Abstract
Objective
It is essential to design technologies and systems that promote appropriate interactions between physicians and patients. This study explored how physicians interact with Electronic Health Records (EHRs) to understand the qualities of the interaction between the physician and the EHR that may contribute to positive physician-patient interactions.
Study Design
Video-taped observations of 100 medical consultations were used to evaluate interaction patterns between physicians and EHRs. Quantified observational methods were used to contribute to ecological validity.
Methods
Ten primary care physicians and 100 patients from five clinics participated in the study. Clinical encounters were recorded with video cameras and coded using a validated objective coding methodology in order to examine how physicians interact with electronic health records.
Results
Three distinct styles were identified that characterize physician interactions with the EHR: technology-centered, human-centered, and mixed. Physicians who used a technology-centered style spent more time typing and gazing at the computer during the visit. Physicians who used a mixed style shifted their attention and body language between their patients and the technology throughout the visit. Physicians who used the human-centered style spent the least amount of time typing and focused more on the patient.
Conclusion
A variety of EHR interaction styles may be effective in facilitating patient-centered care. However, potential drawbacks of each style exist and are discussed. Future research on this topic and design strategies for effective health information technology in primary care are also discussed.
Keywords: Health Information Technology, Clinician’s Interactive Style, Primary care, Human Computer Interaction
1. Introduction
Widespread implementation and usage of electronic health records (EHRs) and other health information technologies can improve the quality and efficiency of health care in the United States (Chaudhry et al., 2006; Fang et al., 2011). The American Recovery and Reinvestment Act (ARRA) provided a $19 billion fund to promote the adoption of EHRs with the requirement of “meaningful use” (Rao et al., 2011). The “meaningful use” requirement states that EHRs should be used effectively and to promote quality and efficiency in the health care system (Blumenthal, 2009). Despite this goal, a National Research Council (NRC) report indicates that most current EHR technologies are poorly designed; and more specifically the technology does not compliment care providers’ cognitive capabilities and needs (Stead & Lin, 2009). Furthermore, the NRC report states that current EHRs are not designed based on human-computer interaction and human factors and ergonomics design principles, which contributes to their inefficient use (Stead & Lin, 2009).
Physician-patient communication is a key element in health care delivery. It is also a significant contributor to patient outcomes, such as patient satisfaction, adherence, rapport, and trust (Ong et al., 1995; Roter et al., 2006). A study on physician-patient interaction found that physicians who maintained high levels of eye contact had better patient satisfaction and perception of physician empathy (Montague et al., 2011). In addition, some studies have found that computer use could potentially improve physician-patient communication (Shachak & Reis, 2009) and increase patient satisfaction (Lelievre & Schultz, 2010). On the other hand, computer use may reduce positive communication cues, such as eye contact, and could make patients feel disengaged or feel that their physicians are less attentive (Margalit et al., 2006). Computer use may also increase physicians’ mental workload, making it difficult for them to simultaneously enter data and engage in patient-centered care (Holden, 2011). Despite its importance, the effects of EHR use on physician-patient communication are not covered in the core requirements of meaningful use (Graham-Jones et al., 2012). In addition, teaching interventions in medical schools for EHR-specific communication skills are lacking (Morrow et al., 2009). In practice, physicians develop their EHR-use skills based on experience and observation rather than formal training (Rouf et al., 2007), and medical students have expressed concern about their preparedness and ability to effectively use clinical information systems (Otto et al., 2009) and integrate EHR use into clinical communication (Graham-Jones et al., 2012). Current interaction styles with EHR systems may therefore by a byproduct of physicians’ non-standardized training in integrating health information technology into their communication style. An understanding of physicians’ different interaction styles is needed to inform training programs that will help physicians effectively integrate EHR use with patient communication. The NRC report also demonstrates a need for new guidelines to inform EHR design and implementation (Stead & Lin, 2009). To develop these guidelines, it is essential to evaluate how EHRs are used in context.
A sociotechnical system is comprised of people, technologies, and work-system characteristics. In a patient-provider system, patients and providers have interactions with health information technologies. Patient perceptions of health information technologies are developed through the combination of technology characteristics, care provider characteristics, and how the care provider uses the technology (Figure 1). A key component of patient perception of technology is the interaction between the physician and technology. In the model shown in figure 1, the patient receives cues from the technology (e.g. aesthetics, functioning, etc.), care provider (e.g. rapport, communication) and provider’s use of technology (e.g. ease of use and interaction style). These cues influence the patient’s perceptions of the work system as a whole and of individual system elements (Montague & Asan, 2012). The provider’s use of technology can also affect communicative behaviors. For example, heavy technology use may limit the amount of positive communication cues a provider is able to exhibit.
Figure 1.
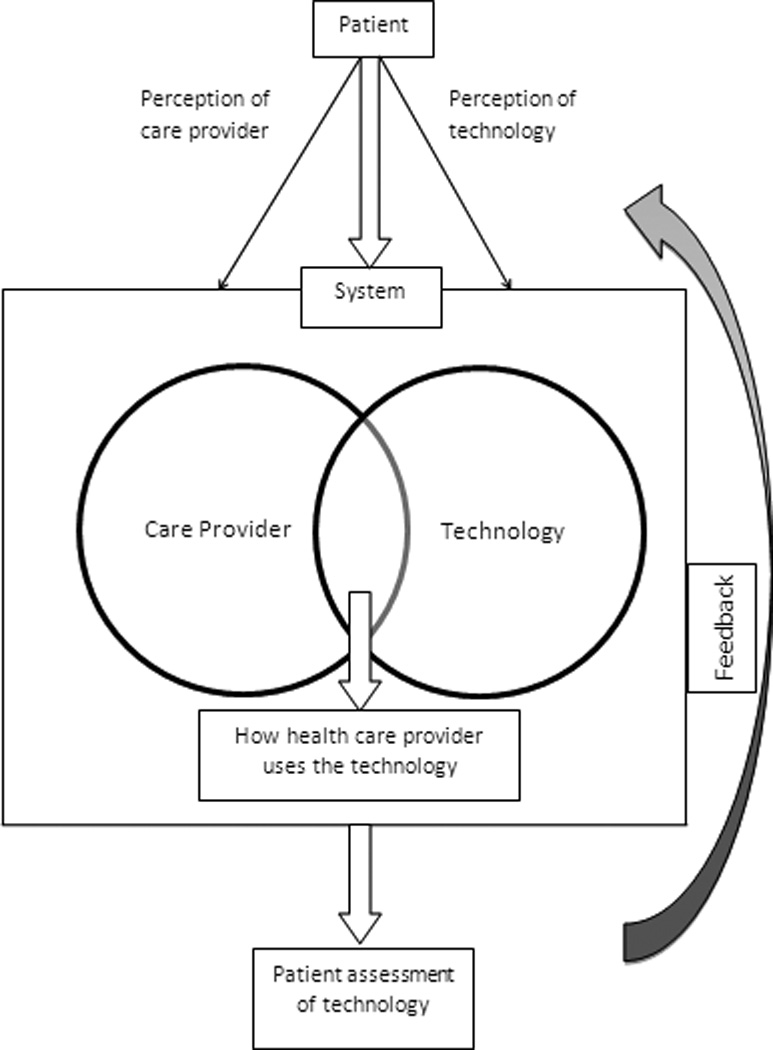
The relationship between physician-patient and technology
This study quantitatively examined how physicians interacted with EHRs in primary care environments. The purpose of this study was to understand how physicians physically interacted with EHRs while providing care to the patients. The study used quantified observational methods to identify different interaction styles, wherein clinical encounters were videotaped and reduced to measureable units. Additionally, qualitative methods were used to describe themes of identified interaction styles. Study findings might contribute to the design of EHRs and other health information technologies that compliment patient and physician capabilities and limitations.
2. Method
2.1. Data collection and sample
100 patients and 10 physicians were recruited from five primary care clinics in 2011. Physicians from the clinic sites were invited to participate in the study by email. Eligible patients (18–65 years old) were identified through the clinic’s electronic scheduling system by a staff member authorized to work with patient data. A research specialist affiliated with the clinic contacted candidate patient participants by phone two days before their clinical appointment. The research specialist described the study, invited the patients to participate in the study, and asked them to arrive at the clinic 15 minutes early to complete the informed consent procedures. Patients who scheduled their visits within the last few days were invited to participate, on the day of their visit, by the receptionist with a standardized script explaining the study. No new patients of physicians were recruited to mitigate the potential effects of processes related to first-time encounters. Informed consent was obtained from both patient and physician participants. The study protocol was approved by university and clinic Institutional Review Boards and HIPAA (Health Insurance Portability and Accountability Act) regulations were fulfilled. All visits were recorded with high-resolution video cameras. Ten patients per physician were recruited; 56 males and 44 females comprised the patient group. 78 participants were White/Caucasian. Of the patients, 10 had some high school education, 27 were high school graduates, 24 had some college education, and 39 were college graduates. Patients were between 18 and 65 years old (mean [M] = 45.2 years old) and were patients of their primary care physicians for 1 to 38 years. Six male and four female physicians volunteered to participate in the study (mean [M] = 47.6 years old) and had been practicing family medicine for 5 to 37 years. The recruited physicians had been using computers in clinical consultations for 3 to 10 years.
2.2. Empirical analysis
2.2.1. Variables
Physician gaze at the computer and typing were the variables of interest (Table 1). Gaze and typing have been used as variables to analyze physician-computer interaction in previous studies (Margalit et al., 2006; Pearce et al., 2011). Typing is an indicator of data entry activities, while physician gaze at the computer is an indicator of information gathering, or data sharing when it is done collaboratively with patients (Montague et al., 2010). Duration of physician gaze at the EHR, typing, and visit length were obtained through coding the data. The percentage of the physician’s time spent gazing at the computer and typing was also calculated. Validated survey questions evaluated patient assessment of their physician and their physician’s use of the EHR after the patient visit (Pearson et al., 2000; Thom et al., 2002; Hall et al., 2002; Montague et al., 2010).
Table 1.
Coding scheme of the study
| Codes | Definition |
|---|---|
| Subjects | |
| Patient | The patient in the encounter. |
| Physician | The primary care provider in the encounter. |
| Behaviours | |
| Gaze | Subject’s head and/or body were in the direction of the target object. |
| Typing | Subject used the keyboard to enter information. |
| Object | |
| Computer | The computer used in the medical visit. |
2.2.2. Temporal video coding
Coding is the process of converting complex data into measurable units (Miles & Hubberman, 1994). A coding scheme was created for the variables of interest (Table 1). Each video was coded temporally for the entire visit length (Figure 2). Start and stop times for each code were annotated using software (Noldus Observer XT) designed for video coding, evaluation, and analysis. The software calculated the start and stop times, duration, and simultaneous occurrence of two or more codes.
Figure 2.
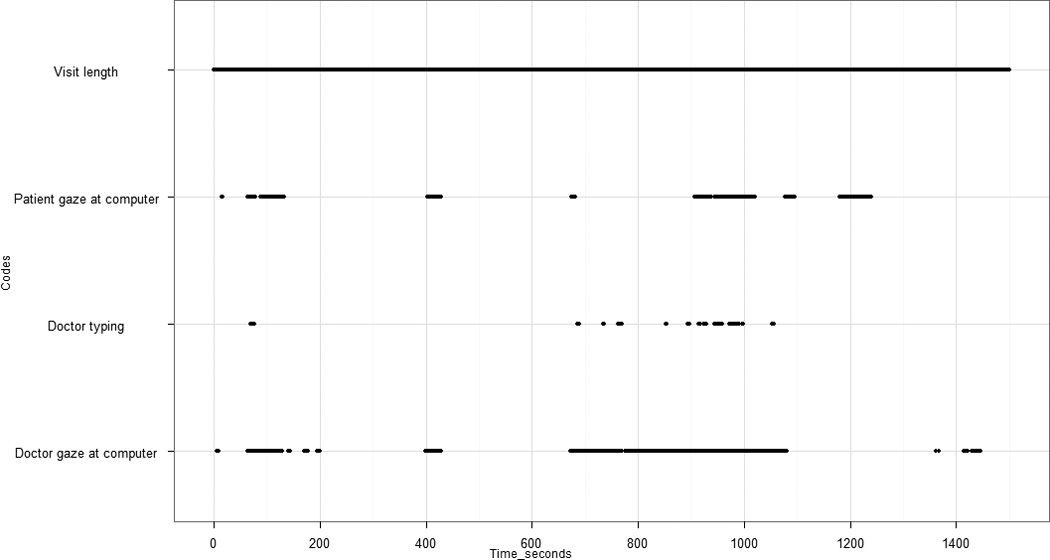
A sample temporal coding of a visit
All videos were coded by five, trained research assistants based on the coding scheme (Table 1). Coders were trained to execute the coding procedures and reliability checks were conducted at regular intervals. Reliability scores (Cohen’s kappa) for codes ranged from 0.62 to 0.88. The Cohen’s Kappa range is considered standard for 0.60 and excellent for 0.75 (Bakeman, 2000). The reliability time period was X±1 second, which is relatively conservative.
2.3. Classification approach and qualitative analysis
This study used a multi stage approach to classify interaction styles:
Physician typing and gaze behaviors were coded temporally through each of the patient visits according to the coding scheme created in Table 1.
Behavior durations (physician gaze at computer and typing) and percentage of times these behaviors occurred during the visit was calculated for each physician.
Cluster analysis was performed with typing and gaze behaviour data, which resulted in grouping physicians into the different interaction styles based on their typing and gaze behaviour.
Finally, qualitative thematic analysis was conducted to analyze videos holistically for themes within each identified interaction style.
Percentage values for the occurrence of each code were estimated as duration of the behavior in the visit length. Visit length is defined as the length of visit time during which the physician and patient used verbal communication, excluding the physical exam period.
Thematic analysis focuses on identifiable themes or behaviors (Boyatzis, 1998). In this study, thematic analysis was used to identify qualitative themes related to physicians’ interaction with EHR and patients during the visits in each identified group (technology-centered, mixed, human-centered). Analysis activities included: video observation and summarizing the observations to develop a list of behavioral markers in the visit. These behavioral markers included the physician’s multi-tasking, body language, ability to maintain eye contact with the patient, and level of engagement with the computer. Each video was analyzed qualitatively according to this list to describe the themes and patterned regularities for each identified interaction groups.
3. Results
The percentage of time the physician gazed at the computer varied from 24.9 to 49.6 % of the visit between interaction groups (Table 2). Typing time also varied ranging from 2.8 to 21.6% between groups. Three distinct classifications of physician interaction behaviors emerged from the data; these were labelled technology-centered, mixed, and human-centered. Interaction behaviors were classified based on the percentage of typing and gazing at computer during the visits. The technology-centered group gazed at the computer for 49.6% of the visit length and typed for 21.6% of the visit length. The mixed group’s gaze was reported at 34.8%, and they typed during 8.5% of the visit length. The human-centered group gazed at the computer for 24.9% and typed only 2.8% of the visit length (Table 2). The cut off values, which were based on mean quartiles, were technology-centered: > 15%, mixed: 5%–15%, and human-centered: < 5% of the visit length for typing; technology-centered: > 40%, mixed: 30%–40%, and human-centered: < 30% of the visit length for physician gaze at computer.
Table 2.
Mean ratings for physician interaction and patient assessments
| Interaction Style |
N= Visits |
Visit Length | MD gaze at computer |
Typing | Patient trust in physician* |
Patient trust in physicians' EHR use* |
Patient satisfaction of physicians' EHR use * |
||
|---|---|---|---|---|---|---|---|---|---|
| Time(sec) | Time (sec) |
% | Time (sec) |
% | Mean rating |
Mean rating | Mean rating | ||
| Technology Centered | 20 | 1449.75 | 717.78 | 49.6% | 269.27 | 21.6% | 4.55 | 4.59 | 4.59 |
| Mixed | 40 | 1011.25 | 348.64 | 34.8% | 84.29 | 8.5% | 4.73 | 4.69 | 4.67 |
| Human Centered | 40 | 924.45 | 225.16 | 24.9% | 29.04 | 2.8% | 4.66 | 4.43 | 4.62 |
Note:
out of 5-point Likert scale
To validate the classification, the relationship between typing time and classification was evaluated with a t-test with α =0.05. level; significant differences in typing time were found between the technology-centered and human-centered groups (p=0.000), technology-centered and mixed groups (p=0.002), and mixed and human-centered groups (p=0.004). There was also a significant difference in physician time gazing at computer between classification groups: technology-centered and human-centered (p=0.000), technology-centered and mixed (p=0.004), and mixed and human-centered (p=0.003). In addition, patient assessments of physicians’ EHR use were obtained with survey items, using a 5-point Likert response scale, five indicating high levels of the construct. The table shows that all physicians received high ratings for patient trust, patient trust in the physician’s EHR use, and patient satisfaction with physician’s EHR use (>4 out of 5). The construct validity of the survey items was also assessed by Cronbach’s alpha. The Cronbach’s alpha score was 0.74, which is above acceptable range.
3.1. Qualitative descriptions of each group
Based on patterns identified across visits, interactions could be linked to individual physicians. For example, if the total number of a physician’s visits were classified as technology-centered, that physician was classified by the interactive characteristics of that group. It was also observed that the behaviors described below for each group were consistent for each physician across all ten patients seen. Similar to previous work (Sykes et al., 2011), age was related to physicians' style of using health information technologies. Physicians with human-centered styles tended to be older (61 to 69 years old), while physicians in the other two groups were younger (37 to 44 years old).
The environment that physicians worked in was relatively similar. Several tasks were conducted by physicians using EHRs during visits. These tasks include information gathering, information documentation, information reviewing, ordering a lab or test, looking up treatment options, and printing patient instructions (Hayrinen et al., 2007). In this study, all physicians used the same EHR system. The physical layout of the exam rooms was also similar, so the layout had minimal effect on physician interactions with patients and EHRs. Finally, paper charts were used by some physicians, as a complement to the EHR, during the visits.
Physicians in the technology-centered group (n=2) typed the most out of the three groups; they typed 21.6% of the visit length and gazed at the computer 49.6% of the visit. They typed continuously throughout the visit (mean [M] = 269.27 s. per visit), compared to physicians in the mixed group who typed periodically in the visit (mean [M] = 84.29 s. per visit). Descriptively, physicians in the technology-centered group had a tendency to multitask; activities included trying to maintain eye contact with the patient while typing, talking to patients while gazing at the computer, verbal and nonverbal backchannels such as affirmative speech (e.g. “ok”, “I see”, “mm hmm”), and nodding. They also tended to type quickly using a touch typing style, which is typically used by individuals with expert typing abilities (Goldberg & Richardson, 1993).
Physicians in the mixed group (n=4) typed 8.5% of the visit and gazed at the computer 34.8% of the visit. Descriptively, physicians in this group did not multitask as much as physicians in the technology-centered group. Physicians in the mixed group tended to interact with EHR through brief, short typing sessions where they focused solely on the EHR. When they spoke to patients they tended to stop typing and focus on the patient. Physicians in this group also maintained positive nonverbal behaviors such as a postural style that allowed the physician to face the patient most of the time.
Physicians in the human-centered group (n=4) typed the least at 2.8% of the visit and gazed at the computer 24.9% of the visit. Descriptively, this group tended to have less developed typing skills and typed more slowly using a hunt and peck style characteristic of novice typers (Goldberg & Richardson, 1993). This group did not multitask. These physicians also used aids to help manage data entry such as paper charts, nurse scribes, and voice dictation. For example, a physician who used a nurse scribe during visits explained to patients that this was due to poor typing skills and that it provided the physician with the opportunity to focus more on the patient. Physicians in this group had higher amounts of positive verbal and nonverbal communication with patients than physicians in the technology-centered and mixed groups. They mostly focused on patients rather than EHR during the visit. Positive verbal and nonverbal communication is essential for a successful clinical practice (Marcinowicz et al., 2010).
4. Discussion
Physicians in this study received high ratings of patient trust (mean [M] = 4.64 out of 5 points) and patient satisfaction with their use of EHRs (mean [M] = 4.62 out of 5 points). Results show that these physicians had different styles of interacting with EHRs, which were called technology-centered, human-centered, and mixed. Because each of these groups received high ratings of patient satisfaction, it may indicate that a variety of different human-technology interactive styles may be effective for physician interaction with health information technology while providing patient care. This finding should be explored with larger samples in future studies. Furthermore, one of the reasons for high ratings might be that an overarching trust in a physician might be associated with patients’ trust and satisfaction in the physician's EHR use regardless of interaction style. A previous study also indicated that patient trust in physicians influences patients’ perceptions of physicians’ technology use (Montague & Asan, 2012). Another reason might be that patients mostly see only their physicians and assume their physicians’ interaction with the EHR is the ideal one, since they do not have a chance to compare with other physicians’ interaction styles.
Physical interaction with the EHR was primarily in the form of typing, though physicians also interacted with the technology through gaze (Pearce et al., 2011). Qualitatively, typing was used to input information (i.e. data entry) (Margalit et al., 2006), while gaze that did not occur while typing was used to extract information (i.e. finding information during discussion about the patient’s past medical record, checking information, or sharing information with the patient). Results show a relationship between the amount of time a physician interacted with the computer through typing and the amount of time they interacted through gaze. Physicians who typed for higher percentages of the visit also tended to gaze at the computer more, while physicians who typed for smaller percentages of the visit tended to gaze at the computer less.
Physicians in the technology-centered group tried to provide positive verbal and nonverbal communication while interacting with the EHR. They used verbal and non-verbal backchannels to illustrate that they were listening. It is possible that inputting information might also be an effective method of showing the patient that they are being heard. In contrast, physicians in the mixed group switched their attention from the patient to the EHR and back throughout the visit; they also provided positive verbal and nonverbal communication during the times they focused on the patient. In contrast to the mixed and technology-centered groups, physicians in the human-centered group spent the majority of their time focusing on the patient and relied on aids and post-visit time to input data.
It was expected that all physicians would spend a similar amount of time gazing at the screen to extract information from EHRs during the visits. However, the results show that technology-centered physicians spent the most time inputting and extracting information, which may illustrate an inability to interact with the technology at high levels or recall information about the patient. One advantage of this style of interaction is that it may be more efficient, in terms of time spent interacting with the patient and inputting necessary data during the visit, which leads to minimal time spent charting after the visits. However, physicians who rely on this interaction style may experience challenges in situations where it may be necessary to provide care without technologies (Singh et al., 2012). Other disadvantages are that this group may not be able to communicate empathy appropriately when it is necessary because of the methods they tend to use (multitasking with short verbal and nonverbal interactions). Attempting to engage in multitasking has been said to be the opposite of “mindful presence” and has been implicated as a source of error (Lown & Rodriguez, 2012). Other potential disadvantages may be that the cognitive demands associated with simultaneous data entry, data extraction, and communication may lead to ineffective allocations among the three. This potential problem has been described in previous EHR interaction studies (Margalit et al., 2006; Shachak & Reis, 2009). For example, physicians in the technology-centered group relied on the EHR to extract information about the patient more than the other groups. This over-reliance on technology to provide information may be because it was difficult for them to remember information about the patient, recall details, or maintain active engagement in the conversation while typing.
Physicians in the mixed group tended to alternate their interactions with the technology with patient-centered interactions throughout the visit. Physicians who used this method also received high ratings for patient satisfaction. Some of the major risks associated with this interaction style are that the physicians might over-rely or under-rely on the technology, falling into the technology-centered or human-centered interaction styles. This can also be considered a benefit as this ability to shift when needed may reduce potential burnout, since physicians can control how much attention they give to the EHR and the patient respectively.
Finally, physicians in the human-centered group tended to under-rely on the technology. They had a tendency to focus their interactions on the patient completely, using a variety of aides to accomplish the necessary task of entering data from the visit into the record. This interaction may have been the most costly in terms of time and cost. In order to keep the record up to date, physicians entered data after the visit and utilized aides such as transcribers. Some of the benefits of this style are that the patients received high levels of patient-centered communicative behaviors, in terms of eye contact and listening. This group of physicians also had lower levels of gaze at the computer, which may indicate that they did not need to extract information about the patients from the EHR as much as the physicians in the mixed and technology-centered groups. This could indicate that human-centered physicians knew their patients better, were better able to remember important information, or that they were interested in information that could not be found in the EHR. One risk of this interaction style is that physicians might lose or forget important information before it is inputted into the record. Secondly, these physicians may be more prone to burn-out because they must be affectively engaged through the entire visit and they must rely heavily on their memory to communicate with the patient. Finally, they may not be fully benefitting from EHRs and other HITs that may enhance the quality of care they are able to provide.
Understanding how physicians’ interaction styles diverge thus plays an important role in identifying specific design features of EHR systems that can better aid physicians for effective encounters (Ventres & Shah, 2007). The United States health care system is transitioning to computer-based systems, so there is a need to optimize EHR system design for more effective patient encounters. An EHR system that is difficult to navigate may demand more attention from the physician, drawing the physician away from the patient, or it may lead the physician to reject the system altogether (Lawler et al., 2011). Different EHR systems might also have the potential to produce various interaction styles between physicians, depending on system design and implementation (Ventres et al., 2005). For instance, human-centered physicians tended to have poor typing skills in this study, so the EHR system should have an easier data input function for them during the visit. One study showed that some of the older physicians considered leaving the hospital after the it transitioned to a computer-based system, because they were uncomfortable using the computers due to poor computer skills (Rippen et al., 2012). In addition, future EHR designs might have a patient device integrated within the EHR so patients can input data to the system while waiting for the encounter. This might decrease data input time for the physicians during the visit. New devices that have the mobility of paper charts might also be used to extract information, thus facilitating facing the patient while using EHR. Furthermore, EHR systems should have functions to reduce time and cognitive load associated with EHR use. Some of the proposed EHR features are: having easy to share and visually scan screens with problem lists, providing a summary of previous visits, and offering access to digital data from other relevant sources (Shachak & Reis, 2009).
There are several limitations to this study. First, the sample was limited to primary care encounters; other interactions may emerge in other settings. Data were collected with a single EHR system and physician population (i.e. primary care physicians), so the generalizability of these findings and the classification system used should be validated through further research with larger sample sizes in a variety of contexts. Of the eligible patients, the recruitment rate of the study was 47%. Patients that chose not to participate may have different attitudes towards their clinician or EHR and may have more complex health needs.
5. Conclusion
These findings illustrate that different methods of interaction with EHR may be effective in contributing to patient-centered outcomes. However, each method may have short- and long-term consequences. Data regarding these potential consequences was not collected in this study, but should be explored in future studies.
It is essential to identify effective strategies to integrate EHRs into clinical practice. An effective EHR design would leverage what is known about the physical, cognitive, and social needs of physicians to facilitate effective interaction with both the patient and the technology (Lawler et al., 2011). Future EHR designs and training systems should consider flexible systems that accommodate the variety of interaction styles that physicians in this study used to provide patient-centered care. Training programs could teach the use of health information technology systems during patient visits, focusing on incorporating EHR use with patient communication and potential consequences of EHR use on physician-patient interaction. It may be worthwhile to develop standardized physician health IT training systems to develop physicians’ skills and effective use of EHRs while communicating with patients. Future work in the area should evaluate new technologies that afford each of these interaction styles for their relation to variables relevant to patient and organizational outcomes. Understanding the relationship between HIT design, physician interaction behaviors, and patient-centred communication will be increasingly important as EHR and HITs become more pervasive and contain larger amounts of information, such as data from the home or consumer health technologies.
Acknowledgements
The University of Wisconsin-Madison Systems Engineering Initiative for Patient Safety (SEIPS) and the Wisconsin Research and Education Network (WREN) provided support on this project. We thank undergraduate research assistants who assisted with data analysis and graduate research assistants who assisted with data collection.
Funding Source: This publication was supported by Grant No. 1UL1RR025011 from the Clinical & Translational Science Award (CTSA) program of the National Center for Research Resources of the National Institutes of Health.
Footnotes
Author Contributions
All authors contributed toward the conception and design of the study, acquisition of data, analysis and interpretation of data, drafting of the article or revising it critically for important intellectual content, and the final approval of the version to be submitted.
Conflict of Interest
None of the authors have any conflicts of interest that could bias this work.
Ethics approval: This study was conducted with the approval of the University of Wisconsin-Madison Health Science Institutional Review Board.
REFERENCES
- Bakeman R. Behavioral observation and coding. Handbook of research methods in social and personality psychology. 2000:138–159. [Google Scholar]
- Blumenthal D. Stimulating the adoption of health information technology. New England Journal of Medicine. 2009;360(15):1477–1477. doi: 10.1056/NEJMp0901592. [DOI] [PubMed] [Google Scholar]
- Boyatzis RE. Transforming qualitative information: Thematic analysis and code development. Sage Publications, Inc; 1998. [Google Scholar]
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Shekelle PG. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine. 2006;144(10):e12–e22. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- Fang H, Peifer K, Chen J, Rizzo J. Health information technology and physicians' perceptions of healthcare quality. The American Journal Journal of Managed Care Managed Care. 2011;17(3):e66–e70. [PubMed] [Google Scholar]
- Goldberg D, Richardson C. Touch-typing with a stylus; Paper presented at the INTERACT '93 and CHI '93 conference on Human factors in computing systems; New York, NY. 1993. [Google Scholar]
- Graham-Jones P, Jain SH, Friedman CP, Marcotte L, Blumenthal D. The need to incorporate health information technology into physicians’ education and professional development. The need to incorporate health information technology into physicians’ education and professional development. Health Affairs. 2012;31(3):481–487. doi: 10.1377/hlthaff.2011.0423. [DOI] [PubMed] [Google Scholar]
- Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, Balkrishnan R. Measuring patients’ trust in their primary care providers. Medical Care Research and Review Care Research and Review. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impact of electronic health records: a review of the research literature. International Journal of Medical Informatics. 2007;77:291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Holden RJ. Social and personal normative influences on healthcare professionals to use information technology: Towards a more robust social ergonomics. Theoretical Issues in Ergonomics Science, First published on: 28 March 2011 (iFirst) 2011:1–24. doi: 10.1080/1463922X.2010.549249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler EK, Hedge A, Pavlovic-Veselinovic S. Cognitive ergonomics, socio-technical systems, and the impact of healthcare information technologies. International Journal of Industrial Ergonomics. 2011;41:336–344. [Google Scholar]
- Lelievre S, Schultz K. Does computer use in patient-physician encounters influence patient satisfaction? Canadian Family Physician. 2010;56(1):e6–e9. [PMC free article] [PubMed] [Google Scholar]
- Lown BA, Rodriguez D. Commentary: Lost in translation? how electronic health records structure communication, relationships, and meaning.translation? how electronic health records structure communication, relationships, and meaning. Academic Medicine. 2012;87(4):392–394. doi: 10.1097/ACM.0b013e318248e5ae. [DOI] [PubMed] [Google Scholar]
- Marcinowicz L, Konstantynowicz J, Godlewski C. Patients' perceptions of GP non-verbal communication: A qualitative study. The British Journal of General Practice. 2010;60(571):83–87. doi: 10.3399/bjgp10X483111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician-patient communication: An observational study of Israeli primary care encounters. Patient Education Education and Counseling Counseling. 2006;61(1):134–141. doi: 10.1016/j.pec.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Miles MB, Hubberman AM. Data management and analysis methods. In: Denzin NK, Lincoln YS, editors. Qualitative data analysis: An expanded source book. 2nd ed. CA: Thousand Oaks: 1994. pp. 428–444. [Google Scholar]
- Montague E, Asan O. Trust in technology-mediated collaborative health encounters: Constructing trust in passive user interactions with technologies. Ergonomics, First published on: 16 April 2012 (iFirst) 2012 doi: 10.1080/00140139.2012.663002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montague E, Winchester WW, Kleiner BM. Trust in medical technology by patients and health care providers in obstetric work systems. Behaviour & Information Technology. 2010;29(5):541–554. doi: 10.1080/01449291003752914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montague E, Xu J, Chen P, Asan O, Barrett BP, Chewning B. Modeling Eye Gaze Patterns in Clinician–Patient Interaction With Lag Sequential Analysis. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2011;53(5):502–516. doi: 10.1177/0018720811405986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow JB, Dobbie AE, Jenkins C, Long R, Mihalic A, Wagner J. First-year medical students can demonstrate EHR-specific communication skills: A control-group study. Family Medicine. 2009;41(1):28–33. [PubMed] [Google Scholar]
- Ong L, De Haes J, Hoos A, Lammes F. Doctor-patient communication: A review of the literature. Social Science & Medicine. 1995;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- Otto A, Kushniruk A, Ho K, Joe R, Borycki E. Incorporation of medical informatics and information technology as core components of undergraduate medical education-Time to change. Studies in Health Technology and Informatics. 2009;143:62–67. [PubMed] [Google Scholar]
- Pearce C, Arnold M, Phillips C, Trumble S, Dwan K. The patient and the computer in the primary care consultation. Journal of the American Medical Informatics Association. 2011;18(2):138–142. doi: 10.1136/jamia.2010.006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. Journal of General Intern Medicine. 2000;15:509–513. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao SR, DesRoches CM, Donelan K, Campbell EG, Miralles PD, Jha AK. Electronic health records in small physician practices: Availability, use, and perceived benefits. Journal of the American Medical Informatics Association. 2011;18(3):271–275. doi: 10.1136/amiajnl-2010-000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rippen HE, Pan EC, Russell C, Byrne CM, Swift EK. Organizational framework for health information technology. International Journal of Medical Informatics, First published on: 28 February 2012 (iFirst) 2012 doi: 10.1016/j.ijmedinf.2012.01.012. [DOI] [PubMed] [Google Scholar]
- Roter D, Frankel R, Hall J, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Journal of General Internal Medicine. 2006;21(S1):S28–S34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouf E, Whittle J, Lu N, Schwartz MD. Computers in the exam room: Differences in physician–patient interaction may be due to physician experience. Journal of General Internal Medicine General Internal Medicine. 2007;22(1):43–48. doi: 10.1007/s11606-007-0112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shachak A, Reis S. The impact of electronic medical records on patient–doctor communication during consultation: A narrative literature review. Journal of Evaluation in Clinical Practice. 2009;15(4):641–649. doi: 10.1111/j.1365-2753.2008.01065.x. [DOI] [PubMed] [Google Scholar]
- Singh R, Lichter MI, Danzo A, Taylor J, Rosenthal T. The adoption and use of Health Information health information technology in Rural rural areas: Results of a National national survey. The Journal of Rural Health. 2012;28(1):16–27. doi: 10.1111/j.1748-0361.2011.00370.x. [DOI] [PubMed] [Google Scholar]
- Stead WW, Lin H. Computational technology for effective health care: immediate steps and strategic directions. Natl Academy Pr; 2009. [PubMed] [Google Scholar]
- Sykes TA, Venkatesh V, Rai A. Explaining physicians' use of EMR systems and performance in the shakedown phase. Journal of the American Medical Informatics Association. 2011;18(2):125–130. doi: 10.1136/jamia.2010.009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom DH, Kravitz RL, Bell RA, Krupat E, Rahman A. Patient trust in the physician: relationship to patient requests. Family Practice. 2002;19:476–483. doi: 10.1093/fampra/19.5.476. [DOI] [PubMed] [Google Scholar]
- Ventres W, Kooienga S, Marlin R, Vuckovic N, Stewart V. Clinician style and examination room computers: a video ethnography. Family Medicine. 2005;37:276–281. [PubMed] [Google Scholar]
- Ventres W, Shah A. How do EHRs affect the physician-patient relationship? American Family Physicians. 2007;75(9):1389–1391. [PubMed] [Google Scholar]


