Abstract
Objectives
Although it is well known that people with alcohol dependence are at a markedly elevated risk for suicide, much less is known about the role of acute alcohol use in suicidal behaviours. The primary aims of this epidemiological study were to assess the prevalence and factors associated with acute alcohol intoxication among 57 813 suicide decedents in 16 states.
Methods
Data from the restricted National Violent Death Reporting System 2003–2009 for male and female suicide decedents aged 18 years and older were analysed by multiple logistic regression to compare decedents with and without acute alcohol intoxication (defined as blood alcohol concentration (BAC) ≥0.08 g/dl).
Results
Among men, those who were younger, American Indian/Alaska Native, Hispanic, veterans, of lower educational attainment, deceased from a self-inflicted firearm injury or hanging/suffocation and residing in rural areas were more likely to have been intoxicated at the time of death. Among women, the factors associated with a BAC ≥0.08 g/dl were younger age, being American Indian/Alaska Native, and using a firearm, hanging/suffocation or falling as method of death.
Conclusions
In both men and women, alcohol intoxication was associated with violent methods of suicide and declined markedly with age, suggesting that addressing risks associated with acute alcohol use may be of the greatest aid in the prevention of violent suicides among young and middle age adults.
Introduction
Suicide is a major public health problem in the USA and around the world.1, 2 With nearly 37 000 deaths annually, suicide ranked as the 10th leading overall cause of death in the USA in 2009.3 The age-adjusted suicide rates for male and female subjects were 19.2 and 5.0 per 100 000 population, respectively.3 One of the most well-established findings in the suicide research field is that ongoing difficulties with alcohol as exemplified by an alcohol use disorder (ie, alcohol abuse, alcohol dependence) confer an increased risk for suicide.4, 5 A comprehensive review of cohort studies estimated that individuals with alcohol dependence who come to clinical attention are at approximately ninefold higher risk to die by suicide compared with the general population.5 A meta-analysis of psychological autopsy studies worldwide concluded that alcohol use disorders confer increased risk and are second only to mood disorders as the most common condition among suicide decedents.4
Besides chronic alcohol use, it is also essential to consider the role of acute use of alcohol in suicide, which is the use of alcohol in the final hours of life. Indeed, acute use of alcohol preceding suicidal behaviour is also highly prevalent, with a systematic review reporting that a median of 37% of suicide decedents (range 10%–69%) and 40% of non-lethal suicide attempters (range 10%–73%) had used alcohol prior to the event.6 Moreover, prior analyses suggest that acute use of alcohol confers greater risk for suicide attempt7, 8 and suicide9 than the risk attributable to pattern of alcohol use. Data comparing risk associated with acute and chronic alcohol use on other types of injuries show similar results,10, 11 reinforcing that acute use of alcohol is a potent independent risk factor over and above any risk conferred by chronic alcohol use pattern.
Collectively, data on suicide and non-lethal suicide attempts suggest that it is essential to consider both chronic patterns of alcohol use and acute use of alcohol in suicidal behaviour, yet the data on acute use of alcohol are much more limited, particularly when considering suicide mortality studies. Although it is well known that people with alcohol dependence are at markedly elevated risk for suicide,5, 12 much less is known about the role of acute alcohol use in suicidal behaviours.6 Research on toxicological characteristics has typically been constrained by small samples and limited geographic coverage.13 Consequently, with the exception of a recent controlled report on acute use of alcohol and firearm suicides in a large urban area,9 existing research about acute alcohol use and suicide is limited and largely provides a demographic description of suicide decedents along with exploratory correlational analyses. Yet, more and better data on acute alcohol use and suicide are essential if suicides among drinkers are to be reduced. Newly available data from the National Violent Death Reporting System (NVDRS) can be used to address this issue.
The purpose of the present study was to provide a comprehensive descriptive epidemiological profile stratified by gender of blood alcohol concentration (BAC) levels among 57 813 suicide decedents in 16 states. Specifically, the aims of the research were to (a) estimate the prevalence of BAC ≥0.08 g/dl (which, as noted by the US Department of Transportation,14 is consistent with driving while intoxicated laws in many states) among suicide decedents and (b) examine the socio-demographic factors associated with acute alcohol intoxication among suicide decedents.
Methods
Data source
This study used restricted data for decedents aged 18 years and older from the 2003–2009 NVDRS. The NVDRS is a state-based active surveillance system that provides a detailed account of violent deaths that occur in the participating states. Although a smaller cohort of states participated in 2003 and 2004, as of 2005, 16 states (Alaska, Colorado, Georgia, Kentucky, Maryland, Massachusetts, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, South Carolina, Rhode Island, Utah, Virginia and Wisconsin) contributed data to the NVDRS. The data were gathered from the coroner/medical examiner (C/ME) records; police reports; death certificates; toxicology laboratories; crime laboratories; and alcohol, tobacco, firearms and explosives firearm trace reports. Information on acute alcohol use is based on toxicological analyses of decedents as part of the C/ME investigation. Suicide decedents were identified as those with death certificates that listed International Classification of Diseases, 10th Revision codes X60–84 or Y87.0. A total of 57 813 persons died by suicide in the 16 NVDRS states during 2003–2009.
Measures
Measures included in the analyses were based on previous findings in the literature. The main outcome of the analysis was legal limit for intoxication for driving (BAC ≥0.08 g/dl) versus below the limit (BAC <0.08 g/dl) at the time of suicide. Blood alcohol levels were coded as a continuous measure in terms of weight by volume, and then classified as <0.08 g/dl or ≥0.08 g/dl. More than three-quarters (76%) of all decedents were tested for the presence of alcohol. Socio-demographic variables, obtained from death certificates, included gender, age groups (18–24, 25–34, 35–44, 45–54, 55–64, 65–74 and 75+), race/ethnicity (white, African American, American Indian/Alaska Native, Asian/Pacific Islander and Hispanic), educational attainment (<12 years, 12 years, more than 12 years of education), veteran status and metropolitan status. Of note, in all but two states, educational attainment was missing in fewer than 10% of the cases. Only in Rhode Island and Georgia, where the data are gathered on a voluntary basis, did the education missing rate exceed 95%. Therefore, a `missing' category was included to maximise the number of cases in the multivariate analysis. Counties of residence were assigned a rural–urban continuum code based on a classification system developed by the US Department of Agriculture Economic Research Service.15 The continuum contains nine categories and characterises metropolitan counties by population size and non-metropolitan counties by level of urbanisation and proximity to metropolitan areas. The categories range from `1' (counties in metropolitan areas of 1 million population or more) to `9' (completely rural counties or those with <2500 urban population, not adjacent to a metropolitan area). The nine categories were then reduced to two categories: metropolitan (codes 1 through 3) and non-metropolitan (codes 4 through 9) status. In addition, mental health and substance abuse information, obtained from family, friends, other informants or scene investigation, included mental health status (`perceived' depressed mood and diagnosed with a mental health problem), chronic alcohol problem and other substance abuse problem.
Statistical analysis
Descriptive and logistic regression analyses were conducted. The prevalence of male and female decedents with a BAC ≥0.08 g/dl was estimated and compared using Pearson's χ2 tests. Multiple logistic regression analyses were then used to examine the independent effect of discrete socio-demographic factors on the odds of intoxication (BAC ≥0.08 g/dl vs <0.08 g/dl) at the time of death by suicide. Separate logistic models were constructed for male and female suicide decedents. All analyses were performed using the Statistical Package for the Social Sciences (V.19.0). Although fewer states participated in the NVDRS in 2003–2004, a sensitivity analysis revealed that the estimates with and without these 2 years were virtually identical (data not shown).
Results
Table 1 describes the suicide decedents who were chiefly male, middle-aged, white and urban residents. The decedents generally had high school or greater education and were not veterans of military service. Male and female decedents were each (on average) about 47 years old but both younger and older men were over-represented among the deceased compared with the women. Male subjects had less education than female subjects. Whereas most male decedents employed firearms for suicide, proportionately more female suicide decedents used poisoning.
Table 1.
Characteristics of suicide decedents
| Men | Women | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age | ||||
| 18–24 | 5,258 | 11.6 | 975 | 7.8 |
| 25–34 | 7,411 | 16.3 | 1,780 | 14.3 |
| 35–44 | 9,145 | 20.1 | 2,879 | 23.2 |
| 45–54 | 9,893 | 21.8 | 3,395 | 27.3 |
| 55–64 | 6,284 | 13.8 | 1,971 | 15.9 |
| 65–74 | 3,488 | 7.7 | 759 | 6.1 |
| 75+ | 3,907 | 8.6 | 665 | 5.4 |
| Race/Ethnicity | ||||
| White | 38,509 | 85.1 | 10,843 | 87.4 |
| African American | 3,340 | 7.4 | 641 | 5.2 |
| American Indian/Alaska Native | 737 | 1.6 | 198 | 1.6 |
| Asian/Pacific Islander | 648 | 1.4 | 341 | 2.7 |
| Hispanic | 2,032 | 4.5 | 384 | 3.1 |
| Veteran Status | ||||
| Veteran | 11,393 | 27.6 | 383 | 3.4 |
| Non-veteran | 29,917 | 72.4 | 10,861 | 96.6 |
| Educational Attainment | ||||
| <12 years | 8,458 | 21.6 | 1,649 | 15.2 |
| 12 years | 18,671 | 47.6 | 18,671 | 43.2 |
| >12 years | 12,084 | 30.8 | 12,084 | 41.6 |
| Suicide Method | ||||
| Firearm | 25,321 | 55.8 | 3,877 | 31.2 |
| Sharp or blunt instrument | 934 | 2.1 | 199 | 1.6 |
| Poison | 5,569 | 12.3 | 4,924 | 39.6 |
| Hanging or suffocation | 10,369 | 22.9 | 2,283 | 18.4 |
| Fall | 722 | 1.6 | 277 | 2.2 |
| Drowning | 437 | 1.0 | 238 | 1.9 |
| Other | 2,002 | 4.4 | 622 | 5.0 |
| Metropolitan Status | ||||
| Metropolitan | 34,341 | 76.7 | 9,800 | 79.8 |
| Non-metropolitan | 10,432 | 23.3 | 2,480 | 20.2 |
| BAC | ||||
| < .08 g/dl | 22,742 | 76.3 | 7,121 | 82.8 |
| ≥ .08 g/dl | 7,025 | 23.7 | 1,463 | 17.2 |
Characteristics of all suicide decedents
Among suicide decedents tested for alcohol, men were more likely than women to have alcohol present at the time of death (36% vs 29%, p<0.001). Acute intoxication (defined as BAC ≥0.08 g/dl) was found in 24% of men and 17% of women. Moreover, 21% and 9% of male decedents had BACs ≥0.10 g/dl and ≥0.20 g/dl, respectively. Conversely, among women, 15% and 7% had BACs ≥0.10 g/dl and ≥0.20 g/dl, respectively.
Table 2 shows that prevalence of acute intoxication peaked between 35 and 44 years, and then decreased with older age for both genders. Regarding race and ethnicity, the prevalence of acute intoxication was the highest among American Indians/Alaska Natives for both genders. Educational attainment was significantly correlated with intoxication among male suicide decedents. Male subjects with 12 years of education (25%) or <12 years (26%) were more likely to be intoxicated than those with more than 12 years of education (21%, p<0.001). No such correlation was observed among female suicide decedents. Decedents who had served in the military were less likely than non-veterans to have been intoxicated at time of death. Men who used the most lethal suicide methods (as defined by Shenassa et al 16) were most likely to be intoxicated at the time of death (25% of those who used firearms and 25% of those who died from hanging, respectively).
Table 2.
Characteristics of suicide decedents with BACs ≥ 0.08 g/dl
| Men | Women | |||
|---|---|---|---|---|
| n | % | n | % | |
| Age | ||||
| 18–24 | 3,131 | 25.1 | 721 | 19.7 |
| 25–34 | 5,238 | 28.6 | 1,324 | 18.9 |
| 35–44 | 6,395 | 29.3 | 2,090 | 20.6 |
| 45–54 | 6,794 | 26.0 | 2,479 | 18.7 |
| 55–64 | 4,078 | 20.5 | 1,376 | 13.5 |
| 65–74 | 2,110 | 11.3 | 501 | 7.6 |
| 75+ | 2,211 | 4.6 | 410 | 5.1 |
| Race/Ethnicity | ||||
| White | 25,599 | 23.9 | 7,705 | 17.3 |
| African American | 2,461 | 16.9 | 489 | 10.6 |
| American Indian/Alaska Native | 466 | 40.8 | 140 | 32.9 |
| Asian/Pacific Islander | 468 | 14.3 | 249 | 10.4 |
| Hispanic | 1,520 | 29.8 | 311 | 22.8 |
| Veteran Status | ||||
| Veteran | 7,342 | 25.3 | 280 | 18.2 |
| Non-veteran | 20,505 | 20.0 | 7,776 | 17.4 |
| Educational Attainment | ||||
| <12 years | 5,938 | 25.9 | 1,190 | 17.5 |
| 12 years | 13,117 | 25.4 | 3,453 | 17.7 |
| >12 years | 8,798 | 20.5 | 3,442 | 16.7 |
| Suicide Method | ||||
| Firearm | 16,833 | 25.4 | 2,607 | 20.9 |
| Sharp or blunt instrument | 659 | 12.0 | 147 | 10.9 |
| Poison | 4,320 | 19.1 | 3,892 | 14.1 |
| Hanging or suffocation | 7,314 | 24.9 | 1,631 | 19.4 |
| Fall | 512 | 12.3 | 207 | 16.4 |
| Drowning | 288 | 22.2 | 184 | 17.9 |
| Other | 635 | 20.9 | 233 | 16.3 |
| Metropolitan Status | ||||
| Metropolitan | 24,123 | 23.1 | 7,220 | 16.9 |
| Non-metropolitan | 6,260 | 26.4 | 1,634 | 18.2 |
Characteristics of suicide decedents with BACs ≥0.08 g/dl
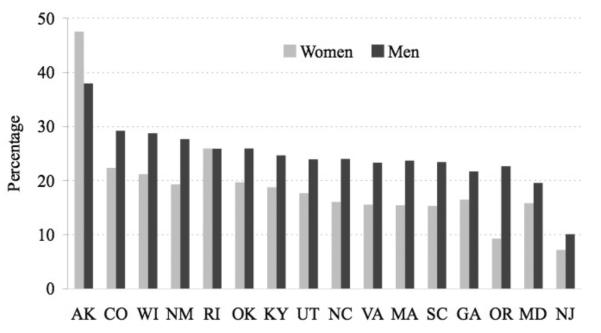
The prevalence of BAC ≥0.08 g/dl among men was higher in non-metropolitan than metropolitan areas (p<0.001). Although most NVDRS states had, on average, BAC ≥0.08 g/dl prevalence rates below 30%, Alaska's rate exceeded 40% (figure 1).
Figure 1.
Percent of suicide decedents with a blood alcohol concentration ≥0.08 g/dl by National Violent Death Reporting System states and gender. AK, Alaska; CO, Colorado; GA, Georgia; KY, Kentucky; MA, Massachusetts; MD, Maryland; NC, North Carolina; NJ, New Jersey; NM, New Mexico; OK, Oklahoma; OR, Oregon; RI, Rhode Island; SC, South Carolina; UT, Utah; VA, Virginia; WI, Wisconsin.
Table 3 presents the adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for BAC ≥0.08 g/dl. All the independent variables were entered simultaneously into gender-stratified multivariate logistic models. Among the male decedents, those who were younger, American Indian/Alaska Native, Hispanic, veterans, of lower educational attainment, deceased from a self-inflicted firearm injury or hanging/suffocation, and residing in rural areas were more likely to have been intoxicated at the time of death. Among women, the factors associated with a BAC ≥0.08 g/dl were younger age, being American Indian/Alaska Native, and using a firearm, hanging/suffocation, falling or drowning as the method of death.
Table 3.
Factors associated with acute alcohol intoxication (BAC ≥ .08 g/dl) among suicide decedents
| Men | Women | |
|---|---|---|
| AOR (95%CI) | AOR (95%CI) | |
| Age | ||
| 18–24 | 1.00 | 1.00 |
| 25–34 | 128 (1.16 – 1.42) | 1.07 (0.84 – 1.37) |
| 35–44 | 133 (1.21 – 1.47) | 1.10 (0.87 – 1.38) |
| 45–54 | 1.12 (1.01 – 1.23) | 1.07 (0.85 – 1.34) |
| 55–64 | 0.78 (0.70 – 0.88) | 0.65 (0.50 – 0.84) |
| 65–74 | 033 (0.28 – 0.38) | 037 (0.25 – 0.55) |
| 75+ | 0.12 (0.10 – 0.15) | 025 (0.15 – 0.41) |
| Race / Ethnicity | ||
| White | 1.00 | 1.00 |
| African American | 0.53 (0.47 – 0.59) | 0.46 (0.34 – 0.63) |
| American Indian / Alaska Native | 1.78 (1.46 – 2.17) | 1.99 (136 – 2.90) |
| Asian / Pacific Islander | 0.59 (0.44 – 0.77) | 0.50 (0.32 – 0.79) |
| Hispanic | 1.19 (1.06 – 1.35) | 1.28 (0.96 – 1.71) |
| Veteran Status | ||
| Veteran | 1.12 (1.04 – 1.20) | 1.04 (0.75 – 1.42) |
| Non-veteran | 1.00 | 1.00 |
| Educational Attainment | ||
| <12 years | 1.41 (1.29 – 1.54) | 1.11 (0.91 – 1.35) |
| 12 years | 124 (1.15 – 1.33) | 1.07 (0.94 – 1.23) |
| >12 years | 1.00 | 1.00 |
| Missing | 1.11 (0.99 – 1.25) | 1.09 (0.87 – 1.36) |
| Suicide method | ||
| Firearm | 1.76 (1.61 – 1.93) | 1.68 (1.46 – 1.93) |
| Sharp or blunt instrument | 0.66 (0.51 – 0.86) | 0.69 (0.37 – 1.26) |
| Poison | 1.00 | 1.00 |
| Hanging or suffocation | 138 (1.25 – 1.53) | 1.48 (1.25 – 1.75) |
| Fall | 0.75 (0.56 – 1.00) | 1.51 (1.01 – 2.27) |
| Drowning | 1.38 (0.99 – 1.94) | 1.61 (1.05 – 2.47) |
| Other | 1.12 (0.89 – 1.41) | 1.20 (0.81 – 1.78) |
| Metropolitan Status | ||
| Metropolitan | 1.00 | 1.00 |
| Non-metropolitan | 1.09 (1.02 – 1.17) | 0.95 (0.81 – 1.10) |
AOR: adjusted odd ratio; CI: confidence interval. Significant findings at p<0.05 are in bold.
Factors associated with acute alcohol intoxication (BAC ≥0.08 g/dl) among suicide decedents
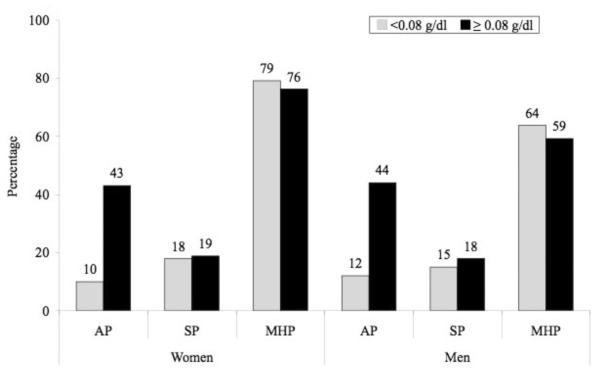
Finally, we compared the substance use and mental health characteristics of suicide decedents with BAC <0.08 g/dl versus ≥0.08 g/dl (separately by gender). It is important to note here that these variables were coded as `1' (presence of the circumstance could be determined) and `0' (not present or no information was available from C/ME or police reports to reliably ascertain their presence or absence). Figure 2 shows that the two BAC groups were similar in terms of the prevalence of mental health and other substance problems. In contrast, and not surprisingly, the rate of chronic alcohol problem was substantially higher among male and female suicide decedents who were acutely intoxicated at the time of death.
Figure 2.
Comparison of substance use and mental health variables of suicide decedents with blood alcohol concentration <0.08 g/dl and ≥0.08 g/dl by gender. AP, alcohol problem (including dependence); MHP, current mental health problem including mental illness diagnosis and/or current depressed mood; SP, substance problem other than alcohol. These percentages are based on suicides for which circumstances could be determined from official sources.
Discussion
Similar to previous findings,17, 18 the present study found that up to 24% of male and 17% of female suicide decedents were intoxicated at the time of death. The study shows that the prevalence of acute intoxication at the time of death was the highest among male subjects, persons aged 35–44 years, American Indians/Alaska Natives and male subjects with less education.
Some findings likely reflect patterns of alcohol consumption in the general population. Of course, it is well known that male subjects are more likely to drink alcohol than women. For example, the 2010 National Survey on Drug Use and Health (NSDUH)19 found that among persons aged 18 and over, 91% of male subjects had ever consumed alcohol versus only 84% of female subjects. Among adult drinkers, 63% of men had consumed alcohol in the past month versus only 50% of women. Moreover, male drinkers typically consume more alcohol than female subjects. For example, the 2010 NSDUH found that the past month prevalence of binge drinking (five or more drinks on an occasion) was 33% for men versus 16% for women.
The results reported here clearly show dramatic differences by race/ethnicity. Compared with other population subgroups, American Indians/Alaska Natives had the highest prevalence of acute alcohol intoxication regardless of gender. These results are consistent with those of other studies that found American Indians/Alaska Natives have a higher prevalence of every alcohol outcome analysed (including suicide) compared with all other racial/ethnic groups.20 Of note, a recent analysis of National Epidemiologic Survey on Alcohol and Related Conditions data (2001–2002) showed that the prevalence of weekly heavy drinking (ie, eight or more drinks per week for women and 15 or more drinks per week for men) among American Indian/Alaska Native women was slightly higher than the rate for men (22.2% vs 21.6%, respectively).21 Therefore, intervention and prevention programmes to reduce acute alcohol use are urgently needed to lower the incidence of alcohol-associated suicides in population subgroups at especially high risk such as American Indians/Alaska Natives. Furthermore, regulating the availability of alcohol in geographically isolated communities, such as those in Alaska, may be an effective public health intervention to reduce alcohol-associated suicides.22
Indeed, population-wide policies designed to reduce inappropriate alcohol use might lower overall rates of suicide related to acute intoxication. For example, in a study of the impact of state alcohol policy on suicide in the former Union of Soviet Socialist Republics, Värnik et al 23 found that rigorous alcohol restrictions produced a decrease in BAC-positive suicide mortality among both genders. A major implication is that overall alcohol regulation, as noted in Babor et al,24 might be an effective universal (also known as primary) suicide prevention strategy.
On the other hand, findings such as the peak of alcohol intoxication prevalence among middle-aged suicide decedents are not easily explained. In the 2010 NSDUH, the highest prevalence of past month binge drinking was 41% in the youngest age group (18 through 25) whereas for persons aged 35 through 49 the prevalence was only 27%. More research is needed to understand the demographic details of acute alcohol intoxication among suicide decedents. This information could lead to targeted (also known as secondary) prevention strategies designed for population subgroups at high risk of alcohol-associated suicide. Research in this area can aid in the harmonisation of alcohol policy and suicide prevention strategies. For example, the data suggest there may be value in designing programmes for reducing intoxication among middle-aged individuals. Such programmes might logically be housed in healthcare or workplace venues frequented by individuals in this age group.
This study also makes a key contribution to understanding health consequences associated with alcohol use. Again, the high prevalence of intoxication among young and middle-aged suicide decedents is especially noteworthy. The implication here is that acute alcohol ingestion may be associated with substantial years of potential life lost. Future work can address the possibility that alcohol sales are connected with social losses not balanced by ethanol taxes.
These data have clinical implications for indicated (also known as tertiary) prevention strategies. In this regard, it is worth noting that prevalence of acute intoxication declined markedly with age. Indeed, intoxication was rare among decedents over the age of 65. Previous work has shown that functional limitations (often associated with ageing) as well as psychiatric conditions are powerful predictors of suicide.25 Consequently, suicide prevention efforts for older individuals should focus chiefly on health-related issues.
Conversely, alcohol intoxication needs to be addressed for younger individuals at risk of suicide. Other studies suggest that acute alcohol consumption serves as an intermediate or facilitator factor between the `reason' for suicide and its consummation, and not only as a risk factor itself.26–28 In other words, acute alcohol use may act as a behavioural disinhibitor. Indeed, for some intoxicated individuals, the act of self-destruction may have been precipitous and (almost by definition) not the result of sober reflection. Elimination or (at least) minimisation of alcohol consumption by high-risk individuals could be a powerful strategy for suicide prevention in this age group (eg, through easier access to screening, brief intervention and referral services).29 Alcohol taxation would be an appropriate mechanism to finance such services.
Although the study's focus on acute alcohol use and suicide, as opposed to chronic alcohol use, is substantially innovative, the findings are subject to several limitations. First, there is variation across states in the percent of suicide decedents who were tested for blood alcohol levels. Fortunately, only two states (Alaska and Oregon) had low BAC testing rates (45% and 24%, respectively). A sensitivity analysis was performed where the states of Oregon and Alaska were excluded (data not shown). The patterns of results were not altered. Second, coroners and medical examiners may be less likely to test decedents considered unlikely to have an alcohol problem or where the cause of death is obvious (eg, non-toxicological) and the alcohol concentration is viewed as a correlate. In addition, toxicology testing is often determined by availability of state or local funding. Unfortunately, federal resources provided to the NVDRS states do not cover toxicological testing. However, in a supplementary analysis (data not shown), all demographic subgroups under the age of 65 had toxicological testing rates at or above 70% (for decedents 65 and older the testing rate was 65%). Third, the NVDRS, as noted above, is limited to 16 states. Finally, other known risk factors for suicide that could confound significantly the association investigated (eg, social support, unemployment) were not available in the NVDRS.
Despite these limitations, data from the NVDRS have numerous strengths. First, the NVDRS is the only surveillance system for recent violent deaths in the USA. Second, the NVDRS collects information from multiple sources to characterise violent deaths as opposed to using only death certificates (which contain limited data). Third, the NVDRS is the first to provide BAC for suicide decedents. Fourth, although the NVDRS states are not necessarily representative of the USA, the populations of these 16 states are similar to the country as a whole in terms of gender, age, ethnic/racial composition, urban/rural characteristics and overall suicide rates.3, 30 Finally, collection of postmortem data are particularly challenging when states have decentralised medico-legal death investigative systems rather than a centralised C/ME system. It is worth noting that 69% of the states participating in the NVDRS have a centralised C/ME compared with only 15% in non-NVDRS states.31
In summary, suicide remains a significant global public health problem and alcohol is a common concomitant of suicidal behaviour. Therefore, future investigations should focus on how modifiable alcohol control policies (eg, hours of sales, price, taxes and density of outlets) may reduce the incidence of alcohol-associated suicides.
What is already known on the subject
Alcohol use disorders confer increased risk for suicide mortality.
Although it is well known that people with alcohol dependence are at a markedly elevated risk for suicide, much less is known about the role of acute alcohol use in the final hours of life.
What this study adds
A sizeable proportion of male and female suicide decedents were legally intoxicated at the time of death.
Patterns of acute alcohol intoxication varied substantially among population subgroups, including age, race/ethnicity, education and veteran status.
Results of the present study could lead to targeted prevention strategies designed for population subgroups at high risk of alcohol-associated suicide.
Acknowledgments
Funding This study was supported by grant R01 AA020063 from the National Institute on Alcohol Abuse and Alcoholism. All analyses, interpretations and conclusions based on the analysis of these data are solely the responsibility of the authors.
Ethics approval Ethics approval was provided by the Portland State University Human Subjects Research Review Committee.
Footnotes
Contributors MK originated the study, led the writing and synthesised the analyses. BMcF and NH provided important intellectual content and helped draft the manuscript. MK and NH acquired the data. BMcF provided statistical expertise. KC, RC, NG and KN helped conceptualise ideas, interpret findings and review drafts of the manuscript. All the authors reviewed and approved the final draft.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Nock MK, Borges G, Bromet EJ, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–54. doi: 10.1093/epirev/mxn002. Abstract/FREE Full text. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Research Council . Reducing Suicide: A National Imperative. The National Academies Press; Washington, DC: 2002. [Google Scholar]
- 3.Centers for Disease Control and Prevention. National Centers for Injury Prevention and Control [(accessed 22 Feb 2012)];Web-based Injury Statistics Query and Reporting System (WISQARS) 2009 http://www.cdc.gov.proxy.bib.uottawa.ca/ncipc/wisqars.
- 4.Cavanagh JT, Carson AJ, Sharpe M, et al. Psychological autopsy studies of suicide: a systematic review. Psycholo Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. CrossRef. [DOI] [PubMed] [Google Scholar]
- 5.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;(76 Suppl):S11–19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Cherpitel CJ, Borges GL, Wilcox HC. Acute alcohol use and suicidal behavior: a review of the literature. Alcohol Clin Exp Res. 2004;28(5 Suppl):18S–28S. doi: 10.1097/01.alc.0000127411.61634.14. [CrossRef][Medline] [DOI] [PubMed] [Google Scholar]
- 7.Powell KE, Kresnow MJ, Mercy JA, et al. Alcohol consumption and nearly lethal suicide attempts. Suicide Life Threat Behav. 2001;(32 Suppl):30–41. doi: 10.1521/suli.32.1.5.30.24208. [DOI] [PubMed] [Google Scholar]
- 8.Borges G, Cherpitel CJ, MacDonald S, et al. A case-crossover study of acute alcohol use and suicide attempt. J Stud Alcohol. 2004;65:708–14. doi: 10.15288/jsa.2004.65.708. [Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 9.Branas CC, Richmond T, Ten Have TR, et al. Acute alcohol consumption, alcohol outlets, and gun suicide. Subst Use Misuse. 2011;46:1592–603. doi: 10.3109/10826084.2011.604371. [CrossRef][Medline][Web of Science] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vinson DC, Borges G, Cherpitel CJ. The risk of intentional injury with acute and chronic alcohol exposures: a case—control and case crossover study. J Stud Alcohol. 2003;64:350–7. doi: 10.15288/jsa.2003.64.350. [Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 11.Vinson DC, Maclure M, Reidinger C, et al. A population-based case-crossover and case-control study of alcohol and the risk of injury. J Stud Alcohol. 2003;64:358–66. doi: 10.15288/jsa.2003.64.358. [Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 12.Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–33. doi: 10.1016/S0140-6736(09)60746-7. [CrossRef][Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 13.Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: a metaanalysis. Ann Emerg Med. 1999;33:659–68. [Medline][Web of Science] [PubMed] [Google Scholar]
- 14.U.S. Department of Transportation Research and innovative Technology Administration Bureau of Transportation Statistics [(accessed 22 Dec 2011)];National Transportation Statistics. 2010 http://www.bts.gov.proxy.bib.uottawa.ca/publications/national_transportation_statistics/
- 15.United States Department of Agriculture Economic Research Service [(accessed 20 Apr 2009)];Measuring rurality: Rural-Urban Continuum Codes. 2003 www.ers.usda.gov/briefing/rurality/ruralurbcon/
- 16.Shenassa ED, Catlin SN, Buka SL. Lethality of firearms relative to other suicide methods: a population based study. J Epidemiol Community Health. 2003;57:120–4. doi: 10.1136/jech.57.2.120. [Abstract/FREE Full text] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holmgren A, Jones AW. Demographics of suicide victims in Sweden in relation to their blood-alcohol concentration and the circumstances and manner of death. Forensic Sci Int. 2010;198:17–22. doi: 10.1016/j.forsciint.2009.12.015. [CrossRef][Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Alcohol and suicide among racial/ethnic populations -17 states, 2005–2006. MMWR Morb Mortal Wkly Rep. 2009;58:637–41. [Medline] [PubMed] [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration . Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. (NSDUH Series H-41). HHS Publication No. (SMA) 11-4658. [Google Scholar]
- 20.Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiol Rev. 2012;34:89–102. doi: 10.1093/epirev/mxr018. [Abstract/FREE Full text] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chartier K, Caetano R. Ethnicity and health Disparities in alcohol research. Alcohol Res Health. 2010;33:152–60. [Medline][Web of Science] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiu AY, Perez PE, Parker RN. Impact of banning alcohol on outpatient visits in Barrow, Alaska. JAMA. 1997;278:1775–7. [CrossRef][Medline][Web of Science] [PubMed] [Google Scholar]
- 23.Värnik A, Kõlves K, Väli M, et al. Do alcohol restrictions reduce suicide mortality? Addiction. 2007;102:251–6. doi: 10.1111/j.1360-0443.2006.01687.x. [Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 24.Babor T, Caetano R, Casswell S, et al. Alcohol: No Ordinary Commodity—Research and Public Policy—Revised Edition. Oxford University Press; Oxford: 2010. [Google Scholar]
- 25.Kaplan MS, McFarland BH, Huguet H, et al. Physical illness, functional limitations, and suicide risk: a population-based study. Am J Orthopsychiatry. 2007;77:56–60. doi: 10.1037/0002-9432.77.1.56. [CrossRef][Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 26.Kaplan MS, McFarland BH, Huguet N. Characteristics of adult male and female firearm suicide decedents: findings from the National Violent Death Reporting System. Inj Prev. 2009;15:322–7. doi: 10.1136/ip.2008.021162. [Abstract/FREE Full text] [DOI] [PubMed] [Google Scholar]
- 27.Sher L. Alcohol consumption and suicide. QJM. 2006;99:57–61. doi: 10.1093/qjmed/hci146. [Abstract/FREE Full text] [DOI] [PubMed] [Google Scholar]
- 28.Gossop M. Alcohol in suicide attempts and completions. Psychiatr Ann. 2005;35:513–21. [Web of Science] [Google Scholar]
- 29.Kaner EFS, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28:301–23. doi: 10.1111/j.1465-3362.2009.00071.x. [Medline][Web of Science] [DOI] [PubMed] [Google Scholar]
- 30.United States Department of Commerce,Bureau of the Census . American Community Survey (ACS): Public Use Microdata Sample (PUMS), 2003–7 [Computer file] Inter-university Consortium for Political and Social Research [distributor]; Ann Arbor, MI: 2008. ICPSR22101–v1. [Google Scholar]
- 31.National Research Council . Strengthening Forensic Science in the United States: A Path Forward. The National Academies Press; Washington, DC: 2009. [Google Scholar]