Abstract
Background
Cervical disorders in rheumatoid arthritis (RA) patients have been an important problem for a long time. Although the recent progression of the treatment strategies for RA might change the progression of atlantoaxial vertical subluxation (VS) in RA patients, to reveal the risk factors for VS progression should be important at present. Osteoporosis (OP) and RA share the same risk factors. The purposes of this study were to identify the progression of VS in RA, and to evaluate the relationship between the VS development and OP.
Methods
Eighty female patients with RA and 18 female patients with OP were retrospectively analyzed. The RA patients were divided into VS (10 patients) and non-VS groups (70 patients). Morphological parameters on coronal reconstructed computed tomography images were evaluated. Three-dimensional analysis was used to measure volumes and volumetric bone mineral densities (vBMDs) at the upper cervical spine (UCS).
Results
The VS group had higher age, longer RA symptom duration, and lower BMD at the lumbar spine compared to the non-VS group. Volumes and vBMDs at the UCS in RA group were greater than those in the OP group. In accordance with VS development, the lateral masses at the UCS became shorter, the C1 facet angle became sharper, and the volumes at the UCS decreased. However, there was no statistically significant relationship between vBMDs at the UCS and the VS development.
Conclusion
The C1 facet angle became sharper with VS progression. Although 3-dimensional analysis revealed that decreases in the volumes at the UCS were associated with VS development, no significant relationship between OP and the VS development was observed.
Keywords: bone mineral density, osteoporosis, rheumatoid arthritis, vertical subluxation
Atlantoaxial vertical subluxation (VS) is one of the common instabilities and the most fatal complication for patients with rheumatoid arthritis (RA). Several cross-sectional studies revealed that the incidence of VS ranges from 4 to 35%.1, 2 Since patients with atlantoaxial instabilities are not always symptomatic, the real incidence of VS may actually be higher. VS may be caused by rheumatoid synovitis at the upper cervical spine (UCS), following the joint destruction of atlanto-occipital joint (AOJ) and atlantoaxial joint (AAJ). 3, 4, 5, 6, 7 However, there have been few reports on the development of lateral mass collapse in the UCS with progression of VS.8, 9 Symptoms include headache, myelopathy, dyspnea and sometimes death. Therefore, to detect subclinical VS patients and to prevent the VS progression, it is important to reveal the morphological changes at the UCS and prognostic factors for VS progression.
Many prognostic factors for VS have been reported previously, including age, sex, menopausal status, duration of RA symptoms, severity of RA, number of erosive peripheral joints, a subset with mutilating disease, and use of glucocorticoids.10, 11, 12, 13, 14, 15, 16 Some of the reported prognostic factors for VS are also risk factors for osteoporosis (OP). RA, itself, is one of the causes for secondary OP. Moreover, it has been reported that lumbar vertebral deformity in RA patients had an association with areal bone mineral density (BMD).17, 18 Therefore, we hypothesize that OP could affect the progression of VS. This study had 2 aims: to identify the morphological changes in VS progression, and to evaluate the relationship between the progression of VS and OP.
SUBJECTS AND METHODS
Subjects
Subjects were recruited from outpatient clinics at Tottori University Hospital between April 2008 and March 2009. Female patients were eligible if they had a definitive diagnosis of RA, met the revised criteria of the American College of Rheumatology, 19 and had the ability to understand and complete a written informed consent form. Patients with postmenopausal OP were recruited as controls. Patients were defined as having OP if they: i) were over 45 years of age, ii) had no history of symptoms or medication use that can induce OP (including glucocorticoids) and iii) had BMD below 70% or a T-score of −2.6 below the young adult mean as measured by a Hologic QDR bone densitometer (Hologic, Bedford, MA) or osteopenia (BMD below 80% or T-score of −1.7 below the young adult mean) with at least 1 fragility fracture, as defined by the criteria of the Japanese Society for Bone and Mineral Research. A total of 111 patients (86 patients with RA and 25 with OP) fulfilled these inclusion criteria. Investigators provided written and verbal explanations of the study and obtained a written informed consent from each subject.
To investigate the etiology of VS, RA patients were divided into 2 groups, those with VS (VS group) and those without VS (non-VS group). VS was diagnosed when the Redlund-Johnell (R-J) value was less than 29 mm on plain lateral radiographs.20
Morphological analysis by using reconstructed CT images
The morphological parameters of the UCS were evaluated on coronal reconstructed computed tomography (CT) images (Aquilion 64; Toshiba Medical Systems, Otawara, Japan). During CT scanning, subjects were in a supine position with their necks in an extended position using a special pillow. Bone mineral reference phantoms, made of hydroxylapatite (Kyoto Kagaku, Kyoto, Japan), were placed on the neck to quantify volumetric BMD (vBMD) at the UCS. In patients with dentures and implants around the occipitocervical junction, several artifacts (including halation) affected the CT data. To avoid the influence of artifacts, the CT gantry was tilted 30˚ caudally. After locating the region from the basiocciput to C3 on a lateral scout-view of the UCS, these levels were encompassed with 0.5 mm slices at 120 kV/200 mA, with a 0.5-s/rot pitch and a 153.8-mm diameter field of view.
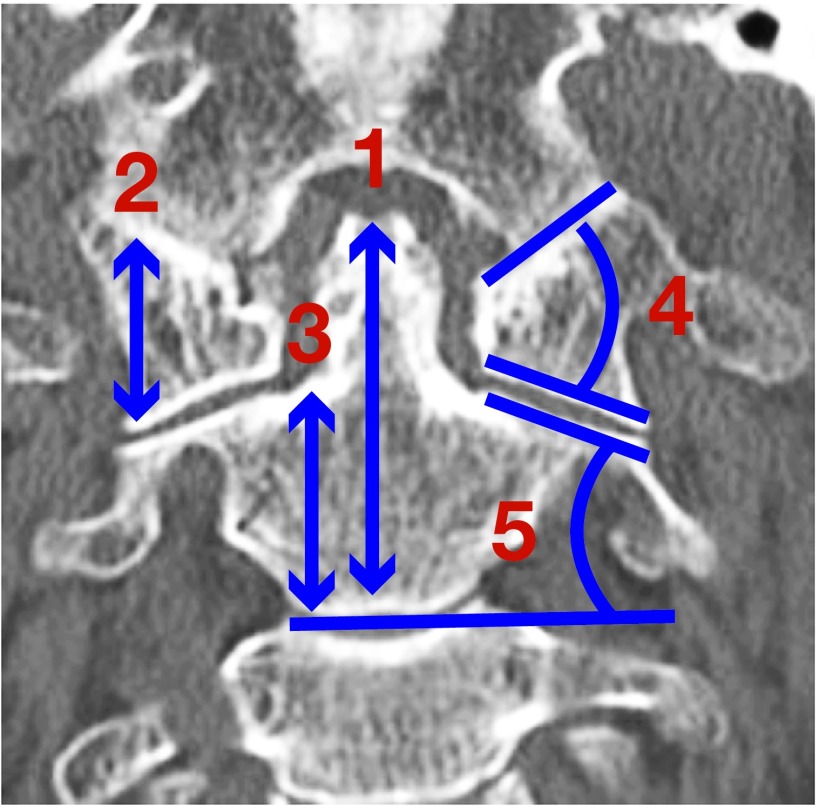
The coronal CT images were reconstructed with the axis parallel to the odontoid process. Using coronal reconstructed CT views, AOJ and AAJ were morphologically evaluated. The anatomical parameters included the odontoid height, lateral mass height (LMH) of the atlas and axis [LMH(C1) and LMH(C2), respectively], and the facet angle (FA) of the atlas and axis [FA(C1) and FA(C2), respectively] (Fig. 1). We defined these parameters as follows: LMH(C1) was the perpendicular distance from the upper to the lower peak of the C1 lateral mass. LMH(C2) was defined as the length between the lower endplate to the upper surface of the C2 facet. FA(C1) was the angle between the upper and lower facet surfaces, and FA(C2) was the angle between the lower endplate of the axis and upper facet surface of the axis. Odontoid height was defined as the perpendicular distance from the tip of the odontoid process to the lower endplate of the axis. Morphological changes at the AOJ and AAJ on the coronal reconstructed CT images were classified into 3 types: normal, erosive and ankylosing.21 Bone defects in the odontoid process were classified into 3 types: spot, small and large.22
Fig. 1.
Anatomical parameters are defined as follows:
1: odontoid height (OH)
2: lateral mass height of the atlas, LMH(C1)
3: lateral mass height of the axis, LMH(C2)
4: facet angle of the atlas, FA(C1)
5: facet angle of the axis, FA(C2)
BMD measurements at the lumbar spine and hip
The measurements of BMD at the lumbar spine (L2-4) [BMD(lumbar)] and right hip were performed using postero-anterior dual X-ray energy absorptiometry with the QDR Discovery instrument (Hologic). For the BMD of the hip [BMD(hip)], we used the neck BMD value.
vBMD measurements at the UCS
To measure vBMD at the UCS, we employed the 3-dimensional TEIJIN Bone Structure Analysis System (3D-TBSAS; Teijin Pharma, Tokyo, Japan), which was based on the theory of Azuma et al.23
The original raw CT data in DICOM format was obtained from the same CT device (described above) with a slice thickness of 0.5 mm and pixel width of 0.35 mm and used by 3D-TBSAS to construct a 3-dimensional model. The system could distinguish and separate each structure according to bone continuity. The watershed of discontinuity was set at 0.5 mm. For each structure, 3D-TBSAS calculated the whole tissue volume, bone volume, the percentage of bone tissue (bone volume/ tissue volume) and the average CT value for the whole tissue. We analyzed each phantom (200, 300, 400, 500, 600 mg/mL, made with hydroxylapatite and 1,550 mg/mL phantom, made with alumina) and the structures in the UCS. Once each structure was distinguished, we could unite the separate bones and calculate the combined vBMD using this system. Since a linear correlation between vBMD and averaged CT values of the phantom was confirmed, the average CT value of each skeletal structure was calculated. Finally, the vBMD was calculated as follows: vBMD = average CT value × (bone volume/tissue volume).
The percentage of coefficient of variation in this system was evaluated by 105 repeated measurements for the phantoms (300, 400, 500 and 600 mg/mL). The percentage of coefficient of variation was defined as less than 0.1%.
Using 3D-TBSAS, we could calculate the volume of the atlas, axis and C1-2 [V(C1), V(C2) and V(C1-2), respectively], and the vBMD of the atlas, axis and C1-2 [vBMD(C1), vBMD(C2) and vBMD(C1-2), respectively]. In cases of severely destructed or fused bony structures, 3D-TBSAS could neither distinguish each structure nor calculate the correct vBMDs. RA patients with severe rheumatoid changes at the UCS were unable to calculate vBMDs at the UCS. The remaining 33 patients with RA in the non-VS group and 18 with OP were analyzed 3-dimentionally.
Statistical analysis
Differences in demographic data and characteristics between 2 groups were analyzed using the Mann-Whitney U test, and those for 3 groups were analyzed using the Kruskal-Wallis test and the Steel-Dwass test for multiple comparisons. Pearson’s chi-square test or Fisher’s exact test were used to compare the categories or ratios of variables. Spearman’s rank correlation coefficient was used for the analysis between 2 parameters. P < 0.05 was considered to indicate statistical significance.
To clarify the effects of OP, we performed multiple logistic regression analysis for the development of VS by using the statistical significant factors from the comparison between the VS and non-VS groups. Statistical analyses were performed using PASW Statistics version 18.0.0 (SPSS, Chicago, IL).
The present study was approved by the Ethics Committee of Tottori University (No. 1088).
RESULTS
Demographic data
Ultimately, 99 eligible patients [80 patients with RA and 19 with OP (OP group)] agreed to participate in this study. Six patients with RA and 6 with OP did not agree to participate, and 4 patients with OP withdrew their consents. There were 10 patients in the VS group and 70 in the non-VS group (Table 1). The incidence of VS in the present study was 12.5% (10 out of 80 RA subjects) and all but 1 patient were asymptomatic (1 patient was classified as Ranawat I24).
Table 1. Characteristics of study patients.

Data are expressed as means (range).
BMD, bone mineral density; CRP, C-reactive protein; DAS, disease activity score; ESR, erythrocyte sedimentation rate; MMP-3, matrix metalloproteinase-3; NS, not significant; OP, postmenopausal osteoporosis; RA, rheumatoid arthritis; RF, rheumatoid factor; VS, vertical subluxation.
P < 0.05 was considered statistically significant among 3 groups. When there was a statistical significance between 2 groups, we showed the relationships as follows in the table: *P < 0.05. **P < 0.01. ***P < 0.001.
Demographic data are shown in Table 1. All subjects were postmenopausal, except for 2 in the non-VS group. The mean age of the non-VS group was significantly lower than in the VS and OP groups, but there were no other significant differences between the VS and OP groups.
Between VS and non-VS groups, there were no significant differences in glucocorticoid usage, neurological function and severity of RA (Table 1). The duration of RA in the VS group was significantly longer than in the non-VS group.
Differences in BMD
BMD(lumbar) in the OP group was significantly lower than in the VS and non-VS groups, but there was no significant difference between the VS and non-VS group (Table 1). There were no statistical differences in BMD(hip) among the 3 groups.
Morphological findings on coronal reconstructed CT images
Left and right levels of LMH(C1) in the VS group were significantly lower than in the OP group (Fig. 2). Left and right levels of LMH(C2) in the VS group were significantly lower than in the non-VS and OP groups; however, there was no statistical difference between the non-VS and OP groups (Fig. 3). Right FA(C1) in the VS group was significantly more acute than in the OP group. There were no significant differences in left and right FA(C2) levels and odontoid height (Table 2).
Fig. 2.
Measurements of LMH(C1) in the OP, non-VS and VS groups. The VS group shows lower levels of right and left LMH(C1) than the OP group. There is no statistical difference between the VS and non-VS groups. P < 0.05 was considered statistically significant. LMH(C1), lateral mass height of the atlas; OP, osteoporosis; VS, vertical subluxation. [ ], number of subjects.
Fig. 3.
Measurements of LMH(C2) in the OP, non-VS and VS groups. The VS group shows lower levels of right and left LMH(C2). P < 0.05 was considered statistically significant. LMH(C2), lateral mass height of the axis; OP, osteoporosis; VS, vertical subluxation. [ ], number of subjects.
Table 2. Morphological findings on coronal reconstructed CT images.
| OP group [n = 19] | Non-VS group [n = 70] | VS group [n = 10] | P value | |||
| Odontoid height (mm) | 31.9 (27.6–35.5) | 32.2 (27.1–38.9) | 29.7 (27.4–32.0) | 0.236 | ||
| LMH(C1) (mm) | L | 11.1 (7.5–15.2) | 9.4 (6.1–14.5) | 7.5 (4.1–10.5) | 0.075 | |
| R | 10.9 (7.0–13.7) | 9.7 (6.4–15.7) | 7.1 (3.1–10.4) | 0.075 | ||
| LMH(C2) (mm) | L | 12.2 (9.8–14.1) | 12.6 (9.4–17.0) | 9.4 (3.8–13.8) | 0.001 | |
| R | 12.7 (10.9–15.7) | 12.9 (10.6–16.8) | 9.8 (8.4–13.0) | 0.001 | ||
| FA(C1) (°) | L | 59.3 (47.8–70.0) | 55.6 (35.2–71.4) | 49.7 (42.1–58.0) | 0.075 | |
| R | 63.5 (51.3–76.5) | 54.8 (33.6–75.7) | 41.7 (8.5–58.5) | 0.013 | ||
| FA(C2) (°) | L | 22.6 (17.2–28.9) | 21.1 (11.1–31.3) | 21.3 (14.0–29.7) | 0.658 | |
| R | 24.2 (16.8–31.1) | 21.3 (11.6–34.8) | 20.8 (9.3–27.0) | 0.286 | ||
| AOJ changes | Normal | L | 15 (78.6) | 35 (50.0) | 1 (10.0) | |
| R | 15 (78.6) | 35 (50.0) | 1 (10.0) | |||
| Erosive | L | 4 (21.4) | 30 (42.9) | 6 (60.0) | L: < 0.001 | |
| R | 4 (21.4) | 30 (42.9) | 4 (40.0) | R: < 0.001 | ||
| Ankylosing | L | 0 (0.0) | 5 (7.1) | 3 (30.0) | ||
| R | 0 (0.0) | 5 (7.1) | 5 (50.0) | |||
| AAJ changes | Normal | L | 17 (89.5) | 38 (54.3) | 1 (10.0) | |
| R | 16 (64.2) | 34 (48.6) | 2 (20.0) | |||
| Erosive | L | 2 (10.5) | 27 (38.6) | 5 (50.0) | L: < 0.001 | |
| R | 2 (10.5) | 31 (44.3) | 3 (30.0) | R: < 0.001 | ||
| Ankylosing | L | 0 (0.0) | 5 (7.1) | 4 (40.0) | ||
| R | 1 (5.3) | 5 (7.1) | 5 (50.0) | |||
| Bone defects in the odontoid process | Spot | 9 (47.4) | 34 (48.6) | 0 (0.0) | < 0.001 | |
| Small | 5 (26.3) | 31 (44.3) | 6 (60.0) | |||
| Large | 5 (26.3) | 5 (7.1) | 4 (40.0) | |||
Data of parameters are expressed as means (range) and non-parametrical data are expressed as the number of patients (%).
AAJ, atlantoaxial joint; AOJ, atlanto-occipital joint; CT, computed tomography; FA, facet angle; L, left; LMH, lateral mass height; NS, not significant; OP, postmenopausal osteoporosis; R, right; VS, vertical subluxation.
Mann-Whitney’s U test was used to compare between non-VS and VS groups. Pearson’s chi-square test or Fisher’s exact test, when appropriate, was employed for comparisons.
P values were derived by the comparison between non-VS and VS groups.
Compared with the non-VS and OP groups, erosive and ankylosing changes in AOJ and AAJ were more frequently recognized in the VS group, and larger bone defects in the odontoid process were also found in the VS group (Table 2).
Three-dimensional analysis using 3D-TBSAS
The average V(C1) in the RA and OP groups was 6.91 mL (4.33–8.96 ) and 5.68 mL (3.22–8.67), respectively. The average V(C2) in the RA and OP groups was 7.69 mL (4.08–11.96) and 5.91 mL (3.60–8.62), respectively. The average V(C1-2) in the RA and OP groups was 14.32 mL (9.25–21.63) and 12.67 mL (6.81–19.97), respectively. The average vBMD(C1) in the RA and OP groups was 809.7 mg/mL (625.4–1067.9) and 755.5 mg/mL (639.9–842.6), respectively. The average vBMD(C2) in the RA and OP groups was 762.3 mg/mL (639.6–1106.8) and 741.7 mg/mL (673.3–840.2), respectively. The average vBMD(C1-2) in the RA and OP groups was 782.4 mg/mL (633.6–1086.2) and 740.9 mg/mL (590.1–902.0), respectively. Volumes and vBMDs at UCS in the RA group were larger than in the OP group, but the difference was not significant. vBMD(C1) was greater than vBMD(C2) in both the RA and OP groups. V(C2) was larger than V(C1) in both the RA and OP groups.
vBMD(C1), vBMD(C2) and vBMD(C1-2) showed a positive significant correlation with BMD(lumbar) but not BMD(hip) [vBMD(C1) versus BMD(lumbar): r = 0.580, P < 0.001, vBMD(C2) versus MD(lumbar): r = 0.466, P = 0.003, vBMD(C1-2) versus BMD(lumbar): r = 0.466, P = 0.001]. vBMDs at the UCS were strongly positively correlated with each other [vBMD(C1) versus vBMD(C2): r = 0.950, P < 0.001, vBMD(C1) versus vBMD(C1-2): r = 0.972, P < 0.001, vBMD(C2) versus vBMD(C1-2): r = 0.992, P < 0.001].
Relationship between the progression of VS and other parameters
There were significant positive correlations between the R-J value and left and right LMH at C1 and C2. Additionally, left and right FA(C1) values were positively correlated with left and right LMH(C1) values and the R-J value (Table 3).
Table 3. Relationships between the development of VS and other parameters.
| Correlation coefficient | P value | ||
| R-J value versus | LMH(C1)(R) | 0.525 | < 0.001 |
| LMH(C1)(L) | 0.287 | 0.013 | |
| LMH(C2)(R) | 0.401 | 0.003 | |
| LMH(C2)(L) | 0.414 | < 0.001 | |
| FA(C1)(R) | 0.473 | < 0.001 | |
| FA(C1)(L) | 0.320 | 0.006 | |
| V(C1) | 0.499 | 0.058 | |
| V(C2) | –0.036 | NS | |
| V(C1-2) | 0.418 | 0.047 | |
| vBMD(C1) | 0.018 | NS | |
| vBMD(C2) | 0.045 | NS | |
| vBMD(C1-2) | 0.084 | NS | |
| FA(C1)(R) versus | LMH(C1)(R) | 0.276 | 0.019 |
| FA(C1)(L) versus | LMH(C1)(L) | 0.167 | 0.015 |
FA, facet angle; L, left; LMH, lateral mass height; NS, not significant; R, right; R-J, Redlund-Johnell; V, volume; vBMD, volumetric bone mineral density; VS, vertical subluxation.
Spearman’s rank correlation coefficient was employed for the analysis of relationships between the parameters.
Statistical significance was set at P < 0.05.
V(C1-2) was significantly correlated with the R-J value and V(C1) had a tendency to correlate positively with the R-J value; however, there was no relationship between V(C2) and the R-J value (Table 3).
There was no significant correlation between vBMDs at the UCS and the R-J value. vBMD(C1) was negatively correlated with left and right FA(C1) [r = −0.468 (P = 0.023) and r = −0.600 (P = 0.038), respectively].
In the present study, there were significant differences in age, duration of RA and BMD(lumbar). However, when we performed multiple regression logistic analysis using the above factors as explanatory variables for VS, we found that age [odds ratio: 1.089 for 1 SD, 95% confidence interval (CI): 1.004–1.183, P = 0.041] was the only factor that contributed to the progression of VS [duration of RA, odds ratio: 1.000 for 1 SD, 95% CI: 0.992–1.007, P = 0.911; BMD(lumbar), odds ratio: 0.665 for 1 SD, 95% CI: 0.006–75.23, P = 0.866].
DISCUSSION
We hypothesized that OP could promote the development of VS, because Neva et al. 15 proposed BMD(hip) to be a risk factor for VS. However, we could not find statistically significant relationships between BMD(spine, hip or both) and the development of VS. To evaluate the relationship between OP and VS progression, it is essential to measure the BMD at the UCS.
To the best of our knowledge, there have been only a few reports on the BMD at the UCS.25, 26 In those reports, BMD levels at only subaxial regions were analyzed using quantitative CT. In the occipitocervical junction, there are many bony and artificial structures (false teeth and implants), which produce halation and make it difficult to perform BMD measurements with high precision and reproducibility. We resolved these issues by using 3D-TBSAS.
Three-dimensional analysis revealed that RA patients had almost the same vBMD as OP patients at the UCS, even though RA patients were significantly younger and had significantly higher BMD(lumbar). Moreover, the volumes at the UCS became smaller with progression of VS. However, vBMDs at the UCS were not significantly correlated with the development of VS. These results were not consistent with our hypothesis, perhaps for the following reasons. First, there is a possibility that vBMD at the UCS might become condensed with progression of VS. Although we could not discern a relationship between the volumes and vBMDs at the UCS (data not shown), we found that FA(C1) became sharper with progression of VS. Additionally, FA(C1) was negatively correlated with vBMD(C1). These findings could support this possibility. Second, there is another possibility that a structural specificity at UCS might affect vBMDs at the UCS. The ratio of cortical to cancellous bone is higher in the UCS than the lumbar spine; therefore, the effects of RA itself or generalized OP might be smaller. Moreover, instabilities at the UCS cause sclerotic changes. These factors might affect the measurements of vBMDs.
Our results indicated that VS could be induced by the collapse of the lateral masses in the UCS. Although many previous reports3, 6, 9, 27, 28, 29, 30 referred to active synovial proliferation at unstable AAJs, these reports did not show how the collapse of the lateral masses progressed. Some reports 21, 28 focused on the AOJ in RA patients found that rheumatoid changes (ankylosing and fusion) at the AOJ may progress into VS. In general, it has been thought that the orientation of the AAJ changes from horizontal to nearly vertical with progression of VS.8 However, the present study showed that the orientation of the AAJ did not significantly change even in VS patients and that FA(C1) became sharper with progression of VS. We considered the following: RA patients with long symptom duration had more destructive changes at the AOJ than those with short symptom duration. If disease activity in RA patients were generally maintained in moderate conditions for long periods, these patients had lower LMH(C1), lower LMH(C2) and sharper FA(C1) than early-stage RA patients. On the other hand, RA patients with high disease activity, such as mutilating RA patients, tend to develop VS when the lateral masses in the UCS collapse rapidly.
The risk factors for VS development was age, RA symptom duration and BMD(lumbar). However, we could not show statistical relationship between OP and VS development. There were several limitations in the present study. First, the present study was an observational study. To investigate the etiology of VS and the relationship between the progression of VS and OP more clearly, a prospective study should be performed. Second, 3D-TBSAS could not calculate vBMD at the UCS in RA patients with severe rheumatoid changes. Since it was able to measure vBMDs at the UCS in early-stage RA, we should recruit more candidates with early-stage RA and follow them prospectively.
In conclusions, VS progressed based on the collapse of the lateral masses at the UCS. The C1 facet angle became more acute with progression of VS. The VS group had rheumatoid changes at the AAJ, AOJ or both, and had more bone defects in the odontoid process than the non-VS group. Three-dimensional analysis revealed a decrease in the volumes at the UCS with the development of VS.
Acknowledgments
Acknowledgments: The authors would like to thank Dr. J. Hashimoto and Prof. H. Yoshikawa of Osaka University for their advice and help in performing this study. The authors would also like to thank Mr. J. Kishimoto and other radiological technologists of Clinical Radiology in Tottori University Hospital for their help in performing this study.
Portions of this work were presented at the 2nd Annual Meeting of Cervical Spine Research Society, Asia Pacific Section in Busan, Republic of Korea, on 28–30 April, 2011, and in poster form at the Eurospine 2010 Annual Meeting in Vienna, Austria on 15–17 September, 2010.
The authors declare no conflict of interest.
References
- 1.Kauppi M, Hakala M. Prevalence of cervical spine subluxations and dislocations in a community-based rheumatoid arthritis population. Scand J Rheumatol. 1994; 23: 133-136 [DOI] [PubMed] [Google Scholar]
- 2.Halla JT, Hardin JG, Vitek J, Alarcón GS. Involvement of the cervical spine in rheumatoid arthritis. Arthritis Rheum. 1989; 32: 652-659 [DOI] [PubMed] [Google Scholar]
- 3.Santavirta S, Hopfner-Hallikainen D, Paukku P, Sandelin J, Konttinen YT. Atlantoaxial facet joint arthritis in the rheumatoid cervical spine. a panoramic zonography study. J Rheumatol. 1988; 15: 217-223 [PubMed] [Google Scholar]
- 4.Santavirta S, Kankaanpää U, Sandelin J, Laasonen E, Konttinen YT, Slätis P. Evaluation of patients with rheumatoid cervical spine. Scand J Rheumatol. 1987; 16: 9-16 [PubMed] [Google Scholar]
- 5.Henderson DR. Vertical atlanto-axial subluxation in rheumatoid arthritis. Rheumatol Rehabil. 1975; 14: 31-38 [DOI] [PubMed] [Google Scholar]
- 6.Eulderink F, Meijers KA. Pathology of the cervical spine in rheumatoid arthritis: a controlled study of 44 spines. J Pathol. 1976; 120: 91-108 [DOI] [PubMed] [Google Scholar]
- 7.Ochi T, Iwase R, Yonemasu K, Matsukawa M, Yoneda M, Yukioka M.Natural course of joint destruction and fluctuation of serum C1q levels in patients with rheumatoid arthritis. Arthritis Rheum. 1988; 31: 37-43 [DOI] [PubMed] [Google Scholar]
- 8.Casey AT, Crockard HA, Geddes JF, Stevens J. Vertical translocation: the enigma of the disappearing atlantodens interval in patients with myelopathy and rheumatoid arthritis. Part I. Clinical, radiological, and neuropathological features.. J Neurosurg. 1997; 87: 856-62 [DOI] [PubMed] [Google Scholar]
- 9.O’Brien MF, Casey AT, Crockard A, Pringle J, Stevens JM. Histology of the craniocervical junction in chronic rheumatoid arthritis: a clinicopathologic analysis of 33 operative cases. Spine. 2002; 27: 2245-2254 [DOI] [PubMed] [Google Scholar]
- 10.Oda T, Fujiwara K, Yonenobu K, Azuma B, Ochi T. Natural course of cervical spine lesions in rheumatoid arthritis. Spine. 1995; 20: 1128-1135 [DOI] [PubMed] [Google Scholar]
- 11.Fujiwara K, Fujimoto M, Owaki H, Kono J, Nakase T, Yonenobu K. Cervical lesions related to the systemic progression in rheumatoid arthritis. Spine. 1998; 23: 2052-2056 [DOI] [PubMed] [Google Scholar]
- 12.Neva MH, Isomäki P, Hannonen P, Kauppi M, Krishnan E, Sokka T. Early and extensive erosiveness in peripheral joints predicts atlantoaxial subluxations in patients with rheumatoid arthritis. Arthritis Rheum. 2003; 48: 1808-1813 [DOI] [PubMed] [Google Scholar]
- 13.Neva MH MH, Kaarela K K, Kauppi M M. Prevalence of radiological changes in the cervical spine--a cross sectional study after 20 years from presentation of rheumatoid arthritis. J Rheumatol. 2000; 27: 90-93 [PubMed] [Google Scholar]
- 14.Zikou AK, Alamanos Y, Argyropoulou MI, Tsifetaki N, Tsampoulas C, Voulgari PV. Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol. 2005; 32: 801-806 [PubMed] [Google Scholar]
- 15.Neva MH, Kotaniemi A, Kaarela K, Lehtinen JT, Belt EA, Kauppi M. Atlantoaxial disorders in rheumatoid arthritis associated with the destruction of peripheral and shoulder joints, and decreased bone mineral density. Clin Exp Rheumatol. 2003; 21: 179- 184 [PubMed] [Google Scholar]
- 16.Winfield J, Cooke D, Brook AS, Corbett M. A prospective study of the radiological changes in the cervical spine in early rheumatoid disease. Ann Rheum Dis. 1981; 40: 109-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Başkan BM, Sivas F, Alemdaroğlu E, Duran S, Ozoran K. Association of bone mineral density and vertebral deformity in patients with rheumatoid arthritis. Rheumatol Int. 2007; 27: 579-584 [DOI] [PubMed] [Google Scholar]
- 18.Ursum J, Britsemmer K, van Schaardenburg D, Lips PT, Dijkmans BA, Lems W. High prevalence of vertebral deformities in elderly patients with early rheumatoid arthritis. Ann Rheum Dis. 2009; 68: 1512-1513 [DOI] [PubMed] [Google Scholar]
- 19.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS.The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988; 31: 315-324 [DOI] [PubMed] [Google Scholar]
- 20.Redlund-Johnell I, Pettersson H. Radiographic measurements of the cranio-vertebral region. Designed for evaluation of abnormalities in rheumatoid arthritis. Acta Radiol Diagn. 1984; 25: 23-28 [DOI] [PubMed] [Google Scholar]
- 21.Iizuka H, Sorimachi Y, Ara T, Nishinome M, Nakajima T, Iizuka Y. Relationship between the morphology of the atlanto-occipital joint and the radiographic results in patients with atlanto-axial subluxation due to rheumatoid arthritis. Eur Spine J. 2008; 17: 826-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lakshmanan P, Jones A, Howes J, Lyons K. CT evaluation of the pattern of odontoid fractures in the elderly--relationship to upper cervical spine osteoarthritis. Eur Spine J. 2005; 14: 78-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azuma Y, Harada Y, Takagi H, Kamimura T, Ohta T, Yamada N. [Micro-focused X-ray computed tomography for three-dimensional analysis of trabecular bone]. Nippon Kotsu Keitai Keisoku Gakkai Zasshi. 2000; 10: 53- 61 Japanese. [Google Scholar]
- 24.Ranawat CS, O’Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979; 61: 1003-1010 [PubMed] [Google Scholar]
- 25.Weishaupt D, Schweitzer ME, DiCuccio MN, Whitley PE. Relationships of cervical, thoracic and lumbar bone mineral density by quantitative CT. J Comput Assist Tomogr. 2001; 25: 146-150 [DOI] [PubMed] [Google Scholar]
- 26.Yoganandan N, Pintar FA, Stemper BD, Baisden JL, Aktay R, Shender BS. Bone mineral density of human female cervical and lumbar spines from quantitative computed tomography. Spine. 2006; 31: 73-76 [DOI] [PubMed] [Google Scholar]
- 27.Zikou AK, Argyropoulou MI, Alamanos Y, Tsifetaki N, Tsampoulas C, Voulgari PV. Magnetic resonance imaging findings of the cervical spine in patients with rheumatoid arthritis. a cross-sectional study. Clin Exp Rheumatol. 2005; 23: 665-670 [PubMed] [Google Scholar]
- 28.Sorimachi Y, Iizuka H, Ara T, Nishinome M, Iizuka Y, Nakajima T. Atlanto-axial joint of atlanto-axial subluxation patients due to rheumatoid arthritis before and after surgery: morphological evaluation using CT reconstruction. Eur Spine J. 2011; 20: 798-803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Czerny C, Grampp S, Henk CB, Neuhold A, Stiskal M, Smolen J. Rheumatoid arthritis of the craniocervical region: assessment and characterization of inflammatory soft tissue proliferations with unenhanced and contrast-enhanced CT. Eur Radiol. 2000; 10: 1416- 1422 [DOI] [PubMed] [Google Scholar]
- 30.Kawaida H, Sakou T, Morizono Y, Yoshikuni N. Magnetic resonance imaging of upper cervical disorders in rheumatoid arthritis. Spine. 1989; 14: 1144- 1148 [DOI] [PubMed] [Google Scholar]