Abstract
Background
Despite widespread use of 12-step treatment approaches and referrals to Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) by youth providers, little is known about the significance of these organizations in youth addiction recovery. Furthermore, existing evidence is based mostly on short-term follow-up and is limited methodologically.
Methods
Adolescent inpatients (N = 160; M age = 16, 40% female) were followed at 6-months, and at 1, 2, 4, 6, and 8 years post-treatment. Time-lagged, generalized estimating equations (GEE) modeled treatment outcome in relation to AA/NA attendance controlling for static and time-varying covariates. Robust regression (LOWESS) explored dose-response thresholds of AA/NA attendance on outcome.
Results
AA/NA attendance was common and intensive early post-treatment, but declined sharply and steadily over the 8-year period. Patients with greater addiction severity and those who believed they could not use substances in moderation were more likely to attend. Despite declining attendance, the effects related to AA/NA remained significant and consistent. Greater early participation was associated with better long-term outcomes.
Conclusions
Even though many youth discontinue AA/NA over time, attendees appear to benefit, and more severely substance-involved youth attend most. Successful early post-treatment engagement of youth in abstinence-supportive social contexts, such as AA/NA, may have long-term implications for alcohol and drug involvement into young adulthood.
Keywords: Mutual-help Groups, Self-help, Alcoholics Anonymous, Narcotics Anonymous, Adolescents
Despite limited experimental evidence in support of Alcoholics Anonymous (AA) as a “stand alone” intervention (e.g., Ferri, Amato et al, 2006), a large body of quasi-experimental and correlational research indicates that post-treatment attendance at mutual-help groups, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), is consistently associated with improved substance use outcomes for a wide variety of alcohol dependent patients and may help reduce health care costs (Bond et al., 2003; Gossop et al, 2007; Humphreys, 2004; Humphreys and Moos, 2001; 2007; Kaskutas et al., 2002; Kelly, 2003; Kelly et al., 2006; Kissin et al., 2003; Magura et al., 2005; McKay, 2001; Tonigan et al., 2002; Weiss et al., 2005). Consequently, newer, state of the art interventions, such as those tested in the COMBINE Study, incorporate standard referral to such groups (Longabaugh et al., 2005; Pettinati et al., 2005) and prominent addiction and mental health focused organizations advocate use of these resources in practice guidelines(e.g., American Psychiatric Association, 2006; Institute of Medicine, 1998; National Insititue of Drug Abuse, 2000; Veterans Health Administration, 2001).
While clinical confidence in the utility of these resources has increased for adults, comparatively little is known about how helpful these organizations are as continuing care resources for adolescents, despite widespread use of 12-step treatment approaches and referrals to AA/NA groups by youth treatment providers (Brown, 2004; Drug Strategies, 2003; Kelly et al., in press b).
Available adolescent-specific evidence is limited in quantity and in methodological rigor (Kelly and Myers, 2007), but suggests that youth who participate in 12-step fellowships have better treatment outcomes, at least in the short-term (Brown, Mott and Myers, 1990; Alford et al., 1991; Kennedy and Minami, 1993; Hsieh et al., 1998; Kelly et al., 2000; Kelly et al, 2002). However, despite this body of research, there remain a number of key questions that have not been fully answered regarding the role of AA/NA in youth recovery following treatment. For example, we still know very little about the proportions of treated youth that actually utilize AA/NA, and which youth, in particular, are more or less likely to attend. Similarly, little is known regarding the extent to which adolescents benefit from AA/NA over the longer-term and whether some minimum threshold of attendance is needed before benefits may be realized.
Predictors of AA/NA attendance
Of clinical significance is the question of which adolescents may be more or less likely to attend AA/NA, as more information in this regard could help tailor interventions accordingly. Prior research has examined predictors of adolescent attendance at (Hohman and LeCroy, 1996; Kelly et al., 2000), and active involvement in (Kelly et al., 2002), AA and NA. As with adults (e.g., Emrick et al., 1993; Kelly et al., 2000; Kissin et al., 2003; McKay et al., 1998; Weiss et al., 2000), indices related to addiction severity (e.g., alcohol-related consequences, dependence symptoms) appear to be consistent predictors of initial participation, with more severely substance-involved persons being more likely to participate (Hohmann and LeCroy, 1996; Kelly et al., 2000). These types of predictor constructs appear to fit well within the Health Beliefs Model (HBM) of behavior change (Conner and Norman, 1996; Rosenstock, 1974), especially the central tenet of “perceived severity” (Finney and Moos, 1995). From a social-cognitive learning theory framework (Bandura, 1986) additional psychological variables that pertain to patients’ self-appraisal of the extent to which they believe they can consume alcohol or other drugs in moderation, and are confident that they can successfully abstain (abstinence self-efficacy) may also be important to examine since they directly relate to the central abstinence focus of AA/NA. Common co-occurring behavioral problems (e.g., conduct disorder), and demographic variables, such as age, ethnicity, and gender may also be important to examine. Women, in particular, have been underrepresented in studies of AA (Emrick et al., 1993), but appear to attend meetings at least as frequently as men and report higher involvement than men (Del Boca and Mattson, 2001; Timko et al., 2005; Weisner, Greenfield and Room, 1995). The extent to which this may be true of adolescent girls/young women is unknown.
Religious involvement may be an important consideration since 12-step fellowships, while purportedly “spiritual” rather than “religious” in nature, contain a great deal of seemingly religious reference and connotation, which may be a barrier for some (Alcoholics Anonymous, 2001). Although non-religious adult attendees appear to benefit as much as the more religious, there is evidence that less religious involvement is associated with less attendance (Winzelberg and Humphreys, 1999; Kelly et al., 2006). Thus, the spiritual emphasis may be a barrier for less religiously inclined youth, but has not been examined (Kelly and Myers, 2007).
The Influence of Early Post-treatment 12-step Involvement
A critical juncture occurs when patients treated in residential settings are discharged back to their respective communities. This early post-residential phase (i.e., the first six months) often requires demanding adjustments and remains the highest risk period in terms of alcohol and drug relapse for both adults and youth (Brown, 1993; Brown et al., 1989; Godley et al., 2002; Hunt et al., 1971; Vik et al., 1992). Consequently, most programs focus on engaging patients with formal (e.g., outpatient counseling) and informal (e.g., AA/NA) continuing care resources during these early months (Godley et al., 2002). Findings from adult studies suggest also that patients who achieve immediate, rather than delayed, AA/NA attendance may experience significantly better long-term outcomes (Moos and Moos, 2004). Given the pervasive use of the 12-step treatment modality in addressing youth alcohol and other drug problems and increased pressure for evidence-based practice (Institute of Medicine, 1998), further research is needed to assess the extent to which treated adolescents meet this key proximal outcome goal and whether such utilization is associated with better long-term outcomes. Such research could have important implications for 12-step theory and efforts to facilitate AA/NA participation (Finney, 1995; Suchman, 1967).
Long-term Recovery in Relation to AA/NA attendance
Existing research with adolescents consistently reveals beneficial associations between AA/NA attendance and substance use outcomes up through one year post-treatment, and in one study up through two years post-treatment (Brown, Mott and Myers, 1990; Alford et al., 1991; Kennedy and Minami, 1993; Hsieh et al., 1998; Kelly et al., 2000; Kelly et al, 2002). However, despite the treatment emphasis on long-term, even life-long, AA/NA mutual-help participation (Kelly and Yeterian, in press), we are not aware of any studies that have examined youth AA/NA attendance and any associated benefits over an extended follow-up as youth transition into young adulthood.
Furthermore, although a number of studies have shown associations between AA/NA attendance and outcomes in adolescents, the conclusions that can be drawn remain tenuous due to some key methodological limitations. First, in most youth studies, AA/NA attendance and substance use outcomes are examined concurrently. Second, in many studies, the potential influence of relevant confounds related to better prognosis, such as baseline measures of substance involvement, have not been taken into consideration. Third, when examining AA/NA attendance in predicting subsequent outcomes, most existing youth studies have not taken into account other important factors that may vary over time and influence outcomes, such as use of professional treatments and levels of substance use during preceding follow-up periods. These shortcomings in existing youth studies obfuscate the connection between AA/NA attendance and outcome (Kazdin and Nock, 2003). Thus, a main aim of the current study is to examine adolescent treatment outcome in relation to AA/NA attendance over an extended, 8-year follow-up period using rigorous longitudinal statistical modeling while controlling for potential static and time-varying confounds.
How Often Should Youth Be Advised to Attend AA/NA Groups? Dose-Response Thresholds
Prior studies support the notion that, in general, more frequent AA or NA attendance is associated with better outcomes (i.e., there is a linear relationship). However, little is known about optimal levels of participation or whether some minimum “dose” of participation may be required before benefits are realized. Greater knowledge would help inform clinical recommendations regarding participation levels.
The present study has several aims. First, we describe the rates of AA/NA attendance over eight years following inpatient treatment and examine predictors of attendance. We hypothesize that youth with greater levels of alcohol/drug involvement and who believe they cannot use alcohol/drugs in a moderate fashion will be more likely to attend these abstinence-oriented organizations. We also predict more religiously-involved youth will be more likely to attend, and that girls/young women will be at least as likely to attend as boys/young men. Second, we conduct a rigorous evaluation of the extent to which post-treatment outcome is related to both early, and ongoing, AA/NA attendance by testing lagged, generalized estimation equations (GEE), in which we control for static baseline predictors (e.g. pretreatment use), as well as time-varying predictors of outcome (e.g., days abstinent in preceding follow-ups; ongoing professional treatment). Finally, using a robust, locally weighted, regression approach (LOWESS), we explore thresholds and optimal levels of AA/NA attendance in relation to outcome.
Methods
Participants
Participants (N = 166) were consecutive admissions to two privately-funded, adolescent inpatient substance use disorder (SUD) treatment centers in the metropolitan San Diego, California region and were recruited for a longitudinal investigation of alcohol and drug problems during adolescence. These centers were abstinence-focused and based on a 12-step treatment model. The average length of stay was 4 weeks (range 4-6 weeks). Adolescents who met DSM-III-R (APA, 1987) lifetime criteria for an alcohol use disorder or other drug use disorder were recruited. Adolescents who had history of significant head trauma, lived more than 50 miles from research facility, or did not have a parent or resource person willing to provide corroborating information were excluded. Adolescents displaying evidence of a DSM-III-R Axis I psychiatric disorder, other than conduct disorder, predating the onset of alcohol or drug problems were also excluded.
From the initial sample of 166 adolescents who entered the study, 160 (96.4%) completed the 6-month follow-up assessment, 159 (95.8%) the 1-year follow-up, 150 (90.4%) the 2-year follow-up, 159 (95.8%) completed the 4-year follow-up, 153 (92.2%) the 6-year follow-up, and 139 (83.7%) the 8-year follow-up. At treatment entry the average age of the sample was about 16 years old (M = 15.9, SD = 1.27) and 40% were female. The sample consisted of ethnically diverse adolescents: Caucasian (75%), Hispanic (5%), African-American (5%), and other (15%). Socio-economic status (SES; Hollingshead, 1975) at intake was based on parental income, education, and type of employment (M Hollingshead Index = 29.8 ± 12.3). At treatment entry, nearly half (47%) of the current sample had received prior alcohol/drug-related outpatient treatment (M sessions = 16.2, SD = 20.1; median = 10.0; range 1-98). However, for the vast majority (92%), this was their first inpatient treatment experience. Although alcohol was the most commonly used drug, the reported “drug of choice” was amphetamines (53%), followed by cannabis (32%), hallucinogens (7%), alcohol (4%), cocaine (3%), and opiates (<1%). Approximately three-quarters (73.8%) of the sample was enrolled in public or private school; 19.2% reported quitting school, and 6.2% were expelled or suspended. Neither demographic nor baseline treatment/clinical variables were associated with participant follow-up (ps > .27).
Procedure
Informed consent from the parent or legal guardian and separate assent from youth were obtained for participation. The consent procedure was approved by the University of California San Diego institutional review board. Following detoxification and medical stabilization in the first week adolescents were recruited during the second week of treatment. We were unable to recruit only a small number of participants (7%) who left treatment during the first week. Adolescents voluntarily participated in a 90-minute confidential, structured interview and parents completed a separate interview with different interviewers to corroborate information. Interviews were conducted using trained clinical research interviewers and participants were assured of confidentiality to maximize open disclosure. Post-treatment interviews and assessments were conducted at the 6-month, and 1-, 2-, 4-, 6-, and 8-year time points either at the research facility or in the participant's home. For cases in which the participant had moved out of the area, interviews were completed by phone. At each interview point, a random sample of participants (approximately 15%) completed urine toxicology screens to verify self-report data. In only 2 cases were self-report data changed to include additional substance use.
Measures
Customary Drinking and Drug Use Record (CDDR)
The CDDR (Brown et al., 1998) is a well-validated structured interview that assesses alcohol and drug involvement and DSM-IIIR/IV substance use disorder diagnoses. The Lifetime version of the CDDR was administered during treatment to assess substance use history, as well as onset and recency of substance problems. Alcohol and drug use to intoxication, abuse/dependence symptoms, and withdrawal symptoms are also assessed. The CDDR has been found to be both reliable and valid when used with adolescents and adults from clinical and community samples (Brown et al., 1998).
Structured Clinical Interview (SCI)
The SCI (Brown et al., 1989) is a 90-minute confidential structured interview used to assess functioning on a variety of personal and behavioral domains. It was administered at baseline and each follow-up and covered the entire follow-up period (e.g., up to two years at a time). For the present study, interview data included demographic information (i.e., gender, age, and ethnicity), family history of alcohol/drug problems, religious background and religious practices, as well as previous SUD treatment experiences. Single-item, Likert-scale questions were employed to assess participants’ abstinence self-efficacy, perceptions of their ability to use substances in moderation, and perception that their alcohol or drug use was a problem. Participants were also asked how many AA/NA meetings they attended, as well as how many days they used alcohol and/or drugs during each follow-up . These data were used to calculate the AA/NA attendance and percent days abstinent.
Socioeconomic Status (SES)
The Hollingshead (1975) is a well-established, valid and reliable measure of socioeconomic status (SES). This was utilized to obtain an estimate of SES. SES was based on a composite of parental income, and occupational and educational status.
Conduct Disorder Questionnaire (CDQ)
The CDQ (Brown et al., 1996) is a structured interview designed to obtain DSM-III-R/DSM-IV diagnostic criteria for conduct disorder and antisocial personality disorder. The CDQ is administered to both the adolescent and the parent. Parent and teen reports were combined so that if any behavior was endorsed by either person it was included in diagnostic classification (Brown et al., 1998).
Missing Data and Imputation
We were unable to verify some of the total percent days abstinent at 6-, 12-, and 24-month follow-ups for some participants, because data had been obtained for the first three relapse episodes only in these periods. Thus, if a patient had more than three relapses that did not account for the entire follow-up period only that proportion of the period was covered (corrected in later follow-ups). This occurred for 16% (n=25) of patients at the 6m, 21% (n=34) at the 12m, and 25% (n=39) at the 24m follow-up. To minimize loss of these data, we prorated available cases for which the first three relapse episodes covered a minimum of 70% of the period. The number of cases meeting this criterion was 12, 16, and 19, for the 6-, 12-, and 24m follow-up periods, respectively (range = 70%-99%). We then prorated this observed proportion for the entire period. We ran results with, and then without, the prorated cases, and found that the pattern of findings did not differ in any substantive way. We report the results below using the prorated data.
Results
Rates of AA/NA attendance across 8 Years
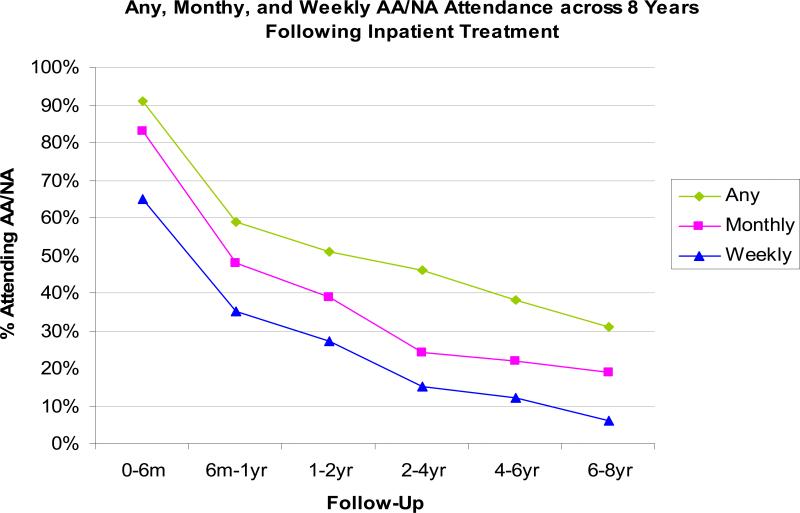
The proportion of youth attending AA/NA was high in the early months post-treatment and dropped steadily over the 8-years (figure 1). During the first 6 months, almost all youth attended AA/NA at least once, with 83% attending at least monthly, and 65% attending at least weekly, on average. These initially high rates dropped substantially between 6 and 12 months with the proportion of youth attending “any” meetings dropping to just under two-thirds, “monthly” down to about half, and “weekly” down to about one third. Between 2- and 8-years, just under one third to just under one half (range 31-46%) attended any AA/NA meetings, with about one-quarter (range 19-25%) attending at least monthly. Rates of more intensive (i.e. at least weekly) attendance also dropped across the 8 years, from two-thirds of youth in the first six months to just over one-quarter between 1- and 2-years, and only 6% between 6 and 8 years.
Figure 1.
Percent of Patients attending Any, Monthly, and Weekly AA/NA meetings across 8 Years Following Inpatient Treatment
Predictors of AA/NA attendance
We next examined baseline predictors of AA/NA attendance over the 8-year follow-up period. We tested four sets of pertinent baseline variables in relation to AA/NA attendance using Spearman correlations. These four sets of variables were (a) demographic (i.e., age, ethnicity, gender), (b) clinical (i.e., substance dependence symptoms, frequency of withdrawal symptoms, frequency of substance use, lifetime frequency of alcohol and drug intoxication, perception of having an alcohol or drug problem, perception of ability to use alcohol/drugs in moderation, abstinence self-efficacy, conduct disorder), (c) prior treatment (outpatient or inpatient), and (d) religious (i.e., religious background and religious practices).
Age, gender, and ethnicity were not associated with AA/NA attendance at any follow-up time point (ps > .18). Of the clinical/psychological predictor variables, lifetime frequency of alcohol intoxication predicted more attendance at 6 months (r = .22, p = .004), and the perception that one suffered from an alcohol problem predicted more attendance at 6 months (r = .22, p = .004) and 6 years (r=.18, p=.03). Similarly, DSM-IV substance dependence symptoms predicted more attendance at 6m (r = .22, p = .005) and 6-years (r=.19, p=.02). A stronger perception of the ability to use alcohol/drugs in moderation was a predictor of less AA/NA attendance at 6 months (r = - .32, p <.001), 1-year (r = -.22, p = .003), 2-year (r = - .19, p=.01) and 4-years (r= -.25, p=.002). Pre-treatment substance use was not related at any follow-up (ps > .94). Regarding prior treatment, more professional outpatient services for alcohol/drug-related problems was associated with greater AA/NA attendance at 8-years (r = .23, p =.006). Neither religious background nor religious practices were associated with attendance at any time points (ps > .14).
We ran a simultaneous linear regression model with these four significant predictors of AA/NA attendance to examine their unique, additive predictive ability for early post-treatment attendance (0-6m). These variables accounted for 12% of variance (adjusted) in 6-month AA/NA attendance (R2 Adj = .12, F = 6.31, p < .001). Significant variables in the prediction equation were perceived ability to consume alcohol or drugs in moderation (b = -4.13, SE= 1.68, t = -2.46, p = .01) and perception of having a problem with alcohol (b = 0.32, SE= 0.14, t = 2.26, p = .02).
Relations between AA/NA attendance and Outcomes
Table 1 shows the zero-order Spearman rank correlational relationships between AA/NA attendance and percent days abstinent (PDA) from alcohol and other drugs throughout the eight years of follow-up. The magnitudes of these bivariate correlations are initially moderate to large (rs = .46-.65), but decrease over time. These correlations reveal a pattern of significant relationships in the expected direction across time. Of further note is that AA/NA attendance in the first 6 and 12 months post-treatment was significantly associated with better outcome at every subsequent outcome time point, but the relationship between early (6-month) AA/NA attendance and PDA can be seen to gradually decline in magnitude over the 8-year follow-up.
Table 1.
Spearman Rank Order Correlations of the Relations between Youth AA/NA attendance and Substance Use Outcome
| % Days | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | AA/NA 6m | - | |||||||||||
| 2. | AA/NA 1yr | .548(**) | - | ||||||||||
| 3. | AA/NA 2yr | .490(**) | .710(**) | - | |||||||||
| 4. | AA/NA 4yr | .282(**) | .483(**) | .619(**) | - | ||||||||
| 5. | AA/NA 6yr | .174(*) | .316(**) | .339(**) | .361(**) | - | |||||||
| 6. | AA/NA 8yr | .013 | .240(**) | .179(*) | .294(**) | .471(**) | - | ||||||
| 7. | Abstinence 6m | .543(**) | .510(**) | .431(**) | .205(*) | .305(**) | .050 | - | |||||
| 8. | Abstinence 1yr | .463(**) | .650(**) | .456(**) | .281(**) | .253(**) | .169 | .722(**) | - | ||||
| 9. | Abstinence 2yr | .375(**) | .612(**) | .533(**) | .365(**) | .231(**) | .236(**) | .431(**) | .674(**) | - | |||
| 10. | Abstinence 4yr | .299(**) | .391(**) | .349(**) | .333(**) | .233(**) | .077 | .304(**) | .428(**) | .561(**) | - | ||
| 11. | Abstinence 6yr | .270(**) | .311(**) | .284(**) | .249(**) | .125 | .019 | .205(*) | .310(**) | .364(**) | .665(**) | - | |
| 12. | Abstinence 8yr | .172(*) | .336(**) | .340(**) | .275(**) | .180(*) | .148 | .216(*) | .311(**) | .363(**) | .606(**) | .741(**) | - |
p<.05
p<.01
n's vary between 133 and 159 across follow-up points due to missing data
Controlled Longitudinal Modeling of AA/NA attendance and PDA
To test the prospective relationship between AA/NA attendance in a given follow-up period and substance use in the subsequent period, we used generalized estimation equations (GEE) to model PDA at the 12-month assessment (i.e., 6-12m PDA) through 8-years incorporating both static (intake) and lagged, time-varying predictors. To determine which baseline variables to control , we examined five sets of predictor variables (a) demographic (age, gender, ethnicity, religious background and practices), (b) substance-related (pre-treatment frequency of use, lifetime frequency of alcohol and other drug intoxication, DSM-IV alcohol/drug dependence symptoms, withdrawal symptoms, beliefs about ability to use alcohol or other drugs in moderation) (c) psychological (conduct disorder diagnosis, self-efficacy), (d) treatment (prior outpatient or inpatient services), and (e) family (family history of alcohol/drug dependence). Given the number of follow-up points, we retained only those variables that predicted outcome on at least two follow-up occasions.
We found two baseline predictors of post-treatment alcohol/drug use. A greater perceived ability to use alcohol/drugs in moderation was a consistent predictor of less abstinence at every follow-up time point up through 8 years (M r = −.21; range = −.18 to −.22, ps .008−.03). And, gender predicted outcome at 4-, 6-, and 8-year follow-ups with girls/young women having more abstinent days than boys (M r = −.30, ps<.001). Therefore, these were retained as control variables. Baseline frequency of substance use (i.e. in the 90 days prior to treatment) was also retained as a static covariate. Percent days abstinent in each preceding post-treatment follow-up period was entered as a time-varying covariate to help rule out the possibility that only patients with good outcomes were attending and benefiting from AA/NA. To control for further variables that might confound AA/NA-outcome associations, the formal service utilization variables of post-treatment professional aftercare sessions, as well as any ongoing outpatient/inpatient treatment received in any follow-up, were also included as time-varying lagged covariates.
We first wanted to examine the influence of early post-treatment AA/NA attendance (0-6m) on later substance use outcomes and to test whether this effect changed over the 8-year follow-up. Concordant with the zero-order correlational results in table 1, the significant interaction between AA/NA attendance and time shown in table 2 (b= −0.1158, p=.0002) suggests that early participation predicted greater subsequent abstinence over time, but the effect was not consistent. Rather, its influence diminished across the eight years of the study such that the predicted effect of attendance in the first six months on subsequent PDA was reduced to essentially zero by the final follow-up. (This can be calculated by subtracting the AA6m × time interaction effect (−0.12) from the effect of AA6m (0.51) for each follow up time point).
Table 2.
Lagged GEE Model of Youth Treatment Outcome over 8 Years in Relation to AA/NA Attendance in the first 6 months post- treatment
| GEE Parameter Estimates Empirical Standard Error Estimates | ||||||
|---|---|---|---|---|---|---|
| Parameter | Estimate | Standard Error | 95% Confidence Limits | Z | P | |
| Intercept | 51.5854 | 10.9072 | 30.2077 | 72.9631 | 4.73 | <.0001 |
| Time | 1.0041 | 1.6354 | −2.2012 | 4.2094 | 0.61 | 0.5392 |
| Gender | −11.0712 | 4.1317 | −19.1692 | −2.9733 | −2.68 | 0.0074 |
| PDA 6m | 0.3156 | 0.0681 | 0.1821 | 0.4491 | 4.63 | <.0001 |
| Pre-treatment PDA | −0.0987 | 0.0860 | −0.2673 | 0.0700 | −1.15 | 0.2514 |
| Moderate use | −2.6835 | 1.5748 | −5.7702 | 0.4031 | −1.70 | 0.0884 |
| Formal Treatment 6m | −0.4683 | 4.6025 | −9.4889 | 8.5524 | −0.10 | 0.9190 |
| Aftercare1 6m | 0.7602 | 0.8735 | −0.9519 | 2.4724 | 0.87 | 0.3841 |
| AA/NA 6m | 0.5079 | 0.1213 | 0.2702 | 0.7455 | 4.19 | <.0001 |
| Time × AA/NA 6m | −0.1158 | 0.0316 | −0.1777 | −0.0540 | −3.67 | 0.0002 |
Square root transformed N = 150
Table 3 shows the results of the ongoing effects of AA/NA attendance over the entire 8-years using the lagged, longitudinal GEE models controlling for various confounds. For those unfamiliar with GEE, the single parameter estimates for time-varying covariates shown in tables 2 and 3 represent averaged, lagged, effects over the entire 8-year period. As shown in Table 3, participation in AA/NA across the 8-year follow-up period independently and consistently predicted a greater PDA after taking other static and time-varying covariates into account (p = .0001). Specifically, for every AA/NA meeting youths attended there was an additional subsequent gain of almost two days (1.95) days of abstinence over and above the effects of other factors. Gender also made a significant independent contribution to the model with girls, on average, having about 9 days more abstinence than boys (p=.0004). Substance use in the preceding follow-up period was found also to independently predict use in subsequent follow-ups (p < .0001). Youth perceptions that they could not moderate their substance use was on the border of statistical significance (p=.05) and there was a trend for formal treatment (p=.09).
Table 3.
Lagged GEE Model of Youth Treatment Outcome in relation to AA/NA attendance over 8 Years
| GEE Parameter Estimates Empirical Standard Error Estimates | ||||||
|---|---|---|---|---|---|---|
| Parameter | Estimate | Standard Error | 95% Confidence Limits | Z | P | |
| Intercept | 37.3071 | 6.9601 | 23.6656 | 50.9486 | 5.36 | <.0001 |
| Time | 1.4424 | 0.8693 | −0.2614 | 3.1462 | 1.66 | 0.0971 |
| Gender | −9.3380 | 2.6605 | −14.5526 | −4.1234 | −3.51 | 0.0004 |
| Pre-treatment PDA | −0.0811 | 0.0490 | −0.1772 | 0.0150 | −1.65 | 0.0980 |
| Moderate use | −1.8816 | 0.9646 | −3.7722 | 0.0090 | −1.95 | 0.0511 |
| Aftercare1 6m | 0.4349 | 0.5158 | −0.5761 | 1.4460 | 0.84 | 0.3991 |
| Formal Treatment2 | 5.5669 | 3.2856 | −0.8727 | 12.0065 | 1.69 | 0.0902 |
| AA/NA2 | 1.9517 | 0.4512 | 1.0674 | 2.8360 | 4.33 | <.0001 |
| PDA2 | 0.5030 | 0.0371 | 0.4304 | 0.5757 | 13.56 | <.0001 |
Square root transformed
Lagged, time-varying, covariate N= 160
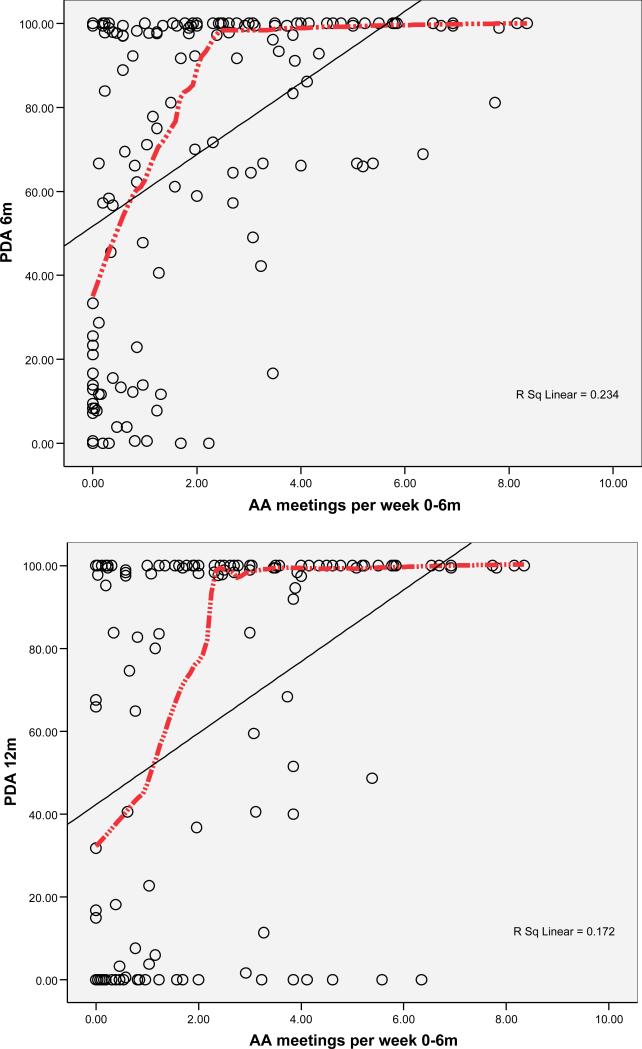
Dose-Response Curves
To examine the relation between dose of AA/NA attendance and substance use outcome, robust, locally weighted scatterplot smoothing (LOWESS) curves were fit to the data depicting the relation between AA/NA attendance in the first six months and concurrent (same 6-month period) and subsequent (following 6-month period) PDA. Rather than forcing a single linear functional relationship on the data, the LOWESS approach allows the observations to pull the regression line using a localized, weighted least squares approach (Cleveland, 1993). Figure 2 shows the relationship between the average number of 12-step meetings attended per week in the first six months (calculated as a simple average of total number of meetings divided by the number of weeks) and PDA during the same and subsequent six month time periods (the straight OLS regression lines are shown for comparison). Observable in both graphs, is that there is no noticeable minimum threshold of attendance before benefits are realized. Rather, there is a steep linear increase in PDA with better outcomes associated with as few as one meeting per week. The graph does suggest an upper threshold with attendance of three or more meetings per week, on average, associated with complete abstinence. Of note, these figures also illustrate that among those who do not attend AA/NA, there is a large range of outcomes. By contrast, among those who attend 12-step meetings very regularly, the large majority have high rates of abstinence.
Figure 2.
Exploration of Thresholds of AA/NA attendance in Relation to Concurrent and Subsequent PDA using Robust Locally weighted Scatterplot Smoothing (LOWESS) Curves (OLS Regression line also shown).
Discussion
This study found that youth AA/NA attendance early post-treatment was common and relatively intensive, but declined steadily over time. We found also that objective and subjective indices related to addiction severity predicted youth AA/NA attendance following treatment. Despite the observed declining attendance rates over the eight years, early post-treatment AA/NA attendance predicted long-term salutary outcomes. Furthermore, the effects associated with ongoing attendance remained significant and consistent. Finally, exploratory dose-response curve analyses suggested that even relatively small amounts of AA/NA was associated with benefits, with a strong linear association evident up through three meetings per week.
Rates of Attendance
The rates of AA/NA attendance in the current sample were somewhat higher than those reported previously (Brown, 1993; Kelly and Myers, 2007). Youth in the current study were recruited from traditional 12-step-oriented residential programs that may have been particularly adept at facilitating youth involvement and/or directing youth to suitable AA/NA groups. However, the decline in the proportion of youth attending and the frequency of attendance was comparable to other studies (Kelly and Myers, 2007). Noticeable in our data was a steep decline in AA/NA attendance during the six to twelve month time period after leaving residential treatment, followed by a continuing, although less sharp, decline over the remaining eight years.
Decelerating rates of AA/NA meeting attendance are also the norm among adult samples (Bond et al., 2003; Kelly and Moos, 2003; Tonigan et al., 2002) and could be explained by a number of different processes. For example, a substantial proportion may find the logistics of sustained attendance difficult, certain aspects of AA/NA meetings objectionable, or perceive it to be unhelpful or insufficient to meet their recovery needs, and subsequently discontinue. Alternatively, individuals may relapse and feel reluctant to return (Kelly et al., in press a). On the positive side, patients may benefit sufficiently from initial exposure and/or participation so that they stabilize in their recovery and do not perceive a need for continued attendance. Some of these individuals may continue to practice 12-step-related behaviors over time, despite little or no attendance (e.g., “non-attending participators”, Weiss et al., 2005). Although one study with youth found that 12-step meeting attendance was very highly correlated with 12-step practices and facilitated maintenance of abstinence motivation (Kelly et al., 2002), the influence of 12-step practices beyond meeting attendance warrants further focus in future investigations.
Of potential clinical importance is that the rates and duration of AA/NA attendance were lower than many treatment clinicians perceive as optimal (Kelly et al., in press b), suggesting potential barriers for youth in meeting this theoretically key proximal 12-step treatment outcome (Kelly et al., in press a). At least some of these barriers could be developmental (Vik et al., 1992), related to the large age difference between youth and most community AA members, whose average age is 48 years old in the U.S. (Alcoholics Anonymous, 2005). Prior research has found that youth are unlikely to find AA/NA helpful, attend as often, or benefit as much unless at least some other youth are present, suggesting that a concentrated focus on identifying and referring adolescents to suitable youth-oriented meetings might enhance engagement and retention (Brown, 1993; Kelly et al., 2005). Although such meetings are not common, most large communities have youth-specific AA/NA meetings; locating such meetings in smaller communities may be more difficult and could pose a barrier to youth AA/NA attendance.
Predictors of AA/NA attendance
Similar to other studies youth in the current study were more likely to participate if they had greater history of alcohol/drug involvement, thought they had a problem with alcohol, and did not consider themselves able to control their substance use. Interestingly, the most robust predictor of both AA/NA attendance and substance use outcomes over time was related to this construct of perceived addiction severity (Finney and Moos, 1995), such that those who believed that they were unable to use in moderation were significantly more likely to be abstinent and to be attending AA/NA compared to those who believed they could successfully moderate their use. If confirmed by additional research, this may prove useful as an efficient screening question for tailoring interventions.
Contrary to findings among adult treatment samples (Kelly et al., 2006; Tonigan et al., 2002; Winzelberg and Humphreys, 1999), the degree of religious involvement at the time of treatment entry was not a significant predictor of youth AA/NA attendance. The explicit quasi-religious/spiritual elements of AA/NA meetings may not be perceived by youth as a significant barrier to ongoing participation (Kelly et al., in press a). In terms of other demographic predictors, girls/young women were just as likely as boys/young men to attend AA/NA, similar to results found with adults (Del Boca and Mattson, 2001; Timko et al., 2005; Weisner et al, 1995).
We were able to explain only a minority of the variance in early AA/NA attendance using indirect patient-level variables (i.e., 12%). Asking patients directly whether they intend to go to AA/NA meetings may improve prediction. Also, given that family member AA/NA participation (Kelly, Myers & Rodolico, in press) and treatment staffs’ degree of 12-step facilitation (e.g., Kelly & Moos, 2003; Sisson & Malams, 1981; Tonigan et al, 2002), have both been shown to have a significant influence on patient attendance, it is likely that taking these other levels into account will help explain further variability in AA/NA attendance.
AA/NA Attendance and Treatment Outcome
Despite quite high rates of AA/NA discontinuation over time, the relationship between AA/NA attendance and outcomes remained quite stable and positive. Specifically, AA/NA attendance was consistently associated with better substance use outcomes over the 8-year period. Importantly, this effect held even after controlling for other possible confounds related to better prognosis (i.e., levels of substance use prior to treatment and in each preceding follow-up period), ongoing formal treatment service utilization, and other significant predictors of outcome. Furthermore, our examination of the short- and long-term outcome effects of early post-treatment AA/NA attendance (0-6m) suggests that what is accomplished therapeutically during this demanding early post-treatment period may have long term recovery ramifications (Moos and Moos, 2004). Whether this effect is mediated through behavioral and environmental changes provoked by AA/NA (e.g., avoidance of high risk environments; “social self-regulation”, Kelly, 2001) or cognitive and emotional shifts (e.g., belief that one cannot use substances in moderation) remains to be clarified. Given the potential importance of this finding, a possible area for future research could be in developing and testing a brief, motivational, 12-step facilitation targeting youth AA/NA attendance early post-treatment (e.g., Kahler et al., 2004).
Developmental barriers notwithstanding, the present findings, in combination with other shorter-term investigations, suggest that AA/NA may be beneficial for some youth in their recovery in the short- and long-term, particularly those who are more severely affected and who believe it is unlikely that they can successfully moderate their substance use. Little is known empirically regarding exactly why or how 12-step group participation might aid in the recovery process, but useful theoretical explications have been proposed (e.g., McCrady, 1994; Moos, 2007). Ongoing recovery-specific support from organizations like AA may help reduce relapse risk, in part, by providing a social context where sober role-models and friends are available and provide alternative socially rewarding activities (Brown, 2001; Moos, 2007; Longabaugh et al., 1998). Studies that conducted formal mediational tests to examine how AA/NA exert beneficial effects have found that participation may help maintain motivation for abstinence, enhance coping and self-efficacy, and facilitate abstinence-reinforcing changes in the social network (Bond et al., 2003; Connors and Tonigan, 2001; Humphreys and Noke, 1997; Kaskutas et al., 2002; Morgenstern et al., 1997; Morgenstern and Bates, 1999; Kelly et al., 2000; 2002; Owen et al., 2003). More research is needed to understand how robust such mechanisms are across samples and through developmental transitions, and whether these mechanisms are temporally stable or change over time (Brown, 1993; Brown and Ramo, 2006; Gorski and Miller, 1992).
Thresholds of AA/NA attendance
Our investigation of thresholds of AA/NA attendance in relation to outcome suggest youth may benefit from even limited exposure post-treatment. For patients selecting into AA/NA, even one or two meetings per week were associated with marked increases in abstinence, and a threshold of three meetings per week was associated with complete abstinence. These findings suggest that meeting a criterion of “90 meetings in 90 days” or other highly intensive adult-derived clinical recommendation may not be critical for this age-group. Furthermore, qualitative investigations of AA/NA attendance with youth (e.g., Kelly et al., in press a), suggest that while adolescents may not immerse themselves as intensively into 12-step-specific program content as adults (e.g., working the 12-steps), they may still derive benefit from the more general group therapy processes (Yalom, 1995) inherent in AA/NA group meetings (e.g, “universality”, “instillation of hope”, “catharsis”; McCrady, 1994; Kelly et al., in press a). These findings imply adolescents may not need to attend as frequently as their more chronically dependent older adult counterparts in order to obtain similar outcomes. Furthermore, compared to adults, youth may obtain AA/NA recovery-related benefits through different processes, or by similar processes, that possess a different degree of salience depending on developmental stage (Kelly et al., 2000).
Limitations
Generalizations should be made with caution in light of some important limitations. First, we used only a simple measure of frequency of AA/NA attendance and did not assess the degree of involvement. Although this straightforward measure was predictive in our study, we do not know the extent to which these youth may be continuing to engage in 12-step practices, such as using a sponsor or helping others. In addition, observational study design precludes true cause and effect inferences regarding the benefits of AA/NA attendance. However, we conducted controlled, time lagged, analyses to help rule out possible confounds. A further limitation is that we used data aggregated over long time periods (up to 2 years at a time), which does not allow for examination of the more fine-grained, dynamic relationships between 12-step attendance topography and substance use outcomes. The data also were obtained mostly by self-report, which can be prone to recall and social desirability biases. However, standardized procedures to minimize these biases were implemented (Babor et al., 1987; Brown, 2004). Also, in keeping with other reports (Harrison et al., 2007) our urine toxicology verification on a random sample of subjects suggests the self-reports are valid. This study also examined only 12-step and not other mutual-help groups (e.g., SMART Recovery, Secular Organization for Sobriety). Further investigation is warranted to see if youth might derive more or less benefit from other organizations. Finally, generalizations to other treated youth should be made with caution since our sample was comprised of adolescents, recruited from 12-step-oriented inpatient settings and contained a high number of youth reporting amphetamine use (53%), which may be higher than other U.S. regions where amphetamine use is less common. To the extent that youth who use amphetamine/methamphetamine in addition to alcohol and other drugs may differ systematically from youth that do not use amphetamines, findings here may not generalize.
Summary and Conclusions
Alcohol and other drug use disorders are chronic conditions that frequently require ongoing management, monitoring, and intervention to achieve lasting remission and recovery (McLellan, 2002). Widely available, recovery-specific resources, such as AA and NA, have shown to have both utility and cost-effectiveness (Humphreys and Moos, 2001; 2007; Kelly & Yeterian, in press), and thus serve an important public health role in helping to reduce the endemic problems arising from substance misuse. For youth that develop sufficiently severe alcohol- and drug-related problems to warrant residential treatment so early in their development, ongoing support from fellowships like AA and NA may help buffer the risk of relapse as normative rates of substance use rise among their peers in the general population and where support for recovery may be minimal (Grant et al., 2004; Johnston et al., 2007; SAMHSA, 2006). From a recovery management perspective (White et al., 2006), this study suggests that, similar to older adults, treated youth with more severe substance-involvement appear to attend and benefit from the use of these organizations over time. Successful early post-treatment engagement of youth in abstinence-supportive social contexts may have long-term implications for alcohol and drug involvement into young adulthood.
Acknowledgments
Sources of Support: NIAAA R01AA015526-01A1
Contributor Information
John F. Kelly, Massachusetts General Hospital, Center for Addiction Medicine & Harvard Medical School, and University of California, San Diego
Sandra A. Brown, Veterans Affairs San Diego Healthcare System, and University of California, San Diego
Ana Abrantes, Butler Hospital & Brown University, Medical School, and University of California, San Diego
Christopher Kahler, Brown University Center for Alcohol and Addiction Studies, and University of California, San Diego
Mark Myers, Veterans Affairs San Diego Healthcare System, and University of California, San Diego
References
- Alcoholics Anonymous . Twelve Steps and Twelve Traditions. Alcoholics Anonymous World Services; New York: 1953. [Google Scholar]
- Alcoholics Anonymous . Alcoholics Anonymous: The Story of How Thousands of Men and Women Have Recovered from Alcoholism. 4th ed. Alcoholics Anonymous World Services; New York: 2001. [Google Scholar]
- Alcoholics Anonymous . 2004 Membership Survey. Alcoholics Anonymous World Services; New York: 2005. [Google Scholar]
- Alford GS, Koehler RA, Leonard J. Alcoholics Anonymous-Narcotics Anonymous model inpatient treatment of chemically dependent adolescents: a 2-year outcome study. J Stud Alcohol. 1991;52:118–126. doi: 10.15288/jsa.1991.52.118. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 3rd ed., rev. Author; Washington, D.C.: 1987. [Google Scholar]
- American Psychiatric Association . Practice Guideline for Psychiatric Evaluation of Adults. 2nd ed. Author; Washington, DC: 2006. [Google Scholar]
- Babor TF, Stephens RS, Marlatt GA. Verbal report methods in clinical research on alcoholism: response bias and its minimization. J Stud Alcohol. 1987;48:410–424. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and Alcoholics Anonymous on abstinence. J Stud Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Brown SA. Recovery patterns in adolescent substance abuse. In: Marlatt GA, Baer JS, editors. Addictive Behaviors across the Life Span: Prevention, Treatment, and Policy Issues. Sage Publications, Inc; Newbury Park, CA: 1993. pp. 161–183. [Google Scholar]
- Brown SA. Facilitating change for adolescent alcohol problems: a multiple options approach. In: Wagner EF, Waldron HB, editors. Innovations in Adolescent Substance Abuse Intervention. Elsevier Science; Oxford, UK: 2001. pp. 169–187. [Google Scholar]
- Brown SA. Measuring youth outcomes from alcohol and drug treatment. Addictions. 2004;99:38–46. doi: 10.1111/j.1360-0443.2004.00853.x. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn AA, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. J Stud Alcohol. 1996;57:314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Brown SA, Mott MA, Myers MG. Adolescent alcohol and drug treatment outcome. In: Watson R, editor. Drug and Alcohol Abuse Reviews: Drug and Alcohol Abuse Prevention. Humana Press; Clifton, NJ: 1990. pp. 373–403. [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. J Stud Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Ramo DE. Clinical course of youth following treatment for alcohol and drug problems. In: Liddle H, Rowe C, editors. Adolescent Substance Abuse: Research and Clinical Advances. Cambridge University Press; Cambridge, UK: 2006. pp. 79–103. [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addict Behav. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Cleveland WS. Visualizing Data. Hobart Press; Summit, NJ: 1993. [Google Scholar]
- Cleveland WS, Devlin SJ. Locally weighted regression: an approach to regression analysis by local fitting. Journal of the American Statistical Association. 1988;83:596–610. [Google Scholar]
- Conner M, Norman P. Predicting Health Behavior: Research and Practice with Social Cognition Models. Open University Press; Buckingham, England: 1996. [Google Scholar]
- Connors GJ, Tonigan JS. A longitudinal model of intake symptomatology, AA participation and outcome: retrospective study of the project MATCH outpatient and aftercare samples. J Stud Alcohol. 2001;62:817–825. doi: 10.15288/jsa.2001.62.817. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Mattson ME. The Gender Matching Hypothesis. Project MATCH monograph series. U.S. Department of Health and Human Services; Bethesda, MD: 2001. [Google Scholar]
- Drug Strategies . Treating Teens: A Guide to Adolescent Programs. Author; Washington, D.C.: 2003. [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: what is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. Rutgers Center of Alcohol Studies; Piscataway, NJ: 1993. pp. 41–76. [Google Scholar]
- Fenster J. Characteristics of clinicians likely to refer clients to 12-Step programs versus a diversity of post-treatment options. Drug Alcohol Depend. 2006;83:238–246. doi: 10.1016/j.drugalcdep.2005.11.017. [DOI] [PubMed] [Google Scholar]
- Finney JW. Enhancing substance abuse treatment evaluations: examining mediators and moderators of treatment effects. J Subst Abuse. 1995;7:135–150. doi: 10.1016/0899-3289(95)90310-0. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk R, Passetti LL. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23:21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- Gorski T, Miller M. Staying sober: a guide for relapse prevention. Staying Sober Workbook: A Serious Solution for the Problem of Relapse. Herald House/Independence Press; 1992. [Google Scholar]
- Grant B, Dawson D, Stinson F, Chou S, Dufour M, Pickering R. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Harrison LD, Martin SS, Enev T, Harrington D. Comparing Drug Resting and Self-Report of Drug Use among Youths and Young Adults in the General Population (DHHS Publication No. SMA 07-4249, Methodology Series M-7) Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2007. [Google Scholar]
- Hohman L, LeCroy CW. Predictors of adolescent AA affiliation. Adolescence. 1996;31:339–352. [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Position. Yale University; New Haven, CT: 1975. [Google Scholar]
- Hsieh S, Hoffman NG, Hollister DC. The Relationship between pre-, during-, post-treatment factors, and adolescent substance abuse behaviors. Addict Behav. 1998;23:477–488. doi: 10.1016/s0306-4603(98)00028-8. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Clinicians’ referral and matching of substance abuse patients to self-help groups after treatment. Psychiatric Services. 1997;48:1445–1449. doi: 10.1176/ps.48.11.1445. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Circles of Recovery: Self-help Organizations for Addictions. Cambridge University Press; Cambridge, UK: 2004. [Google Scholar]
- Humphreys K, Moos R. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol Clin Exp Res. 2001;25:711–716. [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Encouraging post-treatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcohol Clin Exp Res. 2007;31:64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Noke JM. The influence of posttreatment mutual help group participation on the friendship networks of substance abuse patients. Am J Community Psychol. 1997;25:1–16. doi: 10.1023/a:1024613507082. [DOI] [PubMed] [Google Scholar]
- Hunt WA, Barnett LW, Branch LG. Relapse rates in addiction programs. J Clin Psychol. 1971;27:455–456. doi: 10.1002/1097-4679(197110)27:4<455::aid-jclp2270270412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Bridging the Gap: Forging New Partnerships in Community-based Drug Abuse Treatment. National Academy Press; Washington, D.C.: 1998. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975-2006: Volume I. Secondary school students (NIH Publication No. 07-6205) National Institute on Drug Abuse; Bethesda, MD: 2007. [Google Scholar]
- Kahler C, Read J, Stuart G, Ramsey S, McCrady B, Brown R. Motivational enhancement for 12-step involvement among patients undergoing alcohol detoxification. J Consult Clin Psychol. 2004;72:736–741. doi: 10.1037/0022-006X.72.4.736. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly JF. Do adolescents affiliate with 12-step groups? A multivariate process model of effects. Dissertation Abstracts International. 2001;62(3B):AAT 3007131. doi: 10.15288/jsa.2002.63.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF. Self-help for substance use disorders: history, effectiveness, knowledge gaps and research opportunities. Clin Psychol Rev. 2003;23:639–663. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Moos RH. Dropout from 12-step self-help groups: prevalence, predictors and counteracting treatment influences. J Subst Abuse Treat. 2003;24:241–250. doi: 10.1016/s0740-5472(03)00021-7. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Myers MG. Adolescents’ participation in Alcoholics Anonymous and Narcotics Anonymous: review, implications, and future directions. Journal of Psychoactive Drugs. 2007;39:259–269. doi: 10.1080/02791072.2007.10400612. 2007. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychol Addict Behav. 2000;14:376–389. [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Brown SA. Do adolescents affiliate with 12-step Groups? A multivariate process model of effects. J Stud Alcohol. 2002;63:293–304. doi: 10.15288/jsa.2002.63.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Brown SA. The effects of age composition of 12-step groups on adolescent 12-step participation and substance use outcome. Journal of Child & Adolescent Substance Abuse. 2005;15:67–76. doi: 10.1300/J029v15n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Rodolico J. What do adolescents think about 12-step groups? Perceptions and experiences of two AA-exposed clinical samples. J Subst Abuse. in press a. [Google Scholar]
- Kelly JF, Stout R, Zywiak W, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcohol Clin Exp Res. 2006;30:1381–1392. doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Yeterian J. Mutual-Help Groups. In: O'Donohue W, Cunningham JR, editors. Empirically Supported Adjunctive Therapies. Elsevier; New York: in press. [Google Scholar]
- Kelly JF, Yeterian JD, Myers MG. Treatment staff referrals, participation expectations, and perceived benefits and barriers to adolescent involvement in 12-step groups. Alcoholism Treatment Quarterly. doi: 10.1080/07347320802347053. in press b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy BP, Minami M. The Beech Hill Hospital/Outward Bound Adolescent Chemical Dependency Treatment Program. J Subst Abuse Treat. 1993;10:395–406. doi: 10.1016/0740-5472(93)90025-w. [DOI] [PubMed] [Google Scholar]
- Kissin W, McLeod C, McKay J. The longitudinal relationship between self-help group attendance and course of recovery. Evaluation and Program Planning. 2003;26:311–323. [Google Scholar]
- Laudet AB, White WL. An exploratory investigation of the association between clinicians’ attitudes toward twelve-step groups and referral rates. Alcoholism Treatment Quarterly. 2005;23:31–45. doi: 10.1300/J020v23n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93:1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Zweben A, Locatsro JS, Miller WR. Origins, issues and options in the development of the combined behavioral intervention. J Stud Alcohol. 2005;66:179–187. doi: 10.15288/jsas.2005.s15.179. [DOI] [PubMed] [Google Scholar]
- Magura S, Fong C, Staines GL, Cleland C, Foote J, Rosenblum A, Kosanke N, DeLuca A. The combined effects of treatment intensity, self-help groups and patient attributes on drinking outcomes. J Psychoactive Drugs. 2005;37:85–92. doi: 10.1080/02791072.2005.10399751. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Have we evaluated addiction treatment correctly? Implications from a chronic care perspective. Addiction. 2002;97:249–252. doi: 10.1046/j.1360-0443.2002.00127.x. [DOI] [PubMed] [Google Scholar]
- McCrady BS. Alcoholics Anonymous and behavior therapy: can habits be treated as diseases? Can diseases be treated as habits? J Consult Clin Psychol. 1994;62:1159–1166. doi: 10.1037//0022-006x.62.6.1159. [DOI] [PubMed] [Google Scholar]
- McElrath D. The Minnesota model. J Psychoactive Drugs. 1997;29:141–144. doi: 10.1080/02791072.1997.10400180. [DOI] [PubMed] [Google Scholar]
- McKay JR. The role of continuing care in outpatient alcohol treatment programs. In: Galanter M, editor. Recent Developments in Alcoholism, Vol. 15, Services Research in the Era of Managed Care. Plenum Publishing; New York: 2001. pp. 357–373. [DOI] [PubMed] [Google Scholar]
- McKay JR, McLellan AT, Alterman AI, Cacciola JS, Rutherford MJ, O'Brien CP. Predictors of participation in aftercare sessions and self-help groups following completion of intensive outpatient treatment for substance abuse. J Stud Alcohol. 1998;59:152–162. doi: 10.15288/jsa.1998.59.152. [DOI] [PubMed] [Google Scholar]
- Moos R. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88:109–121. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R, Moos B. Long-term influence of duration and frequency of participation in Alcoholics Anonymous on individuals with alcohol use disorders. J Consult Clin Psychol. 2004;72:81–90. doi: 10.1037/0022-006X.72.1.81. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Bates ME. Effects of executive treatment. J Stud Alcohol. 1999;60:846–855. doi: 10.15288/jsa.1999.60.846. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. J Consult Clin Psychol. 1997;65:768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- NIDA . Principles of Drug Abuse Treatment: A Research-Based Guide. NIH Publication No. 00-4180. NIDA; Rockville, MD: 2000. [Google Scholar]
- Nowinski J, Baker S, Carroll K. Project MATCH Monograph Series, Vol. 1. (NIH Pub. No. 94-3722) National Institute on Alcoholism and Alcohol Abuse; Rockville, MD: 1995. Twelve Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- Owen PL, Slaymaker V, Tonigan JS, McGrady BS, Epstein EE, Kaskuatas LA, Humphreys K, Miller WR. Participation in AA: intended and unintended change mechanisms. Alcohol Clin Exp Res. 2003;27:524–532. doi: 10.1097/01.ALC.0000057941.57330.39. [DOI] [PubMed] [Google Scholar]
- Pettinati HM, Weiss RD, Dundon W, Miller WR, Donovan D, Ernst DB, et al. A structured approach to medical management: a psychosocial intervention to support pharmacotherapy in the treatment of alcohol dependence. J Stud Alcohol. 2005;66:170–178. doi: 10.15288/jsas.2005.s15.170. [DOI] [PubMed] [Google Scholar]
- Roman PM, Blum TC. National Treatment Center Study, Summary 3. University of Georgia; Athens, GA: 1999. [Google Scholar]
- Rosenstock I. Historical origins of the health belief model. Health Education Monographs. 1974;2 doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Sisson RW, Mallams JH. The use of systematic encouragement and community access procedures to increase attendance at Alcoholic Anonymous and Al-Anon meetings. American Journal of Drug and Alcohol Abuse. 1981;8(3):371–376. doi: 10.3109/00952998109009560. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2005 National Survey on Drug Use and Health: National Findings. (NSDUH Series H-30, DHHS Publication No. SMA 06-4194) Office of Applied Studies; Rockville, MD: 2006. [Google Scholar]
- Suchman EA. Evaluative Research: Principles and Practice in Public Service & Social Action Programs. Russell Sage Foundation; New York: 1967. [Google Scholar]
- Timko C, Finney JW, Moos RH. The 8-year course of alcohol abuse: gender differences in social context and coping. Alcohol Clin Exp Res. 2005;29:612–621. doi: 10.1097/01.alc.0000158832.07705.22. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Schermer C. Atheists, agnostics, and Alcoholics Anonymous. J Stud Alcohol. 2002;63:534–541. doi: 10.15288/jsa.2002.63.534. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. J Stud Alcohol. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- Veterans Health Administration . Management of Substance Use Disorders in the Primary and Specialty Care. Office of Quality and Performance and the Veterans Affairs and Department of Defense Development Work Group; Washington, D.C.: 2001. [Google Scholar]
- Vik PW, Grizzle KL, Brown SA. Social resource characteristics and adolescent substance abuse relapse. Journal of Adolescent Chemical Dependency. 1992;2:59–74. [Google Scholar]
- Weisner C, Greenfield T, Room R. Trends in the treatment of alcohol problems in the US general population, 1979 through 1990. Am J Public Health. 1995;85:55–60. doi: 10.2105/ajph.85.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Gallop R, Luborsky L, Siqueland L, Frank A, et al. Predictors of self-help group participation in cocaine dependent patients. J Stud Alcohol. 2000;61:714–719. doi: 10.15288/jsa.2000.61.714. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Gallop RJ, Najavits LM, Frank A, Crits-Christoph P, et al. The effect of 12-step self-help group attendance and participation on drug use outcomes among cocaine-dependent patients. Drug Alcohol Depend. 2005;77:177–184. doi: 10.1016/j.drugalcdep.2004.08.012. [DOI] [PubMed] [Google Scholar]
- White W, Kurtz E, Sanders M. Recovery Management. Great Lakes ATTC Monograph; Chicago: 2006. [Google Scholar]
- Winzelberg A, Humphreys K. Should patients’ religiosity influence clinicians’ referral to 12-step self-help groups? Evidence from a study of 3018 male substance abuse patients. J Consult Clin Psychol. 1999;67:790–794. doi: 10.1037//0022-006x.67.5.790. [DOI] [PubMed] [Google Scholar]
- Yalom ID. Theory and Practice of Group Psychotherapy. Basic Books; New York: 1995. [Google Scholar]