Abstract
Weight loss reduces energy expenditure, but it is unclear whether dietary macronutrient composition affects this reduction. We hypothesized that energy expenditure might be modulated by macronutrient composition of the diet. The POUNDS LOST study, a prospective, randomized controlled trial in 811 overweight/obese people who were randomized in a 2×2 design to diets containing 20en% or 40en% fat and 15en% or 25en% (diets with 65%, 55%, 45% and 35% carbohydrate) provided the data to test this hypothesis. Resting energy expenditure (REE) was measured at baseline, 6 and 24 months using a ventilated hood. REE declined at 6 months by 99.5±8.0 kcal/d in men and 55.2±10.6 kcal/d in women during the first 6 months. This decline was related to the weight loss, and there was no difference between the diets. REE had returned to baseline by 24 months, but body weight was still 60% below baseline. Measured REE at 6 months was significantly lower than the predicted (−18.2±6.7 kcal/d) and was the result of significant reductions from baseline in the low fat diets (65% or 55% carbohydrate), but not in the high fat diet groups. By 24 months the difference had reversed with measured REE being slightly but significantly higher than predicted (21.8±10.1 kcal/d). In conclusion, we found that REE fell significantly after weight loss but was not related to diet composition. Adaptive thermogenesis was evident at 6 months, but not at 24 months.
Introduction
The prevalence of obesity is increasing in the US, which is the result of a small positive energy balance in individuals that occurs over an extended time period (1, 2). Since energy intake comes from the food and beverages we eat, dietary recommendations to lose and maintain weight loss have been a cornerstone in the treatment of obesity. Many different diets have been recommended (3) and a number of studies have compared whether one or another diet produces more weight loss, seeking an approach to make it easier to lose weight and sustain weight losses (4–7).
Targeting macronutrient composition of diets is based on the effect that increasing dietary protein intake might have on metabolic rate or satiety. A recent study showed that resting energy expenditure was increased by dietary protein during overfeeding (8). Dietary protein might also increase satiety (9).
The Prevention of Obesity Using Novel Dietary Strategies (POUNDS) LOST Study was the largest study yet to compare the effects of diets with different macronutrient composition on weight loss. In this trial 811 overweight or obese individuals were randomized in a 2 by 2 factorial design to one of 4 diets that contained either 20% or 40% fat and either 15% or 25% protein. They were followed for 2 years. There was no difference in weight loss by diet assignment or in comparing high versus average protein, or high versus low fat diet assignment.
In a sub-study of 99 individuals in POUNDS LOST, measurement of total energy expenditure by doubly-labeled water showed a decrease during weight loss (10). The decrease in energy expenditure could be accounted for primarily by the decrease in resting energy expenditure. In the POUNDS LOST study, resting energy expenditure was measured at baseline to predict energy needs, and was measured again at 6 and 24 months. This paper reports the relation of resting energy expenditure to diet composition and weight loss.
Methods
The design of the POUNDS LOST study has been presented in detail elsewhere (4). Briefly, it was a randomized clinical trial (NCT00072995) comparing the effects on body weight of four energy-reduced diets that differed in their targets for macronutrients. The trial was conducted at two sites, one in Boston at the Harvard School of Public Health and Brigham & Women’s Hospital; and the other in Baton Rouge at the Pennington Biomedical Research Center of the Louisiana State University System. The data coordinating center was at the Brigham & Women’s Hospital, and there was participation of National Heart, Lung, and Blood Institute (NHLBI) project staff.
Participants
The goal was to recruit 800 overweight and obese participants, 400 at each site, with 40% men, aged 30–70 yrs, body mass index between 25 kg/m2 and ≤40 kg/m2. Major exclusions were diabetes, unstable cardiovascular disease, use of medications that affect body weight, or insufficient motivation as assessed by interviews and questionnaires at screening. The study was approved by the human subjects committees at each institution and participants gave written informed consent. They were informed that they would be randomly assigned to one of 4 diets. Mass mailings were the primary means of recruitment using lists of registered voters or drivers. Randomization assignments were generated by the data manager at the coordinating center upon request of a study dietitian and after confirming eligibility.
Protocol
The details of the design, dietary intervention, and results have been published (4). Briefly, at the completion of screening and baseline measurements volunteers were randomly assigned to one of four dietary treatment groups, using a factorial design with high or low fat diets and high or average protein diets. These diets were as follows: 1) Low fat/average protein (20% fat/15% protein = LF/AP); 2) Low fat/high protein (20% fat/25% protein = LF/HP); 3) High fat/average protein (40% fat/15% protein = HF/AP) or 4) High fat/high protein (40% fat/25% protein = HF/HP). These 4 diets thus had a graded carbohydrate composition of 65%, 55%, 45% and 35%. The volunteers were initially given individual instruction in their dietary plan by a registered dietitian. When a complete cohort was recruited they met 3 weeks out of each month with a dietary counselor for 6 months in separate groups according to their assigned diet. Intervention sessions continued at a slightly reduced frequency for an additional 18 months. At these sessions, participants were educated on their specific nutrient diet plan and taught behavioral techniques and skills to purchase, prepare, and follow their assigned diets and to self-monitor their intakes. They were given 14-day menus to enable them to strictly adhere to the diet regimen, as well as to be able to visualize the types and amounts of foods to help them meet their targets. Other strategies for adherence to diet were implemented if the participant tired of the structured menus. Participants were also instructed on how to use a computer tracking system in which they recorded their intake and received feedback on their success in achieving the goals of their assigned diet expressed as percentages above or below the mean target values. At the end of the recording session the participant received a graphic feed back on how they were doing with their specific diet. Participants in all 4 diet groups received similar lifestyle information in a standard form, including advice to increase physical activity to 90 minutes per week.
Resting Energy Expenditure (REE)
Resting energy expenditure was measured in all participants in the POUNDS LOST study at baseline, and at 6 and 24 months. Participants came to the laboratory after an overnight fast and 24 hr abstinence from caffeine, alcohol and exercise. After resting quietly for 30 minutes, a transparent plastic hood was placed over the head of the participant for another 30 minutes. They remained still and awake during the test, and the last 20 minutes of measurements were used for calculations. Oxygen consumption and carbon dioxide production were determined using a Deltatrac II Metabolic Monitor (Datex-Ohmeda, Helsinki, Finland). Calculations of O2 consumption and CO2 production were made from continuous measurements of O2 and CO2 concentrations in inspired and expired air diluted with a constant air flow (~40 L/min) generated by the metabolic cart and provided the estimate of energy expenditure.
Calculated Data
Surface Area Equation: (11)
Prediction Equation for Resting Energy Expenditure:
Statistical Analysis
Baseline data are presented as mean±SD, and changes from baseline as mean±SE. The primary outcomes of this study were the change in resting energy expenditure at 6 and 24 months in the four groups of 2×2 design (low or high fat and average or high protein). The data were also analyzed using the primary contrasts of high fat versus low fat and high protein versus average protein. Data were pooled for the two factorial comparisons of high fat vs. low-fat and high protein vs. average protein, and compared using two-sample t-tests. The difference in change by diet was evaluated using analysis of covariance (ANCOVA) with age, sex, and baseline values included in all models. Relationships between changes in body weight and REE were explored using linear regression. Equations for calculating the expected change were determined from baseline weight, height, age and sex, and used to determine expected values of REE at 6 and 24 months by substituting the observed body weights at those times into the equation. A two-sided significance level of 0.05 was set for all statistical tests. All analyses were performed using JMP 7 (SAS Institute Inc., 2011).
Results
Baseline Characteristics
Baseline characteristics of the participants by assigned diets ranked in order of percentage carbohydrate are shown in table 1. A total of 811 individuals (515 women, 296 men) were randomized (4). There was no difference in REE by diet assignment at baseline (P=0.33). Gender and race were equally distributed among diet groups. Height, weight, BMI, and waist circumference were significantly higher in men than women (data not shown). Baseline REE were significantly higher in men [1831±12.2 kcal/d (mean±SE)] than women [1385±9.2 kcal/d)](p<0.0001). Adjusting for baseline weight or surface area reduced the difference, but baseline REE still remained significantly higher in men than women (M = 1697±9.8 kcal/d; F =1462±7.1kca/d; P<0.0001). Baseline body weight was strongly and positively correlated with resting energy expenditure and waist circumference (P<0.0001). REE declined with age by about 60 kcal/decade in women and 50 kcal/decade in men (p <0.001).
Table 1.
Baseline Characteristics by Diet Assignment
| Variable | LF/AP (65% Carb) | LF/HP (55% Carb) | HF/AP (45% Carb) | HF/HP (35% Carb) | P-value |
|---|---|---|---|---|---|
| N | 204 | 202 | 204 | 201 | |
| M/F | 78/126 | 67/135 | 9/123 | 72/129 | |
| Age | 51.3±8.9 | 50.5±9.5 | 51.7±9.3 | 50.8±9.1 | 0.56 |
| REE (kcal/24h) | 1554±288 | 1516±253 | 1556±340 | 1566±311 | 0.33 |
| RQ | 0.84±0.044 | 0.84±0.043 | 0.85±0.045 | 0.84±0.042 | 0.38 |
| Height (m) | 1.69±0.09 | 1.67±0.09 | 1.68±0.09 | 1.68±0.09 | 0.22 |
| Weight (kg) | 93.8±15.8 | 91.5±13.1 | 92.0±16.9 | 94.3±16.02 | 0.098 |
| BMI (kg/m2) | 32.64±3.66 | 32.6±13.66 | 32.3±83.9 | 33.17±4.17 | 0.18 |
| Surface Area (m) | 2.07±0.21 | 2.03±0.18 | 2.04±0.23 | 2.06±0.21 | 0.22 |
| Waist (cm) | 103.6±13.4 | 102.5±11.6 | 103.4±13.8 | 104.1±13.2 | 0.66 |
Data are Mean±SD. REE = resting energy expenditure; RQ =respiratory quotient; BMI = body mass index.
Changes In Resting Energy Expenditure related to diet and weight loss
Changes from baseline to 6 and 24 months are arranged by assigned diet groups in Table 2A and 2B. The change in RQ was significantly different between the 2 low fat (high carbohydrate) diets compared to the 2 high fat (low carbohydrate) diets at 6 months (p<0.05) and 24 months (p<0.05). Waist circumference was significantly smaller at 6 and 24 months and at 24 months.
Table 2A.
Change from Baseline to 6 months by Diet Assignment
| Variable | LF/AP (65% Carb) | LF/HP (55% Carb) | HF/AP (45% Carb) | HF/HP (35% Carb) | P-value |
|---|---|---|---|---|---|
| N | 157 | 164 | 158 | 162 | |
| REE (kcal/24h) | −75.2±10.7 | −72.8±10.4 | −78.1±10.6 | −65.5±10.8 | 0.68 |
| RQ | +0.0049±0.0033 | −0.0013±.0033 | −0.013±0.0033 | −0.0044±0.0033 | 0.16 |
| Weight (kg) | −6.54±0.42 | −6.80±0.42 | −6.37±0.42 | −6.42±0.42 | 0.68 |
| BMI (kg/m2) | −2.27±0.15 | −2.37±0.14 | −2.27±0.25 | −2.26±0.16 | 0.82 |
| Surface Area (m2) | −0.063±0.0042 | −0.066±0.0042 | −0.063±0.041 | −0.063±0.041 | 0.77 |
| Waist (cm) | −6.52±0.46 | −693±0.46 | −6.87±0.46 | −7.03±0.46 | 0.78 |
Data are Mean±SE with baseline covariate adjusted for age and sex. REE = resting energy expenditure; RQ =respiratory quotient; BMI = body mass index.
Table 2B.
Change from Baseline to 24 months by Carbohydrate Diet Assignment
| Variable | LF/AP (65% Carb) | LF/HP (55% Carb) | HF/AP (45% Carb) | HF/HP (35% Carb) | P-value |
|---|---|---|---|---|---|
| N | 123 | 128 | 114 | 132 | |
| REE (kcal/24h) | −15.1±19.6 | −19.9±19.2 | −16.4±20.4 | +035±19.1 | 0.65 |
| RQ | −0.0040±0.0037 | −0.0070±0.0036 | −0.027±0.0039 | −0.016±0.0036 | 0.11 |
| Weight (kg) | −3.26±0.56 | −5.03±0.58 | −3.87±0.59 | −3.98±0.42 | 0.092 |
| BMI (kg/m2) | −1.10±0.19 | −1.73±0.20 | −1.40±0.21 | −1.41±0.20 | 0.11 |
| Surface Area (m2) | −0.032±0.0055 | −0.049±0.056 | −0.039±0.057 | −0.039±0.057 | 0.096 |
| Waist (cm) | −4.92±0.61 | −6.84±0.63 | −5.81±0.65 | −5.95±0.62 | 0.11 |
Data are Mean±SE with baseline value as a covariate and adjusted for age and sex. REE = resting energy expenditure; RQ =respiratory quotient; BMI = body mass index.
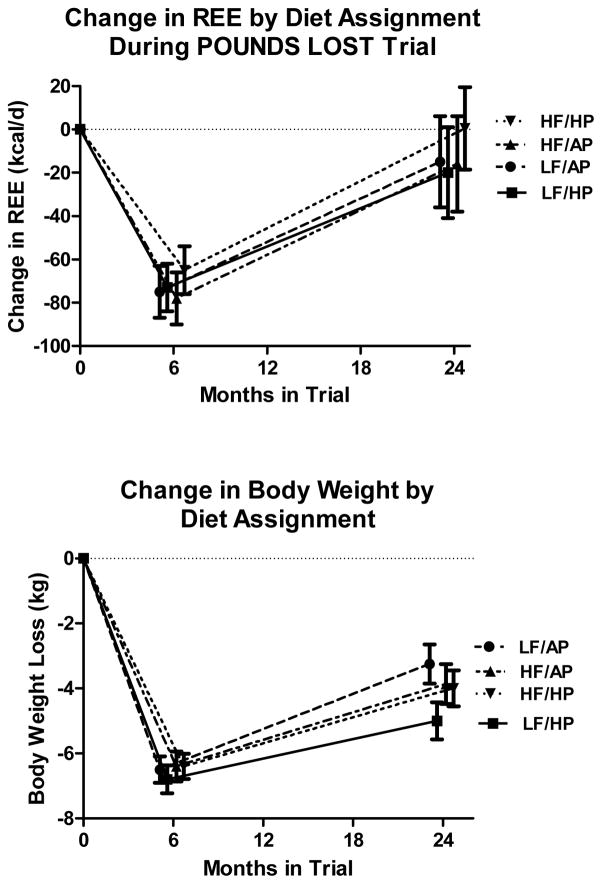
The change in REE and body weight from baseline to 6 and 24 months by diet group is shown in Figure 1. REE declined at 6 months by an average of 72±5.8 kcal/d (p<0.0001), and the decrease was significantly smaller in women than men (55.2±10.6 kcal/d vs 99.5±8.0 kcal/d; p <0.0001), but there was no difference between diets. At the end of 24 months, REE had risen and was not significantly different from the baseline value and there was again no difference between diet groups. Body weight fell significantly from baseline over the first 6 months (5.89±0.27 in women and 7.6±0.34 in men p = 0.0002), but there was no effect of diet composition. At 24 months, body weight was still significantly lower than baseline in all diet groups by an average of 60%.
Figure 1.
Change in resting energy expenditure (Top Panel) and body weight at 6 and 12 months in the POUNDS LOST Study. Data are expressed as mean±SE and includes all subjects who were measured at each time.
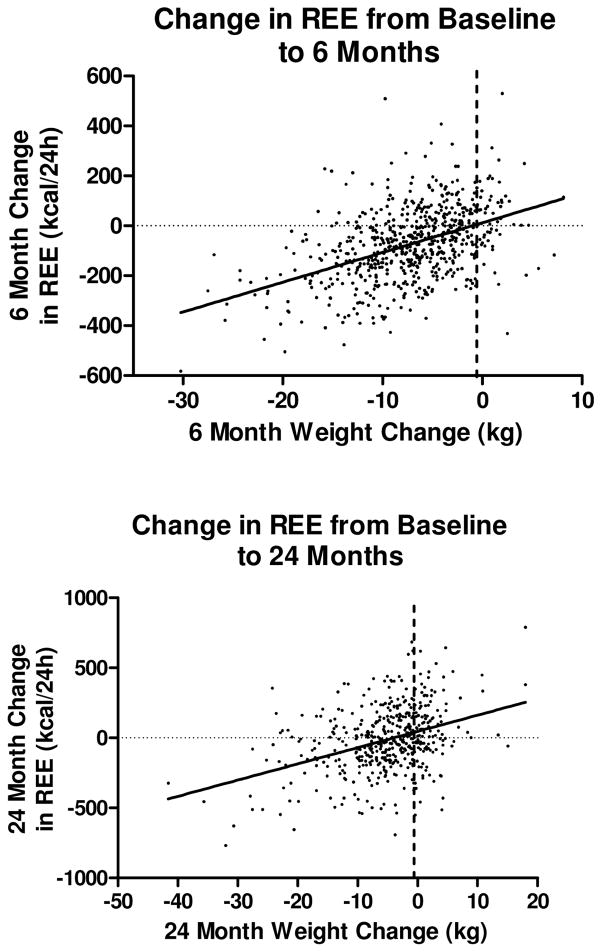
Since there were no clear diet effects on change in REE, the data from all participants were pooled to examine the effects of other factors. The fall in weight predicted the decline in REE at both 6 and 24 months (Figure 2). In women, REE decreased to a greater extent over the course of the study than it did in men (β=−49±6.4 kcal; P<0.0001), after adjusting for weight change, age, baseline weight, and baseline REE. Age was negatively associated with change in REE (β=−2.7±0.5; P<0.0001). This suggests that for a 1-year increase in baseline age, the change in REE decreased by 2.7 kcal, after adjusting for change in weight, sex, baseline weight, and baseline REE. Baseline weight was positively associated with change in REE (β=4.7±0.5; P<0.0001). This suggests that for a 1-kg increase in baseline weight, the change in REE increased by 4.7 kcal, after adjustment for baseline REE, sex, age, and change in weight. Baseline resting energy expenditure was negatively associated with change in REE (β= −0.47±0.03; P<0.0001), suggesting that each additional 1 kcal-REE at baseline resulted in a −0.5 kcal decrease in average REE over the course of the study, after adjustment for weight change, gender, age, and baseline weight.
Figure 2.
Relation of Change in Weight to Change in Resting Energy Expenditure
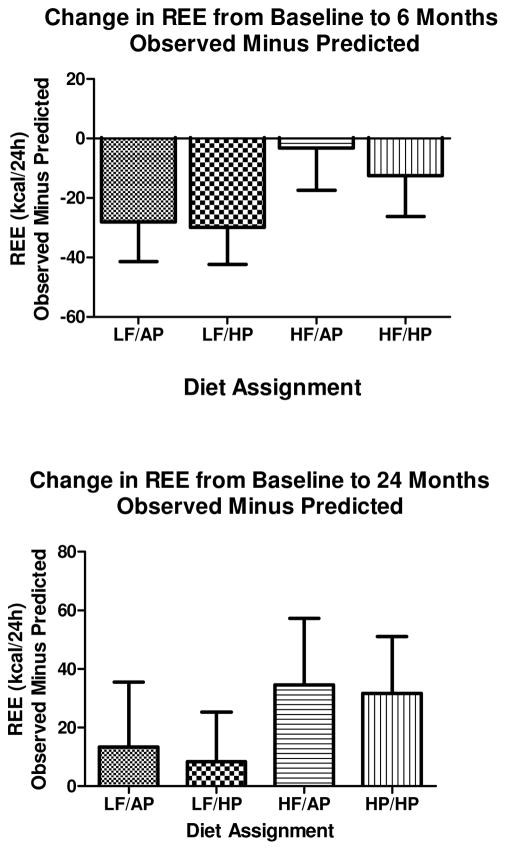
Predicted Changes in REE
Using baseline body weight, sex and age, a prediction equation for REE was derived and used to predict 6 and 24 month REE by substituting 6 and 24 month values for weight, sex and age. At 6 months, the measured resting energy expenditure was significantly lower than predicted (−18.2±6.7 kcal/24 h p<0.0068), suggesting adaptive thermogenesis. After 24 months, this had reversed, with measured REE being significantly higher than predicted (+21.8±10.1; p = 0.032). The difference from baseline between observed and predicted values for REE by diet assignment at 6 and 24 months is shown in Figure 3. At 6 months both the LF/AP and LF/HP (65% and 55% carbohydrate diets) diet groups had observed minus predicted values of REE that were significantly below zero (P<0.05) which is consistent with adaptive thermogenesis. By 24 month the observed minus predicted values for REE were not different from zero in any of the diet groups.
Figure 3.
Relation of Diet to Observed minus Predicted Values for Resting Energy Expenditure.
Discussion
Protein, carbohydrate, and fat in food stimulate oxygen consumption to different degrees (12), which suggests that dietary composition might affect energy expenditure (13) and thus the rate of weight loss. Mikkelsen et al (14) found that substituting either animal protein (pork) or soy protein for carbohydrate increased energy expenditure by 3% in mildly obese men over 24 hours in a respiration calorimeter. In another study, Whitehead et al (15) examined the effect of 15% or 35% protein intake on 24-h energy expenditure in subjects eating an energy restricted diet and found that on a high protein diet, the energy decrease was 71 kcal/d smaller. In a short-term study lasting only 19–21 days, Bandini et al found that total energy expenditure was significantly higher with a very high carbohydrate diet (83.1%) compared to a very high fat diet (83.5%), but resting energy expenditure was the same suggesting reduced physical activity on the high fat diet (16). Racette et al compared a low fat versus a low carbohydrate diet with or without exercise in a small study of 23 women that lasted 12 weeks. Resting energy expenditure declined comparably in the 2 diet groups (17).
In this trial we tested the effect of diet composition on body weight and resting energy expenditure over 24 months in a large group of overweight or obese patients. Both body weight and REE decreased by 6 months, but were unaffected by diet composition. The return of REE to baseline in all of the diet groups by 24 months, contrasted with the weight regain which was less than halfway back to baseline by 24 months. If there is any metabolic advantage to higher protein diets because of their higher thermic effect or effect on satiety (9, 18), it did not translate into measurably greater weight loss over the 24 month interval in free-living overweight or obese adults in the POUNDS LOST study.
The question of whether the fall in REE could be predicted from the decrease in body weight was evaluated by developing prediction equations for REE at baseline and using them to predict REE at 6 and 24 months from body weight at each time. At 6 months, the predicted energy expenditure was significantly higher than the measured REE in the two low fat diets (65% and 55% carbohydrate), but not in the two high fat diets. This metabolic adaptation at 6 months had disappeared by 24 months, showing that adaptive thermogenesis is indeed adaptive over time. The possibility of “adaptive” thermogenesis has been suggested in many studies (17, 24–26, 28, 34), but not when weight-matched controls were used (35–37) and not in 2 studies using individuals as their own control (38.39). One might have anticipated that the higher carbohydrate diets (lower fat) would stimulate energy expenditure more than the low carbohydrate (higher fat) ones, but this appears to have been overcome by the weight loss. Surprisingly, the difference between observed and predicted REE was not significantly different between the average and high protein diets as one might have expected from other studies (9). By 24 months adaptive change in REE had disappeared or been reversed.
Several other studies have previously examined the effect of underfeeding on resting energy expenditure (9, 17–32) and some of this data has been summarized by Saltzman and Roberts (33). In their analysis, the change in REE was predicted in pooled studies that included 153 men and women by this equation [Change in REE = −78.8 + 11.9*(change in body weight)]. In our data set with 640 overweight and obese men and women who had measurements at baseline and 6 months, the equation was [change in REE = −12.06 + (11.9*change in body weight)]. The slope of the regression in our study was nearly identical to Saltzman and Roberts (33), although the intercepts were different. In their analysis, Saltzman and Roberts (33) also reported that the average rate of weight change was −0.53 ± 0.14 g/d which is much more rapid than in our study (−0.036±0.0012 g/d m±SE), probably because most of the other studies had larger weight losses (range 7.9 to 27.0 kg) compared to the 6.5 kg in our study.
This study has several major strengths. It is the largest study to provide measurements of REE at baseline and again after 6 and 24 months in participants assigned to one of 4 diets differing in macronutrient composition. Second, in addition to being a large sample, it had nearly 40% men, and had a high percentage of participants [497/811 (61%)] who completed the measurement at 24 months. Weaknesses include the fact that adherence to the assigned diets was below expectations (4, 40) and that the percentage of minorities was low. The lower adherence to the diet than predicted from diet prescription would reduce the likelihood of finding differences related to diet, if they existed.
In summary, resting energy expenditure in this large study declined in with weight loss and the decline can be accounted for by the decrease in body weight. Macronutrient composition of the diet assignment did not influence the changes in resting energy expenditure at 6 months, but there were suggestive changes relating body weight to the higher fat diets. There was an adaptive metabolic response to weight loss at 6 months that had disappeared by 24 months.
Acknowledgments
Supported by Grant: HL 073286 from the National Heart, Lung and Blood Institute, NIH and GCRC grant RR 02635
References
- 1.Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, Rosenbaum M, Luke A, Schoeller DA, DeLany JP, Butte NF, Ravussin E. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009 Jun;89(6):1723–8. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray GA. A Guide to Obesity and the Metabolic Syndrome: Origins and Treatment. New York: CRC Press: Taylor and Francis Group; 2011. [Google Scholar]
- 3.Freedman MR, King J, Kennedy E. Popular diets: a scientific Review. Obes Res. 2001;9:1S–39S. doi: 10.1038/oby.2001.113. [DOI] [PubMed] [Google Scholar]
- 4.Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009 Feb 26;360(9):859–73. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dansinger ML, Gleason JA, Griffith JL, Selker JP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight-Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293:43–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 6.Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women. JAMA. 2007;297:969–77. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 7.Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C, Stein RI, Mohammed BS, Miller B, Rader DJ, Zemel B, Wadden TA, Tenhave T, Newcomb CW, Klein S. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med. 2010 Aug 3;153(3):147–57. doi: 10.1059/0003-4819-153-3-201008030-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray GA, Smith SR, de Jonge L, Xie H, Rood J, Martin CK, Most M, Brock C, Mancuso S, Redman L. Effect of dietary protein content on weight gain, energy expenditure, and body composition during overeating: a randomized controlled trial. JAMA. 2012;307(1):47–55. doi: 10.1001/jama.2011.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westerterp-Plantenga MS, Nieuwenhuizen A, Tomé D, Soenen S, Westerterp KR. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr. 2009;29:21–41. doi: 10.1146/annurev-nutr-080508-141056. [DOI] [PubMed] [Google Scholar]
- 10.Bray GA, Smith SR, DeJonge L, de Souza R, Rood J, Champagne CM, Laranjo N, Carey VJ, Obarzanek E, Loria CM, Anton SD, Ryan DH, Greenway FL, Williamson D, Sacks FM. Effect of Diet Composition on Energy Expenditure during Weight Loss: The POUNDS LOST Study. Intern J Obes. 2011 Sep 27; doi: 10.1038/ijo.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DuBois EF. Basal Metabolism in Health and Disease. Philadelphia: Lea and Febiger; 1924. [Google Scholar]
- 12.Swaminathan R, King RF, Holmfield J, Siwek RA, Baker M, Wales JK. Thermic effect of feeding carbohydrate, fat, protein and mixed meal in lean and obese subjects. Am J Clin Nutr. 1985 Aug;42(2):177–81. doi: 10.1093/ajcn/42.2.177. [DOI] [PubMed] [Google Scholar]
- 13.Schoeller DA, Buchholz AC. Energetics of obesity and weight control: does diet composition matter? J Am Diet Assn. 2005;105(Suppl 1):S24–S28. doi: 10.1016/j.jada.2005.02.025. [DOI] [PubMed] [Google Scholar]
- 14.Mikkelsen PB, Toubro S, Astrup A. Effect of fat-reduced dies on 24-h energy expenditure: comparisons between animal protein, vegetable protein and carbohydrate. Am J Clin Nutr. 2000;72:1135–1141. doi: 10.1093/ajcn/72.5.1135. [DOI] [PubMed] [Google Scholar]
- 15.Whitehead JM, McNeill G, Smith JS. The effect of protein intake on 24-h energy expenditure during energy restriction. Intern J Obes Relat Metab Disord. 1996;20:727–732. [PubMed] [Google Scholar]
- 16.Bandini LG, Schoeller DA, Dietz WH. Metabolic differences in response to a high-fat vs a high-carbohydrate diet. Obes Res. 1994;2:348–354. doi: 10.1002/j.1550-8528.1994.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 17.Racette SB, SChoeller DA, Kushner RF, Neil KM, Herling-Iaffaldano K. Effects of exercise and dietary carbohydrate on energy expenditure and body composition during weight reduction in obese women. Am J Clin Nutr. 1995:486–494. doi: 10.1093/ajcn/61.3.486. [DOI] [PubMed] [Google Scholar]
- 18.Westerterp-Plantenga MS, Lejeune MP, Nijs I, van Ooijen M, Kovacs EM. High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes Relat Metab Disord. 2004 Jan;28(1):57–64. doi: 10.1038/sj.ijo.0802461. [DOI] [PubMed] [Google Scholar]
- 19.Mathieson RA, Walberg JL, Gwazdauskas FC, Hinkle DE, Gregg JM. The effect of varying carbohydrate content of a very-low-caloric diet on resting metabolic rate and thyroid hormones. Metabolism. 1986 May;35(5):394–8. doi: 10.1016/0026-0495(86)90126-5. [DOI] [PubMed] [Google Scholar]
- 20.de Souza RJ, Bray GA, Carey VJ, Hall KD, Leboff MS, Loria CM, Laranjo NM, Sacks FM, Smith SR. Effects of 4 weight-loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J Clin Nutr. 2012 Mar;95(3):614–25. doi: 10.3945/ajcn.111.026328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ravussin E, Lillioja S, Anderson TE, Christin L, Bogardus C. Determinants of 24-hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest. 1986 Dec;78(6):1568–78. doi: 10.1172/JCI112749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Boer JO, van Es AJC, Roovers LCA, van Raaij JMA, Haustvast JGAJ. Adaptation of energy metabolism of overweight women to low-energy intake, studies with whole-body calorimeters. AJCN. 1986;44:585–595. doi: 10.1093/ajcn/44.5.585. [DOI] [PubMed] [Google Scholar]
- 23.Hill JO, Sparling PB, Shields TW, Heller PA. Effects of exercise and food restriction on body composition and metabolic rate in obese women. AJCN. 1987;46:622–630. doi: 10.1093/ajcn/46.4.622. [DOI] [PubMed] [Google Scholar]
- 24.Elliot DL, Goldberg L, Kuehl KS, Bennett WM. Sustained depression of the resting metabolic rate after massive weight loss. AJCN. 1989;49:93–96. doi: 10.1093/ajcn/49.1.93. [DOI] [PubMed] [Google Scholar]
- 25.Heshka S, Yang M, Wang J, Burt P, Pi-Sunyer FX. Weight loss and change in resting metabolic rate. AJCN. 1990;52:981–986. doi: 10.1093/ajcn/52.6.981. [DOI] [PubMed] [Google Scholar]
- 26.Froidevaux F, Schutz Y, Christin L, Jequier E. Energy expenditure in obese women before and during weight loss, after refeeding and in the weight-relapse period. AJCN. 1993;57:35–429. doi: 10.1093/ajcn/57.1.35. [DOI] [PubMed] [Google Scholar]
- 27.Svendsen O, Hassager C, Christiansen C. Effect of an energy-restrictive diet, with or without exercise, on lean tissue mass, resting metabolic rate, cardiovascular risk factors, and bone in overweight postmenopausal women. Am J Med. 1993;95:131–140. doi: 10.1016/0002-9343(93)90253-l. [DOI] [PubMed] [Google Scholar]
- 28.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. NEJM. 1995;332:621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 29.Foster GD, Wadden TA, Swain RM, Anderson DA, Vogt RA. Changes in resting energy expenditure after weight loss in obese African American and white women. Am J Clin nutr. 1999;69:13–17. doi: 10.1093/ajcn/69.1.13. [DOI] [PubMed] [Google Scholar]
- 30.Weinsier RL, Hunter GR, Zuckerman PA, Redden DT, Darnell BE, Larson DE, Newcomer BR, Goran MI. Energy expenditure and free-living physical activity in black and white women: comparison before and after weight loss. Am J Clin Nutr. 2000 May;71(5):1138–46. doi: 10.1093/ajcn/71.5.1138. [DOI] [PubMed] [Google Scholar]
- 31.Redman LM, Heilbronn LK, Martin CK, de Jonge L, Williamson DA, Delany JP, Ravussin E Pennington CALERIE Team. Metabolic and behavioral compensations in response to caloric restriction: implications for the maintenance of weight loss. PLoS One. 2009;4(2):e4377. doi: 10.1371/journal.pone.0004377. Epub 2009 Feb 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin CK, Heilbronn LK, de Jonge L, DeLany JP, Volaufova J, Anton SD, Redman LM, Smith SR, Ravussin E. Effect of calorie restriction on resting metabolic rate and spontaneous physical activity. Obesity (Silver Spring) 2007 Dec;15(12):2964–73. doi: 10.1038/oby.2007.354. [DOI] [PubMed] [Google Scholar]
- 33.Saltzman E, Roberts SB. The role of energy expenditure in energy regulation: Findings from a decade of research. Nutr Rev. 1995;53:209–220. doi: 10.1111/j.1753-4887.1995.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 34.Rosenbaum M, Hirsch J, Gallagher DA, Leibel RL. Long-term persistence of adaptive thermogenesis in subjects who have maintained a reduced body weight. Am J Clin Nutr. 2008 Oct;88(4):906–912. doi: 10.1093/ajcn/88.4.906. [DOI] [PubMed] [Google Scholar]
- 35.James WPT, Lean MEJ, McNeill G. dietary recommendations after weight loss: how to avoid relapse of obesity. Am J Clin Nutr. 1987;45:1135–1141. doi: 10.1093/ajcn/45.5.1135. [DOI] [PubMed] [Google Scholar]
- 36.Astrup A, Buemann B, Christensen NJ, Madsen J. 24-hour energy expenditure and sympathetic activity in postobese women consuming a high-carbohydrate diet. Am J Physiol. 1992;262:E282–E288. doi: 10.1152/ajpendo.1992.262.3.E282. [DOI] [PubMed] [Google Scholar]
- 37.Amatruda JM, Statt MC, Welle SL. Total and resting energy expenditure in obese women reduced to ideal body weight. J Clin Invest. 1993;92:1236–1242. doi: 10.1172/JCI116695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weigle DS, Sande KJ, Iverisu P-H, Monsen ER, Brunzell JD. Weight loss leads to a marked decrease in non-resting energy expenditure in ambulatory human subjects. Metabolism. 1988;37:930–936. doi: 10.1016/0026-0495(88)90149-7. [DOI] [PubMed] [Google Scholar]
- 39.Wadden TA, Goster GD, Letizia KA, Mullen JL. Long-term effects of dieting on resting metabolic rate in obese out-patients. JAMA. 1990;264:707–711. [PubMed] [Google Scholar]
- 40.Williamson DA, Anton SD, Han H, Champagne CM, Allen R, LeBlanc E, Ryan D, Rood J, McManus K, Laranjo N, Carey VJ, Loria CM, Bray GA, Sacks FM. Early behavioral adherence predicts short and long-term weight loss in the POUNDS LOST study. J Behav Med. 2010;33(4):305–314. doi: 10.1007/s10865-010-9253-0. [DOI] [PMC free article] [PubMed] [Google Scholar]