Abstract
HIV/AIDS is a chronic illness, with a range of physical symptoms and psychosocial issues. The complex health and social issues associated with living with HIV mean that people living with HIV/AIDS (PLWHA) have historically often turned to complementary and alternative medicine (CAM). This article provides an overview of the literature on HIV and CAM. Databases were searched using keywords for CAM and HIV from inception to December 2012. Articles in English and in Western countries were included; letters, commentaries, news articles, articles on specific therapies and basic science studies were excluded. Of the 282 articles identified, 94 were included. Over half reported prevalence and determinants of CAM use. Lifetime use of CAM by PLWHA ranged from 30% to 90%, with national studies suggesting CAM is used by around 55% of PLWHA, practitioner-based CAM by 15%. Vitamins, herbs, and supplements were most common, followed by prayer, meditation, and spiritual approaches. CAM use was predicted by length of time since HIV diagnosis, and a greater number of medications/symptoms, with CAM often used to address limitations or problems with antiretroviral therapy. CAM users rarely rejected conventional medicine, but a number of CAM can have potentially serious side effects or interactions with ART. CAM was used as a self-management approach, providing PLWHA with an active role in their healthcare and sense of control. Clinicians, particularly nurses, should consider discussing CAM with patients as part of patient-centered care, to encourage valuable self-management and ensure patient safety.
Introduction
Complementary and alternative medicine (CAM) is defined as “a group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine,”1 for example acupuncture, herbal medicine, osteopathy, homeopathy, or massage. CAM has been historically popular among people living with HIV/AIDS (PLWHA), as before the development of antiretroviral therapy (ART) in the mid-1990s, PLWHA experienced frustration and despair due to the lack of and slow progress of treatment options.2 Since this initial uptake of CAM by the HIV/AIDS community, the experience of living with HIV has changed radically, mainly due to the development and widespread effective use of highly active ART (HAART). PLWHA have, in general, demonstrated adaptability to the changing treatments available, including CAM.3
HIV is now a manageable chronic illness,4–6 with life expectancy in the developed world similar to that of people without HIV.7 PLWHA experience a range of physical symptoms and psychosocial issues, some in common with other chronic diseases, some unique. These include abnormal psychology, mood and related disorders, personal and social uncertainty, identity issues, stigma, social isolation, poor quality of life, and unemployment,5 and a range of side effects from ART such as gastrointestinal and dermatological effects, cardiac and liver problems, and bone loss.8 The impact of HIV on physical and emotional health may be worse than for many other chronic diseases.9 CAM is still often used to address these complex health and social issues associated with living with HIV/AIDS,10 including stress reduction, relieving side-effects and symptoms, and boosting the immune system.11
It is important that conventional clinicians are aware of CAM use and, where appropriate, discuss its use with their patients, both to improve the practitioner-patient relationship and adherence to ART, and to identify potential safety issues.12,13 Practitioners therefore need to have up-to-date knowledge regarding CAM use. Previous reviews have often focused only on the prevalence and determinants of CAM use, often with a methodological rather than clinical focus;14,15 this review aims to provide a broader overview of the current literature on the use of CAM for PLWHA to identify issues which may have implications for patient care.
Methods
The following databases were systematically searched in December 2012 with no date limits: Medline, Cinahl, PsycArticles, AMED, Sciencedirect, Cochrane library. Search terms were for HIV and complementary therapy/medicine (Table 1).
Table 1.
Search Strategy and Results
| HIV | CAM | Results | |
|---|---|---|---|
| Medline | HIV (mesh) OR HIV Infection (mesh) | Complementary therapies (mesh) | 189 |
| Cinahl | MH human immunodeficiency virus | MH alternative therapies | 4 |
| PsycArticles | HIV OR “human immunodeficiency virus” | “Complementary therapies” OR “complementary medicine” OR “alternative therapies” OR “alternative medicine” OR “complementary and alternative medicine” | 3 |
| AMED | SH HIV | 8 | |
| Sciencedirect | HIV (abs/title/key) | “Complementary therapies” OR “complementary medicine” OR “alternative therapies” OR “alternative medicine” OR “complementary and alternative medicine” (abs/title/key) | 61 |
| Cochrane library | HIV | 17 | |
| 282 |
In order to identify studies with relevance for patient care in the UK and other Western countries, inclusion criteria were: about complementary or alternative medicine and HIV; in English; based in a Western country. Exclusion criteria were: studies on a specific CAM therapy; letters, commentaries, news articles; basic science studies (animal or lab-based).
Results
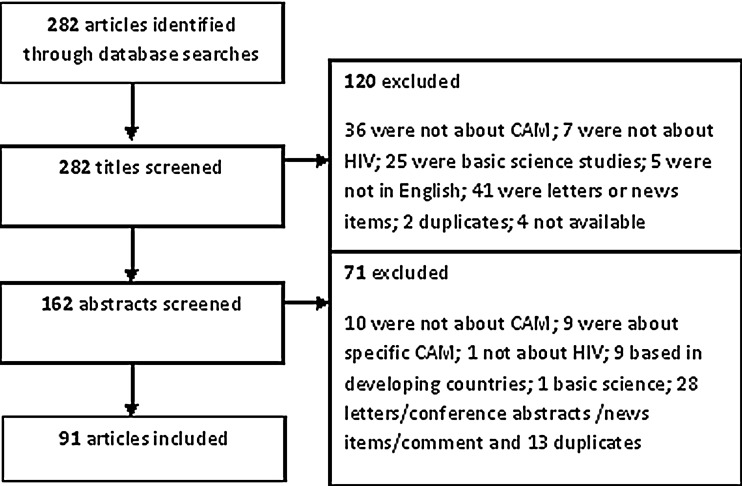
A total of 282 articles were identified, 119 were excluded from reviewing the titles, and a further 71 from screening abstracts, leaving a total of 91 articles for review. See Fig. 1 for details. Many of the studies were conducted in the USA. The 91 articles were published between 1989 and 2012 and were grouped as below:
FIG. 1.
Flowchart of study selection.
Studies of the prevalence and determinants of CAM use for PLWH—54 articles14–68
Studies of PLWHA attitudes to CAM, reasons for use and decision-making process—15 articles10,69–81
Overviews of the evidence for CAM—nine reviews82–90 and one two-part overview of the use of CAM in HIV91,92
Prevalence
Of the 54 articles identified on the prevalence of CAM use, one was a systematic review15 and there were three other reviews.14,45,46 Thirty-five were carried out in North America,16,19–56,64 five in Europe,57–61 and two in Australia.62,63 Three studies used national samples.52,63,64
Prevalence figures for lifetime use of CAM varied from 30% to 90%; use over the past 6–12 months ranged from 15.4% to 100%. Variations in prevalence figures are partly due to differing definitions of CAM, for example, when restricted to practitioner-based CAM, prevalence was only 15–16%.32,35 The three national studies35,63,64 and two multistate studies32,34 give the most externally valid results. They suggest that CAM is used by around 55–60% of PLWHA;63,64 15–16% practitioner-based CAM.32,35
Vitamins, herbs, and supplements were the most common approaches used, followed by prayer, meditation and spiritual approaches, massage, and acupuncture.
Higher levels of education and being female were the most common predictors of CAM use (reported as significant in 1316,20,22–24,28,30,32,36,57,59,62,63 and seven 19,23,31,59,62,63,66 studies, respectively). Other determinants were Caucasian,23,28 higher income,20,35 gay/lesbian,24,35 younger,20,63 and having depression.25,35 HIV-specific predictors included longer disease duration/time on ART (5 studies16,21,36,57,62), and using a higher number of medications (2),19,60 more symptoms/infections (3),25,36,57 and ART side effects (2).16,59 CAM use was associated with having an HIV diagnosis;43 and Carwein and Sabo27 found that 100% of participants with HIV used CAM, compared to 16% before HIV diagnosis. Other predictors suggest an association with having a more active role in healthcare, for example, reading more information or having more health promoting behaviours.25,26,35,63
Reasons for use varied, from reducing symptoms and improving well-being to improving immunity. Five studies reported the use of CAM for people with specific symptoms (depression,51,65 anxiety,56 peripheral neuropathy,55 and pain52). In these studies, prayer and meditation were preferred options and use varied from 18% to 52% of respondents. CAM use was associated with less illicit drug use in one study.48 Four prevalence studies specifically focused on adherence to HAART therapy,47–49,61 but results were equivocal, with no firm pattern suggested as to whether adherence was improved as a result of CAM use.
Given the strong influence of the introduction of HAART, particularly the latest one-pill-once-daily regimens, on the behaviour, treatment, and lifestyle of PLWHA,101 we compared prevalence articles published pre- and post-modern HAART regimens (i.e., before/after 2005 when single dose regimens became widely available and recommended).4,102–104 However, there were no differences in prevalence figures, determinants, or reasons for use, suggesting that ART does not have a strong influence on CAM use by PLWHA, discussed further below.
Attitudes to CAM, reasons for use and decision-making
Fifteen studies were identified regarding patients' attitudes to CAM, reasons for use and decision-making. Ten were north American,67,69,71–74,77–79,81 four from Australia,10,70,76,80 and one from Switzerland.75
One of the key reasons for using CAM was to provide a method to self-manage health or to give a sense of control,10,71,77,80 to cope with uncertainty,71 manage symptoms,71 give freedom from and additional choice to medical regimens,10,71,76,80 and attempt to normalize health status, maintain health, or find wellness.71,77,78 CAM was also used for personal growth or fulfilment77,78 with different CAM used along a journey, from those focusing on the physical self to those facilitating inner awareness, such as meditation.77
Another key reason was to address the limitations or problems with conventional ART.70,80,81 However, most studies found that CAM users did not reject conventional medicine;78 only one study found that a preference for CAM predicted non-use of ART.74 In fact, one study found that patients used conventional parameters such as CD4 counts to make their decisions about CAM.79
One study described the decision-making process of selecting a CAM, often based on friends and family, judging which approaches work and are safe, from subjective personal experience, attempting to combine conventional medicine and CAM.73 Cultural values appear likely to influence the decision to use CAM.69,78 One study found that psychologically needier people were more likely to seek CAM.75
Barriers to CAM use include cost, access, time/discipline/energy needed, overwhelming choice, and the need for evidence.72,73
Guidance for clinicians
Six articles were identified giving guidance for clinicians, looking at the issues of combining CAM with HIV conventional medication.12,13,93–96
Four articles provided guidance for nurses to make decisions regarding CAM, advising that nurses discuss CAM use with their HIV patients.13,93,95,96 Irish, although this article is now very outdated, suggests that discussing CAM with patients is part of nurses' obligation to provide patient-centred care, and that nurses should assess whether CAM are harmful and encourage disclosure by being nonjudgmental, which can help to maintain health.13 Palmer provides an overview for HIV nurses on CAM, CAM use and reasons, safety issues, and benefits.93 He concludes that nurses have an ethical obligation to provide patients with up-to-date information about CAM products so that they can make an informed choice.93 Haddad presents a clinical scenario of a patient with HIV who wishes to use CAM instead of conventional treatment.95 She discusses the need for nurses in this situation to avoid jumping to the conclusion that they should dissuade the patient and instead suggests exploring the reasons behind the patient's wishes, particularly any concerns about conventional treatment, and ensuring the patient makes an informed decision. Freeman and MacIntyre also advise that nurses have an understanding of CAM in order to improve their relationships with patients.96
The other two articles,12,94 although somewhat outdated, potentially provide useful HIV-specific guides to a range of CAM. Steinberg94 also provides some suggestions for how conventional practitioners, or PLWHA themselves, can integrate CAM and conventional treatment. This includes ‘finding the right balance’, ‘dealing with uncertainty’ regarding new symptoms and illness progression, ‘anger’ related to the social/financial impact of HIV, ‘nonexclusivity’ (using CAM to complement other treatments), and encouraging patient responsibility and empowerment. Elion and Cohen12 emphasise the need for discussion and disclosure of CAM use, for safety reasons, but also issues of cost, fraud and the evidence-base.
These articles illustrate how a discussion of CAM can form part of nurses' holistic and patient-centered care of PLWHA and emphasize the need for primary care providers and nurses to engage in dialogue with patients regarding CAM, and encourage disclosure by being nonjudgmental.
Reviews of treatments
Nine review articles provided descriptive information on various treatments82–90 and a two-part review additionally covered a range of other issues.91,92 Reviews on the effect of CAM were generally positive and suggest that CAM has a potential use for a range of health issues,84,86–89,105 although many highlighted that the evidence base is still inconclusive. Massage therapy84,105 and stress management86,87 were highlighted as the CAM most likely to be beneficial treatments. Two reviews highlighted the limitations of the evidence base, which was seen as insufficient to support use of any CAM.85,90
Safety
Only four articles were identified regarding the safety of CAM and HIV, plus the Spanish study by Vaszquez et al., which includes safety information.61 Ernst97 described some of the risks of CAM, although these were not HIV specific, and then gave a single case study example of an HIV patient being exploited by an ‘energy’ therapy. An article by Gilmour et al.98 is not specifically about HIV; they describe natural health product–drug interactions in general and the need to ask patients about CAM use, using the case example of an HIV -positive patient taking St Johns wort, which interacts with indinavir. Ladenheim et al.99 provide a more thorough study of the potential health risks of CAM for PLWHA, using a survey of the use of herbal medicine and supplements among PLWHA to identify any potential risks. They identified 59 patients (20% of those using CAM) whose CAM use necessitated a warning, 29 of whom were advised to stop their CAM use due to concerns about serious interaction with ART or adverse effects. The most common adverse effect was with echinacea (used by 22 patients) which, in theory, could increase the number of infected leucocytes by stimulating the immune system, resulting in increased HIV viral load. Eight patients were using garlic, and two were using St Johns wort, which can both interact with ART, reducing its therapeutic levels. One patient was using kava, which may cause hepatotoxicity. Other CAM being used were not as high a safety risk but patients were advised to use with caution. These included aloe vera, gingko biloba, and vitamin C megadoses, which can reduce the effectiveness of ART, and cat's claw, DHEA, ginseng, liquorice, milk thistle, and red yeast, which can cause ART-related side effects. Vaszquez et al. (included above as a prevalence study)61 additionally documented potential herbal medicine-ART interactions, which also included echinacea, milk thistle, garlic, ginseng, and cat's claw, as well as grapefruit (can reduce concentrations of indinavir and saqyinavir), valerian (can increase hepatotoxicity), marijuana (reduces Cmax), hypericum (reduces ART effectiveness). Ladenheim et al. highlighted that the main risk of CAM use in PLWHA is potential ART–interaction, through the cytochrome pathways, making CAM use with protease inhibitor and non-nucleoside reverse transcriptase inhibitor ARTs particularly risky. A focus group study identified that safety of CAM is important in patients' decision making, but that they had limited knowledge, although this study was nearly 10 years old.100
Discussion
CAM appears to be popular with PLWHA, although there is a paucity of recent, large-scale, national survey data, particularly outside of the USA. Prevalence figures vary widely, though this is known to be a common issue in studies of CAM.106 Vitamins, herbs, and supplements emerge as the most common approaches used, followed by prayer, meditation, and spiritual approaches.
Supplements and herbs may be used for a range of reasons, including cleansing or strengthening the body.88 Their popularity may be related to a generally high knowledge of nutrition amongst PLWHA, encouraged by the community and by healthcare clinicians.107 These oral CAM can cause potential safety issues through interaction with conventional medication, in particular ART, with implications for the role of conventional clinicians.98,99 However, as seen in this review, there is a lack of research on the specific safety implications of CAM use by PLWHA.3
Prayer, meditation, and spiritual approaches may be used to provide an approach to understanding and coping with chronic illness and providing emotional support and a stabilizing force within daily life.108 It is important that clinicians understand that these approaches may be important to patients, particularly within the context of patient-centred and culturally-competent care.
CAM use appears related to having an HIV diagnosis27 and in many of the articles reviewed, CAM use was predicted by having a longer duration of time since HIV diagnosis and a greater number of medications and symptoms. This may relate in part to ART use, as CAM is often used to address the limitations of or problems with ART. This is most likely in a complementary rather than alternative manner, as most studies found that CAM users did not reject conventional medicine but used CAM as part of an integrated approach.80 Thorpe et al.10 explain that PLWHA did not want CAM to ‘re-medicalize’ health management but instead used CAM as part of a ‘return to normality’. As well as coping with the side effects of ART, CAM may be used for relaxation, to support a positive attitude and to improve energy levels.108
A strong theme from the literature was the use of CAM to provide a method of self-management of health or give a sense of control for PLWHA, as evidenced by the high use by those who are active in their own healthcare. This theme has been identified for other chronic illnesses, including cancer.108,109 Swenderman110 emphasizes that self-management is as important, and complex, in HIV as in other chronic conditions, with additional HIV-specific challenges related to lack of self-monitoring, stigma, disclosure, and transmission routes. The emphasis on self-management may be related to the “AIDS movement” and activism in the HIV/AIDS community.3 Encouraging effective self-management of health is important in HIV as it is associated with medication adherence,111 although this review did not find evidence that CAM use was associated with adherence.
Although it places the emphasis on the patient, healthcare clinicians have a key role in self-management, both providing treatment and advice, as well as encouragement, motivation, and tools.108,111 Only a quarter of HIV clinicians report asking patients about CAM use,112 although PLWHA who use CAM still rely on biomedical knowledge and providers to provide certainty.10 There is clearly a need, even an ethical duty,3 for conventional healthcare providers to discuss CAM with their patients, including perhaps making informed decisions on the use of CAM and being aware of potential safety implications, particularly interactions between herbal and conventional medicines.98,113 Although some evidence-based information is available for clinicians, for example, in a range of articles identified in this review,14,82,83,91,92 there is a need for education of clinicians and perhaps for professional guidance to stipulate discussion of CAM as part of HIV clinicians' duty.3 There is also a need for further research into CAM for HIV/AIDS,3 perhaps starting with massage and stress management which show promising preliminary evidence.
Given the numerous similarities identified between HIV and other chronic diseases, emphasizing HIV as a chronic disease may help to encourage self-management, reduce stigma, and expand access to healthcare.110
In conclusion, CAM is popular with PLWHA, particularly supplements, herbs, and spiritual approaches, and appears related to having an HIV diagnosis. The use of these complementary approaches appears to help PLWHA to cope with symptoms and side effects, but also, perhaps more importantly, to take control of their own health. Clinicians should consider discussing CAM with patients as it may encourage valuable self-management and ensure patient safety.
Acknowledgments
We are grateful to NHS Brent Primary Care Trust for funding this work.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.NCCAM. What Is Complementary and Alternative Medicine? http://nccam nih gov/health/whatiscam. 2010. http://nccam.nih.gov/health/whatiscam. [Feb 8;2013 ]. http://nccam nih gov/health/whatiscamhttp://nccam.nih.gov/health/whatiscam
- 2.Abrams DI. Alternative therapies in HIV infection. AIDS. 1990;4:12. doi: 10.1097/00002030-199012000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Crouch R. Elliott R. Lemmens T. Charland L. Complementary/alternative health care and HIV/AIDS: Legal, ethical and policy issues in regulation. Canad HIV/AIDS Legal Network. 2001 [Google Scholar]
- 4.Yeni P. Update on HAART in HIV. J Hepatol. 2006;44:S100–S103. doi: 10.1016/j.jhep.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 5.Green G. Smith R. The psychosocial and health care needs of HIV-positive people in the United Kingdom: A review. HIV Med. 2004;5:5–46. doi: 10.1111/j.1468-1293.2004.00210.x. [DOI] [PubMed] [Google Scholar]
- 6.Siegel K. Lekas HM. AIDS as a chronic illness: Psychosocial implications. AIDS. 2002;16:S69–S76. doi: 10.1097/00002030-200216004-00010. [DOI] [PubMed] [Google Scholar]
- 7.Rodger AJ. Lodwick R. Schechter M, et al. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS. 2013;27:973–979. doi: 10.1097/QAD.0b013e32835cae9c. [DOI] [PubMed] [Google Scholar]
- 8.Johnson M. Dilworth S. Taylor J, et al. Improving coping skills for self-management of treatment side effects can reduce antiretroviral medicationnonadherence among people living with HIV. Ann Behav Med. 2011;41:83–91. doi: 10.1007/s12160-010-9230-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hays RD. Cunningham WE. Sherbourne CD, et al. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: Results from the HIV cost and services utilization study. Am J Med. 2000;108:714–722. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 10.Thorpe RD. ‘Doing’ chronic illness? Complementary medicine use among people living with HIV/AIDS in Australia. Sociol Health Illness. 2009;31:375–389. doi: 10.1111/j.1467-9566.2008.01137.x. [DOI] [PubMed] [Google Scholar]
- 11.NAM. Reasons why people with HIV use complementary therapies. http://www aidsmap com/Reasons-why-people-with-HIV-use-complementary-therapies/page/1254992/ 2013. http://www aidsmap com/Reasons-why-people-with-HIV-use-complementary-therapies/page/1254992/ , cited Jul 4, 2013.
- 12.Elion RA. Cohen C. Complementary medicine and HIV infection. Primary Care: Clinics Office Practice. 1997;24:905–919. doi: 10.1016/s0095-4543(05)70316-x. [DOI] [PubMed] [Google Scholar]
- 13.Irish AC. Maintaining health in persons with HIV infection. Semin Oncol Nursing. 1989;5:302–307. doi: 10.1016/0749-2081(89)90011-9. [DOI] [PubMed] [Google Scholar]
- 14.Littlewood RA. Vanable PA. A global perspective on complementary and alternative medicine use among people living with HIV/AIDS in the era of antiretroviral treatment. Curr HIV/AIDS Rep. 2011;8:257–268. doi: 10.1007/s11904-011-0090-8. [DOI] [PubMed] [Google Scholar]
- 15.Owen-Smith A. DePadilla L. DiClemente R. The assessment of complementary and alternative medicine use among individuals with HIV: A systematic review and recommendations for future research. J Altern Complem Med. 2011;17:789–796. doi: 10.1089/acm.2010.0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhalla S. Chan KJ. Montaner JSG, et al. Complementary and alternative medicine use in British Columbia: A survey of HIV positive people on antiretroviral therapy. Complem Ther Clin Prac. 2006;12:242–248. doi: 10.1016/j.ctcp.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Barton SE. Davies S. Schroeder K, et al. Complementary therapies used by people with HIV infection. AIDS London, England. 1994;8:561. [PubMed] [Google Scholar]
- 18.Dietrich MA. Rublein JC. Butts JD, et al. Evaluation of the use of nontraditional treatments by patients with HIV. J Am Pharm Assoc Washington, DC. 1998;38:388–389. [PubMed] [Google Scholar]
- 19.Furler MD. Einarson TR. Walmsley S, et al. Use of complementary and alternative medicine by HIV-infected outpatients in Ontario, Canada. AIDS Patient Care STDs. 2003;17:155–168. doi: 10.1089/108729103321619764. [DOI] [PubMed] [Google Scholar]
- 20.Ostrow MJ. Cornelisse PG. Heath KV. et al. Determinants of complementary therapy use in HIV-infected individuals receiving antiretroviral or anti-opportunistic agents. J Acq Immune Def Synd Human Retrovirol. 1997;15:115–120. doi: 10.1097/00042560-199706010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Anderson W. O'Connor BB. MacGregor RR, et al. Patient use and assessment of conventional and alternative therapies for HIV infection and AIDS. AIDS (London, England) 1993;7:561–565. doi: 10.1097/00002030-199304000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Ang JY. Ray-Mazumder S. Nachman SA, et al. Use of complementary and alternative medicine by parents of children with HIV infection and asthma and well children. South Med J. 2005;98:869–875. doi: 10.1097/01.smj.0000173089.51284.69. [DOI] [PubMed] [Google Scholar]
- 23.Bates BR. Kissinger P. Bessinger RE. Complementary therapy use among HIV-infected patients. AIDS Patient Care STDs. 1996;10:32–36. doi: 10.1089/apc.1996.10.32. [DOI] [PubMed] [Google Scholar]
- 24.Bica I. Tang AM. Skinner S, et al. Use of complementary and alternative therapies by patients with human immunodeficiency virus disease in the era of highly active antiretroviral therapy. J Alt Complem Med New York, N Y. 2003;9:65–76. doi: 10.1089/107555303321222955. [DOI] [PubMed] [Google Scholar]
- 25.Bormann JE. Uphold CR. Maynard C. Predictors of complementary/alternative medicine use andintensity of use among men with HIV infection from two geographic areas in the United States. J Assoc Nurses AIDS Care. 2009;20:468–480. doi: 10.1016/j.jana.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Burg MA. Uphold CR. Findley K, et al. Complementary and alternative medicine use among HIV-infected patients attending three outpatient clinics in the Southeastern United States. Intl J STD AIDS. 2005;16:112–116. doi: 10.1258/0956462053057611. [DOI] [PubMed] [Google Scholar]
- 27.Carwein VL. Sabo CE. The use of alternative therapies for HIV infection: Implications for patient care. AIDS Patient Care STDs. 1997;11:79–85. doi: 10.1089/apc.1997.11.79. [DOI] [PubMed] [Google Scholar]
- 28.Chang BL. van Servellen G. Lombardi E. Factors associated with complementary therapy use in people living with HIV/AIDS receiving antiretroviral therapy. J Alt Complem Med. 2003;9:695–710. doi: 10.1089/107555303322524544. [DOI] [PubMed] [Google Scholar]
- 29.Duggan J. Peterson WS. Schutz M, et al. Use of complementary and alternative therapies in HIV-infected patients. AIDS Patient Care STDs. 2001;15:159–167. doi: 10.1089/108729101750123661. [DOI] [PubMed] [Google Scholar]
- 30.Fairfield KM. Eisenberg DM. Davis RB, et al. Patterns of use, expenditures, and perceived efficacy of complementary and alternative therapies in HIV-infected patients. Arch Int Med. 1998;158:2257–2264. doi: 10.1001/archinte.158.20.2257. [DOI] [PubMed] [Google Scholar]
- 31.Gore-Felton C. Vosvick M. Power R, et al. Alternative therapies: A common practice among men and women living with HIV. J Assoc Nurses AIDS Care. 2003;14:17–27. doi: 10.1177/1055329003014003002. [DOI] [PubMed] [Google Scholar]
- 32.Josephs J. Fleishman J. Gaist P, et al. Use of complementary and alternative medicines among a multistate, multisite cohort of people living with HIV/AIDS. HIV Med. 2007;8:300–305. doi: 10.1111/j.1468-1293.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman K. Gregory WL. Discriminators of complementary and alternative medicine provider use among men with HIV/AIDS. Am J Health Behav. 2007;31:591–601. doi: 10.5555/ajhb.2007.31.6.591. [DOI] [PubMed] [Google Scholar]
- 34.Liu C. Yang Y. Gange SJ, et al. Disclosure of complementary and alternative medicine use to health care providers among HIV-infected women. AIDS Patient Care STDs. 2009;23:965–971. doi: 10.1089/apc.2009.0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.London AS. Foote-Ardah CE. Fleishman JA, et al. Use of alternative therapists among people in care for HIV in the United States. Am J Public Health. 2003;93:980–987. doi: 10.2105/ajph.93.6.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mikhail IS. DiClemente R. Person S, et al. Association of complementary and alternative medicines with HIV clinical disease among a cohort of women living with HIV/AIDS. J Acq Immune Defic Syndromes. 2004;37:1415–1422. doi: 10.1097/01.qai.0000130549.65946.3d. [DOI] [PubMed] [Google Scholar]
- 37.Milan FB. Arnsten JH. Klein RS, et al. Use of complementary and alternative medicine in inner-city persons with or at risk for HIV infection. AIDS Patient Care STDs. 2008;22:811–816. doi: 10.1089/apc.2007.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nokes KM. Kendrew J. Longo M. Alternative/complementary therapies used by persons with HIV disease. J Assoc Nurses AIDS Care. 1995;6:19–24. doi: 10.1016/S1055-3290(95)80005-0. [DOI] [PubMed] [Google Scholar]
- 39.Risa KJ. Nepon L. Justis JC, et al. Alternative therapy use in HIV-infected patients receiving highly active antiretroviral therapy. Intl J STD AIDS. 2002;13:706–713. doi: 10.1258/095646202760326471. [DOI] [PubMed] [Google Scholar]
- 40.Shedlin MG. Anastasi JK. Decena CU, et al. Use of complementary and alternative medicines and supplements by Mexican-origin patients in a U.S./Mexico border HIV clinic. J Assoc Nurses AIDS Care. 2012 Nov 1; doi: 10.1016/j.jana.2012.07.001. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siegel K. Brown-Bradley C. Lekas HM. Strategies for coping with fatigue among HIV-positive individuals fifty years and older. AIDS Patient Care STDs. 2004;18:275–288. doi: 10.1089/108729104323076016. [DOI] [PubMed] [Google Scholar]
- 42.Singh N. Squier C. Sivek C, et al. Determinants of nontraditional therapy use in patients with HIV infection. A prospective study. Arch Int Med. 1996;156:197–201. [PubMed] [Google Scholar]
- 43.Sparber A. Wootton JC. Bauer L, et al. Use of complementary medicine by adult patients participating in HIV/AIDS clinical trials. J Alt Comp Med. 2000;6:415–422. doi: 10.1089/acm.2000.6.415. [DOI] [PubMed] [Google Scholar]
- 44.Standish LJ. Greene KB. Bain S, et al. Alternative medicine use in HIV-positive men and women: Demographics, utilization patterns and health status. AIDS Care. 2001;13:197–208. doi: 10.1080/095401201300059759. [DOI] [PubMed] [Google Scholar]
- 45.Wootton JC. Sparber A. Surveys of complementary and alternative medicine: Part III. Use of alternative and complementary therapies for HIV/AIDS. J Alt Comp Med. 2001;7:371–377. doi: 10.1089/107555301750463251. [DOI] [PubMed] [Google Scholar]
- 46.Wootton JC. Sparber A. Surveys of complementary and alternative medicine usage: A review of general population trends and specific patient populations. Sem Integ Med. 2003;1:10–24. [Google Scholar]
- 47.Owen-Smith A. Diclemente R. Wingood G. Complementary and alternative medicine use decreases adherence to HAART in HIV-positive women. AIDS Care. 2007;19:589–593. doi: 10.1080/09540120701203279. [DOI] [PubMed] [Google Scholar]
- 48.Merenstein D. Yang Y. Schneider MF, et al. Association of complementary and alternative medicine use with highly active antiretroviral therapy initiation. Alt Ther Health Med. 2008;14:18–22. [PMC free article] [PubMed] [Google Scholar]
- 49.Wutoh AK. Brown CM. Kumoji EK, et al. Antiretroviral adherence and use of alternative therapies among older HIV-infected adults. J Natl Med Assoc. 2001;93:243–250. [PMC free article] [PubMed] [Google Scholar]
- 50.Merenstein DJ. Hu H. Robison E, et al. Relationship between complementary/alternative treatment use and illicit drug use among a cohort of women with, or at risk for, HIV infection. J Alt Complem Med. 2010;16:989–993. doi: 10.1089/acm.2009.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eller LS. Corless I. Bunch EH, et al. Self-care strategies for depressive symptoms in people with HIV disease. J Adv Nursing. 2005;51:119–130. doi: 10.1111/j.1365-2648.2005.03474.x. [DOI] [PubMed] [Google Scholar]
- 52.Tsao JCI. Dobalian A. Myers CD, et al. Pain and use of complementary and alternative medicine in a national sample of persons living with HIV. J Pain Symptom Manag. 2005;30:418–432. doi: 10.1016/j.jpainsymman.2005.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jernewall N. Zea MC. Reisen CA, et al. Complementary and alternative medicine and adherence to care among HIV-positive Latino gay and bisexual men. AIDS Care. 2005;17:601–609. doi: 10.1080/09540120512331314295. [DOI] [PubMed] [Google Scholar]
- 54.Rowlands C. Powderly WG. The use of alternative therapies by HIV-positive patients attending the St. Louis AIDS Clinical Trials Unit. Missouri Med. 1991;88:807–810. [PubMed] [Google Scholar]
- 55.Nicholas PK. Voss J. Wantland D, et al. Prevalence, self-care behaviors, and self-care activities for peripheral neuropathy symptoms of HIV/AIDS. Nursing Health Sci. 2010;12:119–126. doi: 10.1111/j.1442-2018.2009.00505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kemppainen JK. Holzemer WL. Nokes K, et al. Self-care management of anxiety and fear in HIV disease. J Assoc Nurses AIDS Care. 2003;14:21–29. doi: 10.1177/1055329002250958. [DOI] [PubMed] [Google Scholar]
- 57.Colebunders R. Dreezen C. Florence E, et al. The use of complementary and alternative medicine by persons with HIV infection in Europe. Intl J STD AIDS. 2003;14:672–674. doi: 10.1258/095646203322387929. [DOI] [PubMed] [Google Scholar]
- 58.Manfredi R. Chiodo F. The effects of alternative treatments for HIV disease on recommended pharmacological regimens. Intl J Antimicrob Agents. 2000;13:281–285. doi: 10.1016/s0924-8579(99)00132-6. [DOI] [PubMed] [Google Scholar]
- 59.Agnoletto V. Chiaffarino F. Nasta P, et al. Use of complementary and alternative medicine in HIV-infected subjects. Complem Ther Med. 2006;14:193–199. doi: 10.1016/j.ctim.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 60.Knippels HM. Weiss JJ. Use of alternative medicine in a sample of HIV-positive gay men: An exploratory study of prevalence and user characteristics. AIDS Care. 2000;12:435–446. doi: 10.1080/09540120050123837. [DOI] [PubMed] [Google Scholar]
- 61.Vaszquez Hernandez M. Hurtado Gomez MF. Blanco JR. The influence of alternative medicine in highly active antiretroviral treatment. Farmacia Hospitalaria English Edition. 2009;33:31–36. [PubMed] [Google Scholar]
- 62.Thomas SL. Lam K. Piterman L, et al. Complementary medicine use among people living with HIV/AIDS in Victoria, Australia: Practices, attitudes and perceptions. Intl J STD AIDS. 2007;18:453–457. doi: 10.1258/095646207781147292. [DOI] [PubMed] [Google Scholar]
- 63.de Visser R. Grierson J. Use of alternative therapies by people living with HIV/AIDS in Australia. AIDS Care. 2002;14:599–606. doi: 10.1080/0954012021000005425. [DOI] [PubMed] [Google Scholar]
- 64.Greene KB. Berger J. Reeves C, et al. Most frequently used alternative and complementary therapies and activities by participants in the AMCOA Study. J Assoc Nurses in AIDS Care. 1999;10:60–73. doi: 10.1016/S1055-3290(05)60120-3. [DOI] [PubMed] [Google Scholar]
- 65.Eller LS. Bunch EH. Wantland DJ, et al. Prevalence, correlates, and self-management of HIV-related depressive symptoms. AIDS Care. 2010;22:1159–1170. doi: 10.1080/09540121.2010.498860. [DOI] [PubMed] [Google Scholar]
- 66.Kirksey KM. Goodroad BK. Kemppainen JK, et al. Complementary therapy use in persons with HIV/AIDS. J Holistic Nursing. 2002;20:264–278. doi: 10.1177/089801010202000306. [DOI] [PubMed] [Google Scholar]
- 67.Nightingale VR. Sher TG. Thilges S, et al. Non-conventional practices and immune functioning among individuals receiving conventional care for HIV. J Health Psychol. 2011;16:1241–1250. doi: 10.1177/1359105311405350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reeves C. Calabrese C. Standish LJ, et al. Screening alternative therapies for HIV. AIDS Patient Care STDs. 1998;12:87–89. doi: 10.1089/apc.1998.12.87. [DOI] [PubMed] [Google Scholar]
- 69.Chou FY. Testing a predictive model of the use of HIV/AIDS symptom self-care strategies. AIDS Patient Care STDs. 2004;18:109–117. doi: 10.1089/108729104322802533. [DOI] [PubMed] [Google Scholar]
- 70.de Visser R. Ezzy D. Bartos M. Alternative or complementary? Nonallopathic therapies for HIV/AIDS. Alt Ther Health Med. 2000;6:44–52. [PubMed] [Google Scholar]
- 71.Foote-Ardah CE. The meaning of complementary and alternative medicine practices among people with HIV in the United States: Strategies for managing everyday life. Sociol Health Illness. 2003;25:481–500. doi: 10.1111/1467-9566.00355. [DOI] [PubMed] [Google Scholar]
- 72.Foote-Ardah CE. Sociocultural barriers to the use of complementary and alternative medicine for HIV. Qual Health Res. 2004;14:593–611. doi: 10.1177/1049732304263639. [DOI] [PubMed] [Google Scholar]
- 73.Gillett J. Pawluch D. Cain R. How people with HIV/AIDS manage and assess their use of complementary therapies: A qualitative analysis. J Assoc Nurses AIDS Care. 2002;13:17–27. doi: 10.1016/S1055-3290(06)60198-2. [DOI] [PubMed] [Google Scholar]
- 74.Kremer H. Ironson G. Schneiderman N, et al. To take or not to take: Decision-making about antiretroviral treatment in people living with HIV/AIDS. AIDS Patient Care STDs. 2006;20:335–349. doi: 10.1089/apc.2006.20.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Langewitz W. Ruttimann S. Laifer G, et al. The integration of alternative treatment modalities in HIV infection: The patient's perspective. J Psychosom Res. 1994;38:687–693. doi: 10.1016/0022-3999(94)90021-3. [DOI] [PubMed] [Google Scholar]
- 76.McDonald K. Slavin S. My body, my life, my choice: Practices and meanings of complementary and alternative medicine among a sample of Australian people living with HIV/AIDS and their practitioners. AIDS Care. 2010;22:1229–1235. doi: 10.1080/09540121003668094. [DOI] [PubMed] [Google Scholar]
- 77.Mulkins A. Morse JM. Best A. Complementary therapy use in HIV/AIDS. Can J Public Health Rev Canadienne Sante Publique. 2002;93:308–312. doi: 10.1007/BF03405023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pawluch D. Cain R. Gillett J. Lay constructions of HIV and complementary therapy use. Soc Sci Med. 2000;51:251–264. doi: 10.1016/s0277-9536(99)00450-5. [DOI] [PubMed] [Google Scholar]
- 79.Rosenfeld BD. White M. Passik SD. Making treatment decisions with HIV infection: A pilot study of patient preferences. Med Decision Making. 1997;17:307–314. doi: 10.1177/0272989X9701700307. [DOI] [PubMed] [Google Scholar]
- 80.Thorpe RD. Integrating biomedical and CAM approaches: The experiences of people living with HIV/AIDS. Health Sociol Rev. 2008;17:410–418. [Google Scholar]
- 81.Wutoh AK. Brown CM. Dutta AP, et al. Treatment perceptions and attitudes of older human immunodeficiency virus co-infected adults. Res Soc Admin Pharm. 2005;1:60–76. doi: 10.1016/j.sapharm.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 82.Huber JT. Gullion JS. Complementary and alternative medicine as represented in the HIV/AIDS body of knowledge: A bibliometric analysis. Med Ref Serv Quart. 2003;22:23–32. doi: 10.1300/J115v22n03_03. [DOI] [PubMed] [Google Scholar]
- 83.Ernst J. Alternative treatment modalities in human immunodeficiency virus/acquired immune deficiency syndrome. Clin Infect Dis. 2003;37:S150–S153. doi: 10.1086/375881. [DOI] [PubMed] [Google Scholar]
- 84.Fulk LJ. Kane BE. Phillips KD, et al. Depression in HIV-infected patients: Allopathic, complementary, and alternative treatments. J PsychosomRes. 2004;57:339–351. doi: 10.1016/j.jpsychores.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 85.Hoogbruin A. Complementary and alternative therapy CAT (use and highly active antiretroviral therapy HAART): Current evidence in the literature, 2000–2009. J Clin Nursing. 2011;20:925–939. doi: 10.1111/j.1365-2702.2010.03322.x. [DOI] [PubMed] [Google Scholar]
- 86.Mills E. Wu P. Ernst E. Complementary therapies for the treatment of HIV: In search of the evidence. Intl J STD AIDS. 2005;16:395–403. doi: 10.1258/0956462054093962. [DOI] [PubMed] [Google Scholar]
- 87.Ozsoy M. Ernst E. How effective are complementary therapies for HIV and AIDs?–A systematic review. Intl J STD AIDS. 1999;10:629–635. doi: 10.1258/0956462991913088. [DOI] [PubMed] [Google Scholar]
- 88.Ridge D. Arachne J. From pharmaceuticals to alternative treatments for HIV/AIDS: What is the potential? Health Care Analysis. 1997;5:275–282. doi: 10.1007/BF02678525. [DOI] [PubMed] [Google Scholar]
- 89.Swanson B. Keithley JK. Zeller JM, et al. Complementary and alternative therapies to manage HIV-related symptoms. J Assoc Nurses AIDS Care. 2000;11:40–60. doi: 10.1016/S1055-3290(06)60384-1. [DOI] [PubMed] [Google Scholar]
- 90.Power R. Gore-Felton C. Vosvick M, et al. HIV: Effectiveness of complementary and alternative medicine. Primary Care: Clin Office Prac. 2002;29:361–378. doi: 10.1016/s0095-4543(01)00013-6. [DOI] [PubMed] [Google Scholar]
- 91.MacIntyre RC. Holzemer WL. Philippek M. Complementary and alternative medicine and HIV/AIDS. Part I: Issues and context. J Assoc Nurses AIDS Care. 1997;8:23–31. doi: 10.1016/S1055-3290(97)80035-0. [DOI] [PubMed] [Google Scholar]
- 92.MacIntyre RC. Holzemer WL. Complementary and alternative medicine and HIV/AIDS. Part II: Selected literature review. J Assoc Nurses AIDS Care. 1997;8:25–38. doi: 10.1016/S1055-3290(97)80016-7. [DOI] [PubMed] [Google Scholar]
- 93.Palmer R. Use of complementary therapies to treat patients with HIV/AIDS. Nursing Stand Royal Coll Nursing Great Britain 1987. 2008;22:35–41. doi: 10.7748/ns2008.08.22.50.35.c6641. [DOI] [PubMed] [Google Scholar]
- 94.Steinberg CL. Integrating traditional medicine with other therapies in the treatment of HIV-infected individuals. Maryland Med J: 1985. 1990;39:183–188. [PubMed] [Google Scholar]
- 95.Haddad A. Ethics in action. HIV patient wants “natural” therapy. RN. 2003;66:27–30. [PubMed] [Google Scholar]
- 96.Freeman EM. MacIntyre RC. Evaluating alternative treatments for HIV infection. Nursing Clin N Am. 1999;34:147–162. [PubMed] [Google Scholar]
- 97.Ernst E. The dark side of complementary and alternative medicine. Intl J STD AIDS. 2002;13:797–800. doi: 10.1258/095646202321020026. [DOI] [PubMed] [Google Scholar]
- 98.Gilmour J. Harrison C. Asadi L, et al. Natural health product-drug interactions: Evolving responsibilities to take complementary and alternative medicine into account. Pediatrics. 2011;128:S155–S160. doi: 10.1542/peds.2010-2720C. [DOI] [PubMed] [Google Scholar]
- 99.Ladenheim D. Horn O. Werneke U, et al. Potential health risks of complementary alternative medicines in HIV patients. HIV Med. 2008;9:653–659. doi: 10.1111/j.1468-1293.2008.00610.x. [DOI] [PubMed] [Google Scholar]
- 100.Leonard B. Huff H. Merryweather B, et al. Knowledge of safety and herb-drug interations amongst HIV+ individuals: A focus group study. Can J Clin Pharm. 2004;11:e227–e231. [PubMed] [Google Scholar]
- 101.Airoldi M. Zaccarelli M. Bisi L, et al. One-pill once-a-day HAART: A simplification strategy that improves adherence and quality of life of HIV-infected subjects. Patient Prefer Adher. 2010;4:115–125. doi: 10.2147/ppa.s10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.BHIVA. British HIV Association BHIVA guidelines for the treatment of HIV-infected adults with antiretroviral therapy. 2003. [PubMed]
- 103.BHIVA. British HIV Association BHIVA guidelines for the treatment of HIV-infected adults with antiretroviral therapy. 2005. [DOI] [PubMed]
- 104.Stebbing J. Bower M. Holmes P, et al. A single centre cohort experience with a new once daily antiretroviral drug. Postgrad Med J. 2006;82:343–346. doi: 10.1136/pgmj.2006.044867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hillier SL. Louw Q. Morris L, et al. Massage therapy for people with HIV/AIDS. Cochrane Database Syst Rev. 2010;1:CD007502. doi: 10.1002/14651858.CD007502.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Quandt SA. Verhoef MJ. Arcury TA, et al. Development of an international questionnaire to measure use of complementary and alternative medicine I-CAM-Q) J Altern Complem Med. 2009;15:331–339. doi: 10.1089/acm.2008.0521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Blair O'Connor B. Healing Traditions: Alternative Medicine and the Health Professions Studies in Health, Illness & Caregiving. University of Pennsylvania Press; Philadelphia: 1995. [Google Scholar]
- 108.Thorne S. Paterson B. Russell C, et al. Complementary/alternative medicine in chronic illness as informed self-care decision making. Intl J Nursing Studies. 2002;39:671–673. doi: 10.1016/s0020-7489(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 109.Truant T. McKenzie M. Discussing complementary therapies: There's more than efficacy to consider. CMAJ. 1999;160:351–352. [PMC free article] [PubMed] [Google Scholar]
- 110.Swendeman D. Ingram BL. Rotheram-Borus MJ. Common elements in self-management of HIV and other chronic illnesses: An integrative framework. AIDS Care. 2009;21:1321–1334. doi: 10.1080/09540120902803158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gifford AL. Groessl EJ. Chronic disease self-management and adherence to HIV medications. JAIDS. 2002;31:S163–S166. doi: 10.1097/00126334-200212153-00016. [DOI] [PubMed] [Google Scholar]
- 112.Wynia MK. Eisenberg DM. Wilson IB. Physician-patient communication about complementary and alternative medical therapies: A survey of physicians caring for patients with human immunodeficiency virus infection. J Alt Complem Med. 1999;5:447–456. doi: 10.1089/acm.1999.5.447. [DOI] [PubMed] [Google Scholar]
- 113.NAM. Combining conventional and complementary therapies. http://www aidsmap com/Combining-conventional-and-complementary-therapies/page/1254995/2013. [Jul 4;2013 ]. http://www aidsmap com/Combining-conventional-and-complementary-therapies/page/1254995/2013