Abstract
Background:
Infant death depends upon the care during the infancy and also upon the service utilization during antenatal and intra-natal periods and with its decline, it is necessary to find the under-reporting if any and identify the most appropriate agency for its reporting.
Objectives:
(1) To document disparities between different reporting systems about infant deaths and find out the under-reporting if any and identify the most appropriate agency and (2) To identify utilization of health services during ante, intra and post-natal period for all infant deaths.
Materials and Methods:
Study was conducted in 51 villages of 3 Primary Health Centers (PHCs) from a tribal dominated Taluka (block) of South Gujarat during September - November 2005. Information was gathered for 1 year (1 September 2004 to 31 August 2005) from 4 sources namely health care system, Integrated Child development services (ICDS) scheme, Civil Registration System (CRS) and Investigator himself (Gold standard). Data was collected in a designed verbal autopsy questionnaire by house to house survey and analyzed in Epi Info.
Results:
A total of 48 infant deaths were recorded by investigator against reported 2, 10 and 8 infant deaths by CRS, Health System and ICDS respectively. While profiling these 48 infant deaths it was found that only 29.2% mothers received full antenatal care (ANC) and 60.4% delivered at home (by untrained personnel). Not a single delivery was done at PHCs or its sub centers (SC). In 25% cases there was poor cord care. 39.6% mothers did not breastfeed and 35.4% gave pre-lacteal feeding.
Conclusions:
There was gross underreporting of infant mortality in all 3 agencies. The utilization of ANC and post natal care (PNC) services was poor in these death cases. Health system and ICDS need to be sensitized to work in coordination to provide quality ANC, INC and PNC to prevent such avoidable infant deaths.
Keywords: Antenatal care, data disparity, infant deaths, intra-natal care, post-natal care
Introduction
Infant Mortality Rate (IMR) in India has declined considerably from 146 (1961) to 58 (2005)(1) and currently it is at 47 and 44 per 1000 live births for India and Gujarat respectively(2) though it is still high compared to developed countries. With decrease in IMR, it becomes important to find out a maximally reliable reporting agency to provide the accurate information not only in terms of number of infant deaths but also about causes of infant deaths related with ante natal care (ANC), intra natal care (INC) and post natal care (PNC) service utilization.
In India, barring a few community based studies,(3) data on the locally prevalent causes of death in general and infant death in particular (derived from community based studies) is limited. To our best of knowledge no such community based study has been undertaken in Gujarat. With this background it was proposed to undertake this study with objectives of documenting disparities between different reporting systems about infant deaths, and to find out under-reporting if any amongst any one/all systems as well as to identify utilization of health services during ante, intra and post-natal period for all infant deaths.
Materials and Methods
The study was carried out in all 51 villages of three selected Primary Health Centers (PHCs) of a remote, tribal dominated block of South Gujarat. Purposive sampling was done to select study populations keeping in mind the resources, feasibility, logistics and the availability of time. Population of three PHCs was thought to be sufficient to meet the required sample size to fulfill the objectives of the study. The study incorporated all the infant deaths, which occurred during one year from 1st September 2004 to 31st August 2005. Infant deaths amongst the daughter-in-law of the village only, were included in the study. The field based data were collected in September - November 2005. The information regarding infant deaths was gathered through four sources namely health care system, Integrated Child development services (ICDS) scheme, Civil Registration System (CRS) and Investigator himself (Gold standard). The Information for health care system was collected from PHCs and sub centers (SCs). The information for ICDS was collected from the ICDS office at Taluka (block) level and from each anganwadi worker (AWW). The information for CRS was gathered from Taluka Panchayat Office and from each village secretary (Talati). Data collection by the investigator was done through personal visits carrying out house to house survey in all 51 villages. Houses were covered by using snow ball technique. Due care was taken to ensure that the period of reporting and the denominator population was same for all sources of reporting. In case of infant deaths, the interview was conducted at informant’s house and in the local language. Reason for study was explained to the informant and his or her consent was obtained. Information about ANC, INC and PNC was gathered by interviewing the available parent (preferably mother wherever possible), on a designed questionnaire which was developed with the help of verbal autopsy (VA) questionnaire of various institutions and agencies.(3–5) The data thus collected was entered and analyzed with the help of Epi Info 6.04 version software.
Results
The infant deaths found by the investigator during the study period were 48 and were taken as 100% (gold standard). Five deaths in the study area were not included, where the women belonged to other area and came there (maternal home) for delivery purposes. Other sources during the same period had under reporting and reported only 10 (health system), eight (ICDS) and two (CRS) infant deaths. Information from individual AWK showed 15 infant deaths compared to eight by ICDS office at block level.
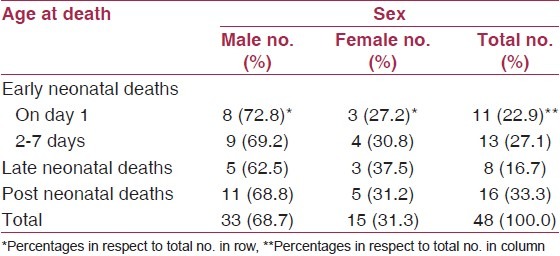
Age distribution showed infant deaths predominantly in neonatal period (66.7%) including 50% within first week and 23% on first day of life. Rests (33.3%) were during post-neonatal period. Sex distribution revealed a consistent preponderance of males (62-72%) in overall infancy as well as during individual periods [Table 1].
Table 1.
Age and sex distribution of infant deaths
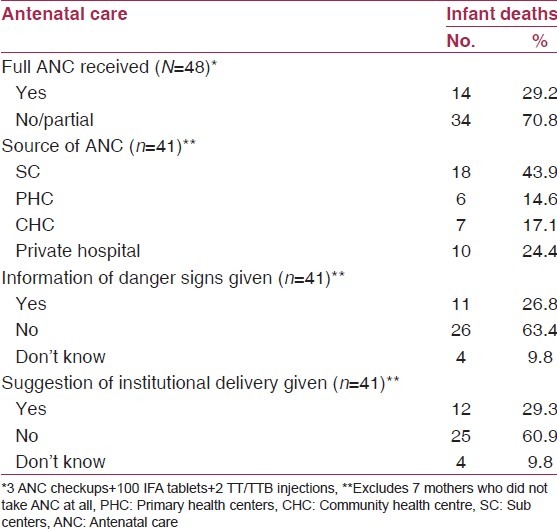
Antenatal care
Out of 48 infant deaths, ANC was not received at all in 7 (14.6%) cases. Only in 14 (29.2%) cases mothers received full ANC (three checkups + 100 Iron Folic acid (IFA) tablets + 2 TT/TTB injections). Source of ANC was government setup in 75.6% cases including SC and PHC/Community Health Centre (CHC) in 43.9% and 31.7% respectively; rests (24.4%) received it from private hospital. In 26.8% cases, ANC was received by home visits of female health worker (FHW). Information about danger signs were provided in 26.8% cases with higher in government (32%) compared to private health facility (10%). Advice of institutional delivery were given in 29.3% cases with better in government (32%) than private facility (20%) [Table 2].
Table 2.
Distribution of infant deaths according to antenatal care
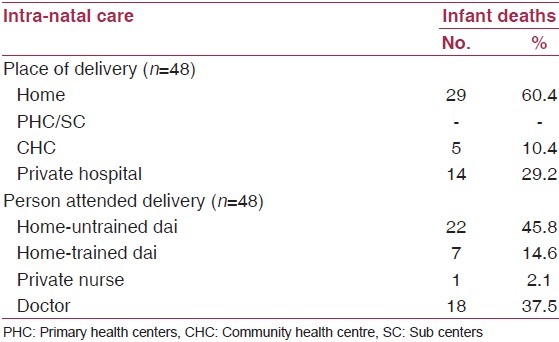
Intra-natal care
Delivery took place at home in 29 (60.4%) infant deaths. Out of 29 home deliveries, 22 were conducted by untrained attendants. While institutional deliveries (39.6%) were only at CHC/Private hospital; not a single delivery took place at SC/PHC [Table 3]. In 25% of cases - all home deliveries, some undesirable substance was applied on the umbilical cord; most common being ash (58.4%), followed by cow dung (25%) and sindoor or vermilion (8.3%).
Table 3.
Distribution of infant deaths according to intra-natal care
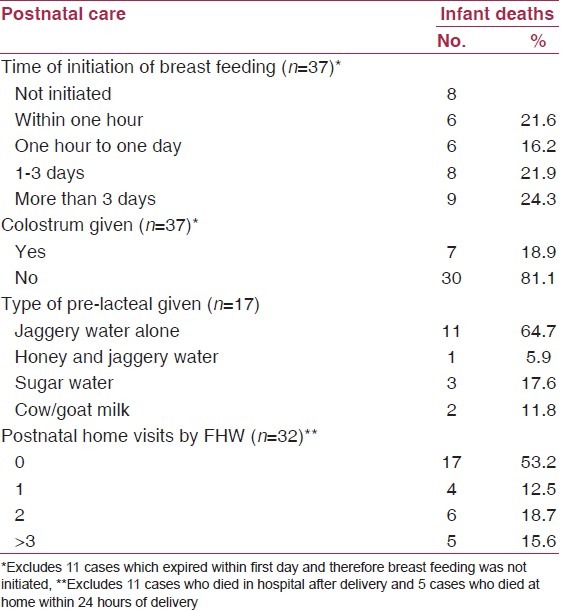
Post natal care
Out of 37 cases (11 died within first day), breastfeeding was initiated only in 29 (78.3%) cases. In 46.2%, it was started after one day. In rest, it was given within 1 day of life including half of them (16.2%) within 1hr of birth. Colostrum was offered only in 18.9% cases of infants. Pre-lacteal feeds were given in 17 cases; most common being jaggery water alone or with honey (70.6%), followed by sugar water (17.6%) and cow/goat milk (11.8%). Contact of infant by FHW in postnatal visits was done in 32 (66.7%) cases. But in 53.2% of those cases, FHW did not go for a home visit. Three or more postnatal home visits were made only in 15.6% cases. While one and two visits were made in 12.5 and 18.7% cases respectively [Table 4].
Table 4.
Distribution of infant deaths according to postnatal care
Discussion
IMR has shown consistent reduction in the past; however the pace of decline has decreased recently and is no more showing the impact of current strategies.(1,2,6–8) Because of non-availability of sample registration system (SRS) data for small units such as PHC, we have to rely mainly on the local agencies like CRS, Health department or ICDS. Under reporting was found in all these agencies with CRS as worst (95.8%), while ICDS and health care system missed 83.3 and 79.2% of total deaths recorded by us. Contrary to our observations, in rural Haryana,(9) AWWs were efficient in recording mortality of “under six children” wherein they picked up 92.4% of these deaths while CRS and Health system could report 16 and 68% deaths respectively. In fact in our study too, infant deaths detected by individual AWW were 15 (31.2%) while the combined number given at block level was surprisingly 8 (16.7%). No explanation was available for it. Common reason for under reporting given by health system and ICDS was that infant deaths among the mothers from other areas are not included as they should go with the area to which these women belong. Other reason to under report such deaths by the health staff is that it may result in series of inquiries and even a punitive action. One early neonatal death was labeled as stillbirth probably for the same reason.
Infant deaths in our study were predominantly in neonatal period (66.7%) similar to Gujarat (67%).(7) In India too, proportion of neonatal mortality in total infant mortality has increased from 62% (NFHS-1, 1992-93) to 68% (NFHS-3, 2005-06).(7) It shows that further reduction in infant mortality can be achieved only by reducing neonatal mortality with interventions designed to improve the health of the mother and her access to care. There is a higher risk of peri-natal and early neonatal mortality among mothers who don’t receive care during pregnancy, labor and the critical hours immediately afterwards.(10,11)
Out of 48 pregnancies in our study, 7 (14.6%) did not receive the ANC at all. In Gujarat(7) and Surat district,(11) 13 and 6.3% mothers respectively did not receive ANC. Aggarwal et al.,(12) recorded no ANC in 4.5% pregnancies. Source of ANC in our study was government health facility in 75.6% cases; double when compared with Gujarat (37.6%).(7) Out of 48 infant deaths, only in 14 (29.2%) cases mothers received full ANC, which was highly variable ranging from 58.6% (rural wardha)(13) to 2.5% (Surat district).(11) Information regarding danger signs during pregnancy and institutional delivery was provided to mothers in 27% and 29% cases respectively. Aggarwal et al.,(12) found it in 4.5% and 31.1% cases correspondingly.
UNICEF estimates based on 192 countries reveal that neonatal mortality increases as deliveries attended by traditional birth attendant increases and decreases as institutional deliveries and deliveries attended by skilled personnel increases.(10) Present study found 75.9% home deliveries and 45.8% of total deliveries by untrained birth attendants, which were 47 and 37% respectively in Gujarat.(7) A study from Maharashtra(13) observed home deliveries in 45% infant deaths and attended by untrained dai in 15% cases.
Studies(14) document role of appropriate breastfeeding practices in the survival of infants. In our study, breast-feeding was not given at all in 8 out of 37 cases (39.6%) much more than in Gujarat (3.2%).(7) It was initiated within the first day of life in 32.4% cases including half of them within 1hr of birth, while in Gujarat they were 58% and 28% respectively.(7) Pre-lacteal feeds given in 35.4% infant deaths were comparatively less than Gujarat (57%). Bottle-feeding was found in 3 (6.2%) cases, comparable with Gujarat (7.7%).(7) FHW didn’t go for a single home visit after delivery in 53.2% cases, which was 39% in Gujarat.(7) This in itself may be a reason for under reporting of infant deaths in this study. In our study, role of FHW in providing ante, intra and postnatal care was unsatisfactory and not a single delivery was done at sub center (SC) or PHC. It reflects that community does not have faith and avail such basic services. Considering the pivotal role of PHC and SC in providing such essential care, they need to be involved more actively.
Conclusion
Barring CRS which is a general agency, under reporting on the part of health system and ICDS is worrisome because they implement various programs to reduce the burden of infant deaths. This event recording and reporting is crucial because actions to prevent such deaths come only thereafter. These two agencies need to be sensitized about the importance of their work and to work in coordination to produce at least same reports. In addition to infant care after delivery, quality antenatal and intra natal services becomes very crucial for further reduction in IMR, as proportion of infant deaths in neonatal period and that too in early neonatal period is growing every day.
Looking to the causes of under reporting in this study especially in health department, it can be suggested that health staff who reports infant death should not be harassed or punished for the occurrence in his/her area. On the contrary person should be encouraged to report such events. Verbal autopsy of all such cases should be done at the earliest with complete details. In cases where the woman has received the ANC, special attempts should be made to know the reasons for her dropping out later. Most deaths occurred within first seven days which again emphasizes the need of first PNC visit in preventing infant deaths.
Limitations
The under reporting of infant deaths reported in this study should be viewed in relation of the facts that (1) it refers to a remote tribal block and (2) period of 2004-05. Therefore it may be a worst case scenario of that period. Since than the situation might have changed for better as thereafter state government has started e-mamta initiative where every woman right from the pregnancy is tracked and kept throughout in the loop of health services.
Selection bias in terms of willingness of local facilities for participation in this study is important while interpreting the findings of this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gupta I, Trivedi M. The slow decline in the infant mortality rate in India. JHD. 2008;4:87–102. [Google Scholar]
- 2.RGI. Sample Registration System Bulletin. 2011;45:1. [Google Scholar]
- 3.Bang AT, Bang RA. Diagnosis of causes of childhood deaths in developing countries by verbal autopsy: Suggested criteria. Bull World Health Organ. 1992;70:499–507. [PMC free article] [PubMed] [Google Scholar]
- 4.RGI. Sample Registration System: Verbal Autopsy. Manual of Instructions for supervisors Registrar General of India, Vital Statistics Division, West Block 1, Wing 1, 2nd Floor, R K Puram, New Delhi, 2004 Sample Registration System: Verbal Autopsy manual of instructions for supervisors. [Last accessed on 2012 Sept 9]. Available from: http://www.researchgate.net/publication/43509841_Sample_Registration_System_Verbal_autopsy_manual_of_instructions_for_supervisors .
- 5.Aga Khan Foundation. Primary Health Care Management Advancement Program. Geneva: Aga Khan Foundation; 1993. User’s Guide. [Google Scholar]
- 6.National Family Health Survey (NFHS-3), 2005-06: India. Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 7.National Family Health Survey (NFHS-3), India, 2005-06: Gujarat. Mumbai: IIPS; 2008. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 8.Lal S, Kumar V, Vashisht B, Malik J, Punia M. Surveillance of vital events in rural areas? [Last accessed on 2011 Jul 14];Indian J Community Med. 1998 23:156–60. Available from: http://www.ijcm.org.in/showbackIssue.asp?issn=0970-0218:year=1998;volume=23; issue=4 . [Google Scholar]
- 9.Chatterjee C, Das K, Bhattacharya S, Ram R. Study of some maternal risk factors influencing early neonatal mortality. Indian J Community Med. 1998;23:87–90. [Google Scholar]
- 10.Lawn JE, Cousens S, Bhutta ZA, Darmstadt GL, Martines J, Paul V. Why are 4 million newborn babies dying each year? Lancet. 2004;364:399–401. doi: 10.1016/S0140-6736(04)16783-4. [DOI] [PubMed] [Google Scholar]
- 11.Govt. of India. Report prepared for Ministry of Health and Family welfare. New Delhi: Govt of India; 2002-03. RCH Rapid Household Survey phase-I, Surat district. [Google Scholar]
- 12.Aggarwal A, Kumar R, Kumar P. Early neonatal mortality in a hilly north Indian state: Socio-demographic factors and treatment seeking behavior. Indian J Prev Soc Med. 2003;34:46–52. [Google Scholar]
- 13.Varkey S. A thesis submitted to Nagpur University. 2003. Role of verbal autopsy in investigating the causes of infant deaths in rural Wardha. [Google Scholar]
- 14.Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, Becker S. Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics. 2001;108:67. doi: 10.1542/peds.108.4.e67. [DOI] [PubMed] [Google Scholar]


