Abstract
Background:
The main stay of primary and secondary prevention of periodontal diseases has been the control of supra gingival plaque. Acceptable plaque control by mechanical means is difficult to achieve by most individuals, so mouth rinses represent one form of attack on oral microbes and the malodor. Chlorhexidine (CHX) is a broad-spectrum antimicrobial agent known to cause damage to the cell membrane of microorganisms and at higher concentrations causes precipitation and coagulation of the proteins in the cytoplasm of the exposed microbes. The aim of this study is to evaluate and compare the efficacy of 0.12% and 0.2% concentration of CHX gluconate clinically as well as microbiologically.
Materials and Methods:
The single blind placebo controlled randomized study design comprising of 75 males with an age between 25 years and 50 years were selected from out-patient Department of Periodontics. The subjects were randomly divided into five groups. After baseline clinical and microbiological examination, the groups were subjected to mechanical plaque control with or without mouthwashes containing various concentrations of CHX and placebo. After 90 days the data pertaining to clinical and microbiological parameters were compared to the baseline data so as to compare the efficacy of different concentrations of mouthwashes.
Results:
The results achieved with the use of 0.2% and 0.12% concentrations of CHX were comparable; taking into consideration of various clinical and microbiological parameters.
Conclusion:
The study recommends the use of low concentration of (0.12%) CHX for better patient compliance with the optimum clinical results
Keywords: Chemical plaque control, chlorhexidine, mouthwashes
INTRODUCTION
Epidemiological studies like experimental gingivitis in human beings[1] and clinical research studies have concluded that plaque is the etiological factor in gingival inflammation and has been found to be associated with the initiation and progression of periodontal diseases. On the basis that plaque-induced gingivitis precedes periodontitis[2] the main stay of primary and secondary prevention of periodontal diseases is the control of supra gingival plaque.
As an acceptable plaque control by mechanical means is difficult to achieve by most individuals, mouth rinses represent one form of attack on oral microbes and the malodor. They have come a long way from preventing oral malodor to reducing the oral microbial load. The first reference to mouth rinsing around 2700 B.C. is credited to Chinese medicine literature for treatment of diseases of the gums by rinsing with urine of a child. We have come a long way since then to the use of chlorhexidine (CHX) now for over three decades. CHX is a broad-spectrum antimicrobial agent with effect on gram positive and gram-negative bacteria as well as on fungi and some viruses.[3] CHX in vitro studies have shown to cause damage to the cell membrane and low molecular weight molecules escape from the microorganisms while CHX at higher concentrations is known to cause precipitation and coagulation of the proteins in the cytoplasm of the exposed microbes.
Different concentrations of CHX have been used by various workers with varying degrees of success. Initially, CHX gluconate 0.2% was introduced as an antiplaque mouth rinse followed by CHX gluconate 0.12% mouth rinse since 1986. Though, the first clinically effective mouth rinse i.e., the 0.2% CHX gluconate is still the most commonly used, but studies have confirmed that 0.12% CHX gluconate has an equal therapeutic benefit at a lower concentration leading to decreased salivary bacterial load by 97%.[4]
The rationale for lowering the concentration of CHX was to reduce the side-effects such as tooth staining, mucosal erosion, and taste disturbance while maintaining the comparable therapeutic effect.
Though various studies[5] have been conducted in the past to assess clinically the effectiveness of commercially available CHX gluconate concentrations i.e., 0.2% and 0.12% on control of plaque and gingivitis but much of the literature eludes their effect on Porphyromonas sps earlier referred to as anaerobic black pigmented bacteria's (BPBs), which form an integral constituent of subgingival bacterial plaque. The aim of this study is to evaluate and compare the efficacy of 0.12% and 0.2% concentration of CHX gluconate clinically as well as microbiologically.
MATERIALS AND METHODS
Seventy five subjects were selected amongst the patients attending the Out-patient Department of Armed Forces Medical College, Pune, India. The subjects were ascertained to be in good general health without any systemic disease. None of the patients selected had received antibiotics, steroids or oral prophylaxis for at least 6 months prior to the start of the study. No female patients were included. Seventy five males with an age between 25 years and 50 years having a set of twenty two or more teeth with the probing depth (PD) < 4 mm; clinical attachment loss < 3 mm at minimum ten teeth with the presence of bleeding on probing and willingness to comply were included. All the subjects had a high standard of oral hygiene and gingival health. They were free from any unusual oral lesions, were not allergic to CHX, and were without any prosthesis.
The design of the study was a single blind placebo controlled randomized study. After selection of the subjects, the informed consent was taken from all the patients.
Clinical examination
Clinical measurements and microbiological samples were collected from the selected sites and recorded in a predesigned performa. The sampling sites selected were in the mandibular molar region with the visible clinical signs of inflammation and PD. At baseline and 90 days, the examination of clinical parameters included, the Gingival index score (GI), Plaque index score (PI) and PD.
Rather than averaging several measurements around each individual tooth, GI and PI were recorded by modified technique. The gingival inflammation and plaque accumulation were recorded at the individual sample site only similarly one reading was taken for PD at sampling location.
Microbiological examination
The plaque samples were collected from the sample sites, which had overt signs of gingivitis with pocket depth of 4 mm at baseline and after 90 days.
After removal of supra gingival and subgingival plaque, samples were obtained using a sterile Gracey curette. Immediately upon obtaining the sample the tip of the curette was transferred to 0.2 ml of ¼th Ringer's solution. The contents of the curette were dislodged into the vial containing solution by agitating the tip of the curette. The test tube was sealed with cotton plug and labeled with specific number as per the sample's subjects and sent to the Department of Microbiology for culture.
The plaque samples collected were vortexed in a cyclomixer after which 10 μl of mixed specimen was inoculated by the micropipette on the following culture medias; (a) blood agar, (b) chocolate agar, (c) kanamycin, vancomycin laked blood, (d) stryptic soy agar, (e) neomycin blood agar with Hemin, and Vitamin K.
After culturing the samples into selective media, the culture plates were incubated in the anaerobic cabinet [Figure 1], with 90% N2, 10% CO2 at 37°C for 72 h. After 72 h, the culture plates were removed and examined for the presence of colonies. Since, longer time is taken by the anerobics for growth the plates were inoculated and reexamined after 48 h. The best growth of colonies in any of the media's was taken into account. The colonies were counted as colony forming units per milliliters (cfus/ml).
Figure 1.
Anaerobic chamber
Grouping
After the initial recording of clinical parameters and collection of microbial samples, the subjects were randomly divided into Groups A, B, C, D, and E; consisting of 15 subjects in each group as under.
Group A: Supra gingival scaling with administration of 0.2% CHX (10 ml)
Group B: Supra gingival scaling with administration of 0.12% CHX (15 ml)
Group C: Supra gingival scaling with administration of mouth rinse identical in composition but without CHX gluconate
Group D: Supra gingival and subgingival scaling with administration of 0.12% CHX (15ml)
Group E: Only supra gingival and subgingival scaling with no administration of any mouthwashes.
Complete plaque removal was assessed using the disclosing solution in all the subjects. The subjects were assessed every week to ascertain that they were following instructions. After 90 days, the same clinical examinations were carried out and microbiological samples were taken for culture in the same way as that during the baseline examination. The 3 months and the baseline difference of clinical and microbiological parameters were analyzed, compared in between the groups.
RESULTS
All the clinical and microbiological parameters at the baseline were subjected to the statistical analysis as showed by ‘f’ value (ANOVA) of 0.10, 0.06, 0.0 and 0.12 thereby showing a non-significant result. Therefore, the groups were randomly selected with no baseline distinctions.
Clinical parameters
In Group A and B, a statistically significant reduction of GI, PI and PD have been assessed, when compared in between the values of baseline to that of 90 days [Table 1]. Group C hardly showed any reduction of GI, PI, and PD (1.57 to 1.54, 1.49 to 1.44 and 4.00 to 3.76 respectively, which are statistically non-significant). The GI value for Group D showed statistically significant reduction from 1.56 to 0.27, PI value with 86.57% reduction and PD from 4 to 2.06, showing the effectiveness of subgingival scaling with root planing. Study subject Group D where highly significant reduction of all clinical parameters (GI, PI and PD).
Table 1.
Comparison of clinical parameters of group A, B, C, D and E (baseline and 90 days)
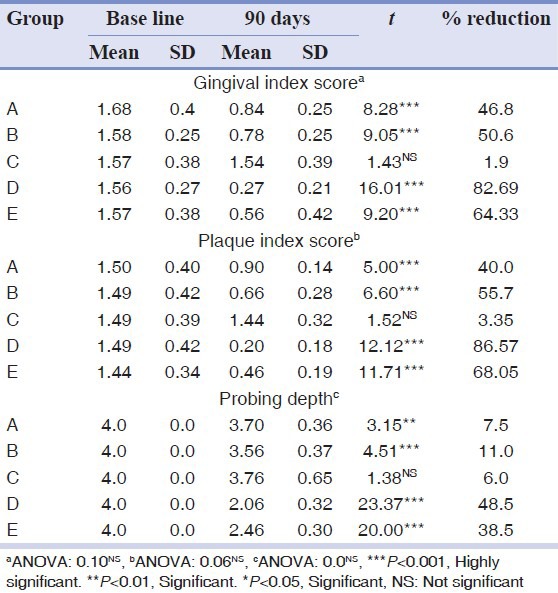
Inter group comparison in between Group A and B study samples showed statistical difference when compared to Group C with a ‘f’ value of 7.65. Group A was compared to Group D and E with ‘f’ value of 4.54 and 2.08 respectively. While comparing the PI, Group A and B didn’t show any statistically significant difference with ‘f’ value of 1.26 whereas comparing it with Group C showed a ‘f’ value of 4.38 which is highly significant. The Group A was compared with Group D and E and the ‘f’ values were 4.25 and 2.49 respectively [Table 2].
Table 2.
Comparison of differences between baseline and 90 days among various groups A, B, C, D and E

Individuals with supra gingival scaling and root planing along with the mouthwash showed a PI value with 86.57% reduction. Subjects under Group E also showed similar trend of reduction of PI from 1.44 (SD-0.34) to 0.46 (SD-0.19) [Table 1].
Intergroup comparison of PD between Groups A and B hardly showed any statistically significant difference. When Group A was compared with Groups D and E respectively, the ‘f’ values were 12.96 and 10.09 [Table 2], thereby showing a marked reduction in the PD.
Microbiological findings
Subgingival plaque samples obtained at baseline level showed no marked variation amongst various clinical groups (f = 0.12), while looking for Porphyromonas species with black pigmentation pertaining to the samples of Groups A and B. The samples pertaining to Groups A and B after intervention showed a reduction of 64.35% and 58.7% respectively while the intergroup comparison showed no significant difference between them [Table 3]. Group C did not show any change on microbial population at 90 days interval [Figures 2 and 3]. Drastic reduction in colony forming units of 97% and 68% could be seen in Groups D [Figures 4 and 5], and E respectively. The placebo Group C when compared to all the other groups showed a highly significant difference (P < 0.001) [Table 3]. Group D showed significant difference when compared to Groups A and B.
Table 3.
CFUs/ml of BPBs intergroup comparison
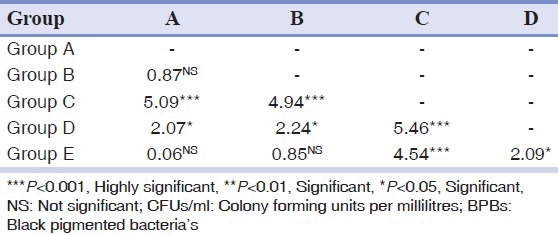
Figure 2.
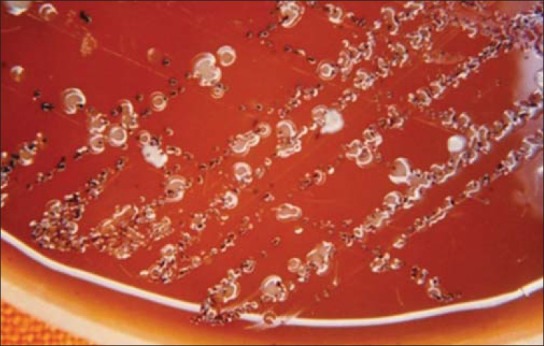
Growth of colonies of BPB's (porphyromas) at baseline (Group C)
Figure 3.
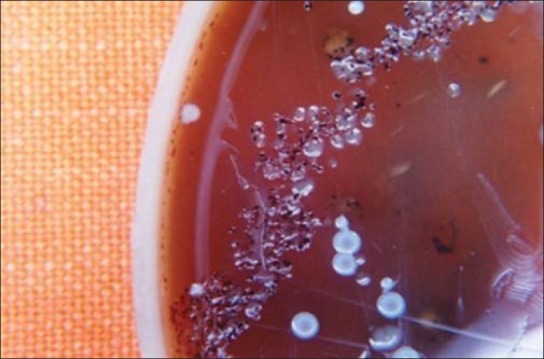
Post-treatment growth of colonies of BPB's (porphyromas) after 90 days (Group C)
Figure 4.
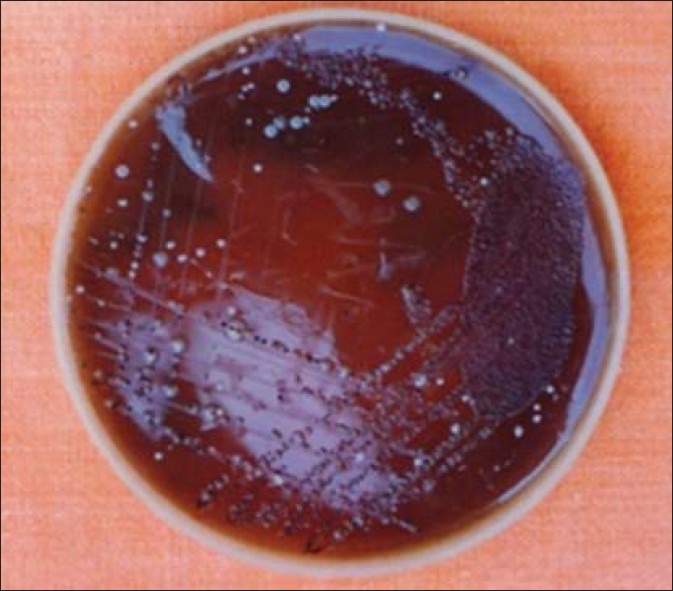
Growth of colonies of BPB's (porphyromas) at baseline (Group D)
Figure 5.
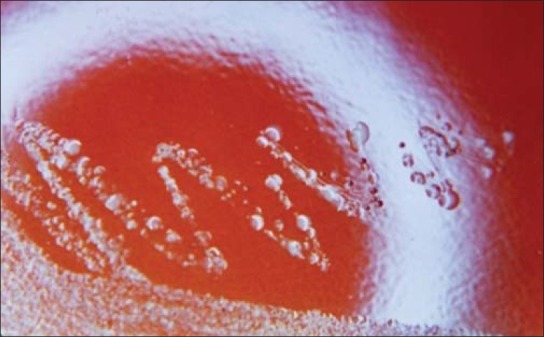
Post-treatment growth of colonies of BPB's (porphyromas) after 90 days (Group D)
DISCUSSION
The clinical parameters at baseline level of all the groups showed no significant differences which clearly point to the random selection of the individuals in various groups. Root surfaces once debrided again repopulate with the pathogenic microbial species in 2-6 months’ time,[6] with an average of 12 weeks interval. However, results obtained at 90 days suggested a steep fall in the microbial population of Porphyromonas sps as well as showed great improvements in the clinical parameters; which may be attributed to the actions of mouthwashes, involved in the study.
Effectiveness of 0.2% on 0.12% CHX in reducing the clinical parameters were proved to be identical in the current study, which is parallel to one of Segreto et al.,[7] while using the lower concentration of CHX is more recommendable and the same has been shown by studies by Jenkins et al.[8] and Greenstein et al.[9]
The local side-effects of CHX are dose dependent,[10,11] and concentration dependent,[12,9] which supports the finding of the present study. Moreover, adsorption of monolayer formed by low concentration CHX is more stable than the multilayered high concentration over the microbial cell wall.[13]
The usefulness of mouth rinses cannot be ruled out, when compared using the various clinical as well as microbiological parameters on Groups A and B. with the placebo Group C where the mouthwash was almost similar in ingredients less the active CHX part was used. However, higher concentration of CHX did not provide any substantial advantage for both the clinical and microbiological parameters in the present study, which is similar to that by Mendieta et al.[14]
The involvement of additional parameter of acceptability of mouthwashes also goes in favor of lower concentration of CHX. Hence, a better compliance can be anticipated while using less concentration of CHX mouthwash.
The most common side-effects associated with the CHX gluconate oral rinse are: (1) An increase in staining of the teeth and other oral surfaces; (2) an increase in calculus formation; and (3) an alteration in taste perception, though this symptom can be reversed by the ceasing its use.
Ten ml of 0.2% CHX mouthwash carries 20 mg of active CHX while comparing the larger quantity of 15 ml of 0.12% CHX. Therefore, following the principles of medicine that the drug would always be optimally effective when its efficacy is balanced against the local side-effects and the user's acceptability.
Looking at the gathered data and information's, Groups D and E undoubtedly showed the best results in comparison to other groups. It can be easily explained being due to proper meticulous local debridement consisting of scaling and root planing reduction at the sites. But in order to keep a check on bacterial recolonisation, additional adjuncts have a tremendous utility in clinical practice, and the use of mouthwash seems to be the simplest and easiest way. Moreover, the lower concentration of CHX showed maximum acceptability amongst the users. Therefore, this study recommends the use of 0.12% CHX gluconate mouthrinse over and above the proper debridement procedure.
The Porphyromonas sps are the established microbial indicators to the prognosis of periodontal disease.[15] Results obtained after local debridement in Group E are still inferior to the similar procedure employed in Group D which can be attributed to the sustained effect of CHX 0.12% over the repopulations of sites by periodontopathogens.
The limitation of this study is the identification of specific types of bacterial response to CHX at different concentrations. Although the culture of bacteria is the gold standard and recent advances in DNA hybridization techniques, Polymerase chain reaction will help in both qualitative and quantitative estimation of bacteria. Secondly, the long-term effect of CHX in checking the response of bacteria has not been studied. Studies of large samples with prolonged duration will definitely help in establishing the adjunctive role of mouthwash in periodontal therapy.
CONCLUSION
The mouth rinses enhance the efficacy of plaque control when used as supplements to mechanical oral hygiene procedures. Thorough debridement consisting of meticulous root planing forms the basis of management in periodontal diseases. Therefore, it can be concluded at this juncture that using an additional adjunct like CHX helps to keep the pathogenic microbial population under check.
The Porphyromonas sps which form the important part of the periodontopathogens causing rapid loss of periodontal structures no doubt can be made to limit their advancement with the use of lower concentration of CHX as an adjunct to meticulous root planing.
It has been seen that the efficacy of 0.2% CHX (10 ml) and 0.12% CHX (15 ml) are similar, though, the side-effects of 0.12% CHX are less due to the lesser concentration of CHX and it has been noted that the patient compliance is better with 0.12% CHX.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 2.Hujoel P, Zina LG, Cunha-Cruz J, Lopez R. Historical perspectives on theories of periodontal disease etiology. Periodontol 2000. 2012;58:153–60. doi: 10.1111/j.1600-0757.2011.00423.x. [DOI] [PubMed] [Google Scholar]
- 3.Lim KS, Kam PC. Chlorhexidine: Pharmacology and clinical applications. Anaesth Intensive Care. 2008;36:502–12. doi: 10.1177/0310057X0803600404. [DOI] [PubMed] [Google Scholar]
- 4.Veksler AE, Kayrouz GA, Newman MG. Reduction of salivary bacteria by pre-procedural rinses with chlorhexidine 0.12% J Periodontol. 1991;62:649–51. doi: 10.1902/jop.1991.62.11.649. [DOI] [PubMed] [Google Scholar]
- 5.Berchier CE, Slot DE, Van der Weijden GA. The efficacy of 0.12% chlorhexidine mouthrinse compared with 0.2% on plaque accumulation and periodontal parameters: A systematic review. J Clin Periodontol. 2010;37:829–39. doi: 10.1111/j.1600-051X.2010.01575.x. [DOI] [PubMed] [Google Scholar]
- 6.Southard SR, Drisko CL, Killoy WJ, Cobb CM, Tira DE. The effect of 2% chlorhexidine digluconate irrigation on clinical parameters and the level of Bacteroides gingivalis in periodontal pockets. J Periodontol. 1989;60:302–9. doi: 10.1902/jop.1989.60.6.302. [DOI] [PubMed] [Google Scholar]
- 7.Segreto VA, Collins EM, Beiswanger BB, La Rosa M, Isaacs RL, Lang NP, et al. A comparison of mouthrinses containing two concentrations of chlorhexidine. J Periodont Res. 1986;21(Suppl):23–32. [Google Scholar]
- 8.Jenkins S, Addy M, Newcombe RG. Dose response of chlorhexidine against plaque and comparison with triclosan. J Clin Periodontol. 1994;21:250–5. doi: 10.1111/j.1600-051x.1994.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 9.Greenstein G, Berman C, Jaffin R. Chlorhexidine. An adjunct to periodontal therapy. J Periodontol. 1986;57:370–7. doi: 10.1902/jop.1986.57.6.370. [DOI] [PubMed] [Google Scholar]
- 10.Cancro LP, Klein K, Picozzi A. Dose response of chlorhexidine gluconate in a model in vivo plaque system. J Dent Res. 1973;52:223–6. [Google Scholar]
- 11.Cancro LP, Paulovic DB, Bolton S, Picozzi A. Dose response of chlorhexidine gluconate in a model in vivo plaque system. J Dent Res. 1974;53:765–6. [Google Scholar]
- 12.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79:119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 13.Emilson CG, Eriksen TH, Heyden G, Magnusson BC. Uptake of chlorhexidine to hydroxylapatite. J Periodont Res. 1973;8:17–21. doi: 10.1111/j.1600-0765.1973.tb02159.x. [DOI] [PubMed] [Google Scholar]
- 14.Mendieta C, Vallcorba N, Binney A, Addy M. Comparison of 2 chlorhexidine mouthwashes on plaque regrowth in vivo and dietary staining in vitro. J Clin Periodontol. 1994;21:296–300. doi: 10.1111/j.1600-051x.1994.tb00321.x. [DOI] [PubMed] [Google Scholar]
- 15.Japoni A, Vasin A, Noushadi S, Kiany F, Japoni S, Alborzi A. Antibacterial susceptibility patterns of Porphyromonas gingivalis isolated from chronic periodontitis patients. Med Oral Patol Oral Cir Bucal. 2011;16:e1031–5. doi: 10.4317/medoral.17174. [DOI] [PubMed] [Google Scholar]


