Abstract
The tunnel restoration has been suggested as a conservative alternative to the conventional box preparation for treating proximal caries. The main advantage of tunnel restoration over the conventional box or slot preparation includes being more conservative and increasing tooth integrity and strength by preserving the marginal ridge. However, tunnel restoration is technique-sensitive and can be particularly challenging for inexperienced restorative dentists. Recent advances in technology, such as the contemporary design of dental handpieces with advanced light-emitting diode (LED) and handheld comfort, offer operative dentists better vision, illumination, and maneuverability. The use of magnifying loupes also enhances the visibility of the preparation. The advent of digital radiographic imaging has improved dental imaging and reduced radiation. The new generation of restorative materials has improved mechanical properties. Tunnel restoration can be an option to restore proximal caries if the dentist performs proper case selection and pays attention to the details of the restorative procedures. This paper describes the clinical technique of tunnel restoration and reviews the studies of tunnel restorations.
Keywords: operative, practice, tunnel preparation, composite, amalgam, glass ionomer
Introduction
Caries is a common oral disease caused by demineralization of tooth structure, which is caused by acid produced by bacteria in the presence of fermentable carbohydrates.1 When this occurs in the proximal area, carious lesions are often located just below the contact point. Proximal caries can be difficult to detect by visual inspection alone, and diagnostic aids include bitewing radiographs, fiber-optic light transillumination, and quantitative light (or laser) induced fluorescence.2 When proximal caries progress extensively into dentin, traditional restoration requires removal of the intact marginal ridge to gain access to the carious lesion beneath. Contemporary caries management involves minimally invasive cavity preparation design, which can be “slot” or “box-only,” as well as “tunnel” and “saucer-shaped” preparations.3
The tunnel preparation was first reported in the 1960s for restoring distal proximal caries of a primary second molar, accessing caries beneath the marginal ridge and thus leaving it intact.4 In the 1980s, tunnel preparation was reintroduced with the use of glass ionomer cement.5,6 Kinomoto et al7 reported that the 2-year clinical success rate of composite tunnel restorations was 96%, which had no significant difference with that of conventional composite slot restoration. The advantage of tunnel restoration over the conventional box or slot preparation includes being more conservative and increasing tooth integrity and strength by preserving the marginal ridge.8 If caries turns out to be more extensive than predicted, or the marginal ridge is at risk of fracture, then the tunnel preparation can be converted to a conventional design. However, the tunnel preparation is technique-sensitive and can be difficult to prepare, particularly for inexperienced clinicians. The marginal ridge can be undermined, resulting in fracture. Recurrent caries caused by the insufficient caries removal, due to the limited access, remains a key concern in the technique, as well as inadequacy in filling the cavity. Pyk and Mejara9 reported that the most common cause of failure was caries found clinically or radiographically adjacent to the tunnel restoration. They also demonstrated that the only factor significantly associated with failure was tooth type, with molars five times more likely to fail than premolars. Another concern is that, in attempting to preserve the marginal ridge and approaching interproximal caries from the occlusal surface away from the ridge, tunnel preparation can endanger pulpal tissues. An early study reported that tunnel preparation often invaded to within 1.0 mm of the pulp, whereas conventional Class II left greater remaining dentinal thickness between the preparation and the pulp.10
There are different types of tunnel preparations described in the literature.4 They differ mainly in whether the proximal enamel is retained. An internal tunnel preparation does not involve the proximal enamel and is actually a Class I cavity. The partial tunnel preparation extends to proximal surface into the cavitation or where enamel disintegrated during cavity preparation, leaving some demineralized enamel adjacent to filling. The proximal enamel is either slightly perforated or not perforated. The total tunnel involves the complete removal of demineralized enamel, with the proximal area perforated.4
Glass ionomer cement could be a material of choice for tunnel preparation because it bonds to enamel and dentine, in addition to releasing fluoride.11 However, it may not be strong enough to withstand the occlusal biting force, and many clinicians have reservations using it as permanent restoration in the adult dentition. Composite resin offers better strength in comparison with glass ionomer.12 It also bonds with dentine and enamel and is therefore a good material for definite restorations. Silver amalgam can also be used as it offers good strength and is easy to handle. This paper aims to perform a literature review of clinical studies of this technique and utilizes two cases to illustrate the restoration of proximal carious lesions with tunnel technique, using sandwich technique (glass ionomer and composite) and silver amalgam.
Literature review
A literature search was performed using PubMed on clinical study in English with the keywords: “tunnel restoration” and “tooth or tunnel preparation” and “tooth” (Figure 1). An additional hand search was performed on references of the papers on tunnel restoration. This review included 18 clinical trials, which are summarized in Table 1. Clinical studies showed that the clinical success rate for tunnel restorations with glass ionomer varied from 100% after 3 years13 to 90% after 3.5 years,14 with the median survival rate of 6 years.15 The long-term success rate varied from 46% after 8.5 years16 to 85% after 8 years.17 The enhanced visibility by use of dental handpieces with light-emitting diodes (LEDs) and magnifying loupes in modern dentistry could provide a better clinical outcome. Wiegand and Attin8 performed a review and could not find a significant difference in the prognosis and success of the restorations with regards to tooth type, lesion size, and the kind of tunnel restorations performed. However, the material selected for restoration, amount of the marginal ridge retained, and caries activity of the patient could be significant factors affecting the clinical success. The restorations were deemed as failed if: (1) the marginal ridge was fractured; (2) recurrent caries were detected; (3) caries had progressed; or (4) the restoration was replaced.8 Of all of the reasons for failure reported in the literature, the main reasons for failure were due to marginal ridge fracture and caries.
Figure 1.
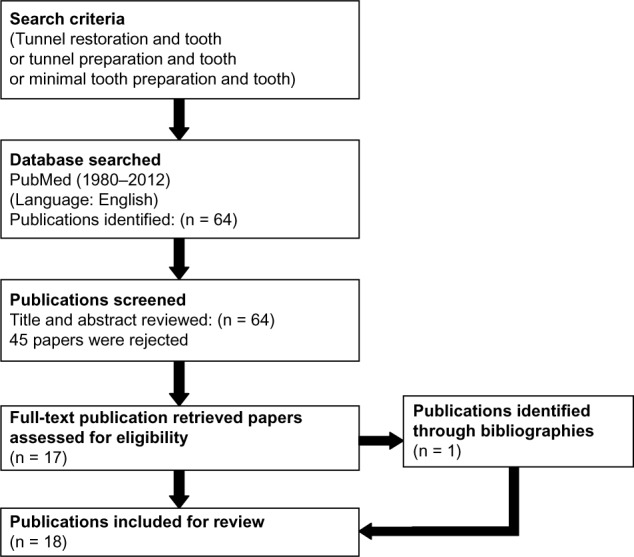
Flowchart of literature search and selection.
Table 1.
Clinical evaluations of tunnel restoration
| Study | Method | Main findings |
|---|---|---|
| Svanberg36 | 18 adolescents had both glass ionomer tunnel restoration and Class II amalgam restoration and were followed up for 3 years. | Less caries developed on the tooth adjacent to tunnel glass ionomer restoration than the amalgam restoration. |
| Hasselrot14 | 318 glass ionomer or composite tunnel restorations from 224 patients were followed up for 3.5 years. | The success rate was 74% in permanent teeth and 10% in primary teeth. |
| Wilkie et al37 | 86 glass cermet tunnel restorations of 26 adults were followed up for 2 years. | Filling defects, surface voids, and occlusal wear with surface crazing and cracking were found in 48% of the restorations. |
| Zenkner et al38 | 51 glass cermet restorations of tunnel type with cermet were followed up for 2 years. | The failures were marginal ridges fractured (4.2%), occlusal wear (4.2%), and white spots lesions (53.8%). |
| de Freitas et al33 | 66 composite tunnel restorations were followed up for 1 year. | All restorations were present. There was no visible wear, no recurrent caries, and no fractures at the marginal crest. |
| Lumley and Fisher13 | 33 glass ionomer tunnel restorations and 14 amalgam restorations on premolar or first molar teeth were followed up for 1 year. | Restorations in both groups were satisfactory after 3 years. The failure rate was 25% after 5 years. |
| Strand et al31 | 161 glass ionomer tunnel restorations were followed up for an average of 3 years. | A high failure rate of restorations was found in patients with high caries activity. |
| Hasselrot22 | 35 glass cermet tunnel restorations in permanent teeth were followed up for up to 7 years. | Annual failure rate was 7%. 50% survival time was 6 years. The failures were mainly marginal ridge facture and caries. |
| Holst and Brannstrom21 | 302 tunnel glass cermet restorations were followed up for 3 years. | The failure rate of restorations was 7%, 10%, and 16% after 1, 2, and 3 years, respectively. |
| Jones17 | 50 glass-ionomer tunnel restorations in 48 patients were followed up for 8 years. | The failure rate was 15%. |
| Pyk and Mejara9 | 242 tunnel restorations in 142 patients were followed up for 2 years. | The success rate was not related to caries activity and did not differ between the two types of tunnel preparation. |
| Nicolaisen et al15 | 182 glass ionomer tunnel restorations from 94 patients were followed up for up to 5 years. | The failure rate was 10% after 3 years and 65% after 5 years. |
| Strand et al18 | 420 glass ionomer tunnel restorations from 179 patients were followed up for up to 4.5 years. | The failure rate was 43%. |
| Pilebro et al30 | 374 glass cermet tunnel restorations were followed up for 3 years. | The failure rate was 20%. The failures were marginal fracture and caries. |
| Odman35 | 89 tunnel restorations of 68 patients were followed up for 3 years. | 19% of the marginal ridges had fractured. |
| Kinomoto et al7 | 63 tunnel restoration or proximal composite restorations from 38 patients were followed up for 2 years. | All restorations were clinically satisfactory (successful rate: 96%). |
| Horsted-Bindslev et al16 | 85 glass ionomer tunnel restorations and 97 composite restorations were followed up for 8.5 years. | The survival rate of glass ionomer tunnel restorations was 46%, and for 97 composite restorations was 76%. |
| Markovic and Peric34 | 233 glass-ionomer tunnel restorations from 203 children were followed up for 3 years. | Survival rate was 72%. The failures were endodontic compilations, caries, and marginal ridge fractures. |
Case selection
Case selection can be critical for the success of this restorative technique. Strand et al18 reported a higher failure rate of glass ionomer tunnel restorations in patients with high caries activity. This is also suggested by Ratledge et al4 who found that people with high caries activity had high risk of secondary caries.4 This may be due to the design of tunnel preparation, which does not clear the proximal contact, and the restorative margin in the proximal contact is subjected to cariogenic challenge by the plaque sheltered below the contact point.
Status of the marginal ridge
Since fracture resistance of a tooth is closely connected to strength of the marginal ridge,19 the amount of marginal ridge retained after the tunnel preparation plays a key role in its success. It was found that the distance from the marginal ridge had more influence on weakening the ridge than did extension of the occlusal opening.20 Another study reported that the amount of marginal ridge retained was related to the strength of the tooth after placing the restoration. It was shown that 2.5 mm was the critical amount, and that strength of the tooth with tunnel restoration would be comparable to that of a sound tooth.19 A brittle layer of enamel would fracture due to inadequate support from dentine if the cavity preparation was too close to the ridge, and, if 3.5 mm of marginal ridge is retained, the preparation would involve excessive removal of dentine. The resulting tunnel preparation could be more sensitive to fatigue crack growth.
Caries extension and type of tunnel preparation
Caries extension affects the clinician’s decision to perform partial or total tunnel preparation. Studies by Holst and Brannstrom21 and Hasselrot22 found that partial tunnel preparations have higher fracture resistance, which could be related to the size of preparation. The partial tunnel preparation extends to the proximal surface into the cavitation or where enamel disintegrated during cavity preparation, leaving some demineralized enamel adjacent to the filling. Some clinicians are concerned with the demineralized enamel that is left. Therefore, this factor remains controversial regarding its role in the clinical success of the restoration. The total tunnel preparation involves more extensive removal of tooth structure, thereby reducing the fracture resistance. Caries extension and activity of the patient should perhaps be considered during case selection, which is important in the clinical success of the tunnel restoration.
Report of cases
Case 1 – treatment with silver amalgam restoration
A patient came to see his dentist (CHC). He presented with distal caries on tooth 36 that was evident on the bitewing radiograph (Figure 2). Rubber dam was placed and stabilized with rubber dam clamp number 7, which did not impinge on the gingival soft tissue (Figure 3). A small access cavity was made through the occlusal fossa about 2 mm away from marginal ridge using the tapered diamond bur (Jota Diamond #837, JOTA AG, Rüthi, SG, Switzerland) angled axially once into dentine. An ovoid preparation was created (Figure 4) where residual caries could be obviously detected with magnifying loupes. A small diamond round bur (Jota Diamond #801, JOTA AG) was then used for further caries removal, and unsupported enamel was trimmed with an excavator. After the Tofflemire matrix band and wooden wedge were placed, a dentin bonding agent (Clearfil Liner Bond 2, Kuraray Co, Ltd, Tokyo, Japan) that bonded to the silver amalgam was applied. The cavity was then overfilled with silver amalgam (Tytin FC, Kerr Corporation, Orange, CA, USA) (Figure 5). Precarving burnishing was performed, and the excess silver amalgam was removed by carver (Figure 6). The occlusion was checked, and postoperative radiograph was taken showing the integrity of the restoration (Figure 7). The good handling properties of amalgam allow proper condensation to the prepared cavity with lateral extension. This could be challenging when restoring with glass ionomer or composite resin because these materials are difficult to “pack” into the tunnel preparation with limited access.
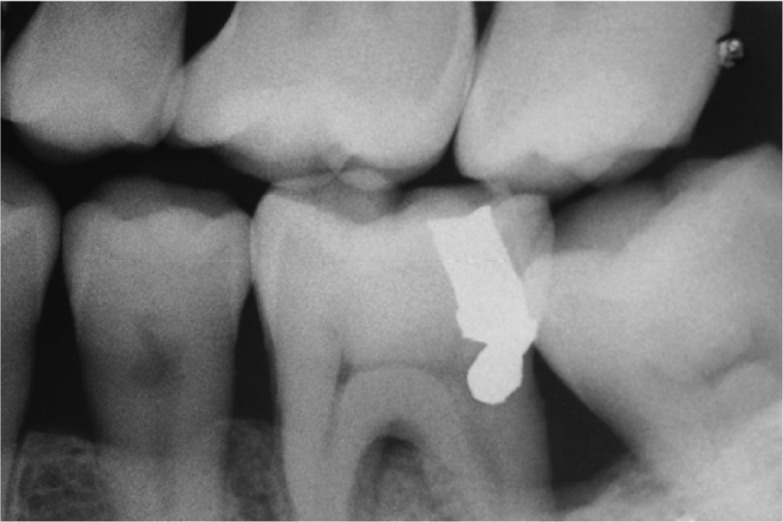
Figure 2.

Radiograph showing caries on 36D.
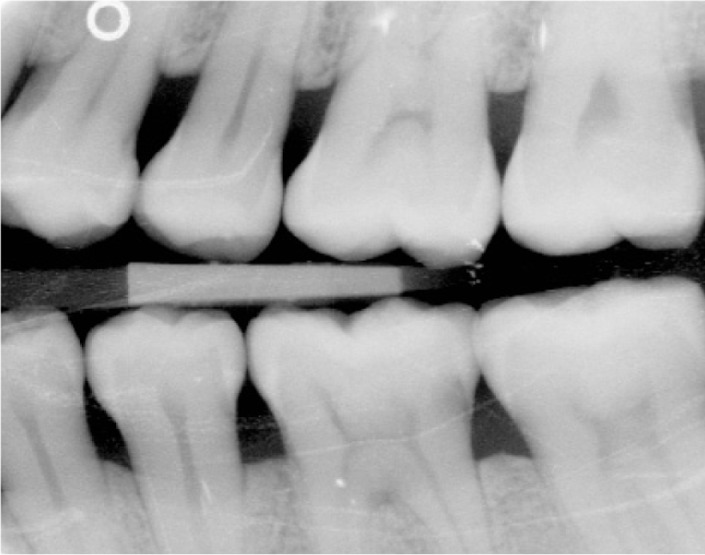
Figure 3.

Rubber dam isolation.
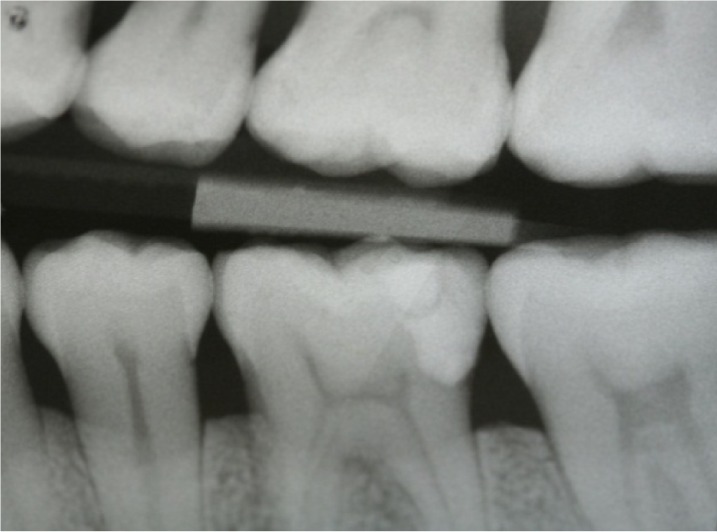
Figure 4.

Tunnel preparation access.
Figure 5.

Overfilled with amalgam.
Figure 6.

Finished amalgam tunnel restoration.
Figure 7.
Post-operative radiograph.
Case 2 – treatment with sandwich composite resin/glass ionomer restoration
A patient came to see her dentist (CHC). She presented with distal caries on tooth 36, which was evident on the bitewing radiograph (Figure 8). After the placement of the rubber dam for moisture control (Figure 9), an ovoid access opening was created with tapered diamond bur (Figure 10). Residual caries was removed with round bur. After placing the Tofflemire matrix band and wooden wedge, the cavity was conditioned with 20% polyacrylic acid (Ketac Conditioner, 3M Company, St Paul, MN, USA) for 15 seconds, then washed thoroughly with water and dried with oil-free air. The cavity was filled with highly viscous glass ionomer cement (Ketac Molar, 3M Company) and could be gently condensed with a condenser to form a flat base of the preparation (Figure 11). The wall of the cavity and occlusal fissures were etched with 35% phosphoric acid for 15 seconds before application of dentine bonding adhesive (Scotchbond, 3M Company). Universal Restorative composite resin (Filtek Z250, 3M Company) was then placed in small increments to reduce the polymerization shrinkage and ensure the marginal integrity of the proximal restoration (Figure 12). The surface and the etched fissures were covered with a thin layer of fissure sealant (Clinpro Pit and Fissure Sealant, 3M Company). After checking the occlusion, a postoperative radiograph was taken to evaluate the integrity of the restoration (Figure 13).
Figure 8.
Radiograph showing caries on 36D.
Figure 9.

Rubber dam isolation.
Figure 10.

Tunnel preparation access.
Figure 11.

Glass ionomer used as base.
Figure 12.

Finished sandwich tunnel restoration.
Figure 13.
Post-operative radiograph.
Discussion
Magnifying loupes were used to improve the operator’s ability to visualize the extent of the lesion.23 Thus, better preparation of the access to the carious lesion may be possible, and more thorough caries removal may result. The area most difficult for caries removal is beneath the marginal ridge.24 The magnifying loupes also allow for the marginal ridge to be checked for fine crack lines prior to placing the restoration. Marginal ridges can develop crack lines prior to or during cavity preparation and can fracture after the restoration.25 In addition, overhangs may be formed on Class II composite resin restorations, and Frankenberger et al26 reported that the use of magnifying loupes was beneficial for reducing marginal overhangs by up to 40% in standard Class II restorations. The rubber dam was placed not only for moisture control, but also to improve visibility for the preparation and restorative procedures.
Apart from being conservative in preparation, the other main reason for tunnel preparation is to preserve the intact marginal ridge, which is important to prevent the restored tooth from fracture.27 Ji et al19 reported that, when a 2.5 mm marginal ridge was conserved in tunnel preparation, the tooth would be as strong as sound teeth against fracture. The angulation of the access is also important. The cavity design should start at about 2.5 mm from the marginal ridge, and ovoid access may extend buccolingually, parallel to the marginal ridge and along the central fissure away from the margin to form a “T” pattern on the occlusal surface. This may enhance the diagnosis of the carious involvement of the tooth. It is noteworthy that the access should not be too far from the marginal ridge as it is less conservative. Additionally, due to angulation, a tunnel preparation can be too close to the pulp if not conservatively prepared. If the tooth was previously restored with an occlusal restoration, removing existing restoration will also facilitate access and increase the visibility.25
Use of adhesive restorative material was also shown to help restore the strength of the marginal ridge.20 Dentine bonding adhesives such as Clearfil Liner Bond 2 (Kuraray Co, Ltd) or Scotchbond Multipurpose (3M Company) can be applied to enhance bonding between dentine and composite resin or silver amalgam. The matrix band and wooden wedge were used for better adaptation to the proximal margin. New matrix bands such as Slick Bands Matrix Kit (Garrison Dental Solutions, Inc, Übach-Palenberg, Germany) are available to provide a very thin (35.6 μm or 0.0014″) nonstick Tofflemire-style matrix band for every type of restoration. The matrix has a coating that eliminates bonding agent and composite adhesion to the matrix, and thus simplifies matrix removal. Deliperi28 demonstrated a restorative method for ultraconservative posterior restorations using a modified matrix band design.
In addition to the concern regarding the fracture resistance of the restored tooth, a common reason for failure is recurrent caries.29 Incomplete removal of caries can be due to the inadequate visibility by inadequate access during the preparation. The area most difficult for caries removal is beneath the marginal ridge.8 In vitro studies of tunnel technique restorations that failed due to caries demonstrated that up to 17% failed due to carious dentin next to the dentino-enamel junction.8 Strand et al24 reported that instruction and training did not seem to influence the efficacy of caries removal. It is noteworthy that the study was conducted approximately 20 years ago, when magnifying loupes were not used by the majority for dental operative procedures. Significant advances in dental handpieces are also emerging with light-emitting diodes (LEDs), which provide superior intraoral illumination to enhance visibility. Finally, radiographic imaging has also improved with the advent of digital radiography.
Tunnel restoration is highly technique-sensitive. A multicenter study found that the operator’s skill was a significant factor in success.30 Kinomoto et al7 also reported a high success rate of tunnel restorations performed by experienced operators. These findings also demonstrated that tunnel restoration is not only technique-sensitive, but that it may also explain the different success rate reported by the clinical studies.31,7
The two cases reported use of silver amalgam and sandwich composite resin/glass ionomer for tunnel restorations. Silver amalgam has a good compressive strength and was used on a patient whose esthetic demand was not high. Aside from its strength, silver amalgam is easy to handle and condense into the cavity. Its good handling properties allow clinicians to achieve solid interproximal contact of the tunnel restoration. Composite resin is a popular definitive restorative material due to increasing esthetic demand by patients. The composite resin used for posterior restorations should consist of high filler content for good compressive strength. Tunnel preparation restored with composite resin was shown to achieve a comparable strength to that of the original tooth.7 However, composite restoration is technique-sensitive. Proper bonding technique and good moisture control are critical for the longevity of the restoration. For better adaptation and marginal integrity, the polymerization shrinkage must be minimized through restoring the tooth in incremental layers.25 Incremental layering is often difficult in tunnel restoration because the access is limited. Thus, a highly viscous glass ionomer can be used as dentine replacement to restore the bulk of the prepared cavity. Glass ionomer cement has little dimensional change on setting and a similar coefficient of thermal expansion. It also bonds to dentin and releases fluoride to reduce risk of recurrent caries development. However, an occlusal access cavity should be sealed with composite resin to prevent wear of the underlying glass ionomer. Selecting suitable cases for tunnel restoration enhances esthetics and minimizes tooth damage, and thus increases patient satisfaction.32
Conclusion
Restoring proximal caries using tunnel technique is a viable and conservative permanent restoration, but case selection and clinician ability are important factors affecting success. The use of magnifying loupes, digital radiography, and dental handpieces with LED light are suggested to help clinicians visualize the carious lesion and perform precise preparation. The preserved marginal ridge can maintain the fracture resistance of the restored tooth. Patient factors also play a role in clinical success. The advantages and disadvantages of this preparation technique should be considered, and the clinician should use his or her experience and judgment before selecting this treatment option.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chu CH. Treatment of early childhood caries: a review and case report. Gen Dent. 2000;48(2):142–148. [PubMed] [Google Scholar]
- 2.Chu CH, Lo EC, You DS. Clinical diagnosis of fissure caries with conventional and laser-induced fluorescence techniques. Lasers Med Sci. 2010;25(3):355–362. doi: 10.1007/s10103-009-0655-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mount GJ. Minimal intervention dentistry: rationale of cavity design. Oper Dent. 2003;28(1):92–99. [PubMed] [Google Scholar]
- 4.Ratledge DK, Kidd EA, Treasure ET. The tunnel restoration. Br Dent J. 2002;193(9):501–506. doi: 10.1038/sj.bdj.4801609. [DOI] [PubMed] [Google Scholar]
- 5.Hunt PR. A modified class II cavity preparation for glass ionomer restorative materials. Quintessence Int. 1984;15(10):1011–1018. [PubMed] [Google Scholar]
- 6.Knight GM. The use of adhesive materials in the conservative restoration of selected posterior teeth. Aust Dent J. 1984;29(5):324–331. doi: 10.1111/j.1834-7819.1984.tb05294.x. [DOI] [PubMed] [Google Scholar]
- 7.Kinomoto Y, Inoue Y, Ebisu S. A two-year comparison of resin-based composite tunnel and Class II restorations in a randomized controlled trial. Am J Dent. 2004;17(4):253–256. [PubMed] [Google Scholar]
- 8.Wiegand A, Attin T. Treatment of proximal caries lesions by tunnel restorations. Dental Materials. 2007;23(12):1461–1467. doi: 10.1016/j.dental.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Pyk N, Mejara I. Tunnel restorations in general practice. Influence of some clinical variables on success rate. Acta Odontol Scand. 1999;57(4):195–200. doi: 10.1080/000163599428779. [DOI] [PubMed] [Google Scholar]
- 10.Papa J, Cain C, Messer HH, Wilson PR. Tunnel restorations versus Class II restorations for small proximal lesions: A comparison of tooth strengths. Quintessence Int. 1993;24(2):93–98. [PubMed] [Google Scholar]
- 11.Chu CH, King NM, Lee AM, Yiu CK, Wei SH. A pilot study of the marginal adaptation and surface morphology of glass-cermet cements. Quintessence Int. 1996;27(7):493–501. [PubMed] [Google Scholar]
- 12.Chu CH, Zhang CF, Jin LJ. Treating a maxillary midline diastema in adult patients: a general dentist’s perspective. J Am Dent Assoc. 2011;142(11):1258–1264. doi: 10.14219/jada.archive.2011.0110. [DOI] [PubMed] [Google Scholar]
- 13.Lumley PJ, Fisher FJ. Tunnel restorations: a long-term pilot study over a minimum of five years. J Dent. 1995;23(4):213–215. doi: 10.1016/0300-5712(95)91185-p. [DOI] [PubMed] [Google Scholar]
- 14.Hasselrot L. Tunnel restorations. A 3 1/2-year follow-up study of Class I and II tunnel restorations in permanent and primary teeth. Swed Dent J. 1993;17(5):173–182. [PubMed] [Google Scholar]
- 15.Nicolaisen S, der Fehr FR, Lunder N, Thomsen I. Performance of tunnel restorations at 3–6 years. J Dent. 2000;28(6):383–387. doi: 10.1016/s0300-5712(00)00024-5. [DOI] [PubMed] [Google Scholar]
- 16.Horsted-Bindslev P, Heyde-Petersen B, Simonsen P, Baelum V. Tunnel or saucer-shaped restorations: a survival analysis. Clin Oral Investigig. 2005;9(4):233–238. doi: 10.1007/s00784-005-0011-6. [DOI] [PubMed] [Google Scholar]
- 17.Jones SE. The theory and practice of internal ‘tunnel’ restorations: a review of the literature and observations on clinical performance over eight years in practice. Prim Dent Care. 1999;6(3):93–100. [PubMed] [Google Scholar]
- 18.Strand GV, Nordbo H, Leirskar J, der Fehr FR, Eide GE. Tunnel restorations placed in routine practice and observed for 24–54 months. Quintessence Int. 2000;31(7):453–460. [PubMed] [Google Scholar]
- 19.Ji W, Chen Z, Frencken JE. Strength of tunnel-restored teeth with different materials and marginal ridge height. Dent Mater. 2009;25(11):1363–1370. doi: 10.1016/j.dental.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Fasbinder DJ, Davis RD, Burgess JO. Marginal ridge strength in Class II tunnel restorations. Am J Dent. 1991;4(2):77–82. [PubMed] [Google Scholar]
- 21.Holst A, Brannstrom M. Restoration of small proximal dentin lesions with the tunnel technique. A 3-year clinical study performed in Public Dental Service clinics. Swed Dent J. 1998;22(4):143–148. [PubMed] [Google Scholar]
- 22.Hasselrot L. Tunnel restorations in permanent teeth. A 7-year follow-up study. Swed Dent J. 1998;22(1–2):1–7. [PubMed] [Google Scholar]
- 23.James T, Gilmour AS. Magnifying loupes in modern dental practice: an update. Dent Update. 2010;37(9):633–636. doi: 10.12968/denu.2010.37.9.633. [DOI] [PubMed] [Google Scholar]
- 24.Strand GV, Tveit AB, Espelid I. Variations among operators in the performance of tunnel preparations in vitro. Scand J Dent Res. 1994;102(3):151–155. doi: 10.1111/j.1600-0722.1994.tb01171.x. [DOI] [PubMed] [Google Scholar]
- 25.Knight GM. The tunnel restoration – nine years of clinical experience using capsulated glass ionomer cements. Case report. Aust Dent J. 1992;37(4):245–251. doi: 10.1111/j.1834-7819.1992.tb04738.x. [DOI] [PubMed] [Google Scholar]
- 26.Frankenberger R, Krämer N, Pelka M, Petschelt A. Internal adaptation and overhang formation of direct Class II resin composite restorations. Clin Oral Investigig. 1999;3(4):208–215. doi: 10.1007/s007840050103. [DOI] [PubMed] [Google Scholar]
- 27.Xie KX, Wang XY, Gao XJ, Yuan CY, Li JX, Chu CH. Fracture resistance of root filled premolar teeth restored with direct composite resin with or without cusp coverage. Int Endod J. 2012;45(6):524–529. doi: 10.1111/j.1365-2591.2011.02005.x. [DOI] [PubMed] [Google Scholar]
- 28.Deliperi S. Modified matrix band design for ultra-conservative posterior restorations. Oper Dent. 2008;33(3):356–360. doi: 10.2341/07-126. [DOI] [PubMed] [Google Scholar]
- 29.Chu CH, Chow TW. Esthetic designs of removable partial dentures. Gen Dent. 2003;51(4):322–324. [PubMed] [Google Scholar]
- 30.Pilebro CE, van Dijken JW. Analysis of factors affecting failure of glass cermet tunnel restorations in a multi-center study. Clin Oral Investig. 2001;5(2):96–101. doi: 10.1007/s007840100106. [DOI] [PubMed] [Google Scholar]
- 31.Strand GV, Tveit AB, Eide GE. Cavity design and dimensions of tunnel preparations versus composite resin Class-II preparations. Acta Odontol Scand. 1995;53(4):217–221. doi: 10.3109/00016359509005975. [DOI] [PubMed] [Google Scholar]
- 32.Chu CH, Yeung CY, Lo EC. Monitoring patient satisfaction with university dental services under two fee-paying systems. Community Dent Oral Epidemiol. 2001;29(5):390–398. doi: 10.1034/j.1600-0528.2001.290509.x. [DOI] [PubMed] [Google Scholar]
- 33.de Freitas AR, de Andrada MA, Baratieri LN, Monteiro Junior S, de Sousa CN. Clinical evaluation of composite resin tunnel restorations on primary molars. Quintessence Int. 1994;25(6):419–424. [PubMed] [Google Scholar]
- 34.Markovic D, Peric T. Clinical evaluation of glass-ionomer tunnel restorations in primary molars: 36 months results. Aust Dent J. 2008;53(1):41–45. doi: 10.1111/j.1834-7819.2007.00007.x. [DOI] [PubMed] [Google Scholar]
- 35.Odman P. A 3-year clinical evaluation of Cerana prefabricated ceramic inlays. Int J Prosthodont. 2002;15(1):79–82. [PubMed] [Google Scholar]
- 36.Svanberg M. Class II amalgam restorations, glass-ionomer tunnel restorations, and caries development on adjacent tooth surfaces: a 3-year clinical study. Caries Res. 1992;26(4):315–318. doi: 10.1159/000261459. [DOI] [PubMed] [Google Scholar]
- 37.Wilkie R, Lidums A, Smales R. Class II glass ionomer cermet tunnel, resin sandwich and amalgam restorations over 2 years. Am J Dent. 1993;6(4):181–184. [PubMed] [Google Scholar]
- 38.Zenkner JE, Baratieri LN, Monteiro SJ, de Andrada MA, Vieira LC. Clinical and radiographic evaluation of cermet tunnel restorations on primary molars. Quintessence Int. 1993;24(11):783–791. [PubMed] [Google Scholar]
- 39.Ratledge DK, Kidd EA, Beighton D. A clinical and microbiological study of approximal carious lesions. Part 2: efficacy of caries removal following tunnel and class II cavity preparations. Caries Res. 2001;35(1):8–11. doi: 10.1159/000047424. [DOI] [PubMed] [Google Scholar]


