goals, and clear lines of communication, barriers such as time constraints and scheduling challenges persist. Role expectations and reimbursement processes for staff nurses on research and process improvement teams also differ among nurse leaders. Other challenges include maintaining consensus on new priorities as they arise and negotiating competing roles within the collaboration. For example, academic priorities increasingly focus on improving care transitions (Naylor, Kurtzman, & Pauly, 2009), yet service settings are not always contiguous business units, able to cross physical boundaries with operational priorities (Kripalani, Jackson, Schnipper, & Coleman, 2007). Likewise, service priorities focus on efficiencies in care (e.g. shorter lengths of stay) that may constrain academic efforts to improve patients' self-care abilities related to transitions (Dilles et al., 2011). Such conflicts are usually resolved through teamwork and communication, but these efforts take time, trust and mutual commitment (Brush, Baiardi, & Lapides, 2011), which is difficult to sustain.
Conclusions
Academic and service settings can more effectively address patients' most pressing quality and safety concerns by joining forces. Through integrated partnerships, healthcare providers are better equipped to develop, implement, and evaluate data-based solutions to patient care delivery problems across settings of care.
Clinical relevance.
Structurally integrated academic-health service partnerships result in improved evidence-based patient care delivery and in a stronger foundation for generating new clinical knowledge, thus improving patient outcomes.
Acknowledgments
This paper is partially supported by a grant from the National Center for Research Resources (UL1RR024128). The authors would like to acknowledge the editorial contribution of Judith Hays.
References
- Abernethy AP, Ahmad A, Zafar SY, Wheeler JL, Reese JB, Lyerly HK. Electronic Patient-Reported Data Capture as a Foundation of Rapid Learning Cancer Care. [Proceedings Paper] Medical Care. 2010;48(6):S32–S38. doi: 10.1097/MLR.0b013e3181db53a4. [DOI] [PubMed] [Google Scholar]
- Abernethy AP, Wheeler JL, Bull J. Development of a health information technology-based data system in community-based hospice and palliative care. Am J Prev Med. 2011;40(5 Suppl 2):S217–224. doi: 10.1016/j.amepre.2011.01.012. doi:S0749-3797(11)00093-6 [pii] 10.1016/j.amepre.2011.01.012. [DOI] [PubMed] [Google Scholar]
- Berwick DM. Improvement, trust, and the healthcare workforce. Qual Saf Health Care. 2003;12(1):i2–6. doi: 10.1136/qhc.12.suppl_1.i2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers MCL, McBroom K. Lost in Translation: Engaging Nurses in Research at the Point of Care. Heart & Lung. 2010;39(4):373. [Google Scholar]
- Brown DS, Donaldson N, Burnes Bolton L, Aydin CE. Nursing-sensitive benchmarks for hospitals to gauge high-reliability performance. J Healthc Qual. 2010;32(6):9–17. doi: 10.1111/j.1945-1474.2010.00083.x. [DOI] [PubMed] [Google Scholar]
- Brush BL, Baiardi JM, Lapides S. Moving toward synergy: lessons learned in developing and sustaining community-academic partnerships. Prog Community Health Partnersh. 2011;5(1):27–34. doi: 10.1353/cpr.2011.0003. doi:S1557055X11100054 [pii] 10.1353/cpr.2011.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Califf RM, Harrington RA, Madre LK, Peterson ED, Roth D, Schulman KA. Curbing the cardiovascular disease epidemic: aligning industry, government, payers, and academics. Health Aff (Millwood) 2007;26(1):62–74. doi: 10.1377/hlthaff.26.1.62. doi:26/1/62 [pii] 10.1377/hlthaff.26.1.62. [DOI] [PubMed] [Google Scholar]
- Committee on Quality of Health Care in America, I. o. M. Crossing the Quality Chasm: A New Health System for the 21st Century Quality Chasm Series: Health Care Quality Reports from the Institute of Medicine Retrieved from WorldCat database. 2001 Retrieved from http://www.nap.edu/catalog/10027.html.
- De Geest S, Sullivan Marx EM, Rich V, Spichiger E, Schwendimann R, Spirig R, Van Malderen G. Developing a financial framework for academic service partnerships: models of the United States and Europe. J Nurs Scholarsh. 2010;42(3):295–304. doi: 10.1111/j.1547-5069.2010.01355.x. doi:JNU1355 [pii] 10.1111/j.1547-5069.2010.01355.x. [DOI] [PubMed] [Google Scholar]
- Dilles A, Heymans V, Martin S, Droogne W, Denhaerynck K, De Geest S. Comparison of a computer assisted learning program to standard education tools in hospitalized heart failure patients. Eur J Cardiovasc Nurs. 2011;10(3):187–193. doi: 10.1016/j.ejcnurse.2010.07.001. doi:S1474-5151(10)00082-4 [pii] 10.1016/j.ejcnurse.2010.07.001. [DOI] [PubMed] [Google Scholar]
- DukeTranslationalNursingInstitute. 2011 Jul 15;2011 Retrieved July 25, 2011, from https://www.dtmi.duke.edu/about-us/organization/duke-translational-nursing-institute. [Google Scholar]
- Ellis M, Benjamin K, Cornell M, Decker K, Farrell D, McGugan L, Granger B. Assessing the SUitability of Capillary Blood Glucose Analysis in Patients Receiving Vasopressors (SUGAR) American journal of critical care: an official publication, American Association of Critical-Care Nurses, in review 2011 [Google Scholar]
- Front Line Care. Report by the Prime Minister's Commission of the Future of Nursing and Midwifery in England. 2010 Retrieved August 2, 2010, from http://cnm.independent.gov.uk.
- Fullwood J, Mostaghimi Z, Granger C, Bride W, Washam JB, Granger B. A Randomized Trial of Strategies to Prevent Withdrawal from Alcohol Following Acute Myocardial Infarction. American journal of critical care: an official publication, American Association of Critical-Care Nurses(in review) 2011 doi: 10.4037/ajcc2013283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granger BB. Research strategies for clinicians. Crit Care Nurs Clin North Am. 2001;13(4):605–615. [PubMed] [Google Scholar]
- Granger BB. Practical steps for evidence-based practice: putting one foot in front of the other. AACN Adv Crit Care. 2008;19(3):314–324. doi: 10.1097/01.AACN.0000330383.87507.d1. 10.1097/01.AACN.0000330383.87507.d1 doi;01256961-200807000-00011 pii. [DOI] [PubMed] [Google Scholar]
- Granger BB, Chulay M. Research Strategies for Clinicians. Prentice Hall; Publishers: 1999. [Google Scholar]
- Guinane CS, Sikes JI, Wilson RK. Using the PDSA cycle to standardize a quality assurance program in a quality improvement-driven environment. Jt Comm J Qual Improv. 1994;20(12):696–705. doi: 10.1016/s1070-3241(16)30118-3. [DOI] [PubMed] [Google Scholar]
- Hobgood C, Sherwood G, Frush K, Hollar D, Maynard L, Foster B, Taekman J. Teamwork training with nursing and medical students: does the method matter? Results of an interinstitutional, interdisciplinary collaboration. Qual Saf Health Care. 2010;19(6):e25. doi: 10.1136/qshc.2008.031732. doi:qshc.2008.031732 [pii] 10.1136/qshc.2008.031732. [DOI] [PubMed] [Google Scholar]
- Hunt JB, Bonham C, Jones L. Understanding the goals of service learning and community-based medical education: a systematic review. Acad Med. 2011;86(2):246–251. doi: 10.1097/ACM.0b013e3182046481. [DOI] [PubMed] [Google Scholar]
- Future of the Public's Health in the 21st Century. Washington DC: 2003. Institute of Medicince. [Google Scholar]
- The Future of Nursing: Leading Change, Advancing Health. 2010. Institute of Medicine. [Google Scholar]
- Johnson RW, Newby LK, Granger CB, Cook WA, Peterson ED, Echols M, Granger BB. Differences in level of care at the end of life according to race. Am J Crit Care. 2010;19(4):335–343. doi: 10.4037/ajcc2010161. quiz 344. doi:19/4/335 [pii] 10.4037/ajcc2010161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim GS, Amato A, James ML, Britz GW, Zomorodi A, Graffagnino C, Olson DM. Continuous and intermittent CSF diversion after subarachnoid hemorrhage: a pilot study. Neurocrit Care. 2011;14(1):68–72. doi: 10.1007/s12028-010-9401-y. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323. doi: 10.1002/jhm.228. 10.1002/jhm.228 doi. [DOI] [PubMed] [Google Scholar]
- Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, Isaac T. Transforming healthcare: a safety imperative. Qual Saf Health Care. 2009;18(6):424–428. doi: 10.1136/qshc.2009.036954. doi:18/6/424 [pii] 10.1136/qshc.2009.036954. [DOI] [PubMed] [Google Scholar]
- Murray MF, Havener JM, Davis PS, Jastremski C, Twichell ML. The rural pipeline: building a strong nursing workforce through academic and service partnerships. Nurs Clin North Am. 2011;46(1):107–121. doi: 10.1016/j.cnur.2010.10.010. doi:S0029-6465(10)00103-9 [pii] 10.1016/j.cnur.2010.10.010. [DOI] [PubMed] [Google Scholar]
- Nabavi FH, Vanaki Z, Mohammadi E. Systematic Review: Process of Forming Academic Service Partnerships to Reform Clinical Education. West J Nurs Res. 2011 doi: 10.1177/0193945910394380. doi:0193945910394380 [pii] 10.1177/0193945910394380. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Kurtzman ET, Pauly MV. Transitions of elders between long-term care and hospitals. Policy Polit Nurs Pract. 2009;10(3):187–194. doi: 10.1177/1527154409355710. 1527154409355710 pii;10.1177/1527154409355710 doi. [DOI] [PubMed] [Google Scholar]
- Olsen L, Aisner D, McGinnis JM. The learning healthcare system: workshop summary Retrieved from WorldCat database. 2007 Retrieved from http://www.loc.gov/catdir/toc/ecip0715/2007015074.html Materials specified: Table of contents only http://www.loc.gov/catdir/toc/ecip0715/2007015074.htmlhttp://www.nap.edu/catalog/11903.html. [PubMed]
- Patrician PA, Loan L, McCarthy M, Brosch LR, Davey KS. Towards evidence-based management: creating an informative database of nursing-sensitive indicators. J Nurs Scholarsh. 2010;42(4):358–366. doi: 10.1111/j.1547-5069.2010.01364.x. [DOI] [PubMed] [Google Scholar]
- Reis SE, Berglund L, Bernard GR, Califf RM, Fitzgerald GA, Johnson PC. Reengineering the national clinical and translational research enterprise: the strategic plan of the National Clinical and Translational Science Awards Consortium. Acad Med. 2010;85(3):463–469. doi: 10.1097/ACM.0b013e3181ccc877. 10.1097/ACM.0b013e3181ccc877 doi;00001888-201003000-00020 pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz-Barcott D, Patterson BJ, Lusardi P, Farmer BC. From practice to theory: tightening the link via three fieldwork strategies. J Adv Nurs. 2002;39(3):281–289. doi: 10.1046/j.1365-2648.2000.02275.x. doi:2275 [pii] [DOI] [PubMed] [Google Scholar]
- Schweikhart SA, Dembe AE. The Applicability of Lean and Six Sigma Techniques to Clinical and Translational Research. Journal of Investigative Medicine. 2009;57(7):748–755. doi: 10.231/JIM.0b013e3181b91b3a. Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutsky JR. Moving closer to a rapid-learning health care system. Health Aff (Millwood) 2007;26(2):w122–124. doi: 10.1377/hlthaff.26.2.w122. doi:hlthaff.26.2.w122 [pii] 10.1377/hlthaff.26.2.w122. [DOI] [PubMed] [Google Scholar]
- Sochalski J, Jaarsma T, Krumholz HM, Laramee A, McMurray JJ, Naylor MD, … Stewart S. What works in chronic care management: the case of heart failure. Health Aff(Millwood) 2009;28(1):179–189. doi: 10.1377/hlthaff.28.1.179. 28/1/179 pii;10.1377/hlthaff.28.1.179 doi. [DOI] [PubMed] [Google Scholar]
- Titler MG, Everett LQ. Translating research into practice. Considerations for critical care investigators. Crit Care Nurs Clin North Am. 2001;13(4):587–604. [PubMed] [Google Scholar]
- Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc. 2007;82(6):735–739. doi: 10.4065/82.6.735. [DOI] [PubMed] [Google Scholar]


