Abstract
Collaborative care models (CCMs) provide a pragmatic strategy to deliver integrated mental health and medical care for persons with mental health conditions served in primary care settings. CCMs are team-based intervention to enact system-level redesign by improving patient care through organizational leadership support, provider decision support, and clinical information systems as well as engaging patients in their care through self-management support and linkages to community resources. The model is also a cost-efficient strategy for primary care practices to improve outcomes for a range of mental health conditions across populations and settings. CCMs can help achieve integrated care aims under healthcare reform yet organizational and financial issues may affect adoption into routine primary care. Notably, successful implementation of CCMs in routine care will require alignment of financial incentives to support systems redesign investments, reimbursements for mental health providers, and adaptation across different practice settings and infrastructure to offer all CCM components.
Keywords: Mental health, Co-occurring conditions, Primary care, PCP, Integrated care, Collaborative care, Chronic Care Model, CCM, Accountable care organization, ACO, Patient centered medical home, Screening, Diagnosis, Treatment, Access, Mental health services, Psychiatry, Bipolar disorder, Mood disorder, Substance abuse disorder, Anxiety disorder, Serious mental illness
Introduction
Mental health conditions are common and are the leading cause of disability worldwide [1]. In the United States, over 25% of the population is affected by one or more of these conditions at any one time [2]. Primary care settings are the locale where up to 70% of patients are diagnosed and treated for the most prevalent mental health conditions including anxiety, mood, and substance use disorders [3, 4]. Furthermore, medical comorbidity is the rule for this population in which the majority suffer from at least one co-occurring chronic medical illness [5]. Because many acute and chronic medical conditions (e.g., chronic pain, COPD, obesity) involve health behaviors or psychosocial issues with the potential to exacerbate symptoms or undermine treatment outcomes, primary care is well-suited as the medical home for provision of essential behavioral health care [6].
Despite the availability of effective mental health treatments, these interventions are rarely employed in a coordinated approach in routine care to yield long-term improvement in mental health outcomes [5, 7]. Among patients with access to primary care who are accurately diagnosed with depression, fewer than 15% receive adequate treatment to achieve remission [8]. Primary care providers (PCPs) continue to encounter barriers to referring patients to specialty mental health settings while patient uptake to these offsite referrals remains low [9-11]. Furthermore, physicians, physician assistants, and nurses often lack the time or training to effectively address mental health needs [12].
Collaborative care models (CCM) provide a pragmatic strategy to deliver integrated mental health and general medical care in primary care settings [7]. CCMs are a team-based, multicomponent intervention to enact care delivery redesign by systematically improving coordination of patient care through organizational leadership support, evidence-based provider decision-making, and clinical information systems as well as engaging patients in their care through self-management support and linkages to community resources. Recent systematic reviews found that CCMs are a cost-efficient strategy for primary care practices to improve mental and physical outcomes for a range of mental health conditions across diverse populations and primary care settings [13, ••14]. However, current payment models discourage integrated primary care through financing carve-ins and carve-outs that make it difficult for PCPs to receive reimbursement for behavioral health services [••15, 16].
The enactment of the U.S. Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 and the U.S. Patient Protection and Affordable Care Act of 2010 (ACA) combine to present an opportunity to implement organizational and financial strategies to better integrate mental health care into primary care settings through CCMs [17-20]. Collaborative care is an underlying tenant in healthcare reform including two ACA mechanisms to control costs in complex patient populations: the patient centered medical home and accountable care organizations (ACOs) [8, 21, ••22, 23, 24-30]. As many aspects of ACA policy have yet to be finalized, mental health providers and PCPs have a vested stake in understanding current issues pertaining to mental health CCMs to better advocate for policies that can promote the uptake of this model to help achieve the triple aim of improving health and quality of care in a cost-efficient manner [17, 31].
In light of emerging healthcare reform initiatives, this paper presents a critical review of the recent literature published about the topic of CCM for mental health in primary care settings, with particular emphasis on highlighting literature relevant to the implementation of this treatment model in routine practice. To achieve this end, we conducted a rigorous search of Pubmed® to identify relevant English-language articles published between January 2012 and March 2013 that included empirically-based research studies, topical reviews, influential commentaries, and guideline/consensus statements focused on collaborative care for mental health in adult patient populations. Key words utilized in the search included: “primary care”, “general medicine”, “collaborative care”, “integrative care”, “chronic care model”, “patient-centered medical home”, “medical home” “treatment model”, “mental health”, “mental health disorders” “mood disorders”, “anxiety disorders”, “depression”, “bipolar disorder”, “substance abuse disorder”, “addiction disorder”, “serious mental illness”, and “behavioral medicine.” A total of 74 articles were identified for inclusion in this review of the literature [5-10, 13, ••14, ••15, 16-21, •22, 23, 24, 26, 27, 29, 30, 32-36, ••37, 38-40, •41, •42, 43-47, ••48, 49-53, ••54, 55-68, •69, 70-83].
Based on this literature review, we identified the following issues pertinent to clinicians, researchers, and policy makers: 1) defining essential components of collaborative care for mental health in primary care; 2) summarizing recent systematic reviews that document CCMs as cost-effective, evidenced-based treatments to achieve integrated care outcomes; and 3) highlighting issues affecting the implementation and sustainability of CCMs in routine care settings.
Key Components of Collaborative Care Models for Mental Health
Because there are a number of models for providing integrated care in primary care settings [84], it is helpful to begin with an operational definition of what constitutes mental health collaborative care. Simply co-locating a mental health professional into a primary care setting has been proven insufficient to improve mental health outcomes [5, 7, 38]. Comparatively, the U.S. Community Preventive Services Task Force defines Collaborative Care Model (CCM) as a multicomponent, healthcare system-level intervention that reorganizes the delivery of care so that care managers link PCPs more efficiently with patients and mental health providers to improve evidence-based treatment of mental disorders [32].
CCMs are based on Wagner's Chronic Care Model [85] that recognizes that medical care tends to prioritize the treatment of acute symptoms over the need to properly managing individuals with chronic conditions. Current CCMs are an iteration of the Chronic Care Model that acknowledges mental disorders also require a long-term and systematic approach to foster access and continuity of care to achieve optimal management. Moreover, mental health CCMs emphasize collaboration among a team of mental health providers and PCPs within a practice to effect these changes including coordination of care with specialists and community resources outside of primary care.
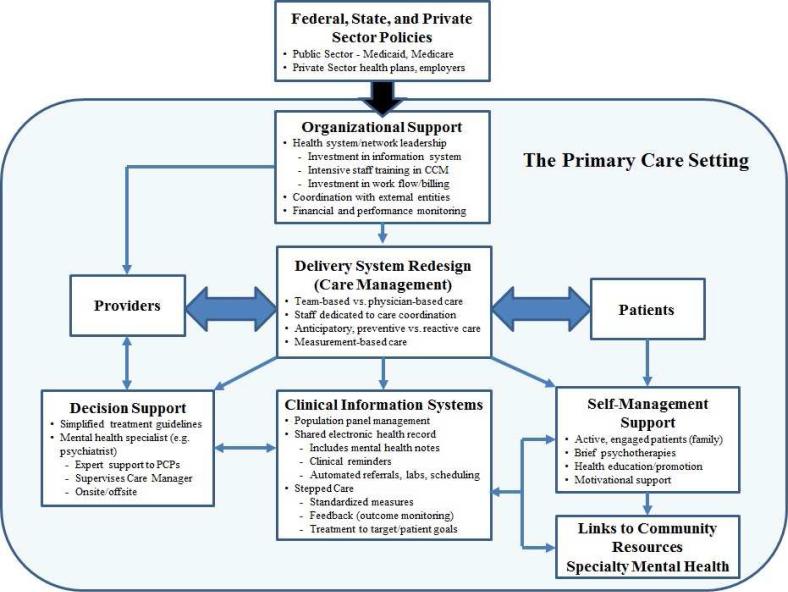
Current CCMs for mental health are commonly identified by six components [7, ••14, 34, ••37, 84] detailed in Figure 1: 1) organizational support from healthcare system leaders for resource allocation and work flow restructuring; 2) delivery system redesign that emphasizes care management; 3) utilization of clinical information systems; 4) provider decision support; 5) patient support for improved self-management of health risks; and 6) linking patients to community resources. These components not only empower providers with improved access to information that supports evidence-based decision making, but also serve to help patients take a more active role in treatment decision-making and managing their health concerns.
Figure 1.
Evidence-based Components of Collaborative Care for Mental Health in Primary Care. Based on the original model articulated in Wagner et al [85].
The basic components of mental health CCMs are predicated by the interrelated principles of population-based care, measurement-based care, and stepped care [7, 35, 46, 85]. Population-based management aims to identify panels of high-risk patients to track through electronic registries created with electronic medical records (EMR). These information systems permit care teams to track the status of patients to anticipate the need for services and target preventive services. Measurement-based practices facilitate this aim by incorporating the use of brief, patient mental health measures such as the PHQ-9 for depression that enable providers to diagnose and monitor patients’ treatment progress over time [8, 46]. CCMs are believed to improve care through the flow of more timely information to PCPs [12, 46]. Care managers facilitate this flow of information between patient and provider by systematically using registries and follow-up contacts with patients to measure mental health symptoms and to track responses and side effects to specific medication dosages, treatment adherence, and service dates that are essential to stepped-care models [7, 8, 12]. This information improves decision-making by improving PCPs’ ability to follow treatment guidelines to achieve more desirable treatment responses (“treat to target” or patient preference) by adjusting/switching medications and treatment with psychosocial treatments while empowering patients with better options to avoid the exacerbation of medical conditions [7, •42].
Care management is a key operational component of CCM healthcare system redesign and represents a significant change from traditional physician-centered, primary care practice [12, 24, 86]. In the CCM practice environment, PCPs are part of a team and are responsible for screening and diagnosis of mental health conditions, prescribing appropriate medications, and referring complex cases to specialty mental health care as needed. PCPs delegate and supervise many treatment tasks to other members of the care team which are coordinated by the care manager. Physicians are indirectly supported by mental health specialists such as psychiatrists who provide decision support for complex cases as well as treatment recommendations [7, 32, 38]. Collaborative communication between these providers and their patients is facilitated by the care manager, usually a nurse, social worker, or other allied health professional who helps patients manage one or more mental health conditions. Care managers also work with PCPs by providing self-management support to patients through the delivery of brief evidence-based psychotherapies, information provision, skills training, or health counseling or, by linking patients to community-based wellness resources [6, 21]. Mental health specialists may be embedded in the practice or based offsite and linked to the practice through phone and the EMR. However, it is the unique role played by care managers that ensures essential information is proactively and systematically collected, monitored, and provided to physicians and patients to facilitate evidence-based decisions that result in better outcomes and lower cost [12].
CCMs for Mental Health Are Evidence-Based Care
Several systematic, meta-analytic reviews were published over the past year which provided robust support for CCMs as an evidenced-based strategy for the management of mental health conditions in primary care settings [14, 37]. Separate and independent analyses were conducted by the Cochrane Collaboration® [34], the U.S. Community Preventive Services Task Force [••37, 13], and leading mental health researchers [5, ••14, 87, 88]. Findings from these reviews when combined with expert qualitative reviews of the literature [7, 12, 38], show that CCMs are more effective than usual care for improving mental health outcomes for periods up to two years.
Of the dozens of studies reviewed in these systematic reviews, the majority of trials examined employed the CCM for integrated care implementation and outcome analyses focused on the treatment of depression. The U.S. Community Preventive Task Force examined outcomes for 69 depression clinical trials and found CCMs were more effective than usual care for improving depression symptoms, treatment adherence, remission and recovery from symptoms, quality of life, and satisfaction with care [••37]. Similarly, the Cochrane Collaboration® review of 79 trials concluded that CCMs were superior to usual care/consultant-liaison models of care for managing depression and anxiety for up to two years with respect to symptom improvement, medication adherence, mental and physical quality of life, and satisfaction with care [34]. A third review of 57 trials also found CCMs to be effective for improving psychiatric symptoms, quality of life, and social role function with results generalized mental health diagnoses of depression, bipolar disorder, anxiety disorders, other diagnoses across both primary and specialty care settings [••14]. Notably, two of the reviews found CCMs to be a good economic value [13, ••14], with results from 30 trials showing CCMs are cost-effective, resulting in little to no net increase in health care costs to healthcare systems. The limited number of trials testing CCMs for the treatment of substance abuse disorders and schizophrenia prohibited conclusions but many have suggested this adaptation is achievable in routine care by emphasizing protocols to coordinate care between practices and specialty mental health and addiction services [••14, 51, 76, 77, 78, 89].
Increasing evidence also demonstrates the effectiveness of multi-condition/cross-diagnosis CCMs that aim to address depression and one or more medical comorbidities [5, 88, ••14]. Results from twelve trials showed that CCMs improved depression outcomes but findings for medical outcomes were indeterminate due to limited reporting of medical outcomes. Studies not included in these reviews subsequently reported that CCMs can concurrently improve management of depression, cardiovascular disease, and diabetes control through medication treatment intensification and self-management support as evidenced by reduced hemoglobin A1c [90], decreased Framingham 10-year CVD risk scores [•69], and LDL cholesterol and systolic blood pressure levels [91, 92]. Moreover, Katon and colleagues reported that the TEAMcare collaborative care intervention was cost-effective for patients diagnosed with depression and either poorly controlled diabetes or heart disease, providing an additional 114 depression free days, 0.335 quality-adjusted life-years (QALYs), and lower mean outpatient costs of $594 per patient at 24 months compared to usual care controls [30]. Collectively, these findings offer compelling reasons to disseminate this evidence-based intervention on a population-level to achieve improvements in healthcare quality and cost.
Issues to Large-scale Translation and Dissemination of CCMs to Routine Care
Systematic, meta-analytic reviews are the foundation of evidence-based care, but translation of these practices from research into routine care is challenging. There have been few rigorous trials of implementation interventions to promote the uptake of evidence-based mental health practices into routine care settings. However, reforms in the American healthcare system, described below, have been a catalyst for literature that examines opportunities, challenges, and new ways of disseminating CCMs as a sustainable model for primary care.
The translation of CCMs for mental health into routine practice holds great promise with the passage of multiple pieces of national healthcare legislation in the U.S. First, the MHPAEA provided Americans with equal insurance coverage for behavioral health and physical health treatment. Second, the ACA created the potential to increase access and quality of care for millions of un- or underinsured Americans [93]. The ACA places a greater priority on the integrated treatment of mental health in primary care and new emphasis on prevention and well-being [21]. Consequently, the ACA provides for a National Prevention, Health Promotion, and Public Health Council to support these health promotion goals and $15 billion-funded Prevention and Public Health Fund to be allocated for states to spend over the next decade.
Patient-centered medical homes (PCMHs) represent one of two ACA mechanisms to improve the coordination and quality of integrated health care. The PCMH model is based on the principles of primary care, patient-centered care, new models of practice (i.e., the CCM), and healthcare payment reform [94]. The six basic CCM components developed in parallel to the PCMH and are the framework with which medical homes implement delivery system redesign to offer patients a more comprehensive, team-based experience that coordinates care across multiple settings and providers [95]. Section 2703 of the ACA provides for a demonstration program for states to enact “health homes” under Medicaid [15] for individuals with chronic mental disorders. Health homes promise to coordinate physical and mental health care through the provision of a variety of services including care management, transitional care from an institution to the community, family education, community linkages, peer-support, and using health information technology to share data between physical and mental health providers [••15]. Under the ACA, implementing health homes for persons with chronic mental health conditions would be reimbursed up to 90% [96].
ACOs are the second mechanism called for by ACA that emphasis integrated care in both Medicare and Medicaid programs as well as the private sector [97]. ACOs are a new payment and care delivery model designed to facilitate care coordination across providers for high-risk patient populations including individuals with mental health conditions. ACOs link financial incentives to the attainment of specific quality improvement targets and reductions in healthcare costs for these specified populations [•22, 97]. ACOs are a response to the current fee-for-service payment model and funding carve-ins and carve-outs that fragmented delivery of mental and physical health services and increased costs. The medical home is one method ACOs can employ to improved integrated care by linking payment to standards of quality care. However, the CCM also represents an evidence-based approach to achieve these aims. Regardless of the approach, improving the quality of care for high-risk populations under the present fee-for-service payment model will be challenging until new pay-for-performance and alternative payment models are implemented [94].
The opportunities afforded by provisions in the ACA must be tempered by the reality that specific aspects pertaining to the implementation of integrated care for primary care settings have yet to be defined for medical homes and ACOs [••15, 16, 24]. Presently, psychiatrists are the only mental health professionals defined by the Centers for Medicare and Medicaid Services (CMS) as participating ACO clinicians, to the exclusion of social workers, psychologists, counselors, and health educators who may serve as care managers in an integrated settings [16, •22]. Furthermore, only one of the 65 quality measures proposed for ACOs pertain to mental health care (depression screening) while no performance incentives or standard billing codes are tied to the provision of prevention or treatment services for mental health needs, nor the delivery of fundamental CCM components such as provider decision support, measurement-based care, self-management support, or registry maintenance [••15, 16, •22].
These trends are inconsistent with mental health parity legislation that calls for essential patient benefits that provide equal treatment for mental and physical needs while ending the fragmentation of care that was created by funding carve-ins and carve-outs [16]. Evidence from Oregon's early implementation of behavioral health parity legislation indicates that patients increasingly chose non-physician behavioral health specialists (e.g., social workers) [18] for mental health care, resulting in little increase in total behavioral treatment costs [27]. Inconsistent fee-for-service billing practices across public and private payers pose a practical barrier to mental health professionals serving as care managers and seeking adequate payment for behavioral health services rendered in primary care [15, 16]. Blended payment models represent a strategy to transition from the fee-for-service model to one which helps practices incentives to the delivery of CCM-consistent care practices that improve outcomes and bundles payments for the start-up and maintenance of implementing these new practices [25]. However, it will be important to build risk adjustment and risk sharing into payment models to avoid incentivizing plans to avoid selecting high-cost patients, including those with mental conditions [20, 25, 26, 29, 93, 97]. CMS, state, national, and professional organizations can play a significant role in developing standards for payers regarding reimbursement rates for specific behavioral services and capability for primary care practices to utilize a broader array of mental health professionals to deliver these services [••15, 16, 25, 26].
Until recently, there have been few examples of organizational strategies that demonstrate how to disseminate CCMs on a large scale [••15, ••48, 56, 98]. Qualitative studies [47, 61, 99, 100], case studies [••48, 51], and qualitative reviews [7, 16, 45] outline the significant challenges to implementing CCMs in primary care. Implementation of integrated care is expensive, presenting a high cost to reorganize existing services, standardize systems of care, adopt an EMR, develop registries, hire new staff, train staff in new treatment protocols, adopt measurement care process, and come to terms with significant role resistance from being a hierarchical, physician-centered practice focused on workflow, to a patient-centered practice [86]. Not only is leadership support important for successful implementation of CCMs, it is also essential to have the commitment of frontline providers and staff. Furthermore, practices need to adapt their business model for care by evaluating utilization and cost data to understand how to achieve performance measures and to identify process costs that should be shared with health payers [26].
Evidence-based implementation interventions are needed to promote uptake of CCMs and improve mental health outcomes, especially in smaller and rural practices [45, 56]. For example, up to 98% of patients with mood disorders receive care from smaller practices, which may not have the tools to fully implement medical homes [33]. For evidence-based practices to reach these patients, evidence-based implementation interventions that leverage outside expertise and local leadership are needed to support community-based providers in delivering these treatments. On such strategy is to employ external facilitators who provide expert consultation to practices in implementing the CCM [55]. Another strategy is for small practices to pool their resources to create regional provider networks, or a “medical neighborhood” that may be anchored by a community hospital or Federally Qualified Health Center (FQHC) [16, 28, 55, 86]. Finally, a randomized trial of an innovative CCM for improving evidence-based depression care for patients served by rural FQHCs [••54] found support for telemedicine-mediated CCM support from a centralized off-site team that was three times as likely to achieve remission in depression than care delivered by an onsite PCP and nurse care manager trained in the CCM protocol. This study highlights the need for diverse CCM implementation strategies to address the heterogeneous needs of practices and patient populations. While the centrally coordinated CCM contracted to offsite providers may seem to go against some clinical researchers’ assertions that onsite integrated care is optimal [53], the off-site providers demonstrated that standardized evidenced treatment delivered by phone can compensate for real world implementation barriers like shortages of mental health providers and the logistical challenge of serving vast rural regions [23, 50].
New large-scale initiatives offer preliminary solutions to the central issue of creating and sustaining a payment model to supported integrated CCM models of care across treatment settings and payers [••15]. DIAMOND (Depression Improvement Across Minnesota, Offering a New Direction) [••48] is a state-level initiative started with the goal of developing a bundled payment model to support the CCM for depression treatment in Minnesota. This initiative utilized a unique approach in which an independent quality improvement organization (the Institute for Clinical Systems Improvement (ICSI)) brokered an arrangement between six private healthcare plans, 22 medical groups, 84 primary care clinics, and the Minnesota Department of Human Services to implement a CCM for depression based on specific goals, and clinical outcomes. A bundled payment model enabled practices to be reimbursed for the costs of implementing and maintaining CCM processes. Implementation was successful and DIAMOND is ongoing because stakeholders were initially engaged to set feasible and shared benchmarks of success, PCPs remained engaged because outcomes were publicized to highlight the success of specific practices, and a business case was made that justified the investment in resources on outcomes shared by multiple stakeholders. Table 1 summarizes similar lessons of implementing each of the CCM components from prior studies. Knowledge gained from state-led initiatives like DIAMOND underscores the need for PCPs and mental health providers to engage healthcare reform initiatives to help negotiate payment policies and performance standards that ensure system redesign interventions like CCMs are sustainable in over time.
Table 1.
Problem-solving Challenges to Implementing Mental Health Collaborative Care in Routine Primary Care Settings. Data from Unutzer and Park [7], Thielke and Vannoy [12], O'Donnell et al [15], O'Donnell et al [22], Whitebird et al [47], Lauren Crain [48], Taylor et al [55], and Kathol et al [99].
| CCM Component | Implementation Step | Challenges | Solutions |
|---|---|---|---|
| Adopt EMR/electronic registries | • High costs to adopt, build, and maintain • Mental health notes separate from medical EMR • Barriers to population registries |
• Seek CMS/HITECH EMR funding • Negotiate EMR costs into bundled payments • Establish payment for measurement-based care • Develop networked “neighborhood” registries |
|
| Clinical Information System | Adopt standardized outcome measures | • Diverse measures and measurement protocols for screening/follow-up |
• Achieving consensus on key mental health and physical tracking measures (embed in EMR) • Standardize frequency of follow-up contacts |
| Negotiate performance measures | • Unknown costs for new workflows • Business model not established |
• Work with practice networks, health agencies, health plans, insurance exchanges to identify common measures to evaluate patient progress, align incentives | |
| Adopt care management/team care | • Lack of staff/provider buy-in • Physician centric culture |
• Physician champion aligns realignment with values • External facilitation to support transition |
|
| Delivery System Redesign | Develop standardized protocols for diagnosis, follow-up measures, stepped-care, referrals Specify care management protocols |
• Cost of training and changing workflow • Poor coordination between team • Role ambiguity, provider competing demands • Provider competing demands |
• Establish blended payments to general and specific care coordination procedures • Specify work roles and methods to communicate patient information, referrals, urgent consultations • Physical colocation of medical and mental health staff |
| Identify MH diagnoses for treatment and who delivers specific treatments | • Supply of interdisciplinary behavioral health staff • Multiple patient comorbidities |
• Negotiate reimbursement and competencies for specified professionals (licensure, credentials, training, skills) • States incentivize interdisciplinary training programs • Negotiate patient goals and treat to “target” |
|
| Engage patients in care | • Practice is patient flow vs. patient-centered | • Measure satisfaction, emphasis feedback, and indicators of shared decision-making in EMR/registries | |
| Self-Management Support | Identify brief evidence-based treatments | • Reimbursement for training/supervision • Practice treatment capacity |
• Negotiations for bundled payments for self-management • Establish protocol length, visits, & stepped-care protocol |
| Implement health promotion counseling and who to deliver | • Focus on single MH or disease condition • Lack of reimbursement for wellness |
• Have cross-disease focus • Available to all patients • Negotiate reimbursement, performance measures |
|
| Referrals to community/specialty care | • Patient and provider stigma • Poor referral uptake by patients • Lack of follow-up |
• Train staff to de-stigmatize MH conditions • Offer onsite or e-health mediated treated when possible • Establish follow-up procedures for community referrals |
|
| Establish space/delivery mode | • Inadequate space/staff | • Contract self-management to phone/e-health provider | |
| Train staff/physicians in guidelines and measurement based care |
• Stigma/negative attitude towards MH • Lack of training in MH diagnose/care |
• Allocate funds for staff/provider training • Train in diagnosis and screening • Create simplified guideline supports for stepped-care medication, psychosocial, and referral strategies |
|
| Provider Decision Support | Establish mental health specialist services | • Undefined role and reimbursement |
• Specify contractual obligations for MH panel and care manager supervision, consultations, facilitating referrals • Decide if colocated or offsite |
| Define care manager functions | • Capitated payments do not cover care management | • Reimbursement based on care management functions of diagnosis, tracking, medication support, brief psycho-education counseling, prompting physicians for treatment changes, relapse prevention, registry updates | |
| Community Linkages | Creating network of community resources (specialty mental health transportation, housing, wellness, , employment) | • ACO serving wide geographic regions or dense urban settings lack sufficient community connections • Poor patient uptake of specialty mental health referrals |
•Local practices create network or health “neighborhood” directories of local resources and providers • Develop links with local specialty mental health resources/providers for warm hand-offs |
| Ensure leadership buy-in and support | •Integration from health plan vs. practice • Poor relationship between leaders and frontline providers and staff |
•Align CCM restructuring with practice values • Consult with practice facilitator |
|
| Build Leadership and Organizational Support | Establish priority for system redesign with CCM components | •Lack of priority for measurement based care • Inertia to redesign workflows, procedures, and billing processes |
• Identify physician and mental health champions |
| Create a sustainable business model | •Lack of financial business model • Financial costs for investing in CCM components and maintenance • Unbillable activities for new provider types, services, and processes of care for • Lack of stakeholder input |
•Achieve consensus on the value of CCM with regional and state healthcare stakeholders, key tracking outcomes • Assess the types of providers, location/size of practices, and the intervention components to deliver • Measure new costs to understand new financial model • Establish working group of stakeholders (e.g., providers, plans, employers, patients) to define performance outcomes • Propose and negotiate a reimbursement model involving neutral 3rd party to move from fee-for-service to bundled payments model that covers costs of CCM redesign |
|
Conclusions and Future Directions
Healthcare reform efforts in America and around the world have drawn attention to CCM for mental health as a strategy to deliver integrated care in primary care settings. The CCM applies concepts of population-based care, measurement-based care, and stepped-care to systematically track patient status to support improved patient and provider treatment decisions. The six CCM components represent evidenced-based practices which have proven more effective than usual care for improving mental health outcomes across settings and diagnoses, with little to no net increase in healthcare costs [13, ••14, 34, ••37]. Further research is needed to more effectively implement CCMs in routine practice, notably by identifying and reducing organizational and financial barriers within emerging health care reform initiatives, and by developing payment models to enhance CCM uptake.
The CCM has potential to be an effective strategy to support U.S. healthcare reforms but practical issues to disseminating the model into routine care have yet to be resolved [••48]. Financial and organizational incentives must be aligned so that public and private health plans have the capacity to adopt and sustain the model [•22, 26]. Evidence in support of CCM effectiveness was based on large, closed health care systems or staff-model health plans whereas most Americans with mental disorders are managed in solo or small practices comprising of fewer than 10 providers [33, ••54]. Small primary care practices and FQHCs need new models of payment to support the costs to implement measurement-based tools like EMRs and electronic registries as well delivery processes of care like decision and self-management support [56]. Further research is needed to evaluate centralized e-health technologies to create shared efficiencies through networked practices or “health neighborhoods” [36, 86]. It will also be necessary to negotiate changes to the current fee-for-service and service carve-outs to enable mental health providers to support PCPs in carrying out CCM care management and mental health specialist roles [••15]. Collaborative demonstration projects like the DIAMOND initiative show promise that multiple stakeholders can work out bundled payment arrangements that help practices cover some of the costs of implementing and carrying out CCMs [••15, 25, 48]. Finally, additional research is needed to understand the finances of these arrangements and performance standards that guide reimbursement for achieving quality and cost savings.
Acknowledgments
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development [HSRD IIR 10-340], the VA Health Services Research and Development Center for Organization, Leadership, and Management Research (COLMR), the National Institute of Mental Health [RO1 MH 79994 and R34 MH 74509], and the University of Michigan Comprehensive Depression Center (Director's Innovation Fund). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
David E. Goodrich declares that he has no conflict of interest.
Amy M. Kilbourne has received consulting fees from Kaiser Permanente, research funding from Agency for Healthcare Research and Quality and National Institute of Mental Health, and royalties from New Harbinger.
Kristina M. Nord declares that she has no conflict of interest.
Mark S. Bauer has received royalties from Springer Publishing Company and New Harbinger. Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest have been highlighted as:
• Of importance
•• Of outstanding importance
- 1.The global burden of disease: 2004 update. World health Organization; Geneva: 2008. [Google Scholar]
- 2.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. 2008;29:115–29. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- 3.Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–50. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baumeister H, Hutter N. Collaborative care for depression in medically ill patients. Curr Opin Psychiatry. 2012;25(5):405–14. doi: 10.1097/YCO.0b013e3283556c63. [DOI] [PubMed] [Google Scholar]
- 6.Auxier A, Runyan C, Mullin D, Menderhall T, Young J, Kessler R. Behavioral health referrals and treatment initiation rates in integrated primary care: a Collaborative Care Research Network study. Translational Behavioral Medicine. 2012;2:337–44. doi: 10.1007/s13142-012-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unutzer J, Park M. Strategies to improve the management of depression in primary care. Prim Care. 2012;39(2):415–31. doi: 10.1016/j.pop.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pence BW, O'Donnell JK, Gaynes BN. The depression treatment cascade in primary care: a public health perspective. Curr Psychiatry Rep. 2012;14(4):328–35. doi: 10.1007/s11920-012-0274-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reilly S, Planner C, Hann M, Reeves D, Nazareth I, Lester H. The role of primary care in service provision for people with severe mental illness in the United kingdom. PLoS One. 2012;7(5):e36468. doi: 10.1371/journal.pone.0036468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glozier N, Davenport T, Hickie IB. Identification and management of depression in Australian primary care and access to specialist mental health care. Psychiatr Serv. 2012;63(12):1247–51. doi: 10.1176/appi.ps.201200017. [DOI] [PubMed] [Google Scholar]
- 11.Cunningham PJ. Beyond parity: primary care physicians’ perspectives on access to mental health care. Health Aff (Millwood) 2009;28(3):w490–501. doi: 10.1377/hlthaff.28.3.w490. [DOI] [PubMed] [Google Scholar]
- 12.Thielke S, Vannoy S, Unutzer J. Integrating mental health and primary care. Primary Care; Clinics in Office Practice. 2007;34:571–92. vii. doi: 10.1016/j.pop.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Jacob V, Chattopadhyay SK, Sipe TA, Thota AB, Byard GJ, Chapman DP, et al. Economics of collaborative care for management of depressive disorders: a community guide systematic review. Am J Prev Med. 2012;42(5):539–49. doi: 10.1016/j.amepre.2012.01.011. [DOI] [PubMed] [Google Scholar]
- •• 14.Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169(8):790–804. doi: 10.1176/appi.ajp.2012.11111616. [A systematic, meta-analytical review that compared CCM for treatment of mental disorders over usual care based on review of 57 trials that revealed the model to be effective for improving mental outcomes in a cost-efficient manner across treatment settings and mental health and medical diagnoses.] [DOI] [PubMed] [Google Scholar]
- •• 15.O'Donnell AN, Williams M, Kilbourne AM. Overcoming roadblocks: current and emerging reimbursement strategies for integrated mental health services in primary care. J Gen Intern Med. 2013 doi: 10.1007/s11606-013-2496-z. doi: 10.1007/s11606-013-2496-z. [Provider and practice reimbursement will be a practical challenge to implementing the collaborative care for mental health in primary care settings. This paper provides a critical analysis of challenges and opportunities to reimbursing CCM compenents under the current fee-for-service reimbursement ystem and presents the argument that employers, health plans, and healthcare organizations will need to work together to establish a bundled payment model to support the implementation of CCMs in the near future.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown-Levey SM, Miller BF, deGruy FV. Behavioral health integration: an essential element of population-based healthcare redesign. Translational Behavioral Medicine. 2012;2:364–71. doi: 10.1007/s13142-012-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shim R, Rust G. Primary Care, Behavioral Health, and Public Health: Partners in Reducing Mental Health Stigma. Am J Public Health. 2013 doi: 10.2105/AJPH.2013.301214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McConnell KJ, Gast SH, McFarland BH. The effect of comprehensive behavioral health parity on choice of provider. Med Care. 2012;50(6):527–33. doi: 10.1097/MLR.0b013e318245a60f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calonge N. Clinical and community prevention and treatment service for depression: a whole greater than the sum of its parts. Am J Prev Med. 2012;42(5):556–7. doi: 10.1016/j.amepre.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Garfield RL, Druss BG. Health reform, health insurance, and mental health care. Am J Psychiatry. 2012;169(7):675–7. doi: 10.1176/appi.ajp.2012.12040506. [DOI] [PubMed] [Google Scholar]
- 21.Shim RS, Koplan C, Langheim FJ, Manseau M, Oleskey C, Powers RA, et al. Health care reform and integrated care: a golden opportunity for preventive psychiatry. Psychiatr Serv. 2012;63(12):1231–3. doi: 10.1176/appi.ps.201200072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • 22.O'Donnell AN, Williams BC, Eisenberg D, Kilbourne AM. Mental health in ACOs: missed opportunities and low hanging fruit. Am J Manag Care. 2013;19(3):180–4. [This paper examines the rationale and need for better integrating mental health into accountable care organizations using the collaborative care model. Mental health care is not well defined under the Medicare Shared Saving Program and the paper succintly summarizes the necessary financial and organizational incentives that must be defined in order for healthcare organizations to successfully implement integrated mental health care in primary care.] [PMC free article] [PubMed] [Google Scholar]
- 23.Simon GE, Ludman EJ. Should mental health interventions be locally grown or factory-farmed? Am J Psychiatry. 2013;170(4):362–5. doi: 10.1176/appi.ajp.2013.13010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Massa I, Miller BF, Kessler R. Collaboration between NCQA patient-centered medical homes and specialty behavioral health and medical services. Translational Behavioral Medicine. 2012;2:332–6. doi: 10.1007/s13142-012-0153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bao Y, Casalino LP, Ettner SL, Bruce ML, Solberg LI, Unutzer J. Designing payment for Collaborative Care for Depression in primary care. Health Serv Res. 2011;46(5):1436–51. doi: 10.1111/j.1475-6773.2011.01272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unutzer J, Chan YF, Hafer E, Knaster J, Shields A, Powers D, et al. Quality improvement with pay-for-performance incentives in integrated behavioral health care. Am J Public Health. 2012;102(6):e41–5. doi: 10.2105/AJPH.2011.300555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McConnell KJ, Gast SH, Ridgely MS, Wallace N, Jacuzzi N, Rieckmann T, et al. Behavioral health insurance parity: does Oregon's experience presage the national experience with the Mental Health Parity and Addiction Equity Act? Am J Psychiatry. 2012;169(1):31–8. doi: 10.1176/appi.ajp.2011.11020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gourevitch MN, Cannell T, Boufford JI, Summers C. The challenge of attribution: responsibility for population health in the context of accountable care. Am J Prev Med. 2012;42(6 Suppl 2):S180–3. doi: 10.1016/j.amepre.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barry CL, Weiner JP, Lemke K, Busch SH. Risk adjustment in health insurance exchanges for individuals with mental illness. Am J Psychiatry. 2012;169(7):704–9. doi: 10.1176/appi.ajp.2012.11071044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katon W, Russo J, Lin EH, Schmittdiel J, Ciechanowski P, Ludman E, et al. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Archives of General Psychiatry. 2012;69(5):506–14. doi: 10.1001/archgenpsychiatry.2011.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 32.Community Preventive Services Task F. Recommendation from the community preventive services task force for use of collaborative care for the management of depressive disorders. Am J Prev Med. 2012;42(5):521–4. doi: 10.1016/j.amepre.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 33.Bauer MS, Leader D, Un H, Lai Z, Kilbourne AM. Primary care and behavioral health practice size: the challenge for health care reform. Med Care. 2012;50(10):843–8. doi: 10.1097/MLR.0b013e31825f2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Katon W. Collaborative depression care models: from development to dissemination. Am J Prev Med. 2012;42(5):550–2. doi: 10.1016/j.amepre.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 36.Compton MT. Systemic organizational change for the collaborative care approach to managing depressive disorders. Am J Prev Med. 2012;42(5):553–5. doi: 10.1016/j.amepre.2012.01.016. [DOI] [PubMed] [Google Scholar]
- •• 37.Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42(5):525–38. doi: 10.1016/j.amepre.2012.01.019. [A large systematic review of 69 randomized controlled trials testing the effectiveness of CCM vs. usual care to improve depression outcomes among 24,000 adult treated for depression in primary care. Findings from the meta-analytical review found CCMs are significantly more effective in improving depressive symptoms, adherence to treatment, remission and recovery from symptoms, quality of life and functional status, and satisfaction of care than usual treatment across a range of populations, settings, and organizations.] [DOI] [PubMed] [Google Scholar]
- 38.Cerimele JM, Katon WJ, Sharma V, Sederer LI. Delivering psychiatric services in primary-care setting. Mt Sinai J Med. 2012;79(4):481–9. [Google Scholar]
- 39.Kilbourne AM, Goodrich DE, O'Donnell AN, Miller CJ. Integrating bipolar disorder management in primary care. Curr Psychiatry Rep. 2012 doi: 10.1007/s11920-012-0325-4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kilbourne AM, Goodrich DE, Lai Z, Clogston J, Waxmonsky J, Bauer MS. Life Goals Collaborative Care for patients with bipolar disorder and cardiovascular disease risk. Psychiatr Serv. 2012;63(12):1234–8. doi: 10.1176/appi.ps.201100528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • 41.Kilbourne AM, Goodrich DE, Lai Z, Post EP, Schumacher K, Nord KM, et al. Randomized controlled trial to reduce cardiovascular disease risk for patients with bipolar disorders: the Self-management Adressing Heart Risk Trial (SMAHRT). J Clin Psychiatry. 2013 doi: 10.4088/JCP.12m08082. In press. [A small randomized controlled trial that demonstrates the feasibility of implementing a cross diagnosis collaborative care model in a staff model integrated system with the aim of managing cardiometabolic and psychiatric risk factors among Veterans diagnosed with bipolar disorder. Results showed that manic symptoms and blood pressure were reduced at two years in the intervention arm. However, results need to be replicated in a larger multi-practice trial which includes greater minority participation and a cost-effectiveness analysis.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- • 42.Kilbourne AM, Goodrich DE, O'Donnell AN, Miller CJ. Integrating bipolar disorder management in primary care. Curr Psychiatry Rep. 2012;14(6):687–95. doi: 10.1007/s11920-012-0325-4. [A succinct overview that summarizes the challenges of diagnosing and treating bipolar disorders in primary care settings, a mental health condition that is frequently misdiagnosed that increased treatment costs and undermines long-term patient outcomes. Emphasis is placed on explaining how this treatment could be delivered using the collaborative care model as well as research issues that need to be addressed to help primary care providers provider guideline concordant care.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kilbourne AM, Greenwald DE, Bauer MS, Charns MP, Yano EM. Mental health provider perspectives regarding integrated medical care for patients with serious mental illness. Adm Policy Ment Health. 2012;39(6):448–57. doi: 10.1007/s10488-011-0365-9. [DOI] [PubMed] [Google Scholar]
- 44.Kilbourne AM, Li D, Lai Z, Waxmonsky J, Ketter T. Pilot randomized trial of a cross-diagnosis collaborative care program for patients with mood disorders. Depress Anxiety. 2013;30(2):116–22. doi: 10.1002/da.22003. [DOI] [PubMed] [Google Scholar]
- 45.Miller BF, Druss B. The role of family physicians in mental health care delivery in the United States: implications for health reform. J Am Board Fam Med. 2013;26(2):111–3. doi: 10.3122/jabfm.2013.02.120346. [DOI] [PubMed] [Google Scholar]
- 46.Kurian BT, Grannemann B, Trivedi MH. Feasible evidence-based strategies to manage depression in primary care. Curr Psychiatry Rep. 2012;14(4):370–5. doi: 10.1007/s11920-012-0290-y. [DOI] [PubMed] [Google Scholar]
- 47.Whitebird RR, Solberg LI, Margolis KL, Asche SE, Trangle MA, Wineman AP. Barriers to Improving Primary Care of Depression: Perspectives of Medical Group Leaders. Qual Health Res. 2013 doi: 10.1177/1049732313482399. [DOI] [PubMed] [Google Scholar]
- •• 48.Lauren Crain A, Solberg LI, Unutzer J, Ohnsorg KA, Maciosek MV, Whitebird RR, et al. Designing and Implementing Research on a Statewide Quality Improvement Initiative: The DIAMOND Study and Initiative. Med Care. 2012 doi: 10.1097/MLR.0b013e318249d8a4. [This paper providers an overview of the Depression Improvement Across Minnesota, Offering a New Direction (DIAMOND) Initiative which aims to test the implementation of an evidence-based, collaborative care model for depression management in primary care using a partnership with employers, health plans, providers, patients, and researchers to develop a financially feasible strategy to implement and sustain CCMs in real world conditions.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hay JW, Katon WJ, Ell K, Lee PJ, Guterman JJ. Cost-effectiveness analysis of collaborative care management of major depression among low-income, predominantly Hispanics with diabetes. Value Health. 2012;15(2):249–54. doi: 10.1016/j.jval.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xierali IM, Tong ST, Petterson SM, Puffer JC, Phillips RL, Jr., Bazemore AW. Family physicians are essential for mental health care delivery. J Am Board Fam Med. 2013;26(2):114–5. doi: 10.3122/jabfm.2013.02.120219. [DOI] [PubMed] [Google Scholar]
- 51.Young J, Gilwee J, Holman M, Messier R, Kelly M, Kessler R. Mental health, substance abuse, and health behavior intervention as part of the patient-centered medical home: a case study. Translational Behavioral Medicine. 2012;2:345–54. doi: 10.1007/s13142-012-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Culpepper L. Does screening for depression in primary care improve outcome? Curr Psychiatry Rep. 2012;14(4):345–52. doi: 10.1007/s11920-012-0275-x. [DOI] [PubMed] [Google Scholar]
- 53.Kessler R. Mental health care treatment initiation when mental health services are incorporated into primary care practice. J Am Board Fam Med. 2012;25(2):255–9. doi: 10.3122/jabfm.2012.02.100125. [DOI] [PubMed] [Google Scholar]
- •• 54.Fortney JC, Pyne JM, Mouden SB, Mittal D, Hudson TJ, Schroeder GW, et al. Practice-based versus telemedicine-based collaborative care for depression in rural federally qualified health centers: a pragmatic randomized comparative effectiveness trial. Am J Psychiatry. 2013;170(4):414–25. doi: 10.1176/appi.ajp.2012.12050696. [This pragrmatic, multi-site randomized trial demonstrated that a collaborative care program for mental health treatment could be more effectively implemented by a centralized mental health team than locally trained primary care providers. This study provides preliminary evidenced that new communication technologies may allow for integrated care to be effectively delivered by offsite mental health teams rather than being delivered by practice personnel who may be less likely to implement the CCM components with fidelity. Findings are particularly salient to networks of small primary care practices and solo practitioners as well as FQHQs serving rural populations where trained mental health staff may unavaible to support CCM delivery.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taylor EF, Machta RM, Meyers DS, Genevro J, Peikes DN. Enhancing the primary care team to provide redesigned care: the roles of practice facilitators and care managers. Ann Fam Med. 2013;11(1):80–3. doi: 10.1370/afm.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hunt JB, Curran G, Kramer T, Mouden S, Ward-Jones S, Owen R, et al. Partnership for implementation of evidence-based mental health practices in rural federally qualified health centers: theory and methods. Prog Community Health Partnersh. 2012;6(3):389–98. doi: 10.1353/cpr.2012.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cummings JR, Wen H, Druss BG. Improving access to mental health services for youth in the United States. JAMA. 2013;309(6):553–4. doi: 10.1001/jama.2013.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson-Lawrence VD, Szymanski BR, Zivin K, McCarthy JF, Valenstein M, Pfeiffer PN. Primary care-mental health integration programs in the veterans affairs health system serve a different patient population than specialty mental health clinics. Prim Care Companion CNS Disord. 2012;14(3) doi: 10.4088/PCC.11m01286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bocker E, Glasser M, Nielsen K, Weidenbacher-Hoper V. Rural older adults’ mental health: status and challenges in care delivery. Rural Remote Health. 2012;12:2199. [PubMed] [Google Scholar]
- 60.Jonas DE, Mansfield AJ, Curtis P, Gilmore JH, Watson LC, Brode S, et al. Identifying priorities for patient-centered outcomes research for serious mental illness. Psychiatr Serv. 2012;63(11):1125–30. doi: 10.1176/appi.ps.201100369. [DOI] [PubMed] [Google Scholar]
- 61.Loeb DF, Bayliss EA, Binswanger IA, Candrian C, deGruy FV. Primary care physician perceptions on caring for complex patients with medical and mental illness. J Gen Intern Med. 2012;27(8):945–52. doi: 10.1007/s11606-012-2005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kaufman EA, McDonell MG, Cristofalo MA, Ries RK. Exploring barriers to primary care for patients with severe mental illness: frontline patient and provider accounts. Issues Ment Health Nurs. 2012;33(3):172–80. doi: 10.3109/01612840.2011.638415. [DOI] [PubMed] [Google Scholar]
- 63.Scott D, Happell B. Utilization and perceptions of primary health care services in Australian adults with mental illness. Popul Health Manag. 2013;16:18. doi: 10.1089/pop.2012.0018. [DOI] [PubMed] [Google Scholar]
- 64.Verhaak PF, van Dijk CE, Nuijen J, Verheij RA, Schellevis FG. Mental health care as delivered by Dutch general practitioners between 2004 and 2008. Scand J Prim Health Care. 2012;30(3):156–62. doi: 10.3109/02813432.2012.688707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Currid TJ, Turner A, Bellefontaine N, Spada MM. Mental health issues in primary care: implementing policies in practice. Br J Community Nurs. 2012;17(1):21–4. 6. doi: 10.12968/bjcn.2012.17.1.21. [DOI] [PubMed] [Google Scholar]
- 66.Hardy S, Gray R. Is the use of an invitation letter effective in prompting patients with severe mental illness to attend a primary care physical health check? Prim Health Care Res Dev. 2012;13(4):347–52. doi: 10.1017/S1463423612000023. [DOI] [PubMed] [Google Scholar]
- 67.Hardy S, Thomas B. Mental and physical health comordibity: political imperatives and practice implications. Int J Ment Health Nurs. 2012;21(3):289–98. doi: 10.1111/j.1447-0349.2012.00823.x. [DOI] [PubMed] [Google Scholar]
- 68.Rodrigo A, Foo L, Majoor J. Have Primary Mental Health Teams lived up to their expectations? Australas Psychiatry. 2013;21(2):127–30. doi: 10.1177/1039856212475324. [DOI] [PubMed] [Google Scholar]
- • 69.Morgan MA, Coates MJ, Dunbar JA, Reddy P, Schlicht K, Fuller J. The TrueBlue model of collaborative care using practice nurses as case managers for depression alongside diabetes or heart disease: a randomised trial. BMJ Open. 2013;3(1) doi: 10.1136/bmjopen-2012-002171. [An exemplary cross-diagnosis trial conducted outside the U.S. healthcare system that tests the collaborative care model for mental health among Australian patients diagnosed with depression and comorbid health conditions. The study demonstrates the feasibility of using nurses to promote treatment intensification for more than one health condition and delivery of wellness self-management for health behavior change to reduce mental and physical risk factors.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schlicht K, Morgan MA, Fuller J, Coates MJ, Dunbar JA. Safety and acceptability of practice-nurse-managed care of depression in patients with diabetes or heart disease in the Australian TrueBlue study. BMJ Open. 2013;3(4) doi: 10.1136/bmjopen-2012-002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hunter CL, Goodie JL. Behavioral health in the Department of Defense patient-centered medical home: history, fianance, policy, work force development, and evaluation. Translational Behavioral Medicine. 2012;2:355–63. doi: 10.1007/s13142-012-0142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huijbregts KM, de Jong FJ, van Marwijk HW, Beekman AT, Ader HJ, Hakkaart-van Roijen L, et al. A target-driven collaborative care model for Major Depressive Disorder is effective in primary care in the Netherlands. A randomized clinical trial from the depression initiative. J Affect Disord. 2013;146(3):328–37. doi: 10.1016/j.jad.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 73.Vlasveld MC, van der Feltz-Cornelis CM, Ader HJ, Anema JR, Hoedeman R, van Mechelen W, et al. Collaborative care for sick-listed workers with major depressive disorder: a randomised controlled trial from the Netherlands Depression Initiative aimed at return to work and depressive symptoms. Occup Environ Med. 2013;70(4):223–30. doi: 10.1136/oemed-2012-100793. [DOI] [PubMed] [Google Scholar]
- 74.Berghofer A, Hartwich A, Bauer M, Unutzer J, Willich SN, Pfennig A. Efficacy of a systematic depression management program in high utilizers of primary care: a randomized trial. BMC Health Serv Res. 2012;12:298. doi: 10.1186/1472-6963-12-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cooper LA, Ghods Dinoso BK, Ford DE, Roter DL, Primm AB, Larson SM, et al. Comparative effectiveness of standard versus patient-centered collaborative care interventions for depression among African Americans in primary care settings: the BRIDGE Study. Health Serv Res. 2013;48(1):150–74. doi: 10.1111/j.1475-6773.2012.01435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bray JW, Zarkin GA, Hinde JM, Mills MJ. Costs of alcohol screening and brief intervention in medical settings: a review of the literature. J Stud Alcohol Drugs. 2012;73(6):911–9. doi: 10.15288/jsad.2012.73.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pating DR, Miller MM, Goplerud E, Martin J, Ziedonis DM. New systems of care for substance use disorders: treatment, finance, and technology under health care reform. Psychiatr Clin North Am. 2012;35(2):327–56. doi: 10.1016/j.psc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 78.Field CA, Klimas J, Barry J, Bury G, Keenan E, Lyons S, et al. Alcohol screening and brief intervention among drug users in primary care: a discussion paper. Ir J Med Sci. 2012;181(2):165–70. doi: 10.1007/s11845-011-0748-7. [DOI] [PubMed] [Google Scholar]
- 79.Gill JM, Chen YX, Grimes A, Diamond JJ, Lieberman MI, Klinkman MS. Electronic clinical decision support for management of depression in primary care: a prospective cohort study. Prim Care Companion CNS Disord. 2012;14(1) doi: 10.4088/PCC.11m01191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gill JM, Chen YX, Grimes A, Klinkman MS. Using electronic health record-based tools to screen for bipolar disorder in primary care patients with depression. J Am Board Fam Med. 2012;25(3):283–90. doi: 10.3122/jabfm.2012.03.110217. [DOI] [PubMed] [Google Scholar]
- 81.McIntyre RS, Rosenbluth M, Ramasubbu R, Bond DJ, Taylor VH, Beaulieu S, et al. Managing medical and psychiatric comorbidity in individuals with major depressive disorder and bipolar disorder. Ann Clin Psychiatry. 2012;24(2):163–9. [PubMed] [Google Scholar]
- 82.McIntyre RS, Alsuwaidan M, Goldstein BI, Taylor VH, Schaffer A, Beaulieu S, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid metabolic disorders. Ann Clin Psychiatry. 2012;24(1):69–81. [PubMed] [Google Scholar]
- 83.Malhi GS, Bargh DM, Cashman E, Frye MA, Gitlin M. The clinical management of bipolar disorder complexity using a stratified model. Bipolar Disorders. 2012;14(Suppl 2):66–89. doi: 10.1111/j.1399-5618.2012.00993.x. [DOI] [PubMed] [Google Scholar]
- 84.Collins C, Hewson DL, Munger R, Wade T. Evolving models of behavioral health integration in primary care. Milbank Memorial Fund; New York, NY: 2010. [Google Scholar]
- 85.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 86.Nutting PA, Crabtree BF, McDaniel RR. Small primary care practices face four hurdles--including a physician-centric mind-set--in becoming medical homes. Health Aff (Millwood) 2012;31(11):2417–22. doi: 10.1377/hlthaff.2011.0974. [DOI] [PubMed] [Google Scholar]
- 87.Ekers D, Murphy R, Archer J, Ebenezer C, Kemp D, Gilbody S. Nurse-delivered collaborative care for depression and long-term physical conditions: A systematic review and meta-analysis. J Affect Disord. 2013 doi: 10.1016/j.jad.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 88.Watson L, Amick HR, Gaynes BN, Brownley KA, Thaker S, Viswanathan M, et al. Comparative Effectiveness Review No. 75. (Prepared by RTI International, University of North Carolina Evidence-based Practice Center under Contract No. 290-2007-10056-I.) Agency for Healthcare Research and Quality; Rockville, MD: Aug, 2012. Practice-based interventions addressing concomitant depression and chronic medical conditions in the primary care setting. Report No.: AHRQ Publication No. 12-EHC106-EF. [PubMed] [Google Scholar]
- 89.Alford DP, LaBelle CT, Kretsch N, Bergeron A, Winter M, Botticelli M, et al. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171(5):425–31. doi: 10.1001/archinternmed.2010.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10(1):15–22. doi: 10.1370/afm.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin EH, Von Korff M, Ciechanowski P, Peterson D, Ludman EJ, Rutter CM, et al. Treatment adjustment and medication adherence for complex patients with diabetes, heart disease, and depression: a randomized controlled trial. Ann Fam Med. 2012;10(1):6–14. doi: 10.1370/afm.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Barry CL, Huskamp HA. Moving beyond parity--mental health and addiction care under the ACA. N Engl J Med. 2011;365(11):973–5. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rittenhouse DR, Shortell SM. The patient-centered medical home: will it stand the test of health reform? JAMA. 2009;301(19):2038–40. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- 95.Amiel JM, Pincus HA. The medical home model: new opportunities for psychiatric services in the United States. Curr Opin Psychiatry. 2011;24(6):562–8. doi: 10.1097/YCO.0b013e32834baa97. [DOI] [PubMed] [Google Scholar]
- 96.Mann C. In: Re: Health Homes for Enrollees with Chronic Conditions (section 2703 of the Affordable Care Act) Centers for Medicare & Medicaid Services, editor. Department of Health & Human Services; Baltimore, MD: 2010. [Google Scholar]
- 97.Lewis VA, Larson BK, McClurg AB, Boswell RG, Fisher ES. The promise and peril of accountable care for vulnerable populations: a framework for overcoming obstacles. Health Aff (Millwood) 2012;31(8):1777–85. doi: 10.1377/hlthaff.2012.0490. [DOI] [PubMed] [Google Scholar]
- 98.Williams JW., Jr Integrative care: what the research shows. N C Med J. 2012;73(3):205–6. [PubMed] [Google Scholar]
- 99.Kathol RG, Butler M, McAlpine DD, Kane RL. Barriers to physical and mental condition integrated service delivery. Psychosom Med. 2010;72(6):511–8. doi: 10.1097/PSY.0b013e3181e2c4a0. [DOI] [PubMed] [Google Scholar]
- 100.Scott D, Happell B. Utilization and Perceptions of Primary Health Care Services in Australian Adults with Mental Illness. Popul Health Manag. 2012 doi: 10.1089/pop.2012.0018. [DOI] [PubMed] [Google Scholar]