Abstract
Temporomandibular joint (TMJ) diseases and disorders refer to a complex and poorly understood set of conditions, manifested by pain in the area of the jaw and associated muscles and limitations in the ability to make the normal movements of speech, facial expression, eating, chewing, and swallowing. The conventional soft occlusal splint therapy is a much safer and effective mode of a conservative line of therapy in comparison to the surgical therapy for temporomandibular joint disorders (TMD). The purpose of this article is to review the Aqualizer™, an hydrostatic oral splint, as accurate, effective treatment and differential diagnostic tool in TMD that allow treating the patient's pain quickly and accurately saving valuable treatment time. The review article has been prepared doing a literature review from the world-wide web and pubmed/medline.
Keywords: Muscles, occlusal splints, temporomandibular joint disorders, temporomandibular joints
INTRODUCTION
The temporomandibular joint (TMJ) is a compound articulation formed from the articular surfaces of the temporal bone and the mandibular condyle. Both surfaces are covered by dense articular fibrocartilage. Each condyle articulates with a large surface area of temporal bone consisting of the articular fossa, articular eminence and preglenoid plane. The TMJ functions uniquely in that the condyle both rotates within the fossa and translates anteriorly along the articular eminence. Because of the condyle's ability to translate, the mandible can have a much higher maximal incisal opening than would be possible with rotation alone. The joint is thus referred to as “ginglymodiarthrodial.” A combination of the terms ginglymoid (rotation) and arthroidial (translation).[1]
TEMPOROMANDIBULAR JOINT DISORDERS (TMDs) AND DENTISTRY
TMD and their relevance to dentistry, has been a highly debated topic in recent years. The TMJ syndrome was first described by Costen in 1934. The American Dental Association President's Conference on Temporomandibular Disorders (American Dental Association, 1983) (Laskin, et al., 1983) defined TMD as – a group of orofacial disorders characterized by pain in the pre-auricular area, TMJ, or muscles of mastication, limitations and deviations in mandibular range of motion, TMJ sounds during jaw function.[2]
TMD refers to a cluster of conditions characterized by pain in the TMJ or its surrounding tissues, functional limitations of the mandible, or clicking in the TMJ during motion.[3,4] Some of the synonyms for conditions causing pain and dysfunction in the TMJ include: Temporomandibular dysfunction syndrome, pain dysfunction syndrome, facial arthromyalgia, TMJ dysfunction syndrome, myofacial pain dysfunction syndrome, craniomandibular dysfunction and myofacial pain dysfunction.[2] TMD is a prevalent disorder most commonly observed in individuals between the ages of 20 years to 40 years. Approximately 33% of the population has at least one TMD symptom and 3.6-7% of the population has TMD with sufficient severity to cause them to seek treatment.[5] The etiology of TMJ disorders remains unclear, but it is likely multifactorial. Capsule inflammation or damage and muscle pain or spasm may be caused by abnormal occlusion, parafunctional habits (e.g., bruxism [teeth grinding], teeth clenching, lip biting), stress, anxiety, or abnormalities of the intra-articular disk. Abnormal dental occlusion appears to be equally common in persons with and without TMJ symptoms.[3,6] Parafunctional habits have been thought to cause TMJ microtrauma or masticatory muscle hyperactivity.[7] Treatment of TMJ disorders starts with conservative therapies which are simple and do not invade the tissues of face, jaw and joints. Since most TMJ disorders are temporary and do not get worse, simple conservative treatment is all that is usually needed to relieve discomfort.[8]
Dental occlusal splinting and permanent occlusal adjustment have been the mainstays of TMJ disorder treatment. Occlusal splint therapy may be defined as “the art and science of establishing neuromuscular harmony in the masticatory system by creating a mechanical disadvantage for parafunctional forces with removable appliances.” Occlusal splint is a diagnostic, relaxing, repositioning, and reversible device. According to the glossary of prosthodontic terms [8th ed.], “occlusal splint is defined as any removable artificial occlusal surface used for diagnosis or therapy affecting the relationship of the mandible to the maxilla. It may be used for occlusal stabilization, for treatment of temporomandibular disorders, or to prevent wear of the dentition.” A common goal of occlusal splint treatment is to protect the TMJ discs from dysfunctional forces that may lead to perforations or permanent displacements. Other goals of treatment are to improve jaw-muscle function and to relieve associated pain by creating a stable balanced occlusion.[9] Two main types of splinting are available: Occluding and non-occluding. Occluding splints, also called stabilization splints, are specially fabricated to improve the alignment of the upper and lower teeth. Non-occluding splints, also called simple splints, primarily open the jaw, release muscle tension, and prevent teeth clenching. Non-occluding splints are typically made of a soft-vinyl and are easier and cheaper to fabricate.[10,11]
The Aqualizer™, a hydrostatic oral splint, is new application that automatically eliminates the distorting influence of the occlusion on the functional position of the jaw, harmonizing muscles, bite, and body. Simple insertion of the Aqualizer™ bite splint creates a muscle-dominant functionally generated occlusion instantly. This occurs because the Aqualizer™ facilitates muscle-dominated mandibular repositioning while it equalizes, axializes, balances, distributes, and makes simultaneous all occlusal forces.
ORAL APPLIANCE DESIGNS AND RELATED CONCEPTS
Flat plane stabilization appliance
The flat plane stabilization appliance (also known as the Michigan splint, muscle relaxation appliance, or gnathologic splint) is generally fabricated for the maxillary arch. Ideally, when a stabilization type of appliance is placed intraorally, there is minimal change to the maxillomandibular relationship other than that produced by the thickness of the material. This is the most commonly used type of intraoral appliance, and when properly fabricated it has the least potential for adverse effects to the oral structures.[12]
Traditional anterior bite plane
In general, they are designed as a palatal-coverage horseshoe shape with an occlusal platform covering six or eight maxillary anterior teeth (e.g., Hawley, Sved, Shore). They prevent clenching, because posterior teeth are not engaged in closing or in parafunctional activities.
Mini anterior appliances
The concept of making an oral appliance that engaged only a small number of maxillary anterior teeth (usually two-four incisors) was first introduced in the mid 1900's as the lucia jig. There have been several variations that have appeared on the market. They include the nociceptive trigeminal inhibition tension suppression system, the best bite, and the anterior midline point stop devices
Anterior repositioning appliance
The anterior repositioning appliance (also known as an orthopedic repositioning appliance) purposefully alters the maxillomandibular relationship so that the mandible assumes a more anterior position. Originally, this type of appliance was supposed to be used to treat patients with internal derangements (usually anterior disk displacements with reduction).[13] Currently it is recommended that repositioning appliances should be used primarily as a temporary therapeutic measure to allow for symptomatic control of painful internal derangements, but not to “permanently” recapture the TMJ disk. This type of appliance should be used with discretion, and only for short periods of time.
Neuromuscular appliances
Advocates of so-called neuromuscular dentistry have claimed that the use of jaw muscle stimulators and jaw-tracking machines enables them to produce an oral appliance at the ideal vertical and horizontal position of the mandible relative to the cranium.[14] After using these appliances to treat a TMD patient, proponents of this methodology usually recommend dental reconstruction at the new jaw relationship.
Posterior bite plane appliances
Posterior bite plane appliances (also known as mandibular orthopedic repositioning appliances) are customarily made to be worn on the mandibular arch. The purpose of this appliance is to produce changes to the vertical dimension and alter the horizontal maxillomandibular relationship. It also has been claimed that this type of appliance has the ability to increase overall physical strength and enhance athletic performance.[15] The major concern regarding this appliance design is that occlusion only occurs on posterior teeth, thereby allowing for over-eruption of the unopposed anterior teeth and/or intrusion of the opposing posterior teeth, resulting in an iatrogenically created posterior open bite.
Pivot appliances
The pivoting appliance is constructed with hard acrylic resin that covers either the maxillary or mandibular arch and incorporates a single posterior occlusal contact in each quadrant. This contact is placed as far posteriorly as possible. The purpose of this design is to reduce intra-articular pressure by condylar distraction as the mandible “fulcrums” around the pivot, resulting in an “unloading” of the articular surfaces of the joint. This appliance was recommended for patients with internal derangements and/or osteoarthritis. Because of the design and force vectors created by this appliance, a potential adverse effect with its use may be occlusal changes manifesting as a posterior open bite where the pivot was placed.
Hydrostatic appliance
This unique appliance was designed by Lerman[16] over 30 years ago. In its original form, it consisted of bilateral water-filled plastic chambers attached to an acrylic palatal appliance, and the patient's posterior teeth would occlude with these chambers. Later this was modified to become a device that could be retained under the upper lip, while the fluid chambers could be positioned between maxillary and mandibular posterior teeth.
WHY THE AQUALIZER™?
Use of Aqualizer™ is indicated in TMJ pain, headache, neck and shoulder pain and stiffness, orthodontic-triggered muscle pain during treatment, pre-surgical differential diagnoses, post-surgical pain and inflammation.[10] Aqualizer™ has flexible fluid layer that equalizes all bite forces by preventing tooth to tooth contact [Figure 1]. The Aqualizer™ has unique water system that immediately optimizes biomechanics, supports the jaw in a comfortable position, removes the teeth from dominance, placing bite and body in harmony, straightens the bite to maximize other structures, enables systemic function and balance, allows the body to naturally balance itself, finds perfect occlusal balance after starting the treatment immediately [Figure 2].[17]
Figure 1.

Self-adjusting oral splint in occlusion
Figure 2.

Oral splint with fluid (water-filling) in occlusion
AQUALIZER™ SIZE SELECTION
Aqualizers are available in three different vertical dimensions: Low, medium, and high [Figure 3]. The amount of fluid in the Aqualizer™ controls the vertical dimension (thickness). Medium volume aqualizers are used in most of the cases. Low volume aqualizers are indicated in the patients with inadequate freeway space or those sensitive to anything in their mouths. High volume aqualizers are used when a patient has excessive freeway space or needs a greater vertical dimension to fill the space between the upper and lower occlusal surfaces.[17]
Figure 3.
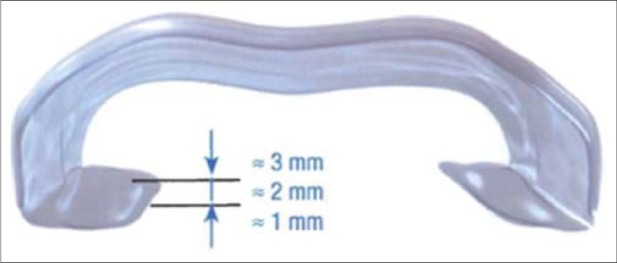
Oral splint offers three fluid volumes - low, medium, high
AQUALIZER™ MODEL SELECTION
Aqualizer™ is available in two basic models that are ultra and Mini. The ultra is a new improved version designed for increased gum comfort and improved retention. It is used for average size mouths. The Mini is the new improved ultra shape with smaller pads and arch size. It is used for kids and small adult mouths.[17]
PROCEDURE
Instruct patient not to take medication for facial jaw pain the day of the appointment. Rule out organic pathology and confirm adequate posterior occlusal support. Remove Aqualizer™ from package and insert in to the mouth. No preparation of the bite splint is necessary. Instruct the patient to keep the fluid pads between the posterior teeth [Figure 4]. The patient should relax and rest their teeth against the fluid pads while swallowing. It is not desirable to clench. Ask the patient to be aware of any change in sensation anywhere in the head, neck, shoulders, and upper back. Monitor the patient's symptoms in every 5-10 min for 30-40 min. Pain relief confirms the diagnosis. Relief of pain usually occurs within 5-10 min after insertion of the Aqualizer™, particularly in the episodic sufferer. Instruct the patient to wear the Aqualizer™ continuously for the next 48 h, except when eating or brushing teeth. At the end of this period, re-examine the patient. If the patient's bruxism improves after wearing the bite splint, occlusal treatment is indicated. If the patient's symptoms do not improve significantly, they are most likely not occlusal in origin and occlusal treatment alone is unlikely to be successful. Patients should not exceed 8 h of Aqualizer™ wear per 24-h period.[17]
Figure 4.
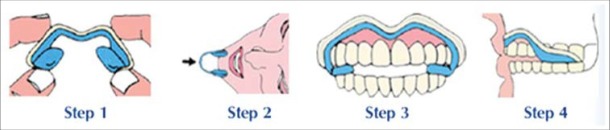
Procedure for applying the oral splint
DISCUSSION
Temporomandibular disorders is a collective term embracing all the problems relating to the TMJ and related musculoskeletal structures.[18] Many therapies have been advocated for treating TMD. A therapy that is commonly provided is an occlusal orthotic, also called a dental or occlusal appliance or a splint.[5] Occlusal splint/occlusal device/orthotics: “Any removable artificial occlusal surface used for diagnosis or therapy affecting the relationship of the mandible to the maxillae. It may be used for occlusal stabilization, for treatment of TMJ disorders, or to prevent wear of dentition.”[19] The appliance can be made to cover the occlusal surfaces of maxillary or mandibular teeth and can be fabricated from many different materials, giving it a hard, soft, or intermediate feel. Occlusal orthotics is beneficial for masticatory muscle pain, TMJ pain, TMJ noises, restricted jaw mobility, and TMJ dislocation.[5]
Splint therapy is considered an adjunct to pharmacologic therapy and most appropriate when nocturnal parafunctional activities can be identified. Typically, a flat-plane maxillary occlusal splint designed for bilateral contact of all teeth is fabricated. Such splints are thought to unload the joint by disarticulating the dentition and increasing the vertical dimension of occlusion. By unloading the joint, there will be a reduction in both synovitis and masticatory muscle activity. Therefore, the result is a reduction in symptoms. These appliances may also change condylar position and the existing occlusal relationship, thereby reducing abnormal muscle activity and spasm.[1] Most occlusal splints have one primary function that is to alter an occlusion so they do not interfere with complete seating of the condyles in centric relation.[19] Following are few concepts, which explain how occlusal splints can help:
Preventing the patient to close in maximal intercuspal position: By occlusal splint, the patient is obliged to place his mandible in a new posture, thus resulting in a new muscular and articular balance. The patient, disturbed in his habits will not clench his teeth any more, like before and protect his TMJ and teeth.[20]
Distribution of forces: The forces generated during bruxism can be as much as 6 times the maximal force generated by normal chewing.[21] The splints distribute these forces across the masticatory system. These appliances can decrease the frequency of bruxing episodes but not the intensity.[22]
Normalizing periodontal ligament proprioception: Proprioceptive fibers contained in the periodontal ligament of each tooth send message to central nervous system, triggering muscle patterns that protect them from overload. An occlusal splint functions to dissipate the forces placed on individual teeth by utilizing a larger surface area covering all teeth in the arch. Thus, a splint balances the load and allows for muscle symmetry.
Relaxing the muscles: Tooth interferences to the CR arc of closure hyper-activate the lateral pterygoid muscles and posterior tooth interferences during excursive mandibular movements cause hyperactivity of the closing muscles. A muscle that is fatigued through ongoing muscle hyper-activity can present with pain. If the hyperactivity is stopped, the pain caused by it will usually disappear. A splint with equal intensity contacts on all of the teeth, with immediate disclusion of all posterior teeth by the anterior guidance and condylar guidance in all movements, will relax the elevator and positioning muscles.[23]
Allowing the condyles to seat in centric relation: For the condyles to seat completely under the disc in anterosuperior position, the superior belly of lateral pterygoid should obtain its full extension. When the lateral pterygoid is triggered to hyperactivity through occlusal stimuli, the disc is pulled anteromedially toward the origin of muscle, resulting in displacement. Overloading of condyle/disc assembly when not in normal physiologic position contributes towards TMJ disorders. A properly balanced splint results in an occlusion associated with relaxed positioning and elevator muscles, allowing the articulator disc to obtain its antero-superior position over the condylar head.
Increase in the vertical dimension of occlusion: Occlusal splints can be adjusted with a vertical height that exceeds the physiologic interocclusal distance. Temporary use of occlusal splints with a vertical height exceeding the physiologic rest position does not cause increase in tonus or hyperactivity of jaw muscles. Studies have shown that elongation of elevator muscles to or near the vertical dimension of least electromyographic activity by means of occlusal splint is effective in producing neuromuscular relaxation.[24,25]
Cognitive awareness theory: This theory can be applied to any or all of the appliances utilized. The cognitive awareness theory is based on the concept that having an interocclusal appliance in the mouth constantly reminds the patient to alter his/her normal behavior so that the opportunity for harmful or abnormal muscle activity with every closure of the teeth is decreased. The increased cognitive awareness of the patient regarding the positioning and use of the jaw, the change in oral tactile stimuli, and the decrease in oral volume can all influence the patient to learn what position or activities are harmful.[26]
Okeson classified the occlusal splints in stabilization appliance and anterior repositioning appliances with other types of occlusal splints which includes, anterior bite plane, posterior bite plane, pivoting appliance, soft/resilient appliance. Dawson classified the occlusal splints into permissive splints/muscle deprogrammer and directive splints/non-permissive splints.[9]
Aqualizer™ works by allowing the muscles to automatically reposition the jaw. For TMJ pain relief, restoring this balance is essential. The Aqualizer™ self-adjusting oral splint allows the body to unravel bite distortions and establish optimal systemic function and balance. While most dental mouth guards simply disable the bite long-term and guess at optimal occlusion, the Aqualizer™ takes the guesswork out of treatment by allowing the body to naturally find TMJ pain relief and functional balance. The Aqualizer™ is a new application of a basic physical law of nature called Pascal's law, which states that that an enclosed fluid will apply equalized fluid pressure regardless of where pressure is applied to the fluid. In other words, biting down on the Aqualizer™ causes the fluid to distribute bite forces evenly across the bite, reducing TMJ pressure and pain and ensuring relief.[17]
The Aqualizer™'s fluid system may also relieves chronic back, neck, and shoulder pain and provides migraine headache relief by taking the pressure off painful joints and muscles by cushioning and floating the jaw. The fluid-filled Aqualizer™ provides bilateral balance and perfectly distributed occlusal forces. Muscle pain can be dramatically relieved and healing can begin immediately. The Aqualizer™'s smooth, flexible surface permits the teeth to easily slide across it. The flexible fluid pads, positioned between the upper and lower occlusal surfaces, eliminate all tooth-to-tooth contact. Proprioceptive guidance is neutralized as the dominant factor in functional mandibular placement. The muscles respond instantly by moving the mandible into its most comfortable, least accommodated position. Generally within the first few minutes, this occlusal-muscle harmony eliminates occlusally triggered facial jaw pain and muscle spasm. The Aqualizer™'s fluid system responds dynamically, continuously re-equilibrating and balancing bilaterally as the mandible shifts to the position most comfortable for the muscles to function.[17] Macedo and Mello evaluated the efficacy of the hydrostatic splint Aqualizer™, microcurrent electrical nerve stimulation-MENS and transcutaneous electrical neural stimulation-TENS therapies in patients with TMD in acute situations and concluded that the MENS and the hydrostatic splint were more effective than TENS.[27] The Aqualizer™ is not indicated for patients with severe bruxism and those without normal gag reflex, If Aqualizers™ are destroyed within hours or one or two nights, the patient is a parafunctional bruxer/clencher. The Aqualizer™ is not tough enough for them. During wear, the Aqualizer™ will gradually lose its fluid. When there is not enough fluid to create the floating action, symptoms may start to return. One should switch to a new Aqualizer™ when this occurs. Aqualizer™ costs US $ 24.86 approximately Rs. 1200/- and is commercially available through Dental Depot.[17]
CONCLUSION
TMD should be treated like any other musculoskeletal complaint. If TMJ/TMD is left untreated, symptoms can worsen and extend far beyond the jaw and mouth area. Conservative therapy is best as a first-line approach for treating the patient. Soft oral splints can be used as effective means of treatment for such patients. This can be easily made and gives good comfort to the patient. The Aqualizer™ technology is a major breakthrough in pain therapy. It is a muscle relaxing, floating action temporary splint which does not cause permanent or irreversible changes in the structure or position of the jaw or teeth. It has better patient compliance, fewer side-effects, and is more cost-effective than surgical treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Herb K, Cho S, Stiles MA. Temporomandibular joint pain and dysfunction. Curr Pain Headache Rep. 2006;10:408–14. doi: 10.1007/s11916-006-0070-7. [DOI] [PubMed] [Google Scholar]
- 2.Al-Riyami S. PhD Thesis. London: UCL Eastman Dental Institute for Oral Health Sciences; 2010. [[Last cited 2012 Jun 20]]. Temporomandibular joint disorders in patients with skeletal discrepancies. Available from: http://discovery.ucl.ac.uk/575469/1/575469.pdf . [Google Scholar]
- 3.Dworkin SF, Huggins KH, LeResche L, Von Korff M, Howard J, Truelove E, et al. Epidemiology of signs and symptoms in temporomandibular disorders: Clinical signs in cases and controls. J Am Dent Assoc. 1990;120:273–81. doi: 10.14219/jada.archive.1990.0043. [DOI] [PubMed] [Google Scholar]
- 4.Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. J Oral Rehabil. 2004;31:287–92. doi: 10.1046/j.1365-2842.2003.01257.x. [DOI] [PubMed] [Google Scholar]
- 5.Wright EF, North SL. Management and treatment of temporomandibular disorders: A clinical perspective. J Man Manip Ther. 2009;17:247–54. doi: 10.1179/106698109791352184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McNamara JA, Jr, Seligman DA, Okeson JP. Occlusion, Orthodontic treatment, and temporomandibular disorders: A review. J Orofac Pain. 1995;9:73–90. [PubMed] [Google Scholar]
- 7.Okeson JP. Orofacial Pain: Guidelines for assessment, diagnosis, and management. Chicago, Ill: Quintessence Pub; 1996. for the American Academy of Orofacial Pain Diffrential diagnosis and management considerations of temporomandibular disorders; pp. 120–2. [Google Scholar]
- 8.The patient education institute Inc; [[Last reviewed: 5/1/2008:1-5]]. X-Plain Temporomandibular Joint Disorders Reference Summary. www.X-Plain.com. Available from: http://www.nlm.nih.gov/medlineplus/tutorials/temporomandibularjointdisorders/ol209104 . [Google Scholar]
- 9.Yadav S, Karani JT. The essentials of occlusal splint therapy. Int J Prosthetic Dent. 2011;2:12–21. [Google Scholar]
- 10.Shankland WE., 2nd Temporomandibular disorders: Standard treatment options. Gen Dent. 2004;52:349–55. [PubMed] [Google Scholar]
- 11.Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: A randomized controlled trial. J Am Dent Assoc. 2006;137:1099–107. doi: 10.14219/jada.archive.2006.0348. [DOI] [PubMed] [Google Scholar]
- 12.Manns A, Chan C, Miralles R. Influence of group function and canine guidance on electromyographic activity of elevator muscles. J Prosthet Dent. 1987;57:494–501. doi: 10.1016/0022-3913(87)90024-2. [DOI] [PubMed] [Google Scholar]
- 13.Farrar WB. Differentiation of temporomandibular joint dysfunction to simplify treatment. J Prosthet Dent. 1972;28:629–36. doi: 10.1016/0022-3913(72)90113-8. [DOI] [PubMed] [Google Scholar]
- 14.Cooper BC. The role of bioelectronic instrumentation in the documentation and management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:91–100. doi: 10.1016/s1079-2104(97)90098-6. [DOI] [PubMed] [Google Scholar]
- 15.Bodenham RS. A bite guard for athletic training. A case report. Br Dent J. 1970;129:85–6. doi: 10.1038/sj.bdj.4802527. [DOI] [PubMed] [Google Scholar]
- 16.Lerman MD. The hydrostatic appliance: A new approach to treatment of the TMJ pain-dysfunction syndrome. J Am Dent Assoc. 1974;89:1343–50. doi: 10.14219/jada.archive.1974.0616. [DOI] [PubMed] [Google Scholar]
- 17.The revolutionary Aqualizer Self-Adjusting oral splint. New harmony between bite and body: TMJ pain relief and treatment with Aqualizer® dental splints. [Last accessed 2013 Feb 17]. Available from: http://www.aqualizer.com/html/aqualizer.html .
- 18.Guidelines for diagnosis and management of disorders involving the temporomandibular joint and related musculoskeletal structures approved by American society of temporomandibular joint surgeons. [[Last accessed 2013 Feb 17]]. Available from: http://astmjs.org/final%20 guidelines-04-27-2005.pdf . [PubMed]
- 19.Deshpande RG, Mhatre S. TMJ disorders and occlusal splint Therapy: A Review. Int J Dent Clinics. 2010;2:22–9. [Google Scholar]
- 20.RèJ P, Perez C, Darmouni L, Carlier JF, Orthlieb J-D. The occlusal splint therapy. J Stomat Occ Med. 2009;2:82–6. [Google Scholar]
- 21.Gibbs CH, Mahan PE, Mauderli A, Lundeen HC, Walsh EK. Limits of human bite strength. J Prosthet Dent. 1986;56:226–9. doi: 10.1016/0022-3913(86)90480-4. [DOI] [PubMed] [Google Scholar]
- 22.Holmgren K, Sheikholeslam A, Riise C. Effect of a full-arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthet Dent. 1993;69:293–7. doi: 10.1016/0022-3913(93)90109-2. [DOI] [PubMed] [Google Scholar]
- 23.Williamson EH, Lundquist DO. Anterior guidance: Its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983;49:816–23. doi: 10.1016/0022-3913(83)90356-6. [DOI] [PubMed] [Google Scholar]
- 24.Manns A, Miralles R, Santander H, Valdivia J. Influence of the vertical dimension in the treatment of myofascial pain-dysfunction syndrome. J Prosthet Dent. 1983;50:700–9. doi: 10.1016/0022-3913(83)90213-5. [DOI] [PubMed] [Google Scholar]
- 25.Manns A, Miralles R, Cumsille F. Influence of vertical dimension on masseter muscle electromyographic activity in patients with mandibular dysfunction. J Prosthet Dent. 1985;53:243–7. doi: 10.1016/0022-3913(85)90120-9. [DOI] [PubMed] [Google Scholar]
- 26.Kumar H, Chandra S, Aggarwal R, Trikha R. Oral appliances in the management of temporomandibular disorders. [[Last accessed 2013 Feb 17]]. Available from: http://guident.net/prosthodontics/oral-appliances -in-the-management-of-temporomandibular-disorders.html .
- 27.Macedo JF, Mello EB. Therapeutic of urgency in temporomandibular disorders. Rev ATMservice. 2002;2:22–8. [Google Scholar]


