Abstract
PURPOSE
To describe racial variations in the prevalence of refractive errors among adult white, Chinese, Hispanic, and black subjects in the United States.
DESIGN
Cross-sectional data from a prospective cohort study—the Multi-Ethnic Study of Atherosclerosis (MESA).
METHODS
A total of 6000 adults aged 45 to 84 years living in the United States participated in the study. Refractive error was assessed, without cycloplegia, in both eyes of all participants using an autorefractor. After excluding eyes with cataract, cataract surgery, or previous refractive surgery, the eye with the larger absolute spherical equivalent (SE) value for each participant was used to classify refractive error. Any myopia was defined as SE of −1.0 diopters (D) or less; high myopia was defined as SE of −5.0 D or less; any hyperopia was defined as SE of +1.0 D or more; clinically significant hyperopia was defined as SE of +3.0 D or more. Astigmatism was defined as a cylinder value of +1.0 D or more.
RESULTS
After excluding 508 participants with cataracts in both eyes, 838 participants with cataract surgery, 90 participants with laser refractive surgery, and 134 participants who refused to remove their contact lenses for the refraction measurement, 4430 adults with refractive error assessment in at least 1 eye contributed to the analysis. The prevalence of myopia among MESA participants was 25.1%, with lowest rates in Hispanic participants (14.2%), followed by black (21.5%) and white participants (31.0%), and highest rates in Chinese participants (37.2%). The overall rates of high myopia and astigmatism were 4.6% and 45.0%, respectively, with Chinese subjects also having the highest rates of high myopia (11.8%) and astigmatism (53.4%). The overall prevalence of any hyperopia was 38.2% and clinically significant hyperopia was 6.1%, with Hispanic participants having the highest rates of hyperopia (50.2%) and clinically significant hyperopia (8.8%). In multivariate analyses adjusting for age, sex, race, and study site, higher education level, being employed, and being taller were associated with a higher prevalence of myopia. In contrast, lower educational level and being shorter were associated with a higher prevalence of hyperopia.
CONCLUSIONS
Myopia and astigmatism were most prevalent in the Chinese population, with Chinese subjects having 3 times the prevalence of myopia as Hispanic subjects. Hyperopia was most common in Hispanic subjects. These findings provide further insights into variations in refractive errors among different racial groups and have important implications for the eye care services in the United States.
REFRACTIVE ERRORS ARE SIGNIFICANT PUBLIC health concerns in the United States1–3 and throughout the world.4–6 Approximately 1.6 billion people worldwide are affected by myopia and the prevalence of myopia is expected to increase to 2.5 billion by the year 2020.7 Uncorrected refractive error is a leading cause of visual loss in the population, and high myopia is associated with higher risks of cataract,8,9 glaucoma,10 and retinal diseases.11,12 It is estimated that globally 153 million people over 5 years of age are visually impaired as a result of uncorrected refractive errors, of whom 8 million are blind.13 It is widely believed that refractive errors, especially myopia, are multi-factorial traits, involving the effect of genes as well as environmental factors.6,14–16 Race may be a surrogate for differences in both genetic biomarkers and environmental exposures such as the intensity of schooling, near work, outdoor activity, and lifestyle factors. Current data, largely based on studies in children, have shown significant racial difference in the prevalence of myopia. For example, in Asia, where a perceived “epidemic” of myopia has been observed, Chinese children have been reported to have higher prevalence of myopia compared with other racial groups.17–19 In the United States, the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEER) found that Asian children had the highest prevalence of myopia (18.5%), followed by Hispanic subjects (13.2%). White subjects had the lowest prevalence of myopia (4.4%), which was not significantly different from black subjects (6.6%).20
However, the exact pattern of racial variations in adult populations remains unclear, and most studies have compared racial differences between disparate populations and used varying definitions. The Tanjong Pagar study21 on a Singapore Chinese population reported a myopia prevalence of 51.7% in female subjects and 45.2% in male subjects in the 40- to 49-year-old group, whereas the meta-analysis by Kempen and associates reported a prevalence of 46.3% for US white female subjects and 36.8% for male subjects in the same age group.7 Given that the analysis by Kempen and associates used a more stringent criterion of -1 diopter (D) whereas the Tanjong Pagar analysis used −0.5 D, it is unclear if there are true racial differences between Singapore Chinese and US white subjects. In the 1999-2004 National Health and Nutrition Examination Survey (NHANES) on a nationally representative sample of the US noninstitutionalized, civilian population 12 years and older, myopia was more common in non-Hispanic white subjects (35.2%) than in non-Hispanic black (28.6%) or Hispanic subjects (25.1%).22 However, the prevalence of myopia in Chinese American subjects was not reported in NHANES. Furthermore, racial differences in other refractive errors such as hyperopia and astigmatism are less well studied.
In this paper, we described the prevalence of refractive errors in the middle- and older-age adults of 4 racial groups in the United States: white, Chinese, black, and Hispanic.
METHODS
STUDY POPULATION
The Multi-Ethnic Study of Atherosclerosis (MESA) is a prospective cohort study of adults aged 45 to 84 years sampled from 6 United States communities who, at the time of study enrollment, were free from clinical cardiovascular disease. Details of the design and methodology of the study have been described elsewhere.23 In brief, the MESA cohort includes 6814 men and women 45 to 84 years old at baseline (July 2000 to July 2002) who were recruited from 6 field centers: Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles, California; New York, New York; and St Paul, Minnesota. Each site planned to examine about 1100 eligible participants, equally divided between men and women, according to site-specified race/ethnicity proportions. Each field site recruited from locally available sources, which included lists of residents, lists of dwellings, and telephone exchanges. In the last few months of the recruitment period, supplemental sources (ie, lists of Medicare beneficiaries from the Centers for Medicare and Medicaid Services and referrals by participants) were used to ensure adequate numbers of minorities and elderly subjects. In general, we sought to recruit a population-based cohort from defined census tracts or an occupational cohort using a random selection process. Of the 6814 adults examined at baseline, 6233 returned for a second examination and 6099 agreed to participate in the refraction component offered to them (August 2002 to February 2004). Table 1 shows the distribution of the MESA study participants in each study site by racial group. All participants completed a study questionnaire inquiring about demographic, behavioral, and personal medical history.
TABLE 1.
Distribution of the Study Participants in Each Study Site by Racial Groups in the Multi-Ethnic Study on Atherosclerosis
| White |
Chinese |
Black |
Hispanic |
|||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Forsyth County, North Carolina | ||||||||
| Baseline examination (n = 6814) | 573 | 53.2 | 0 | 0 | 501 | 46.5 | 3 | 0.3 |
| Second examination (n = 6233) | 536 | 54.4 | 0 | 0 | 446 | 45.3 | 3 | 0.3 |
| Agreeing to refraction (n = 6099) | 531 | 55.4 | 0 | 0 | 423 | 44.3 | 3 | 0.3 |
| Included in the analysis (n = 4430) | 359 | 52.7 | 0 | 0 | 320 | 47.0 | 2 | 0.3 |
| New York, New York | ||||||||
| Baseline examination (n = 6814) | 223 | 20.2 | 2 | 0.2 | 381 | 34.6 | 496 | 45.0 |
| Second examination (n = 6233) | 214 | 20.8 | 2 | 0.2 | 354 | 34.4 | 459 | 44.6 |
| Agreeing to refraction (n = 6099) | 212 | 21.0 | 2 | 0.2 | 347 | 34.4 | 449 | 44.5 |
| Included in the analysis (n = 4430) | 142 | 19.4 | 0 | 0 | 256 | 35.0 | 334 | 45.6 |
| Baltimore, Maryland | ||||||||
| Baseline examination (n = 6814) | 533 | 49.1 | 0 | 0 | 553 | 50.9 | 0 | 0 |
| Second examination (n = 6233) | 483 | 50.5 | 0 | 0 | 473 | 49.5 | 0 | 0 |
| Agreeing to refraction (n = 6099) | 472 | 50.8 | 0 | 0 | 458 | 49.2 | 0 | 0 |
| Included in the analysis (n = 4430) | 323 | 49.4 | 0 | 0 | 331 | 50.6 | 0 | 0 |
| St Paul, Minnesota | ||||||||
| Baseline examination (n = 6814) | 605 | 56.8 | 0 | 0 | 0 | 0 | 461 | 43.2 |
| Second examination (n = 6233) | 567 | 58.5 | 0 | 0 | 0 | 0 | 402 | 41.5 |
| Agreeing to refraction (n = 6099) | 566 | 59.0 | 0 | 0 | 0 | 0 | 394 | 41.0 |
| Included in the analysis (n = 4430) | 396 | 55.5 | 0 | 0 | 0 | 0 | 318 | 44.5 |
| Chicago, Illinois | ||||||||
| Baseline examination (n = 6814) | 557 | 47.9 | 304 | 26.1 | 303 | 26.0 | 0 | 0 |
| Second examination (n = 6233) | 531 | 49.1 | 277 | 25.6 | 273 | 25.3 | 0 | 0 |
| Agreeing to refraction (n = 6099) | 511 | 49.2 | 264 | 25.4 | 264 | 25.4 | 0 | 0 |
| Included in the analysis (n = 4430) | 350 | 46.7 | 192 | 25.6 | 208 | 27.7 | 0 | 0 |
| Los Angeles County, California | ||||||||
| Baseline examination (n = 6814) | 131 | 9.9 | 497 | 37.7 | 155 | 11.8 | 536 | 40.6 |
| Second examination (n = 6233) | 133 | 11.0 | 449 | 37.0 | 145 | 12.0 | 486 | 40.1 |
| Agreeing to refraction (n = 6099) | 128 | 10.7 | 447 | 37.2 | 143 | 11.9 | 483 | 40.2 |
| Included in the analysis (n = 4430) | 97 | 10.8 | 487 | 11.0 | 115 | 12.8 | 392 | 43.6 |
Tenets of the Declaration of Helsinki were followed, and institutional review board approval was granted at each study site. Written informed consent was obtained from each participant.
REFRACTIVE ASSESSMENT
Participants underwent an examination for refractive errors performed using a tabletop autorefractor (NIDEK model ARK-760A; Nidek Co Ltd, Tokyo, Japan). In a dim room, participants had each eye refracted separately without pharmacologic cycloplegia by trained technicians certified for adherence to a standardized study protocol. Refractive error values of sphere and cylinder were measured to the closest 0.25 D using positive cylinder notation.
EXCLUSION CRITERIA
Two participants who had no light perception in both eyes and 1 participant who had a serious eye infection at the time of the examination were considered ineligible for this study. Six participants who wore an eye patch to the examination did not have refraction testing performed on the patched eye. Participants wearing contact lenses were asked to remove them before measurements were taken. Incomplete refraction data were obtained from 96 individuals who did not complete the assessment because of physical limitations, scheduling conflicts, or equipment failure.
Of the 6099 agreeing to participate in the refraction component, spherical equivalent (SE) data in at least 1 eye was available from 6000 participants. We excluded from this analysis 508 participants with cataracts in both eyes, 838 participants with cataract surgery, 90 participants with laser refractive surgery, and 134 participants who refused to remove their contact lenses for the refraction measurement. There were 4430 eligible participants with complete refraction data in at least 1 eye and 1669 participants who either were ineligible, did not have complete refractive data in either eye, or were otherwise excluded.
CLASSIFICATION OF REFRACTIVE ERRORS
For all eyes contributing data to this analysis, we calculated spherical equivalent (SE) by adding the spherical diopter value to half of the cylinder diopter value. Refractive errors were also categorized into types, using values from the eye with the larger absolute SE. High myopia was defined as SE of −5.0 D or less; any myopia was defined as SE of −1.0 D or less; any hyperopia was defined as +1.0 D or more; clinically significant hyperopia was defined as +3.0 D or more. Astigmatism was defined as at least 1 D of cylinder, without reference to the axis.
STATISTICAL ANALYSES
Demographics of subjects included in and excluded from analysis were compared. For those included in analysis, demographics were described and compared stratified by race and sex. The prevalence of different refractive errors was estimated within each racial group, adjusting for age, sex, and height. We adjusted for height since it was significantly associated with the prevalence of refractive errors in our study. Variables of interest significant in univariate analysis were included in multivariate logistic regression models to determine whether a variable of interest was associated with a specific type of refractive error. Odds ratio (OR) and 95% confidence interval (CI) were presented. Statistical analyses were performed using SAS software (SAS Institute Inc, Cary, North Carolina, USA).
RESULTS
THE DISTRIBUTION OF DEMOGRAPHIC CHARACTERISTICS of these included and excluded groups is shown in Table 2. Demographic characteristics of participants by sex are presented separately for white, Chinese, black, and Hispanic subjects in Table 3.
TABLE 2.
Comparison of Participants Included in and Excluded From Analysis of Refraction Data From the Multi-Ethnic Study on Atherosclerosis
| Excluded (N = 1669) |
Included (N = 4430) |
P | |
|---|---|---|---|
| Sex | |||
| Male | 676 (40.5%) | 2215 (50.0%) | <.001 |
| Female | 993 (59.5%) | 2215 (50.0%) | |
| Race | |||
| White | 754 (45.2%) | 1667 (37.6%) | <.001 |
| Chinese | 227 (13.6%) | 487 (11.0%) | |
| Black | 406 (24.3%) | 1230 (27.8%) | |
| Hispanic | 282 (16.9%) | 1046 (23.6%) | |
| Age | |||
| Mean ± SD (y) | 69.7 ± 9.23 | 61.3 ± 9.4 | <.001 |
| 45-54 y | 147 (8.8%) | 1280 (28.9%) | |
| 55-64 y | 262 (15.7%) | 1506 (34.0%) | |
| 65-74 y | 689 (41.3%) | 1196 (27.0%) | |
| 75+ y | 571 (34.3%) | 448 (10.1%) | |
| Education | |||
| <12 y | 294 (17.6%) | 728 (16.4%) | .339 |
| Completed HS/GED | 324 (19.4%) | 785 (17.7%) | |
| Some college | 464 (27.8%) | 1281 (28.9%) | |
| Bachelor’s degree | 292 (17.5%) | 798 (18.0%) | |
| Graduate/professional degree |
295 (17.6%) | 838 (18.9%) | |
| Marital status | |||
| Single | 139 (8.3%) | 377 (8.5%) | <.001 |
| Married | 956 (57.3%) | 2780 (63.2%) | |
| Divorced | 249 (14.9%) | 806 (18.2%) | |
| Widowed | 325 (19.5%) | 443 (10.0%) | |
| Occupation | |||
| Homemaker | 219 (13.1%) | 443 (10.0%) | <.001 |
| Employed | 584 (35.0%) | 2640 (59.6%) | |
| Unemployed | 23 (1.4%) | 137 (3.1%) | |
| Retired | 843 (50.5%) | 1210 (27.3%) | |
| Income | |||
| <20K | 487 (29.2%) | 935 (21.1%) | <.001 |
| 20K-<40K | 464 (27.8%) | 1205 (27.2%) | |
| 40K-<75K | 382 (22.9%) | 1214 (27.4%) | |
| >75K | 336 (20.1%) | 1076 (24.3%) | |
| Medical insurance available |
1632 (97.8%) | 4049 (91.4%) | <.001 |
| Hypertension | 920 (55.1%) | 1869 (42.2%) | <.001 |
| Diabetes | 551 (33.0%) | 1373 (31.0%) | .144 |
| Current smoker | 129 (7.7%) | 576 (13.0%) | <.001 |
| Wear glasses for distance vision |
1237 (74.1%) | 2848 (64.3%) | <.001 |
| Height in cm | 164.5 ± 9.8 | 166.7 ± 9.4 | <.001 |
| Study site | |||
| Forsyth County, NC | 279 (16.7%) | 682 (15.4%) | .139 |
| New York, NY | 279 (16.7%) | 733 (16.5%) | |
| Baltimore, MD | 275 (16.5%) | 652 (14.7%) | |
| St Paul, MN | 245 (14.7%) | 714 (16.1%) | |
| Chicago, IL | 290 (17.4%) | 754 (17.0%) | |
| Los Angeles, CA | 301 (18.0%) | 895 (20.2%) |
GED = general education diploma; HS = high school; K = thousand (US$).
TABLE 3.
Demographics of Participants With Refraction Data by Race and Sex in the Multi-Ethnic Study on Atherosclerosis
| White Subjects N = 1667 |
Chinese Subjects N = 487 |
Black Subjects N = 1230 |
Hispanic Subjects N = 1046 |
|||||
|---|---|---|---|---|---|---|---|---|
| Men n = 860 |
Women n = 807 |
Men n = 251 |
Women n = 236 |
Men n = 641 |
Women n = 589 |
Men n = 530 |
Women n = 516 |
|
| Mean age (SD) | 62.37 (9.59) | 60.86 (9.17) | 61.15 (9.35) | 59.35 (8.70) | 62.04 (9.50) | 61.20 (9.20) | 60.84 (9.55) | 60.64 (9.49) |
| Mean height in cm (SD) | 175.86 (6.91) | 162.30 (6.46) | 168.25 (6.20) | 156.28 (5.46) | 175.95 (6.87) | 162.33 (6.83) | 168.99 (6.37) | 155.44 (6.32) |
| Education | ||||||||
| <12 y | 33 (3.9%) | 28 (3.5%) | 38 (14.8%) | 63 (26.7%) | 68 (10.7%) | 54 (9.1%) | 206 (39.0%) | 236 (45.8%) |
| Completed HS/GED | 107 (12.4%) | 149 (18.5%) | 30 (12.0%) | 55 (23.3%) | 124 (19.3%) | 107 (18.2%) | 103 (19.4%) | 112 (21.7%) |
| Some college | 212 (24.6%) | 269 (33.3%) | 40 (16.0%) | 50 (21.2%) | 219 (34.2%) | 214 (36.3%) | 155 (29.3%) | 122 (23.6%) |
| Bachelor’s degree | 212 (24.6%) | 181 (22.4%) | 71 (28.4%) | 42 (17.8%) | 124 (19.3%) | 108 (18.4%) | 32 (6.0%) | 30 (5.8%) |
| Graduate/ professional degree |
296 (34.5%) | 180 (22.3%) | 72 (28.8%) | 26 (11.0%) | 106 (16.5%) | 106 (18.1%) | 34 (6.4%) | 16 (3.0%) |
| Income | ||||||||
| <20K | 48 (5.6%) | 95 (11.8%) | 83 (32.9%) | 101 (42.7%) | 105 (16.4%) | 109 (18.5%) | 159 (30.0%) | 229 (44.4%) |
| 20K-<40K | 157 (18.2%) | 180 (22.3%) | 60 (24.1%) | 59 (24.8%) | 181 (28.2%) | 200 (33.9%) | 191 (36.0%) | 177 (34.4%) |
| 40K-<75K | 282 (32.8%) | 254 (31.5%) | 44 (17.7%) | 37 (15.8%) | 204 (31.9%) | 188 (31.9%) | 120 (22.7%) | 86 (16.6%) |
| >75K | 373 (43.4%) | 278 (34.5%) | 64 (25.3%) | 39 (16.7%) | 151 (23.5%) | 93 (15.8%) | 60 (11.3%) | 24 (4.6%) |
| Current smoker | 111 (12.9%) | 98 (12.1%) | 26 (10.4%) | 6 (2.5%) | 132 (20.6%) | 89 (15.1%) | 74 (14.0%) | 45 (8.7%) |
GED = general education diploma; HS = high school; K = thousand (US$).
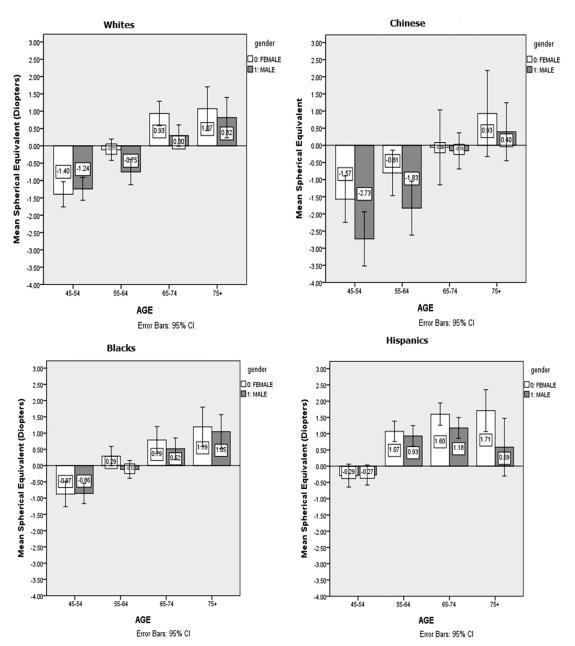
Refractive error, defined as mean SE of both eyes, differs by age and sex and is depicted graphically for each ethnic group in the Figure. Across ethnic groups, negative SE values were more common at the younger ages, whereas positive SE values predominated at the older ages. Women tended to have more extreme SE values as compared with men of comparable age, except among Chinese subjects. Chinese men had lower SE values compared with Chinese women. In contrast to the other racial groups, Chinese subjects had the most variation in SE values across the age range of MESA participants.
FIGURE.
Distribution of mean spherical equivalent by age and sex for white, Chinese, black, and Hispanic subjects in the Multi-Ethnic Study on Atherosclerosis.
Age-, sex-, and height-adjusted rates of specific types of refractive errors are presented by racial group and overall in Table 4. The prevalence of myopia among all MESA participants was 25.1% (1111/4430), although the rates varied from 14.2% (149/1046) in Hispanic subjects to 37.2% (181/487) in Chinese subjects. The overall rates of high myopia and astigmatism were 4.6% (204/4430) and 45.0% (1993/4430), respectively. Again, contrasting the racial groups, Chinese subjects also had the highest rates of high myopia (11.8%, 57/487) and astigmatism (53.4% 260/487). The overall prevalence of any hyperopia was 38.2% (1694/4430) and clinically significant hyperopia was 6.1% (271/4430). Hispanic subjects had the highest rates of hyperopia (50.2%, 525/1046) and clinically significant hyperopia (8.8%, 92/1046).
TABLE 4.
Age-, Sex-, and Height-Adjusted Prevalence of Refractive Errors for Each Racial Group and Overall in the Multi-Ethnic Study on Atherosclerosis
| White | Chinese | Black | Hispanic | P Value | Overall | |
|---|---|---|---|---|---|---|
| High myopia | 90 (5.4%) | 57 (11.8%) | 38 (3.1%) | 19 (1.8%) | <.001 | 204 (4.6%) |
| Any myopia | 517 (31.0%) | 181 (37.2%) | 264 (21.5%) | 149 (14.2%) | <.001 | 1111 (25.1%) |
| Any hyperopia | 585 (35.1%) | 120 (24.7%) | 464 (37.7%) | 525 (50.2%) | <.001 | 1694 (38.2%) |
| Clinically significant hyperopia | 102 (6.1%) | 17 (3.4%) | 60 (4.9%) | 92 (8.8%) | <.001 | 271 (6.1%) |
| Astigmatism | 760 (45.6%) | 260 (53.4%) | 529 (43.0%) | 444 (42.4%) | <.001 | 1993 (45.0%) |
| Emmetropia | 565 (33.9%) | 186 (38.1%) | 502 (40.8%) | 372 (35.6%) | <.001 | 1625 (36.7%) |
Various refractive types adjusted for major demographic factors are presented in Table 5. Controlling for all other factors in the model, the risk of myopia was significantly higher in the younger ages compared with older ages, whereas the opposite was true for hyperopia and astigmatism. Compared with white participants, Chinese subjects were more likely to have myopia, whereas black and Hispanic subjects were less likely. For hyperopia, Chinese subjects were less likely, Hispanic subjects more likely, and black subjects just as likely to have rates comparable to white subjects. For astigmatism, Hispanic subjects were less likely, Chinese subjects more likely, and black subjects just as likely to have astigmatism compared with white subjects. Female subjects were somewhat more likely than male subjects to have myopia or hyperopia; male subjects were more likely than female subjects to have astigmatism. There was no association between income and any type of refractive error; however, those who were currently or formerly employed were more likely to have myopia compared with homemakers. Employment history was not associated with hyperopia or astigmatism. Increasing educational level was associated with increasing risk of myopia in a dose-response manner, whereas those at the highest education levels were least likely to have hyperopia. There was no association between educational level and astigmatism. Height was positively associated with myopia, whereas it was negatively associated with hyperopia. There was no association of height with high myopia, clinically significant hyperopia, or astigmatism.
TABLE 5.
Results From Multiple Logistic Regression Analysis of Factors Associated With Refractive Errors Among Participants of the Multi-Ethnic Study on Atherosclerosis
| High Myopia |
Any Myopia |
Any Hyperopia |
Significant Hyperopia |
Astigmatism |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age (y) | ||||||||||
| 45-54 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| 55-64 | 0.74 (0.55-1.01) | .060 | 0.69 (0.58-0.82) | <.001 | 3.34 (2.77-4.04) | <.001 | 3.43 (2.16-5.44) | <.001 | 1.50 (1.27-1.77) | <.001 |
| 65-74 | 0.29 (0.17-0.48) | <.001 | 0.41 (0.33-0.52) | <.001 | 5.31 (4.27-6.61) | <.001 | 6.48 (3.99-10.52) | <.001 | 2.81 (2.31-3.43) | <.001 |
| 75+ | 0.32 (0.14-0.69) | .004 | 0.43 (0.30-0.60) | <.001 | 5.66 (4.24-7.57) | <.001 | 9.20 (5.28-16.05) | <.001 | 6.18 (4.66-8.25) | <.001 |
| Race | ||||||||||
| White | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Chinese | 3.33 (2.08-5.36) | <.001 | 1.64 (1.24-2.18) | .001 | 0.63 (0.47-0.85) | .002 | 0.65 (0.36-1.16) | .141 | 1.16 (0.89-1.49) | .271 |
| Black | 0.77 (0.52-1.15) | .202 | 0.79 (0.65-0.96) | .019 | 0.93 (0.78-1.11) | .459 | 0.64 (0.45-.89) | .009 | 0.92 (0.78-1.10) | .370 |
| Hispanic | 0.63 (0.37-1.07) | .090 | 0.61 (0.47-0.79) | <.001 | 1.48 (1.18-1.86) | .001 | 1.09 (0.74-1.63) | .643 | 0.79 (0.64-0.98) | .035 |
| Sex | ||||||||||
| Female | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Male | 0.81 (0.54-1.20) | .293 | 0.82 (0.66-1.02) | .072 | 0.82 (0.67-1.00) | .051 | 0.71 (0.50-1.02) | .064 | 1.19 (0.99-1.45) | .058 |
| Income | ||||||||||
| <20K | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| 20K-<40K | 0.72 (0.44-1.17) | .184 | 0.86 (0.67-1.10) | .229 | 1.17 (0.96-1.43) | .121 | 1.02 (0.73-1.43) | .889 | 0.94 (0.78-1.14) | .537 |
| 40K-<75K | 0.77 (0.47-1.25) | .290 | 0.98 (0.76-1.7) | .895 | 0.98 (0.79-1.22) | .869 | 1.08 (0.74-1.59) | .677 | 0.92 (0.75-1.14) | .463 |
| 75K+ | 0.82 (0.50-1.36) | .447 | 0.98 (0.738-1.27) | .800 | 1.17 (0.91-1.51) | .230 | 1.25 (0.79-1.99) | .340 | 0.95 (0.75-1.20) | .651 |
| Occupation | ||||||||||
| Homemaker | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Employed | 1.94 (1.95-3.96) | .068 | 1.59 (1.17-2.16) | .003 | 1.02 (0.80-1.31) | .872 | 1.15 (0.75-1.75) | .521 | 0.88 (0.69-1.11) | .280 |
| Unemployed | 3.63 (1.45-9.08) | .006 | 1.66 (1.01-2.75) | .046 | 0.76 (0.47-1.23) | .266 | 1.45 (0.60-3.49) | .407 | 1.07 (0.70-1.64) | .746 |
| Retired | 2.05 (0.93-4.52) | .075 | 1.37 (0.98-1.92) | .068 | 1.12 (0.86-1.45) | .397 | 1.18 (0.78-1.78) | .436 | 0.92 (0.71-1.18) | .504 |
| Education | ||||||||||
| Less than HS | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| HS diploma | 2.15 (0.88-5.30) | .093 | 1.32 (0.95-1.82) | .095 | 0.91 (0.72-1.15) | .450 | 1.03 (0.72-1.49) | .856 | 0.84 (0.67-1.06) | .150 |
| Some college | 3.36 (1.46-7.70) | .004 | 1.94 (1.44-2.62) | <.001 | 0.79 (0.63-0.99) | .039 | 0.66 (0.45-0.98) | .039 | 0.98 (0.79-1.23) | .885 |
| Bachelor’s degree | 6.88 (2.98-15.90) | <.001 | 2.69 (1.95-3.71) | <.001 | 0.61 (0.47-0.79) | <.001 | 0.72 (0.46-1.15) | .169 | 0.97 (0.75-1.25) | .810 |
| Graduate school | 8.99 (3.85-20.98) | <.001 | 3.45 (2.48-4.81) | <.001 | 0.52 (0.39-0.68) | <.001 | 0.50 (0.30-0.83) | .008 | 1.00 (0.77-1.31) | .974 |
| Height (cm) | 1.00 (0.98-1.03) | .735 | 1.01 (1.00-1.03) | .018 | 0.99 (0.98-1.0) | .015 | 0.99 (0.97-1.01) | .228 | 1.00 (0.99-1.00) | .758 |
| Study site | ||||||||||
| Forsyth County, NC | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| New York, NY | 1.17 (0.65-2.13) | .609 | 1.26 (0.94-1.68) | .118 | 1.11 (.87-1.43) | .389 | 1.82 (1.17-2.82) | .007 | 1.20 (0.94-1.54) | .139 |
| Baltimore, MD | 1.19 (0.68-2.08) | .546 | 1.33 (1.01-1.74) | .040 | .88 (.69-1.13) | .322 | 1.09 (0.69-1.72) | .703 | 1.38 (1.08-1.75) | .008 |
| St Paul, MN | 1.94 (1.11-3.38) | .020 | 1.76 (1.33-2.34) | <.001 | .68 (.53-.89) | .004 | 0.93 (0.58-1.49) | .755 | 1.36 (1.06-1.75) | .015 |
| Chicago, IL | 1.35 (0.80-2.26) | .260 | 1.79 (1.38-2.33) | <.001 | .69 (.54-.89) | .004 | 0.76 (0.46-1.26) | .293 | 1.44 (1.13-1.83) | .003 |
| Los Angeles, CA | 0.81 (0.44-1.49) | .494 | 1.10 (0.82-1.49) | .516 | .71 (.55-.93) | .013 | 0.78 (0.47-1.28) | .323 | 1.42 (1.11-1.83) | .006 |
CI = confidence interval; HS = high school; K = thousand (US$); OR = odds ratio.
DISCUSSION
IN THIS STUDY, WE REPORTED A HIGHER PREVALENCE OF myopia in Chinese subjects compared with other racial groups living in the United States, with a 3-fold higher prevalence of myopia and a 5-fold higher prevalence of high myopia in Chinese subjects as compared with Hispanic subjects. We also reported that hyperopia was most prevalent in Hispanic subjects among the 4 racial groups represented in the study. These data provided new insights into racial differences in the prevalence of refractive errors in the United States, showing that Chinese adults were more likely to be myopic than their non-Chinese counterparts.
Previous studies in children have shown clear racial differences in myopia prevalence between Chinese and white subjects. However, it has been unclear whether Chinese subjects are more susceptible to myopia or more likely to be affected by myopia at an earlier age since the racial differences were not significant in adults. Current data based on comparisons of prevalence between studies must be interpreted with caution because of methodological issues, including differences in sampling strategy, sample size, response rate, age range of the study participants, refraction method, definition of myopia, and other details that may not have been reported in publications.24 In the 1999-2004 NHANES on US citizens aged over 20 years, myopia was more common in non-Hispanic white (35.2%) than in non-Hispanic black (28.6%) or Hispanic subjects (25.1%).2,22 However, the NHANES did not include a sufficient number of Chinese individuals to derive stable estimates of refractive error in this population subgroup. Our study overcame these limitations by comparing the prevalence of myopia and other refractive errors among major racial groups, including Chinese, using the same methods to collect data. Our study partially confirmed the findings from the pediatric population in the CLEER study by showing that Chinese subjects aged over 45 years were also more likely to be myopic compared with other racial groups. However, it was interesting to find that the prevalence of myopia in white subjects was also considerably higher than in Hispanic or black subjects, albeit a bit lower than in Chinese subjects. This finding contrasted with the data from the CLEER study, which showed that white subjects were least likely to be affected by myopia among the 4 racial groups.20 This finding has an important implication, because the increase in prevalence of myopia in white subjects may indicate that there may be an epidemic of myopia in the white population in the future, as has been observed in an Asian population.25
Information on the prevalence of high myopia is important since it is well known to be linked with various ocular morbidities.26,27 The racial patterns of myopia and high myopia were similar, with Chinese subjects being most likely and Hispanic subjects being least likely to be affected. However, the magnitude of the racial difference in the prevalence of high myopia was significantly larger than in myopia. Chinese subjects had a 5-fold higher prevalence of high myopia compared with Hispanic subjects, whereas the racial difference for myopia was only 3-fold. Therefore, Chinese subjects may be at much higher risk of being affected by vision-threatening ocular complications such as myopic macular degeneration11,28 as compared with other racial groups in the United States.
The reasons for the observed racial differences in myopia prevalence are poorly understood. Chinese individuals may have a genetic predisposition to myopia, and they also devote more time to rigorous learning and less time in outdoor play in their early years of life compared to other ethnic groups.4 However, in our study, white subjects were not less educated than Chinese subjects (Table 3). This is noteworthy since educational level is a strong predictor for myopia, which was thought to be mediated through the effects of prolonged amounts of near work, especially in childhood. However, recent cohort studies demonstrated that the effect of near work on the risk of myopia is quite limited. The Singapore Cohort Study of the Risk Factors for Myopia assessed refractive error and near-work activities in 994 nonmyopic Chinese children aged 7 to 9 years over a 3-year period. None of the variables related to near work, alone or in the aggregate, was a significant risk factor for myopia.29 Similar findings were replicated in non-Asian children in the Orinda Longitudinal Study of Myopia.30 Based on current evidence, it is still impossible to conclude that near work is an independent risk factor for myopia.31 Thus, the racial difference may be explained by other factors not captured by our study, including time spent outdoors in childhood or possibly genetic factors. However, we believe that the role of genetic factors might be limited, since there have been no myopia-related genetic loci found to be associated specifically with Chinese ethnicity. In contrast, time spent outdoors has been shown to be a protective factor for myopia in longitudinal studies30,32 as well as meta-analysis.33 This hypothesis was also supported by animal studies, where ambient light levels have been found to influence the rate of visually induced form-deprivation myopia,34,35 as well as the rate of compensation to monocularly imposed myopic and hyperopic defocus.36 Therefore, we hypothesize that differences in time spent outdoors in childhood is the most likely explanation for the racial differences observed in MESA.
Racial differences in other refractive errors such as hyperopia and astigmatism have not been well established yet. In our study, Hispanic subjects were most likely to be hyperopic, whereas Chinese subjects were most likely to be astigmatic. Hyperopia, especially clinically significant hyperopia, is an understudied refractive error, usually receiving less attention than myopia. Although low levels of hyperopia in younger persons may not result in decreased visual acuity, after the age of approximately 35 years many hyperopic individuals are in need of correction for optimal vision. Persons with hyperopia are more likely to complain of headache and eye strain for near-vision tasks and will likely require correction for clear near vision sooner than their peers without this refractive error. It is also true that people with hyperopia may complain of blurry vision in the distance as well as at near. Most importantly, recent studies have identified hyperopia as a potential risk factor for age-related macular degeneration, a major cause of irreversible vision loss in the elderly.26,37–39 In our study, the high prevalence of hyperopia in Hispanic subjects may be attributable to the lower educational level in this ethnic group. Our study and previous ones have confirmed the link between lower educational level and hyperopic shift in refraction.40–43 Since Hispanic subjects in our study were the least educated racial group, this may explain their high prevalence of hyperopia compared with the other racial groups. Myopia and astigmatism are highly correlated, and we believe that the high prevalence of astigmatism in Chinese subjects contributed to their high prevalence of myopia.
The MESA was designed to investigate the prevalence and progression of subclinical cardiovascular disease in adults without known cardiovascular disease at baseline. Thus, the MESA participants are not completely representative of the whole US population. However, the MESA is a population-based study, of which the study sample was selected from the general population rather than hospitals or health care settings. Study participants were also from 6 US communities from a wide range of geographic distributions. Furthermore, the effect of any bias is marginal since cardiovascular disease is unrelated to refractive errors. Therefore, we believe that the MESA cohort could be representative of the pattern of racial variations in refractive errors within the US population at large.
Our findings have important public health implications. The burden of refractive error in all of the major racial groups living in the United States is considerable. Individuals with refractive error require, in most cases, refractive correction to maintain reasonable levels of vision, and to achieve this will entail recurring costs associated with routine eye examinations and the purchase of spectacles, contact lenses, or refractive surgery. The economic burden (including indirect costs) of refractive error in the United States among persons aged 40 years and older was estimated to be $5.5 billion in 2006.44 Many people, even those with health insurance, do not have vision care coverage and need to pay out of pocket for refractive correction. Some people simply cannot afford refractive correction. Therefore, since vision clarity is so critical for many aspects of daily living, including vehicular driving and use of electronic devices, correction of refractive error has impact on quality of life and even public safety.
Although our study has many strengths (eg, a large multi-ethnic cohort and refraction performed using a standard protocol with quality assurance procedures obtained at all study sites), there are limitations as well. Participants enrolled in MESA are adults who were 45-84 years of age and free of overt cardiovascular disease at study entry and, therefore, they cannot be considered a random sample of persons in the designated study areas. We cannot be certain how this sampling might have influenced the findings we report. This limits the comparison of our study with other studies randomly sampling participants of various ages from a specific racial group. However, we believe that the study sample was similar to a random sample and the effect of volunteers was marginal since the study participants were free of cardiovascular disease, which is unrelated to refractive errors. In addition, this study did not perform cycloplegia refraction or collect other biometric measurements such as ocular axial length, an endophenotype of refractive errors. Finally, some important predictors of refractive errors such as time spent outdoors, time spent reading, and place of birth were not captured by our study; therefore, we are unable to estimate the effect of these factors on observed differences among racial groups.
In summary, refractive errors were common among the 4 major racial groups of adults aged 45-84 years living in the United States. Myopia and astigmatism were most prevalent in the Chinese group, whereas hyperopia was most prevalent among Hispanic subjects. These findings have important implications for the eye care services needed by different racial groups in the United States.
Acknowledgments
ALL AUTHORS HAVE COMPLETED AND SUBMITTED THE ICMJE FORM FOR DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST and none were reported. Publication of this article was supported by contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute and National Institute of Health Intramural Research award ZAIEY000403 from the National Eye Institute (M.F.C.), Bethesda, Maryland. Contributions of authors: involved in design of study (B.E.K., Ro.K., A.F., T.Y.W); conduct of study (B.E.K., M.F.C., S.S., Ro.K., A.F., Ri.K., S.J.S, G.L.B., T.Y.W.); collection of data (B.E.K., M.F.C., S.S., Ro.K., A.F., Ri.K., S.J.S, G.L.B., T.Y.W.); management (T.Y.W.), analysis (C.W.P., S.S., S.M.S.), and interpretation (C.W.P., B.E.K., M.F.C., S.S., Ro.K., A.F., Ri.K., S.J.S, G.L.B., S.M.S., T.Y.W.) of data; preparation of manuscript (C.W.P., B.E.K., M.F.C., S.S., Ro.K., A.F., Ri.K., S.J.S., G.L.B., S.M.S., T.Y.W.); and review and approval of manuscript (C.W.P., B.E.K., M.F.C., S.S., Ro.K., A.F., Ri.K., S.J.S, G.L.B., S.M.S., T.Y.W.).
Biosketch
Chen-Wei Pan is currently working as a research fellow at the National University of Singapore. He obtained his medical degree from Fudan University in Shanghai and PhD degree from National University of Singapore. His main research interest is the epidemiology of myopia and other eye diseases.
REFERENCES
- 1.Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2002;43(8):2566–2571. [PubMed] [Google Scholar]
- 2.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 3.Wang Q, Klein BE, Klein R, Moss SE. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1994;35(13):4344–4347. [PubMed] [Google Scholar]
- 4.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 5.Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32(1):3–16. doi: 10.1111/j.1475-1313.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 6.Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005;24(1):1–38. doi: 10.1016/j.preteyeres.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Kempen JH, Mitchell P, Lee KE, et al. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004;122(4):495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- 8.Wong TY, Foster PJ, Johnson GJ, Seah SK. Refractive errors, axial ocular dimensions, and age-related cataracts: the Tanjong Pagar survey. Invest Ophthalmol Vis Sci. 2003;44(4):1479–1485. doi: 10.1167/iovs.02-0526. [DOI] [PubMed] [Google Scholar]
- 9.Wong TY, Klein BE, Klein R, Tomany SC, Lee KE. Refractive errors and incident cataracts: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2001;42(7):1449–1454. [PubMed] [Google Scholar]
- 10.Wong TY, Klein BE, Klein R, Knudtson M, Lee KE. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology. 2003;110(1):211–217. doi: 10.1016/s0161-6420(02)01260-5. [DOI] [PubMed] [Google Scholar]
- 11.Neelam K, Cheung CM, Ohno-Matsui K, Lai TY, Wong TY. Choroidal neovascularization in pathological myopia. Prog Retin Eye Res. 2012;31(5):495–525. doi: 10.1016/j.preteyeres.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Wong TY, Klein R, Klein BE, Tomany SC. Refractive errors and 10-year incidence of age-related maculopathy. Invest Ophthalmol Vis Sci. 2002;43(9):2869–2873. [PubMed] [Google Scholar]
- 13.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86(1):63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mutti DO, Zadnik K, Adams AJ. Myopia. The nature versus nurture debate goes on. Invest Ophthalmol Vis Sci. 1996;37(6):952–957. [PubMed] [Google Scholar]
- 15.Zadnik K, Satariano WA, Mutti DO, Sholtz RI, Adams AJ. The effect of parental history of myopia on children’s eye size. JAMA. 1994;271(17):1323–1327. [PubMed] [Google Scholar]
- 16.Pan CW, Zheng YF, Wong TY, et al. Variation in prevalence of myopia between generations of migrant Indians living in Singapore. Am J Ophthalmol. 2012;154(2):376–381. doi: 10.1016/j.ajo.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 17.Wu HM, Seet B, Yap EP, Saw SM, Lim TH, Chia KS. Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom Vis Sci. 2001;78(4):234–239. doi: 10.1097/00006324-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Dirani M, Chan YH, Gazzard G, et al. Prevalence of refractive error in Singaporean Chinese children: the strabismus, amblyopia, and refractive error in young Singaporean Children (STARS) study. Invest Ophthalmol Vis Sci. 2010;51(3):1348–1355. doi: 10.1167/iovs.09-3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive error and visual impairment in school-age children in Gombak District, Malaysia. Ophthalmology. 2005;112(4):678–685. doi: 10.1016/j.ophtha.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 20.Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121(8):1141–1147. doi: 10.1001/archopht.121.8.1141. [DOI] [PubMed] [Google Scholar]
- 21.Wong TY, Foster PJ, Hee J, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41(9):2486–2494. [PubMed] [Google Scholar]
- 22.Vitale S, Ellwein L, Cotch MF, Ferris FL, 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126(8):1111–1119. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156(9):871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 24.Saw SM. A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom. 2003;86(5):289–294. doi: 10.1111/j.1444-0938.2003.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 25.Park DJ, Congdon NG. Evidence for an “epidemic” of myopia. Ann Acad Med Singapore. 2004;33(1):21–26. [PubMed] [Google Scholar]
- 26.Pan CW, Cheung CY, Aung T, et al. Differential associations of myopia with major age-related eye diseases: The Singapore Indian Eye Study. Ophthalmology. doi: 10.1016/j.ophtha.2012.07.065. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 27.Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25(5):381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 28.Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109(4):704–711. doi: 10.1016/s0161-6420(01)01024-7. [DOI] [PubMed] [Google Scholar]
- 29.Saw SM, Shankar A, Tan SB, et al. A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci. 2006;47(5):1839–1844. doi: 10.1167/iovs.05-1081. [DOI] [PubMed] [Google Scholar]
- 30.Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48(8):3524–3532. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mutti DO, Zadnik K. Has near work’s star fallen? Optom Vis Sci. 2009;86(2):76–78. doi: 10.1097/OPX.0b013e31819974ae. [DOI] [PubMed] [Google Scholar]
- 32.Jones-Jordan LA, Mitchell GL, Cotter SA, et al. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011;52(3):1841–1850. doi: 10.1167/iovs.09-4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012;119(10):2141–2151. doi: 10.1016/j.ophtha.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 34.Ashby R, Ohlendorf A, Schaeffel F. The effect of ambient illuminance on the development of deprivation myopia in chicks. Invest Ophthalmol Vis Sci. 2009;50(11):5348–5354. doi: 10.1167/iovs.09-3419. [DOI] [PubMed] [Google Scholar]
- 35.Smith EL, 3rd, Hung LF, Huang J. Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2012;53(1):421–428. doi: 10.1167/iovs.11-8652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ashby RS, Schaeffel F. The effect of bright light on lens compensation in chicks. Invest Ophthalmol Vis Sci. 2010;51(10):5247–5253. doi: 10.1167/iovs.09-4689. [DOI] [PubMed] [Google Scholar]
- 37.Lavanya R, Kawasaki R, Tay WT, et al. Hyperopic refractive error and shorter axial length are associated with age-related macular degeneration: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2010;51(12):6247–6252. doi: 10.1167/iovs.10-5229. [DOI] [PubMed] [Google Scholar]
- 38.Ikram MK, van Leeuwen R, Vingerling JR, Hofman A, de Jong PT. Relationship between refraction and prevalent as well as incident age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci. 2003;44(9):3778–3782. doi: 10.1167/iovs.03-0120. [DOI] [PubMed] [Google Scholar]
- 39.Wang JJ, Mitchell P, Smith W. Refractive error and age-related maculopathy: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 1998;39(11):2167–2171. [PubMed] [Google Scholar]
- 40.Pan CW, Wong TY, Lavanya R, et al. Prevalence and risk factors for refractive errors in Indians: the Singapore Indian Eye Study (SINDI) Invest Ophthalmol Vis Sci. 2011;52(6):3166–3173. doi: 10.1167/iovs.10-6210. [DOI] [PubMed] [Google Scholar]
- 41.Saw SM, Chan YH, Wong WL, et al. Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology. 2008;115(10):1713–1719. doi: 10.1016/j.ophtha.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 42.Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology. 1999;106(6):1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 43.Krishnaiah S, Srinivas M, Khanna RC, Rao GN. Prevalence and risk factors for refractive errors in the South Indian adult population: The Andhra Pradesh Eye Disease Study. Clin Ophthalmol. 2009;3:17–27. [PMC free article] [PubMed] [Google Scholar]
- 44.Rein DB, Zhang P, Wirth KE, et al. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol. 2006;124(12):1754–1760. doi: 10.1001/archopht.124.12.1754. [DOI] [PubMed] [Google Scholar]