Abstract
Background:
Kano State is the most populous state, and one of those states pronounced with the highest prevalence of drug abuse in Nigeria. However, there is lack of documented data to back the assertion.
Objective:
We determined the pattern, awareness and perceptions of the adult residents of Kano metropolis about self medication.
Materials and Methods:
We used a descriptive cross-sectional design to study a random sample of 380 adult in Kano metropolis. Data was collected using semi-structured questionnaires that were pretested outside the study area. Data analysis was with Epi Info® 3.5.1.
Results:
The mean age of the subjects was 35.43 ± 15.10 years, majority were males (66.32%), singles (47.11%) and had at least secondary education (67.63%). About three-quarter (78.95%) admitted using drug (s) in the past without prescription. Drugs commonly consumed were antimalarials (42.10%), analgesics (40.56%), antibiotics (29.41%), and cough mixtures (13.31%). Common sources of drugs were patent medicine stores (62.54%) and the market (19.81%). Common reasons for self medication were long queues in the hospitals (38.39%), and in-accessibility to doctors (25.08%). About two-thirds (65.00%) correctly perceived that self medication could be hazardous; and half (51.58%) were aware of at least one hazard of self medication.
Conclusion/Recommendations:
Irrational drug use is a growing challenge to public health in Kano, Nigeria. Thus, drug regulatory agencies in Nigeria should work together to ensure that all drug retail outlets and drug sellers are registered, controlled drugs are dispensed only on prescription of the physicians; and the laws safeguarding drug use are duly enforced. Health authorities should also strengthen efforts towards health educating the public.
Keywords: Adult residents, awareness and perceptions, Kano, Nigeria, pattern, self medication
Introduction
The availability of potent and dangerous drugs has increased considerably since the close of 19th century. Recent advances in drug research have provided many synthetic medicines for the treatment of diseases, leading to a drug explosion.(1) Currently, numerous drugs and drug combinations are available, and many of them have been released for general use and are sold directly to the public as over-the-counter (OTC) drugs. Proprietary drugs which are sold over-the-counter include pain relievers, cough remedies, anti-allergies, laxatives, vitamins, tonics, antacids, and many others. Furthermore, dangerous drugs like the antibiotics and hormones can be procured without a valid prescription.(2) The sale of both over-the-counter and controlled drugs without the prescription of a physician predisposes to self medication.
Self-medication is the act of taking medicines or medical devices especially designed and labeled for use in the treatment of common health problems without the authority or prescription of a physician.(3) It is one of the rapidly growing areas of concern to medical professionals, government and the general public. Self-medication may initially result in reduction of distress but in the long-run however, it can cause many serious problems.(4) Symptoms may rebound, resulting in stronger desires to take more drugs. Poisoning, allergy, habituation, addiction, dependence and resistance could occur. In extreme of cases negative consequences such as depression, suicide attempt, interpersonal problems, legal problems, medical problems, and in-patient psychiatric hospitalization could also occur.
The attitudes of some health professionals towards poly-pharmacy, contributed immensely in terms of exposing the general public to a number of drugs and most importantly justifying their subsequent actions of abusing such drugs.(5) Previous study from Tanzania had demonstrated major prescribing problems due to poly-pharmacy and irrational use of antibiotics and injections.(6)
Safe medication is a serious problem in Nigeria. Studies from the southern part of the country show that as many as 60-90% of the population in some communities partake in one way or the other in self medication.(7,8) However, despite the assertion that Kano is one of the cities in Nigeria with the highest prevalence of drug abuse, there is paucity of documented data to back the assertion. We therefore set out on this study to determine the pattern, awareness and perceptions of the adult residents of Kano metropolis about self medication. Findings from this study would enhance clarity on the problems of self medication in Kano to policy makers, programme managers and researchers. This would be useful for designing strategies and interventions to address this menace.
Materials and Methods
Setting/study population
The study was carried out among adult residents of Kano metropolis. The metropolis is made of eight Local Government Areas (L.G.As) consisting of Kano municipal, Dala, Gwale, Fagge, Nassarawa, Tarauni, Kumbotso and Ungoggo LGAs.
Kano State is located in north western Nigeria and is one of the oldest and largest states in the country, and perhaps also the most traditional. Commerce and agricultural production have been the backbone of the Kano economy. Islam is the dominant religion, though there are significant groups of Christians. Urban drift from rural areas within Kano, from other states in Nigeria and from West Africa has provided a steady stream of migrants adding to Kano’s growing population. Kano is therefore a cosmopolitan melting pot of people. The city is characterized by overcrowding, poor sanitation, and inconsistent municipal water supply. Registered drug stores and unregistered drug hawkers "Kafada chemists’ are common on the streets of Kano; and they both contribute significant source of drugs for the population.
There were 9,383,682 people in Kano state during the 2006 National census;(9) and the metropolitan LGAs contributed 2,828,861 (30.1%) of this figure. Majority of the residents are traders, civil servants, farmers and students.
Study design/sampling
We used a descriptive, cross-sectional study design. A sample of 380 adults was selected for the study. This was determined using the formula for estimating minimum sample size for descriptive studies;(10) and 85% prevalence for self medication among general outpatients in a Nigerian community hospital.(11) The calculated minimum sample size was inflated to compensate for incomplete responses and non-response. The multistage sampling technique was used for selection of the study subjects: At first stage, four local government areas (L.G.As) were randomly selected from the eight metropolitan L.G. As of Kano state. At the second stage three wards were randomly selected from each of the selected L.G. As by drawing lots. This gave a total of 12 wards. Thereafter, one settlement was selected from each of the wards by drawing lots arriving at a total of 12 settlements; and using systematic sampling, equal samples (32 houses) were selected from each of the settlements. The sampling interval for the selection was determined by dividing the total number of houses in each of the settlements with the required sample of 32 houses. Finally, an eligible adult was interviewed from each of the selected houses. Where there are two or more adults in a house, one was randomly selected by drawing lots.
Instrument description/data collection
Interviewers administered the pre-tested questionnaire that contained open and closed-ended questions. The questions were phrased based on reports of previous surveys from southern Nigeria(8,11–14) to elicit socio-demographic characteristics of respondents, the pattern of self medication within a recall period of six months preceding the survey (prevalence and types); and the awareness and perceptions of health hazards of self medication in Kano. The questionnaire was pretested on 50 individuals from a different L.G.A other than the study L.G.A; and based on the experience from the pretest the questions on the type of drugs commonly used without the prescription of a physician and the respondents’ reasons for the self medication were changed to multiple response type. The questionnaires were administered by six trained Hausa speaking research assistants. The interviews were conducted in the local language (Hausa). Informed consent was obtained from prospective respondents. The consent form was in the local language (Hausa), and literate respondents indicated acceptance by signing the consent form, while non-literate participants affixed their thumbprint. Permission and ethical clearance for the study were obtained from the Kano State Ministry of Local Government and Chieftaincy Affairs and the Institutional Review Board of Aminu Kano Teaching Hospital respectively. Data was collected in March and April 2011.
Data analysis
Data was analyzed using Epi Info® 3.5.1 statistical software package (CDC Atlanta, Georgia, USA). Quantitative variables were summarized using appropriate measures of location and variability, whereas categorical variables were presented as frequencies and percentages. The Chi-square test was used to test for significant associations between categorical variables. P ≤ 0.05 was considered statistically significant. Binary logistic regression analysis was used to determine factors that were significantly associated with respondents’ use of drugs; and their awareness of health hazards of self medication.
Results
Socio-demographic characteristics of respondents
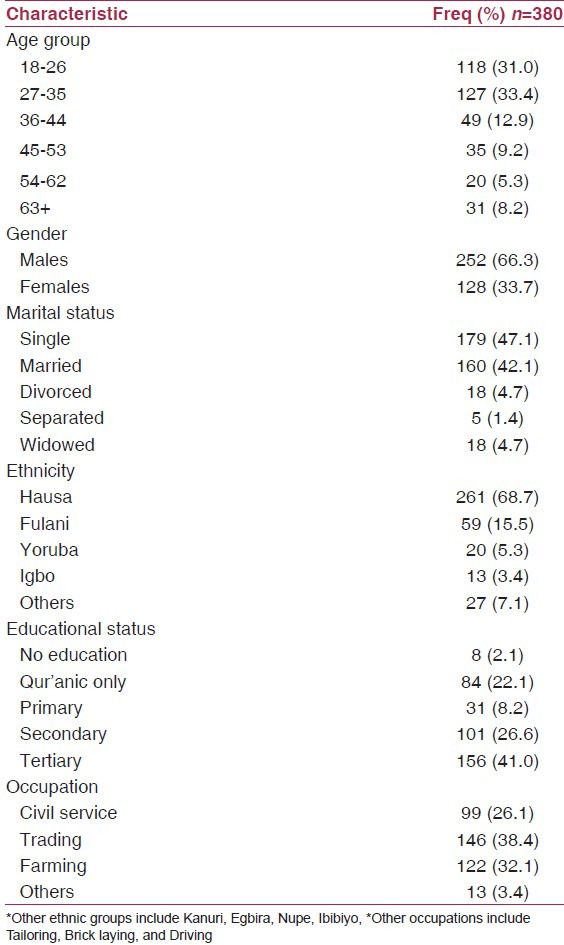
The respondents’ ages ranged from 18 to 89 years with a mean of 35.43 ± 15.10 years. The majority (82.9%) were less than 47 years old, males (66.3%), and singles (47.1%). Two-third of the respondents (67.6%) had at least secondary education whereas a third (38.4%) was traders. The socio-demographic characteristics of the respondents are summarized in Table 1.
Table 1.
Socio-demographic characteristics of respondents
Pattern of self medication in Kano metropolis
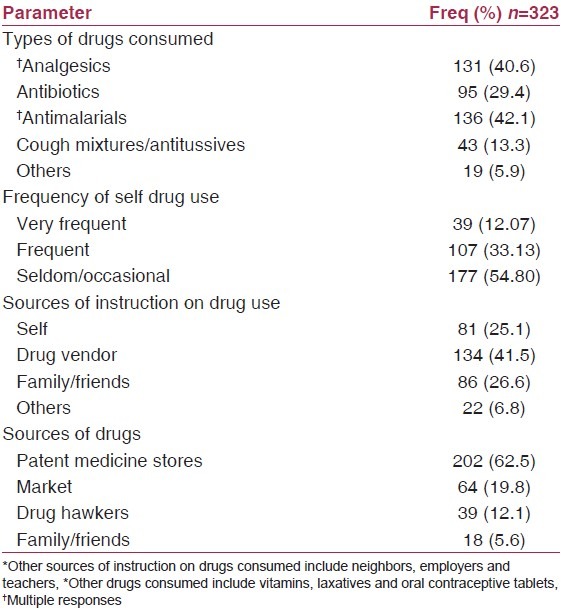
Three hundred (78.9%) out of the 380 subjects studied admitted using drug (s) in the past without the prescription of a physician. About a quarter (26.3%) reported using the drugs on their wards. The observed pattern of self medication among our respondents is as depicted in Table 2. More than half (54.8%) had used drugs occassionally, while 12.1% had been very frequent with them. The respondents reported consumption of one or more drugs without obtaining a prescription. The drugs commonly consumed were antimalarials (42.1%), analgesics (40.6%), and antibiotics (29.4%). Cough mixtures/antitussives were also used by 13.3% of the respondents. Similarly, 5.9% of drugs like vitamins, lexatives and oral contraceptive pills were consumed without the prescription of a doctor or other relevant health workers. Majority of these respondents obtained the drug (s) from either the patent medicine stores (62.5%) in town, or from drug stores in the market (19.8%). The other sources from where respondents obtained their drug (s) include drug hawkers (Kafada chemists) and family/friends as shown in Table 2. The drug vendors (41.5%) and family/friends (26.6%) provided the respondents with instructions on how to use the drugs consume. In 25.1% of cases however, respondents needed no external instruction on the use of the drugs commonly consumed.
Table 2.
Pattern of self medication in Kano metropolis
When asked why doctor (s) were not consulted for prescription before respondents consumed the drug (s), the majority proclaimed that long queues in the hospitals (38.4%), and doctors not being readily available (25.1%) were the most common reasons for their self medication. Other reasons mentioned were “services too expensive” (17.7%) and “found it unnecessary” (18.9%).
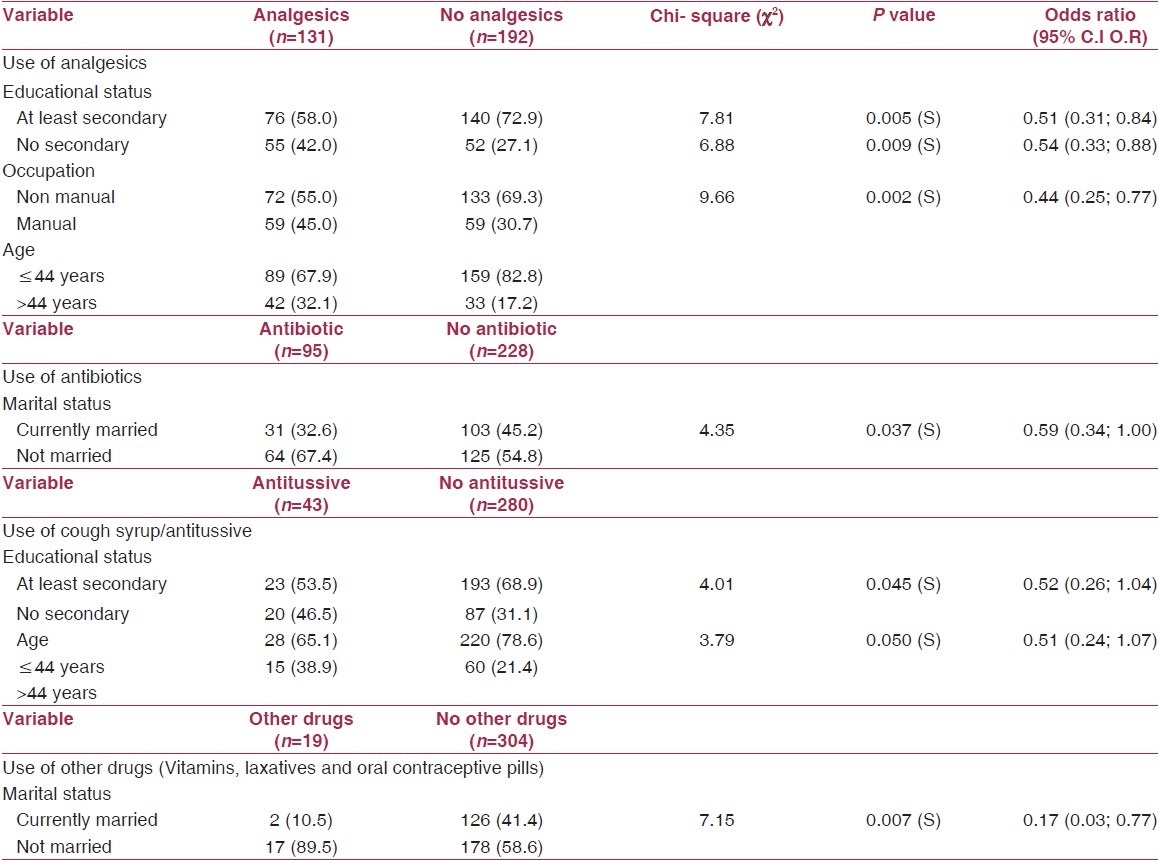
When we examined the effect of some selected socio-demographic variables (Gender, age, marital status, educational status and occupation) on self medication, it was observed that respondents’ educational status (χ2 = 7.81, P < 0.05), occupation (χ2 = 6.88, P < 0.05) and age (χ2 = 9.66, P < 0.05) were significantly associated with consumption of analgesic drugs. Respondents with at least secondary school education were less likely to have consumed analgesics without prescription [(OR = 0.51 (0.31; 0.84)]. Similarly, the non manual workers from among the respondents [OR = 0.54 (0.33; 0.88)], and those that were 44 years or less [OR = 0.44 (0.25; 0.77)] were also less likely to have consumed analgesics without prescription. Also, it was observed that marital status was the only factor that was statistically associated with consumption of antibiotics [(χ2 = 4.35, P < 0.05; O.R = 0.59 (0.34; 1.00)]; and with use of vitamins, laxatives and oral contraceptive drugs without prescription [(χ2 = 7.15, P < 0.05; O.R = 0.17 (0.03; 0.77)]. On the other hand, the inappropriate use of cough syrup was significantly associated with the respondents’ educational status (χ2 = 4.01, P < 0.05) and age (χ2 = 3.79, P < 0.05). Respondents that had attained at least secondary school level of education were less likely to have used cough syrups without the prescription of a doctor or relevant health worker [OR = 0.52 (0.26; 1.04)]. In the same vein, the younger respondents who were 44 years of age or less were less likely to have used cough syrups without prescription [OR = 0.51 (0.24; 1.07)] as shown Table 3. However, none of the socio-demographic factors examined was significantly associated with the use of antimalarial drugs [Age (χ2 = 0.42, P = 0.52); Gender (χ2 = 1.17, P = 0.28); Marital status (χ2 = 0.02, P = 0.89); Educational status (χ2 = 0.50, P = 0.48); and occupation (χ2 = 0.16, P = 0.69)].
Table 3.
Social and demographic factors significantly associated with self medication
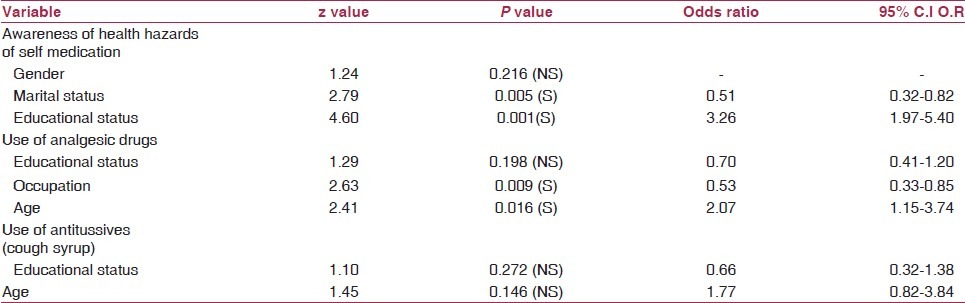
The associated factors were further subjected to binary logistic regression using models consisting of only the significant variables for each of the drug use category. The findings reveal that respondents’ age and occupation were the only factors that were significantly associated with the inappropriate use of analgesic drugs. On the other hand, neither age nor the educational status of the subjects turned out to be risk factors for irrational use of antitussives/cough syrups [Table 4].
Table 4.
Logistic regression of social and demographic factors significantly associated with respondents’ awareness and practices of self medication
Respondents’ awareness and perception of health hazards of self medication
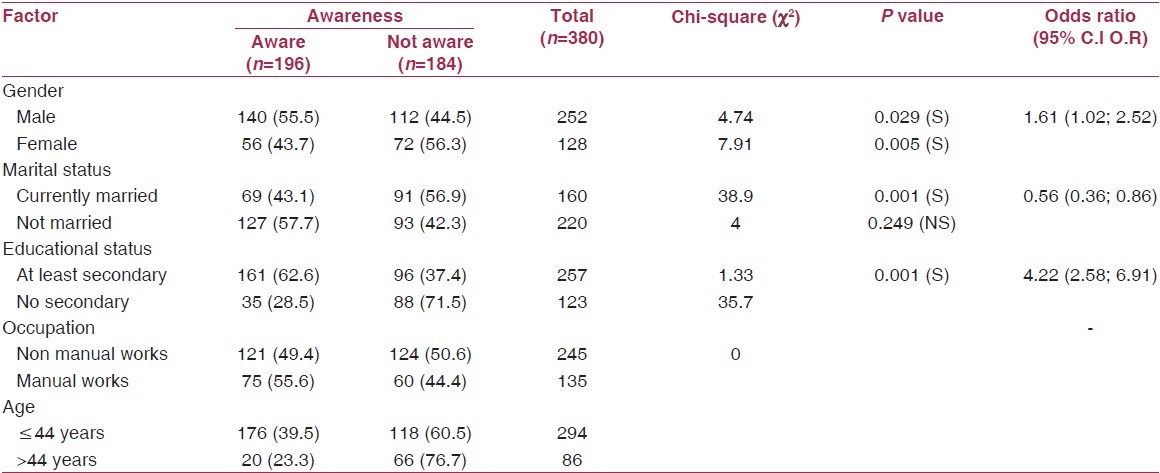
About two-thirds 247 (65.0%) of the respondents correctly perceived that self medication could be hazardous; and about half (51.58%) were aware of at least one hazard of self medication when prompted using unstructured question. The hazards listed by the respondents are as summarized in Table 5. Common hazards identified include drug resistance/drug failure (65.26%), addiction (52.37%) and poisoning (43.42%). The respondents awareness of the health hazards was statistically associated with their gender (χ2 = 4.74, P < 0.05); marital status (χ2 = 7.91, P < 0.05); and educational status (χ2 = 38.94, P < 0.05), but not with their age or occupations as depicted in Table 6. On multivariate analysis using a model that consisted of respondents’ gender, marital status and educational status, only marital status and educational status were significantly associated with the respondents’ awareness of the health hazards of self medication [Table 4].
Table 5.
Respondents’ perception of hazards of self medication
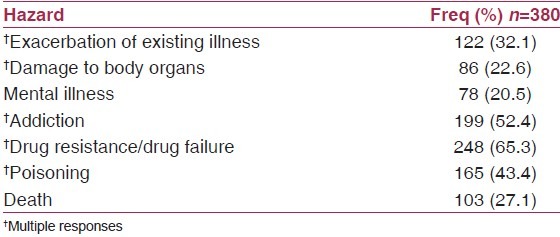
Table 6.
Factors associated with respondents’ awareness of hazards of self medication
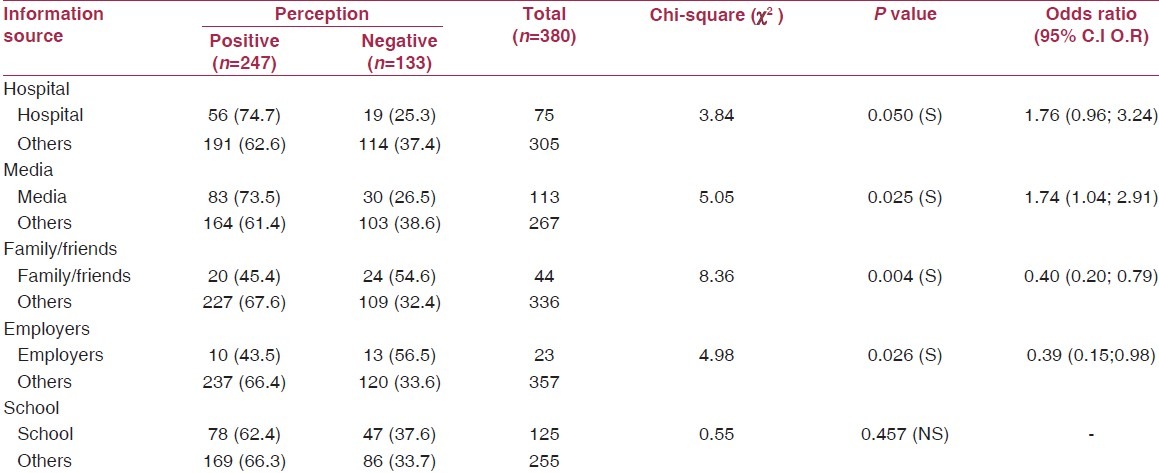
We also asked the respondents questions to elicit their sources of information on the hazards of self medication. The majority obtained their information on drug use and hazards of self medication from school (32.9%), and less than a quarter (19.7%) obtained this information from the hospital. Other sources include media (29.7), family/friends (11.6) and employers (6.1%). Respondents that obtained information on self medication from the hospital [χ2 = 3.84, P < 0.05); O.R = 1.76 (0.96; 3.24)] or the media [χ2 = 5.05, P < 0.05); O.R = 1.74 (1.04; 2.91)] were two times more likely to have construed positively that it can be hazardous compared to those that got information from other sources [Table 7].
Table 7.
Relationship between source of information and respondents’ perception of hazards of self medication
Discussion
Pattern of self-medication
The practice of self-medication has long been in existence world wide, and the situation continues to increase particularly in developing countries where high prevalence had been reported.(12,13) The high prevalence observed in this study (85.0%) is within the 73.0 and 100.0% prevalence respectively reported by Akanbi and colleagues;(8) and Ifedili and Ifedili(14) from the southern part of Nigeria. Similar prevalence was observed in several other African countries.(13,15–17) Interestingly, the prevalence of self medication reported from Ethiopia,(18) Ghana(19) and South Africa(20) were much lower and very similar to those observed in studies conducted in Asia,(21),(22) parts of Europe,(3,4,23) and the United States of America.(24) The lower prevalence reported from these countries may not be unconnected with their improved access to health facilities, health personnel; and high regard for health and safety. This may perhaps serve as an explanation why majority of our respondents proclaimed that long queues in the hospitals and doctors not being readily available were their main reasons for their self medication. The above finding is corroborated by results from Bamgboye and his colleagues where inaccessibility to health facility was reported among the leading promoters of self-medication.(12)
Medicines commonly misused vary from one community to another. We observed that antimalarials, analgesics and antibiotics in that order were inappropriately consumed by our respondents without the prescription of a physician. Previous studies from Nigeria,(8) Mozambique,(16) Sudan,(17) South Africa,(20) Tanzania,(15) Ghana,(19) and Turkey(23) reported that one or more of these drugs topped the list of drugs commonly consumed by their respondents without physician’s prescription. Contrarily, antibiotics were drugs least misused by the public in Niger Republic.(13)
Home management of malaria and other common childhood illnesses are being advocated by the World Health Organization (WHO) and UNICEF as a strategy to promote early and effective treatment for malaria and other common ailments like diarrhoea, acute respiratory infections (ARIs); sexually transmitted infections (STIs); and to promote child survival in order to reduce morbidity and mortality from these diseases particularly in developing countries.(25,26) Although intensive trainings are advanced to the caregivers in the community, and adhoc or voluntary health workers as channels through which these interventions are delivered, access to drugs coupled with the public’s disregard for drug regulations and safety could explain the rampant misuse of drugs in our societies. This is supported by Worku’s observation from a study on safe medication in Ethiopia that 52.4% of his respondents obtained their drugs from informal retail outlets.(18) Okumuraj and other researchers also reported that self medication is commoner among those who have accessibility to drugs, so also when drugs are kept at home.(4) Furthermore, Ouedrawgo and colleagues reported that familiarity of the general public with some disease conditions like malarial symptoms contributed immensely to depressing their will to consult a doctor.(27)
It is well acknowledged that misuse of antibiotics and antimalarials contribute to the widespread antibiotic and the recent chloroquine resistance. Also, unnecessary exposure to cough syrups and other sedatives also lead to addiction. Incidentally, we observed that inappropriate use of cough syrups/antitussives is significantly prevalent among our respondents. This was similarly reported from Turkey,(23) Tanzania(15) and Mozambique.(16) This is a clear indication for more regulatory framework in this regard.
Interestingly, safe care initiatives if correctly implemented can contribute immensely to the rational use of medicines. Promotion of self-care is an educational and empowering process that ensures that people with the right information can make the right decision as far as their own health is concerned.(28) This however needs policy direction and professional support. There is currently no policy on self care in Nigeria, but there are health care initiatives that promote self care in the community such as the community component of integrated management childhood illnesses C-IMCI, Roll-back malaria programme etc., that are already operational in Nigeria. If properly implemented, self care will reduce the problems of irrational use of drugs and its burden on the health service in Kano and Nigeria at large.
The pattern of self medications varies from one community to another, and with individual characteristics. This study similarly observed this differentials with the type of drugs commonly consumed. We found that self medication with analgesics was more common among respondents involved in manual works and in people that were 44 years or more. Furthermore, being single was significantly associated with inappropriate consumption of antibiotics; oral contraceptives and other drugs. Other workers similarly reported that self medication is more common among women than men, and among people who live alone;(3) and that it is commoner among the lower socio-economic class.(21) On the contrary however, other reports showed that self medication is more common among people with higher education,(3,21) and among younger than older individuals.(7) It is worthy of note at this juncture that the agreements and disagreements in the findings of our study with the others may perhaps be due to lack of disaggregation of the individual characteristics studied by the other researchers by the type of drugs consumed as clearly disaggregated in our study.
Awareness and perceptions of hazards of self medication
The health hazards associated with self-medication are enormous, as they affect the overall health of individuals and community.(15) The situation is more disturbing as the concept of self-medication seems unclear to many people to the extent that some do not even regard their practices as form of self-medication. People often go to medical shops and ask for tablets for stomachache, headache, fever, cough or diarrhea. The pharmacies gives some tablets without asking any question; and people buy over-the-counter drugs even for children.(16) Self medication is associated with risks such as misdiagnosis, use of excessive drug dosage, prolonged duration of use, drug interactions and polypharmacy. The latter may be particularly problematic in the elderly.
This study observed that about half of the respondents were aware of at least one hazard of self medication. Paradoxically, about two-thirds of all the respondents correctly perceived that self medication could be hazardous. Awareness levels of 47.9 and 45.2% for self medication were reported from studies conducted in United States of America(24) and Nepal(22) respectively. On the other hand, lower figures ranging from 22.8 to 37.9% were reported from studies conducted in Ethiopia,(18) India,(21) Turkey(23) and the southern part of Nigeria.(14)
The problems of self medication are enormous in Kano metropolis and require urgent interventions. In view of our findings therefore we recommend that the National Agency for Foods and Drugs Administration and Control (NAFDAC), National Drugs Law Enforcement Agency (NDLEA) and the Pharmaceutical Council of Nigeria should work together to ensure that all drug retail outlets and drug sellers are registered, controlled drugs are dispensed only on prescription of the physicians; and the laws safeguarding drug use are duly enforced. Drugs control must be implemented rationally, restricting the availability of drugs to the public. The Ministries of Health (MOH) and development partners should strengthen efforts towards educating the entire public on the dangers of indiscriminate and in-appropriate drug use, and also to improve access of the general public to qualitative and affordable medical care in the hospitals, thus safeguarding them from the dangers of safe medication. Safe care initiatives on safe medication should also be introduced.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Civanera M. A proposal for the prevention of ethical problems related to drugs promotion: A national network for drug information. Turk Psikiyatri Derg. 2008;19:310–7. [PubMed] [Google Scholar]
- 2.Gaillard S, Dellasanta P, Loutan L, Kayser B. Awareness, prevalence, medication use, and risk factors of acute mountain sickness in tourists trekking around the Annapurnas in Nepal: A 12-year follow-up. High Alt Med Biol. 2004;5:410–9. doi: 10.1089/ham.2004.5.410. [DOI] [PubMed] [Google Scholar]
- 3.Figueiras A, Caamano F, Gestal-Otero J. Socio-demographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26. doi: 10.1023/a:1007608702063. [DOI] [PubMed] [Google Scholar]
- 4.Okumaraj, Wakai S, Umenai T. Drug utilization and self-medication in rural communities in Vietnam. Soc Sci Med. 2002;54:1875–86. doi: 10.1016/s0277-9536(01)00155-1. [DOI] [PubMed] [Google Scholar]
- 5.Maselle AY, Nsimba SE, Fulgense J. A survey of prescribing practices of health care workers in Kibaha district in Tanzania. Tanzania Med J. 2007;22:31–33. [Google Scholar]
- 6.Hussong AM, Gould LF, Hersh MA. Conduct problems moderate self-medication and mood related drinking consequences in adolescents. J Stud Alcohol Drugs. 2008;69:296–307. doi: 10.15288/jsad.2008.69.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amaghionyeodiwe LA. Determinants of choice of health care provider in Nigeria. Health Care Manag Sci. 2008;11:215–27. doi: 10.1007/s10729-007-9038-3. [DOI] [PubMed] [Google Scholar]
- 8.Akanbi OM, Odaibo AB, Afolabi KA, Ademowo OG. Effects of self-medication with antimalarial drugs on malarial infection in pregnant women in south western Nigeria. Med Princ Pract. 2005;14:6–9. doi: 10.1159/000081915. [DOI] [PubMed] [Google Scholar]
- 9.National Bureau of Statistics. 2006 Population Census. Federal Republic of Nigeria. [Last accessed on 2010 Mar 7]. Available from: http://www.nigeriastat.gov.ng .
- 10.Lwanga SK, Lemeshow S. Sample size determination in health studies, a practical manual. Publication of World Health Organization. 1991:1–3. [Google Scholar]
- 11.Omolase CO, Adeleke OE, Afolabi AO, Afolabi OT. Self medication amongst general outpatients in a Nigerian community hospital. Ann Ibadan Postgrad Med. 2007;5:64–7. doi: 10.4314/aipm.v5i2.64032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bamgboye EA, Amoran OE, Yusuf OB. Self medication practices among workers in tertiary hospitals in Nigeria. Afr J Med Sci. 2006;35:411–5. [PubMed] [Google Scholar]
- 13.Ezechukwu CC, Eqbuonu I, Chukwuka JO. Drug treatment of common symptoms in Nnewi: What mothers do? Niger J Clin Pract. 2005;8:1–3. [PubMed] [Google Scholar]
- 14.Ifedil CJ, Ifedil CA. Self-medication among academicians in a Nigerian University of Benin: Are there gender or age difference? J Coll Med. 2008;13:29–33. [Google Scholar]
- 15.Nsimba SE. Assessing the performance practices and roles of drug sellers/dispensaries for common conditions, in Kabaha district, Tanzania. Trop Doct. 2007;37:197–201. doi: 10.1258/004947507782333099. [DOI] [PubMed] [Google Scholar]
- 16.Lucas R, Lunet N, Calvarho R, Langa J, Muanantatha M, Nkuanda LP, et al. Pattern in the use of medicines by University students in Maputo Mozambique. Cad Saude Publica. 2007;23:2845–52. doi: 10.1590/s0102-311x2007001200005. [DOI] [PubMed] [Google Scholar]
- 17.Awad AI, Eltayeb IB. Self-medication practices with antibiotics and antimalarials among Sudanese undergraduate University students. Ann Pharmacother. 2007:1249–55. doi: 10.1345/aph.1K068. [DOI] [PubMed] [Google Scholar]
- 18.Worku S, G/Mariam A. Practice of self-medication in Jimma town. Ethiop J Health Dev. 2003;17:111–6. [Google Scholar]
- 19.Buabeng KO, Duwiejua M, Dodoo AN, Matowe LK, Enlund H. Self reported use of antimalarial drugs and health facility management in Ghana. Malar J. 2007;6:85. doi: 10.1186/1475-2875-6-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peltzer K, Mohlala G, Phaswana-Mafuya N, Ramlagan S. Household surveys on the pattern of utilization of medicines in selected communities in South Africa. African. J Phys Health Educ Recreation Dance. 2008;14:163–77. [Google Scholar]
- 21.Durgawale PM. Practice of self-medication among slum-dwellers. Indian J Public Health. 1998;42:53–5. [PubMed] [Google Scholar]
- 22.Samuel G, Dellasanta P, Lountan L, Kayser B. Awareness, prevalence, medication use and risk factors in tourist trekking around the annapumas in Nepal: A 12 year follow up. High Alt Med Biol. 2004;5:410–19. doi: 10.1089/ham.2004.5.410. [DOI] [PubMed] [Google Scholar]
- 23.Hayran O, Karavus M, Aksayan S. Help seeking behavior and self-medication of a population in urban area in Turkey: Cross sectional study. Croat Med J. 2000;41:327–32. [PubMed] [Google Scholar]
- 24.Mainous AG, 3rd, Diaz VA, Carnemolla M. Factors affecting Latino’s use of antibiotics for self-medication. J Am Board Fam Med. 2008;21:28–34. doi: 10.3122/jabfm.2008.02.070149. [DOI] [PubMed] [Google Scholar]
- 25.Bryce J, Victora CG, Habicht JP, Black RE, Scherpbier RW. MCE-IMCI Technical Advisors. Programmatic pathways to child survival: Results of multi-country evaluation of Integrated Management of Childhood Illness. Health Policy Plan. 2005;20(Suppl 1):i5–i17. doi: 10.1093/heapol/czi055. [DOI] [PubMed] [Google Scholar]
- 26.Erin S, Anne T, Julia R. The maternal-newborn-child health continuum of care: A collaborative effort to save lives. Population Reference Bureau Policy perspectives on Newborn Health. [Last accessed on 2006 Mar]. Available from: http://www.prb.org/pdf06/SNL-ContOfCare_Eng.pdf .
- 27.Ouedrawgo LT, Some IT, Diarra M, Guissou IP. Self-medication in the treatment of acute malaria. Study based on uses of private health drug stores in Ovagandoungou, Burkina Faso. Bull Soc Pathol Exot. 2008;101:124–7. [PubMed] [Google Scholar]
- 28.World Health Organization. Self care in the context of Primary Health Care. Report of the Regional Consultation Bangkok, Thailand. [Last accessed on 2009 Jan 7-9]. Available from: http://www.searo.who.int/LinkFiles/Health_System_Strengthening_SEA-HSD-320.pdf .


