Abstract
Increasing social, economic, and political pressures to reform the American approach to medical care makes change likely. A fundamental premise of predictive health is that it should be cheaper (at least per person life year), more efficient, and have a greater return on the investment of keeping people healthy as opposed to waiting for disease to intervene. The Emory Predictive Health and Society Strategic Initiative and its Center for Health Discovery and Well Being have embarked on a program to define health to the extent that modern science permits in the context of the entire human experience, to identify measurable variables that describe and predict a healthy state, and to use that knowledge to design health-focused interventions that are affordable and effective. Initial results from a study of a randomly selected “essentially healthy” cohort, utilizing extensive assessments and a health partner, are promising. Studies of healthy aging over the entire life spectrum promise valuable normative data for age-specific assessments of health and the setting of realistic health goals.
Keywords: Predictive health, health promotion, assessment
INTRODUCTION
If you Googled the topic “health care reform,” on June 1, 2009, you would have retrieved 1,700,000 hits. If you are even a casual reader of the popular press, you are aware of a burgeoning interest in health care and a rising public realization that health care in the United States is not sustainable (and perhaps should not be) in its present form.
We pay too much for health care. Whether normalized to gross domestic product or population number, we spend close to twice as much on health care as most other developed countries. But those extra dollars do not buy better health, at least at a population level. Life expectancy in the United States is less than in most of the countries that pay less for health care, and a calculated value of “mortality amenable to health care” showed the U.S. leading the pack in 2002–20031. There are close to 50 million Americans without health insurance2. This does not mean that they have no access to health care. Rather, they get charity care, mostly in emergency rooms, for acute exacerbations of advanced chronic disease that could have been prevented with effective, timely health care. This is expensive care with less than optimal results.
High-throughput science (genomics, proteomics, metabolomics, etc.), molecular imaging, regenerative medicine, and astounding advances in computational sciences appear to provide powerful tools for understanding human biology and marshalling that knowledge to benefit human health. We are headed that way,3,4 but we’re not there yet5 and we can’t afford to wait. Advances in science and technology will make extraordinary things possible, but politics, social attitudes, and economics will dictate the pace and direction of change.
PREDICTIVE HEALTH: THE CONCEPT
It has been observed that America has a “disease care non-system” rather than a health care system.6,7,8 A number of terms have been used to refer to a new way to focus energies and resources. Most descriptors, for obscure reasons, begin with “P” (eg, predictive, prospective, personalized, participatory).9 We have chosen the term “predictive health” to emphasize prediction as opposed to diagnosis, and health as opposed to disease.10 The elements of the concept are:
Health should be positively defined in the context of the entire human experience. Health is not just the absence of disease (a default condition), and it includes a host of interacting factors not limited to biology.11
There are fundamental processes that can be measured that are not disease specific, but rather define the biology of health. Deviations in these processes are warning signs of “unhealth,” and presage even the earliest evidence for altered organ structure or function, i.e., disease.
A focus of effort and resources on healthy people can: a) identify the most robust predictors of health; b) identify the most effective interventions that optimize quality and duration of health; and c) translate that knowledge to populations in a manner that is efficient and cost effective.
ROLE OF ACADEMIC HEALTH CENTERS IN THE REVOLUTION
For several reasons, there is both an opportunity and an obligation for academic health centers to play a leading role in the coming transformation of American health care.10, 12 For one thing, the revolution requires the focus of a wide array of disciplines on multiple facets of the problem. Academic health centers and their associated universities are havens of the essential cadre of diverse experts. Universities are also uniquely positioned to foster interdisciplinary collaborations on a large scale and to function as catalysts for broadly integrative fundamental and applied research. At their best, Academic health centers can bring both academic rigor and apolitical objectivity to the task and can serve as vehicles for articulating the issues in the national debate.
THE EMORY GEORGIA TECH CENTER FOR HEALTH DISCOVERY AND WELL BEING
Recognizing both the opportunity and the obligation, Emory University adopted “Predictive Health and Society” as an institution-wide initiative integral to its multiyear strategic plan (http://www.phi.emory.edu/). The Center for Health Discovery and Well Being is the initial expression of this broader initiative. The Center is a demonstration project for the basic concepts of focusing on health in its broadest context, exploring novel biomarkers that predict health or its loss, and effecting lifestyles in ways that favorably affect health risks. A goal of the center is to define, predict and maintain health throughout the human lifespan. In this sense, the studies done in the Center complement other ongoing longitudinal studies of aging as suggested below.
The Place
We started with the premise that the entire experience of encountering a health-focused program should be different than the experience of doctor-focused disease care. The Center space was designed to be a pleasant and efficient place for healthy people to come. Creative use of traffic flow design, lighting, and color schemes contrast with the usual medical clinic or doctor’s office. The effect is a more spa-like atmosphere, although the design permits efficient conduct of the measurements and other interactions that are basic to the program.
The Vocabulary
There is an extensive medical vocabulary common to medical professionals and the lay public that is heavily disease focused. In this context, people are often referred to as patients—implying that there is a diagnosis waiting to happen. For a health-focused approach, we think it is important to employ a vocabulary that is more personal and focused on wellness. We do not refer to people as patients, but rather as participants, implying a partnership aimed at optimizing health.
Participants
The Center is intended as a health-focused facility that serves essentially healthy people and does not deliver traditional medical care. The initial cohort is a random sample of employees of a large university who are fully employed, productive people. The employee pool is 60% female, 58% white non-Hispanic, 24% African American, 3% Hispanic, 15% Asian, and <1% other. Specific criteria for enrollment were: a) Inclusion criteria were male or female employees aged ≥18 years and absence of hospitalization in the previous year except for accidents; b) Exclusion criteria were: history in past 1 year of severe Axis 1 psychosocial disorders; addition of new prescription medications to treat a chronic disease condition (with exception of changes in anti-hypertensive or anti-diabetic agents); substance/drug abuse or alcoholism; current active malignant neoplasm; uncontrolled or poorly controlled autoimmune, cardiovascular, endocrine, gastrointestinal, hematologic, infectious, inflammatory, musculoskeletal, neurologic, psychiatric or respiratory disease; any acute illness (such as viral infection) in previous 2 weeks before baseline studies; likely inability to undergo the complete set of CHDWB assessments; inability to give informed consent. The participants understand that the Center is not a medical care facility and that this program complements, but does not substitute for, appropriate medical care.
Health Assessments
The group of health assessments used in the initial cohort was designed to be as comprehensive as was practical. A web-based portal, using validated instruments where they exist, collects information about mental health, social support, family situation, stress, anxiety, depression, spirituality, sleep patterns, diet, physical activity, environmental exposures, health-related behaviors, and symptoms. Many of these questionnaires can be completed at home on a secure web site. Physical measurements done in the Center include resting blood pressure and heart rate, anthropometrics, percent body fat and bone density (iDXA), treadmill fitness test and ultrasonic measurements of carotid artery thickness, arterial compliance, flow-mediated vasodilation, and central blood pressure. Blood samples are drawn for an extensive panel of known biomarkers related to endocrine, immune and metabolic health, and inflammatory and nutrition status. From serum and peripheral blood cells, measurements are made of the four processes that we hypothesize are fundamental mechanisms related to health: redox status, inflammatory cytokines, immune cells (fluorescence activated cell sorting—FACS) and regenerative capacity (circulating stem cells by FACS). A complete list of measurements that are made is given in table II.
Table 2.
Center for Health Discovery List of Questionnaires, Assessments and Laboratory Measurements
| Questionnaires |
| Basic Demographics; Personal and Family Health History; Occupational History and Exposures; Health Symptoms; Tobacco and Alcohol Usage; Medication, Supplement and Herb use; Complimentary Medicine Use |
| Assessments |
| Perceived Stress Scale; Block Food Frequency Questionnaire; CAPS Physical Activity Questionnaire; SF-36 v2; Beck Depression Scale; Family Assessment Device; Enriched Social Support Inventory; Epworth Sleepiness Scale; Pittsburgh Sleep Quality Index; Mental Health Flourishing Index; FACIT-Sp-Ex; Generalized Anxiety Disorder (GAD-7); NexSig Nexade Neurocognitive exam |
| Physical measurements |
| Resting Blood Pressure; Resting Heart Rate; Bioelectrical Impedance Analysis; DEXA scan (for bone mineral density, % fat, lean body mass); Fitness assessment (sub maximal treadmill test); Pulse Wave Analysis; Pulse Wave Velocity; Carotid IMT; Flow Medicated Dilation; Reactive Hyperemia Index; Augmentation Index |
| Laboratory Tests (blood and urine) |
| Lipid panel; Random Urine Microalbumin (w/creatinine); Iron and Total Iron binding capacity; Comprehensive Metabolic Panel w/EGFR; CBC; C-reactive protein; Ferritin; Vitamin B12; Insulin; TSH, 3rd generation; Testosterone; Estradiol; Vitamin D |
| Research Labs |
| Oxidative Stress (GSH, GSSG, Cysteine, Cystine, CysGSH, CysRedox, Serum d-ROMS, Serum Protein Nitrotyrosine, Urine F1a - isoprostanes |
| Inflammation (TNF-alpha, Interleukin-6, Interleukin-8, INF-gamma, matrix metalloproteinase-9) |
| Immune Cells and Regenerative Potential in peripheral blood mononuclear cells by FACS (CD34+, AC133+, KDR+ positive cells) |
The data for each participant are assembled into a “Health Assessment Report,” which summarizes and interprets the information. In addition, all of the data populate a de-identified database, which will be a valuable resource for exploring associations among the many variables related to predicting health. Also, serum and DNA samples from peripheral blood are stored in a bio-repository as a wet archive for future investigations.
The “Health Partner”
We are convinced that extensive use of technology is a critical part of a health-focused care program,13 but optimal health requires partnerships between people. In our program this is a partnership between a participant and a person trained to provide information and support for the participant. It is neither necessary nor economically feasible for highly trained medical professionals (e.g., doctors, physician assistants, nurse practitioners, nurses) to be the initial point of contact in a system for “essentially healthy” people. Therefore, we have introduced the concept of a “Health Partner.” This title is meant to convey a horizontal (as opposed to the traditionally vertical) relationship. Health partners have at least a bachelor’s degree, and a background in human biology, nutrition, exercise physiology, human behavior, or other relevant areas. They are trained by both didactic and practical experiences in the knowledge base and skill set needed for the targeted role of health partner. Upon entry to the program, each participant is assigned a health partner, who assists the participant in completing the surveys and other assessments, reviews and explains the health assessment report, and helps in setting and achieving the participant’s health-related goals. The health partner provides information, aid in navigating the health system, and practical advice and moral support.
The Health Assessment Report and Health Action Plan
All of the information collected on each participant is assembled into the health assessment report, which is organized to provide a general profile (health signature), as well as detailed information. The participant and their partner review the report together, identifying opportunities for improving health. A “Health Action Plan” is then developed, with specific goals set by the participant and detailed strategies for achieving those goals. The health partner stays in touch with the participant by e-mail or telephone at intervals agreed upon when the action plan is made.
Outcomes
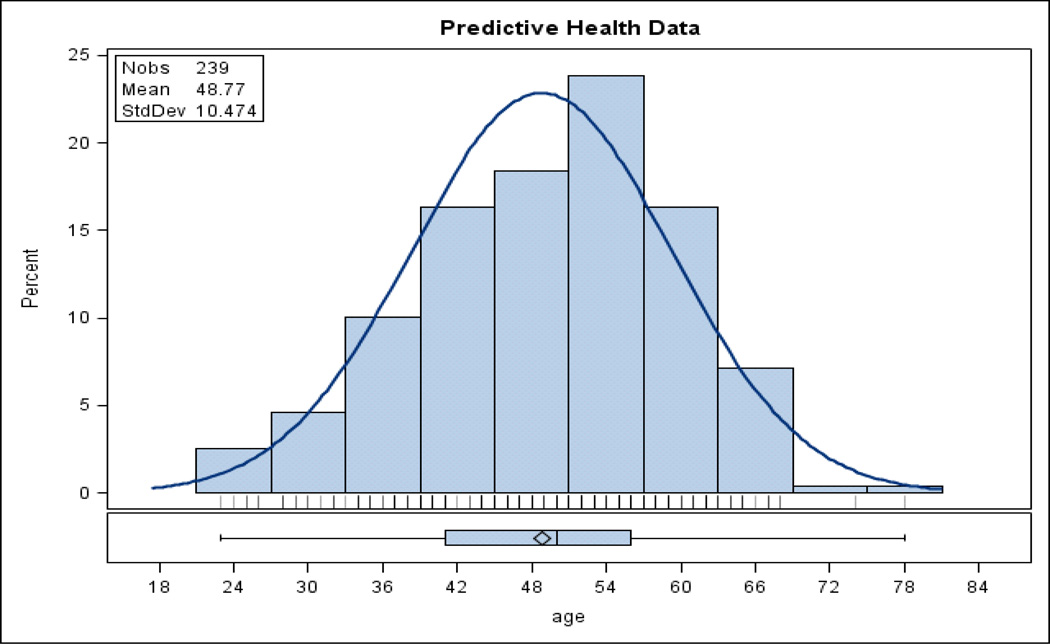
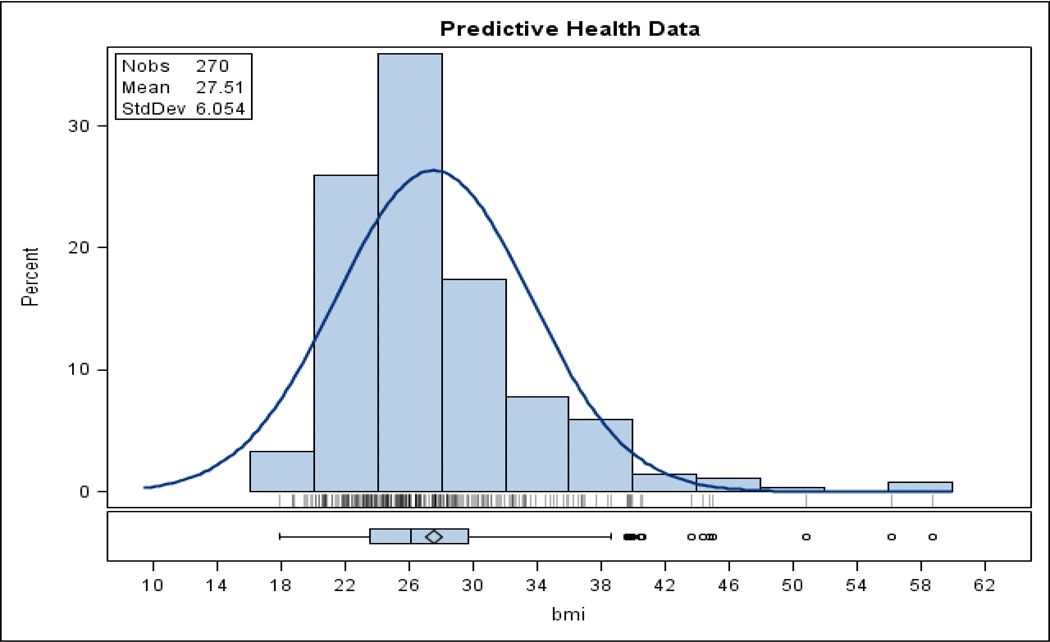
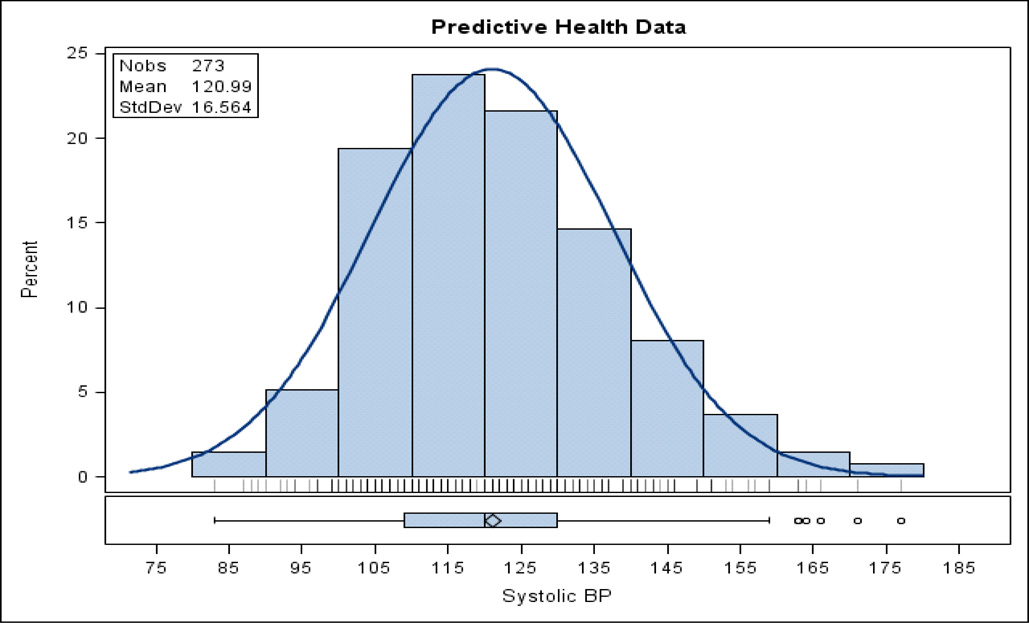
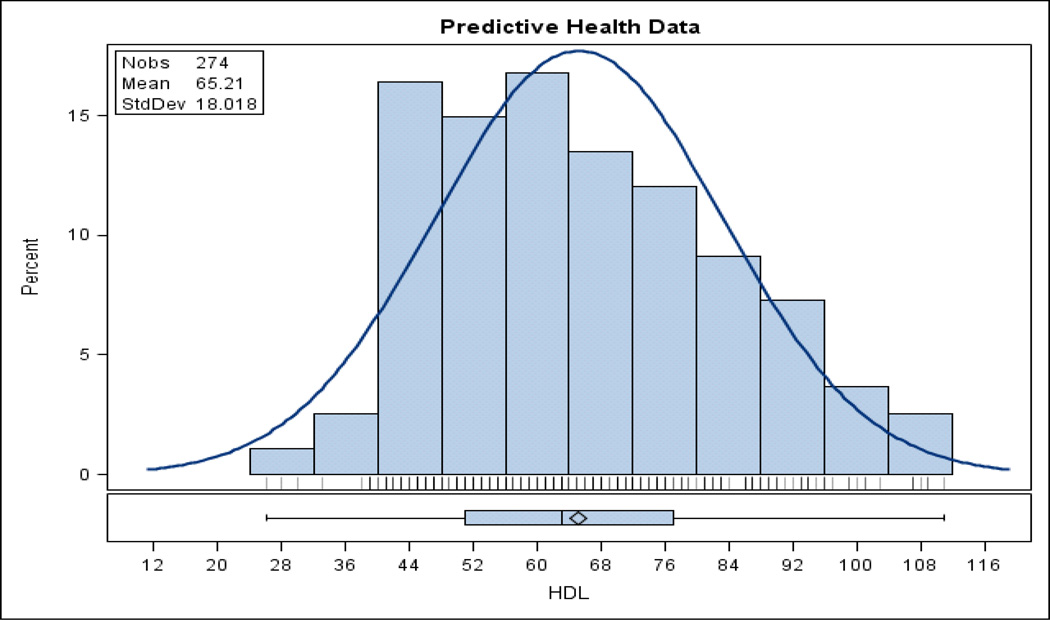
Figure 1 shows the age distribution of the initial Center cohort. The distribution is like that for the Emory employee population as expected. Although we sought to develop a cohort of “essentially healthy” people, it is apparent from the physiologic characteristics of the cohort that most of them had significant health risks. Figures 2–4 show the frequency distributions and summary descriptive statistics for body mass index (BMI), serum high density lipoproteins and systolic blood pressure in this cohort. It is apparent from those data that there are significant opportunites for improving health and disease risk even in an “essentially healthy” population (at least as we defined it).
Figure 1.
Frequency distribution of ages in the initial CHDWB cohort (Nobs is number of observations)
Figure 2.
Frequency distribution (percent of participants to date) of body mass index (BMI) in the initial CHDWB cohort (Nobs is number of observations)
Figure 4.
Frequency distribution (percent of study participants to date) of systolic blood pressure (mmHg) in the initial CHDWB cohort (Nobs is number of observations)
Because the program is so new, data from only fifty-one participants who have completed a six-month follow-up evaluation have been examined. However, the results show significant improvement in the number of biological risk factors as well as in emotional and psychological factors. Table 1 list several health related variables showing the baseline values, the changes at 6 months and the p value. Even in this small group, there were stastically significant reductions in body mass index, percent body fat, and systolic blood pressure. Fitness (VO2max) improved significantly, fasting blood glucose decreased, and serum high-density lipoprotein concentrations increased. Standardized instruments evaluating depression, anxiety, and stress also all improved significantly. Although additional data and longer-term follow-up are essential for an adequate evaluation of the program, we are encouraged by this preliminary information.
Table 1.
Effects of a 6mo Center for Health Discovery and Well Being program on variables related to cardiovascular risk in N=51 participants who have completed both baseline and 6 month evaluations
| variable | Baseline (SD) | Change @6mo (paired mean and SD) |
P |
|---|---|---|---|
| Fasting glucose (mg/dl) | 88.3(12.9) | −2.1(8.1) | 0.04 |
| HDL (mg/dl) | 67.4(19.4) | 2.71(8.43) | 0.01 |
| CD34 count (cells/ul) | 4.7(6.6) | 2.75(8.05) | 0.008 |
| Total cysteine | 168.4(35.7) | 22.6(44.5) | 0.007 |
| Augmentation index | 28.88(10.34) | 3.01(6.17) | 0.0002 |
| Mental quality of life (SF36) | 52.1(9.4) | 3.88(7.8) | 0.05 |
| Beck depression scale | 4.6(5.3) | −1.38(3.77) | 0.0045 |
| General anxiety (GAD7) | 3.94(3.1) | −1.44(2.87) | 0.07 |
| Perceived stress (PSS) | 18.0(7.9) | −2.6(6.5) | 0.07 |
| VO2max | 47.5(14.2) | 10.3(13.3) | <0.0001 |
| Systolic BP (mmHg) | 118.2(15.1) | −3.6(12.5) | 0.02 |
| % body fat | 33.8(7.5) | −0 .49 | 0.05 |
| Body mass index | 34.5(7.7) | −0.51(2.0) | 0.04 |
SUMMARY
Although chronologic aging is inevitable, how much of the usual biologic changes associated with age are an essential part of the process is not clear. Most clinical investigations in older adults have focused on disease or injury (what can go wrong). There is little detailed information available that defines optimal health (what can go right) as a function of age reaching into the eighth and ninth decades of life. In order to address this knowledge gap, the Center is conducting studies of exceptionally healthy people spanning the age spectrum from twenty years to well into the eighth decade of life. These people are on no medications and they have normal blood pressure, no chronic disease, and a normal body mass index. The elaborate series of assessments are the same as those done in the participants in the Center for Health Discovery and Well Being program. While there is physiologic aging of the cardiovascular system (e.g., systolic blood pressure, cardiovascular fitness) and other health-related factors, how the slope of the lines describing these data as a function of age compare to the more general population is a major focus of the Center’s research. These data may describe optimal health-related goals in elderly people that will be of use in the health-focused care of this growing population.
Figure 3.
Frequency distribution (percent of study participants to date) of serum high density lipoproteins (HDL mg/dL) in the initial CHDWB cohort (Nobs is number of observations)
ACKNOWLEDGEMENTS
This paper is based on a January 2009 conference on Longitudinal Studies in Aging, supported by a grant from the Robert Wood Johnson Foundation.
Funding Source: Cousins Foundation Inc. and Emory University
Sponsor’s Role: None
Footnotes
| Elements of Financial/Personal Conflicts |
*Author 1 | Author 2 | Author 3 | Etc. | ||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | x | |||||||
| Grants/Funds | x | |||||||
| Honoraria | x | |||||||
| Speaker Forum | x | |||||||
| Consultant | x | |||||||
| Stocks | x | |||||||
| Royalties | x | |||||||
| Expert Testimony | x | |||||||
| Board Member | x | |||||||
| Patents | x | |||||||
| Personal Relationship | x | |||||||
Author’s Contributions: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, preparation of manuscript.
REFERENCES
- 1.Nolte E, McKee CM. Measuring the health of nations: Updating an earlier analysis. Health Aff. 2008;27:58–71. doi: 10.1377/hlthaff.27.1.58. [DOI] [PubMed] [Google Scholar]
- 2.Center on Budget and Policy Priorities, report. 2006 Aug 29; http://www.cbpp.org/files/8-29-06health.pdf.
- 3.Trevidi B. Biomedical science: Betting the bank. Nature News. 2008;452:926–929. doi: 10.1038/452926a. [DOI] [PubMed] [Google Scholar]
- 4.Metabolomics: Signs of a long life. The Economist. 2008 Jun 26; [Google Scholar]
- 5.Aspinall MG, Hamermesh RG. Realizing the promise of personalized medicine. Harvard Bus Rev Oct. 2007:109–118. [PubMed] [Google Scholar]
- 6.Schroeder SA. We can do better—improving the health of the American people. N Engl J Med. 2007;357:1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 7.Goetzel RZ, Anderson DR, Whitmer RW, et al. The relationship between modifiable health risks and health care expenditures. J Occup Environ Med. 1998;40:843–854. doi: 10.1097/00043764-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Fries JF, Koop CE, Beadle CE, et al. Reducing health care costs by reducing the need and demand for medical services. N Engl J Med. 1993;329:321–325. doi: 10.1056/NEJM199307293290506. [DOI] [PubMed] [Google Scholar]
- 9.Snyderman R, Langheier J. Prospective health care: the second transformation of medicine. [Accessed August 6, 2009];Genome Biol. 2006 7(2):104. doi: 10.1186/gb-2006-7-2-104. (online). Available at: http://genomebiology.com/2006/7/2/104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johns MME, Brigham KL. Transforming health care through prospective medicine: the first step. Acad Med. 2008;83:706. doi: 10.1097/ACM.0b013e31817eb579. [DOI] [PubMed] [Google Scholar]
- 11.Preamble to the Constitution of the WHO as adopted by the International Health Conference, NY, 19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the WHO, no. 2, p. 100) and entered into force on April 7, 1948; [Google Scholar]
- 12.Snyderman R, Yoediono Z. Perspective: Prospective health care and the role of academic medicine: Lead, follow or get out of the way. Acad Med. 2008;83:707–714. doi: 10.1097/ACM.0b013e31817ec800. [DOI] [PubMed] [Google Scholar]
- 13.Satz A. Toward solving the health care crisis: The paradoxical case for universal access to high technology. Yale J Health Policy Law Ethics. 2008;8:93–143. [PubMed] [Google Scholar]