Abstract
Recurrent angina in patients who underwent percutaneous coronary intervention is defined as recurrence of chest pain or chest discomfort. Careful assessment is recommended to differentiate between non-cardiac and cardiac causes. In the case of the latter, recurrent angina occurrence can be related to structural (‘stretch pain’, in-stent restenosis, in-stent thrombosis, incomplete revascularization, progression of coronary atherosclerosis) or functional (coronary micro-vascular dysfunction, epicardial coronary spasm) causes. Even though a complete diagnostic algorithm has not been validated, ECG exercise testing, stress imaging and invasive assessment of coronary blood flow and coronary vaso-motion (i.e. coronary flow reserve, provocation testing for coronary spasm) may be required. When repeated coronary revascularization is not indicated, therapeutic approaches should aim at targeting the underlying mechanism for the patient’s symptoms using a variety of drugs currently available such as beta-blockers, calcium-channel blockers, ivabradine or ranolazine.
Keywords: Recurrent angina, coronary angioplasty
Introduction
In the last decades the number of myocardial revascularization procedures using coronary angioplasty in patients with chronic stable angina (CSA) has continuously increased.1 Despite a lot of innovations in coronary angioplasty techniques, recurrent angina after coronary angioplasty is a frequent problem that many cardiologists in everyday clinical practice have to deal with.2 More than 30% of patients with prior revascularization still report episodes of angina in a three-year follow up.3 The aim of this review is to describe the most common causes of RA after percutaneous coronary intervention (PCI) and to focus on possible diagnostic and therapeutic approaches. According to latest European Society of Cardiology (ESC) guidelines on CSA, revascularization procedures are recommended in the case of symptoms not being controlled by optimal medical treatment.4 However, despite results from the COURAGE trial, supporting the benefits of medical treatment in patients with CSA,5 off-label indications account for many PCI procedures.6 The main advantage of coronary angioplasty compared with medical treatment alone lies in better symptom control.7,8 RA after PCI, although a challenging task for clinicians, represents a severe limitation in quality of life for most patients, proportional to the number of angina episodes per week,9 as well as a frustrating experience for the interventional cardiologist, often synonymous with failed PCI treatment.10,11 In contrast to refractory angina, which is defined as angina due to severe coronary atherosclerosis with evidence of myocardial ischaemia not susceptible to further revascularization,12 this review will focus on recurrent or persistent angina (RA), defined as recurrence of symptoms after PCI.13
Methods
We identified 316 English-language publications through a PubMed search using the keywords ‘recurrent angina’ and ‘coronary angioplasty’ in January 2012. After evaluating these articles, we prepared this review with emphasis on updates on diagnosis and treatment of recurrent angina after coronary angioplasty. We have restricted the citations to, in our view, the most relevant and informative publications.
The bulk of the problem
The prevalence of RA after PCI is high and more than one-half of all patients in community practice had at least one stress test within 24 months of revascularization.14 Data from NHLBI Dynamic Registry, enrolling 1628 patients, mostly affected by CSA and revascularized with PCI, show presence of angina episodes in 26% of subjects at 12-month follow-up.15 In the ARTS trial, angina was still present in 21% of patients one year after PCI, while 42% of patients showed either RA or need of repeat revascularization after five years.16 In the RITA-2 trial, the number of subjects with severe angina (Canadian Cardiovascular Society class >2) was reduced from 60% to 20% by PCI at 12 months, while it was not in the medical treatment group;10,11 at two-year follow up, however, differences were no longer significant. In a large retrospective study from the Mayo Clinic, most of the patients treated with PCI experienced an improvement in episodes of angina, although 30% still reported RA and 12% severe RA:17 drug prescription was substantially not impacted by PCI.
Aetiology of recurrent angina (Table 1)
Table 1.
Recurrent angina: causes.
| Recurrent angina after PCI: causes |
|---|
Structural
|
Functional
|
PCI: percutaneous coronary intervention
First of all, a careful rule-out of several non-cardiac causes of chest pain (gastro-intestinal, lung, osteo-articular, herpes zoster, anxiety) is necessary to get to a correct diagnosis of RA. Cardiac causes of RA are either linked to structural causes (‘stretch pain’, in-stent restenosis, in-stent thrombosis, incomplete revascularization, progression of coronary atherosclerosis) or functional causes (microvascular dysfunction, epicardial coronary spasm), or a combination of both.
‘Stretch-pain’ is chest pain reported early after PCI, mainly caused by coronary stenting and irritation of nerves in the coronary adventitia; it is usually not associated to ECG anomalies and cardiac troponin elevation, although it accounts for several unnecessary coronary angiographic controls. This type of non-ischaemic chest pain develops in almost half of all patients undergoing stent implantation and seems to be related to vessel overexpansion caused by the stent in the diseased vessel segment.18
In-stent restenosis after PCI is a composite process characterized by intimal hyperplasia responsible for coronary lumen reduction and effort angina.19 In-stent restenosis has been the Achilles heel of interventional cardiology for a long time, even though its occurrence has been substantially reduced by the use of drug eluting stents (DESs).20,21 According to a meta-analysis, the use of DESs was able to reduce the occurrence of target vessel revascularization in comparison with bare metal stents (BMSs) by 70%. In-stent restenosis usually appears within six months after PCI, with higher observable rates between the fourth and the sixth month.22 Angiographic restenosis is defined as evidence of >50% narrowing after PCI and is associated with angina or evidence of myocardial ischaemia at the provocative tests in 60% of cases.23 Different patterns of restenosis have been reported according to the different types of stents utilized: focal restenosis (mainly with sirolimus eluting stent) often requires plain old balloon angioplasty (POBA), whereas diffuse and occlusive restenosis (mainly with paclitaxel eluting stent) is often treated by repeat coronary stenting, or, when this is not feasible, coronary artery bypass graft (CABG).24
Despite the advantages of DESs over BMSs, the use of DESs is burdened by a higher rate of sub-acute and late thrombosis: cytostatic drugs eluted by DESs and the polymers ‘storing’ them inhibit neo-intimal proliferation and consequently delay the coronary endothelization after stent implantation.25,26
In-stent thrombosis is defined as acute (within 24 hours), sub-acute (>24 hours <30 days), late (>30 days <12 months) and very late (>12 months).27 The presence of an angiographic confirmation of stent thrombosis (the presence of a thrombus that originates in the stent or in the segment 5mm proximal or distal to the stent) is associated with the presence of at least one of the following criteria within a 48-hour window: acute onset of ischaemic symptoms at rest, new ischaemic electrocardiographic changes that suggest acute ischaemia or typical rise and fall in cardiac biomarkers; or in the presence of a histopathological confirmation of stent thrombosis (evidence of recent thrombus within the stent determined at autopsy or via examination of tissue retrieved following thrombectomy). Clinical variables (pro-thrombotic conditions, diabetes, renal failure, impaired left ventricular systolic function) but also lesion-related (length, diameter, type of lesion), and procedural variables (coronary dissection, stent under-deployment, malapposition, plaque prolapse) were reported as predictors of in-stent thrombosis.28 Incidence of sub-acute and late thrombosis after DES stenting was respectively 1.1% and 0.4%.25 It is noteworthy, however, to underline that in all cases in-stent thrombosis occurred with aspirin mono-therapy, thus supporting the need for a dual anti-platelet treatment (clopidogrel + aspirin) in all patients receiving a DES for at least 12 months.29 Iakovou et al. demonstrated a marked increased risk of in-stent thrombosis after early double anti-platelet therapy stop,28 in diabetics or renal failure patients, after bifurcation stenting.23,26
Other cases of RA are due to incomplete revascularization, as observed in patients with multi-vessel coronary disease treated with PCI according to the SYNTAX trial results,30 in this case, RA occurring within 30 days after PCI.19,29 Data from the ARTS study show that revascularization was incomplete in 30% of patients after PCI.31 Patients with incomplete revascularization had higher occurrence at 12 months of the combined end-point new coronary events and revascularization (30.6% vs. 23.4%), with a five-fold higher need for CABG (10.0 vs. 2.0%) when compared with complete revascularization.33
In spite of convincing results yielded by DESs regarding in-stent restenosis, RA due to progression of coronary atherosclerosis in coronary segments different from those treated with PCI is still very frequent, especially in high risk patients such as diabetics.32 According to some studies, RA due to progression of coronary atherosclerosis usually occurs later (one year) than in-stent restenosis.29 In the BARI trial, the use of DESs significantly lowered rates of restenosis in diabetics with multi-vessel coronary artery disease (CAD), but progression of coronary disease accounted for up to 57% of cases of repeat revascularization.33
Functional causes of RA can be due to (a) impaired vasodilatation and/or (b) enhanced vasoconstriction (epicardial coronary spasm, microvascular dysfunction, coronary spasm at stent edges). Inappropriate constriction of small coronary vessels is a possible cause of chest pain and a positive exercise test early after successful coronary angioplasty.34 Coronary vasoconstriction is exaggerated at distal segments in DES-implanted vessels compared with non-stented vessel segments and stent length was longer in the acetylcholine provocation test positive group in a study by Ito et al.35 Stent implantation may induce distal coronary endothelial dysfunction.36 Acetylcholine test may provoke significant vaso-constrictive responses in the distal but not in the proximal segments of both the stented and the contralateral vessels, which are significantly correlated and completely reverted by nitroglycerine. Impaired vasodilatation and enhanced vasoconstriction can be assessed by intracoronary flow reserve (CFR) measurements and/or intracoronary provocation testing for coronary artery spasm using acetylcholine/ergonovine.
Sometimes, stenting of sub-critical coronary stenosis may be responsible for an increased incidence of RA at follow-up: the DEFER trial showed that PCI on a coronary stenosis not haemodynamically significant (fractional flow reserve (FFR) >0.75%) does not improve either prognosis or symptoms.37 Rates of patients still reporting angina at five-year follow-up after PCI were similar to those in subjects left on medical treatment. In the FAME trial, an adjunctive functional assessment of coronary stenoses already evaluated by angiography was even more crucial in multi-vessel coronary disease, when the real ‘culprit’ lesion is not easy to identify.38
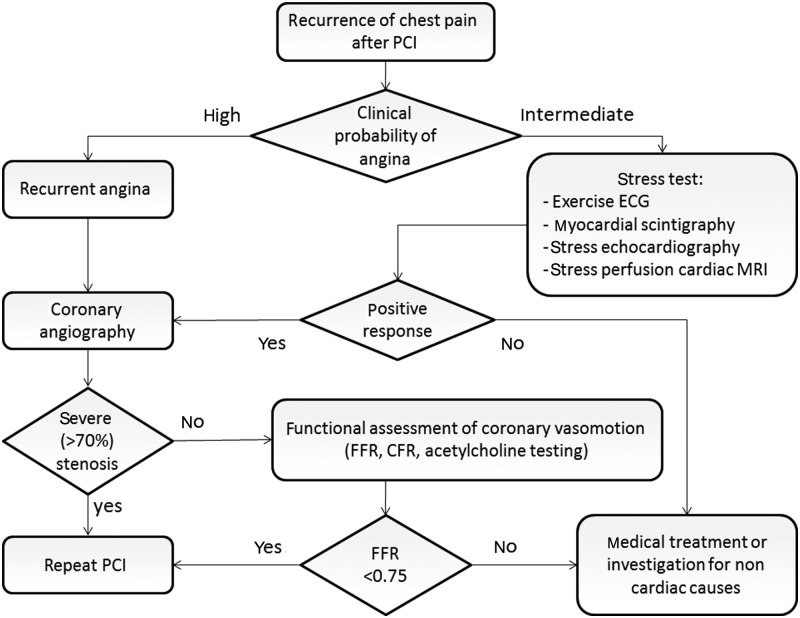
Diagnostic flow-chart (Figure 1)
Figure 1.
Recurrent angina: diagnostic and therapeutic strategies.
PCI: percutaneous coronary intervention; MRI: magnetic resonance imaging; FFR: fractional flow reserve; CFR: intracoronary flow reserve
A rationale diagnostic approach to RA should start from a careful evaluation of chest-pain characteristics, a complete risk stratification and an accurate analysis of prior PCI procedures. In case of suspected non-cardiac symptoms, an exercise stress test should be performed in order to discriminate ‘cardiac’ from ‘non-cardiac’ chest pain and for risk stratification. Negative exercise stress test results should lead towards investigations for ‘non-cardiac’ chest pain (e.g. gastroscopy, chest X-ray), positive findings to coronary angiography. After results from the ROSETTA trial, it is still unknown which is the best type of exercise stress test after PCI and when it should be performed because it has been shown that prognosis did not change whether an exercise stress test was performed routinely after PCI or only after recurrence of symptoms.39-41 Patients complaining of RA with characteristics similar to those prior to PCI may either undergo exercise stress testing or may directly be referred to coronary angiography.42 The later the recurrence of angina, the more probable is a progression of coronary disease rather than in-stent restenosis.43 A careful interview should assess the patient’s compliance to dual anti-platelet treatment as the risk of in-stent thrombosis is higher in patients not receiving both clopidogrel and aspirin, although cases of very late in-stent thrombosis still occur even in patients still on dual anti-platelet treatment.29 Repeat coronary angiography should be performed when typical symptoms occur in patients with higher cardiovascular risk profile (worsening angina, arrhythmias, heart failure, diabetes, renal failure, poor compliance to drug therapy), prior high-risk PCI (left main, bifurcations, chronic total occlusion, ostial lesions, ‘full metal jacket’ stenting, impaired left ventricular function) or incomplete revascularization.44,45
Exercise stress test usefulness in identifying areas of myocardial ischaemia, however, is often limited by concomitant presence of microvascular dysfunction and collateral circulation, which may lead to either false positive or false negative results.46 AHA/ACC guidelines recommend (class I, evidence C) perfusion scintigraphy or exercise echocardiography for the assessment of patients with prior revascularization who presented with new onset of symptoms;47 ESC guidelines on CSA recommend coronary angiography (class I, evidence C) and in the case of RA or high risk of restenosis, when prior PCI may significantly impact prognosis (class II, evidence C).48 Despite good prognostic power in predicting adverse events in ischaemic heart disease,49 exercise ECG yields a poor sensitivity (41%)50 and accuracy (62%)51 when performed after PCI in identifying subjects at risk for restenosis. However, the decision for repeat revascularization needs both the evidence of myocardial ischaemia and the exact identification of the ischaemic area, especially in the case of multi-vessel coronary disease; single photon emission computed tomography (SPECT) and stress echocardiography may therefore better meet these needs.47
Also adenosine stress cardiac magnetic resonance (CMR) may allow accurate detection of non-culprit territory stenosis in patients successfully treated with primary-PCI post ST-segment elevation myocardial infarction (STEMI).52 A combined CMR protocol for the assessment of myocardial perfusion and late gadolinium enhancement is feasible for the detection of relevant coronary vessel stenosis even in patients who previously were treated by PCI or CABG in a routine clinical setting.53
In the case of a moderate stenosis on coronary angiography (50–70%), FFR measurements can be helpful to decide whether or not a stent implantation is justified. In the absence of flow-limiting stenoses, intracoronary assessment of coronary vaso-motion using coronary flow reserve and provocation testing with acetylcholine or ergonovine can reveal functional causes for RA.54
Abnormal coronary vasomotion (i.e. epicardial and microvascular) is defined as a reduced vasodilatation with exercise or a reduced CFR and/or vasospasm at rest.55 During intracoronary acetylcholine provocation testing, incremental doses of acetylcholine 2, 20, 100 and 200 µg are administered over a period of 3 min each into the left coronary artery via the angiographic catheter; in patients who do not develop symptoms or ischaemic ECG changes, acetylcholine is subsequently injected into the right coronary artery (80 µg acetylcholine over 3 min). The acetylcholine test is positive when the visual findings at coronary angiography and the quantitative analysis confirm a vasoconstriction of ≥75% compared with the relaxed state after intracoronary administration of glyceroltrinitrate together with a reproduction of the patient’s symptoms.
CFR describes the amount of additional blood flow that can be supplied to the heart above baseline blood flow.56 Several tools have already measured coronary flow CFR, including coronary sinus thermodilution, cardiac nuclear imaging, inert gas washout method and intracoronary Doppler flow wire.57 However, several of these methods, although helpful for research, have limited clinical applications, being complex, time-consuming, expensive, not easily available and invasive.58
Doppler guidewires make it possible to calculate coronary flow velocity reserve (CFVR), which is the ratio between intra-coronary mean velocity under baseline conditions and after pharmacological induction of maximum hyperaemia.59 In humans, a cut-off value of <2.0 was found to define a significant stenosis.60
CFR may also be measured non-invasively by the combination of coronary flow assessment by Doppler and vasodilator stress.61 With transoesophageal or transthoracic echocardiography, the coronary blood flow velocity profile recorded with pulsed wave Doppler may estimate CFR: coronary flow velocity by Doppler assessment appears to be bi-phasic, with a lower peak during systole and a higher peak during diastole. The coronary flow velocity variation between the baseline and peak effect of a coronary vasodilator allows a coronary flow reserve index to be derived. Peak diastolic flow is the simplest parameter to measure, in addition to being the most reproducible and the one with the closest correlation with coronary perfusion measured by SPECT.
The availability of contrast agents also improved the signal-to-noise ratio, thereby increasing the technique feasibility. The cut-off value of 2 of CFR for detecting significant epicardial coronary stenosis or to predict ischaemia in the underlying territory has been demonstrated in various studies. When CFR is <2 during follow-up after angioplasty, the restenosis in the LAD is detected with high sensitivity and specificity.61,62
CFR can also be performed in patients without in-stent restenosis in order to assess the function of the coronary microcirculation: coronary microvascular reactivity to adenosine may predict adverse outcome in subjects with suspected ischaemia.63
The procedure utilized for the estimation of CFR by radionuclide imaging is based on the consideration that technetium (Tc)-99m labelled tracers are taken up by myocardium according to blood flow.64 A good correlation between CFR values estimated by SPECT imaging and those measured by intravascular Doppler ultrasound in patients undergoing percutaneous coronary intervention has been demonstrated.65
Cardiac positron emission tomography (PET) with oxygen-15 water is the non-invasive gold standard for obtaining quantitative regional blood flows.66 The measurement of CFR has also been performed by means of PET with other tracers, using either generator-produced Rb-82 or cyclotron-produced N-13 ammonia.67
More recently, several studies have shown the usefulness of qualitative assessment of cardiac magnetic resonance imaging (CMRI) perfusion for the functional assessment of CAD.68 CMRI is able to distinguish haemodynamically relevant from non-relevant coronary lesions with a high sensitivity and specificity and may therefore contribute to clinical decision-making. ROC analysis gave a cut-off value of 1.5 for optimal discrimination between haemodynamically significant and non-significant lesions.
Although it may be helpful to distinguish between the different possible causes for RA in patients after PCI it should be noted that in many patients an overlap of several causes will exist. For example, micro-vascular dysfunction may be related to functional as well as structural injuries consequent to micro-embolization, ischaemia or reperfusion damage.69,70 Successful restoration of epicardial coronary artery patency after prolonged occlusion might result in microvascular obstruction (MVO) and is observed experimentally as well as clinically. In addition to these ischaemia-reperfusion-related events (swollen myocytes, voluminous endothelial cells, both occluding capillaries, infiltration and activation of neutrophils and platelets, deposition of fibrin), coronary micro-embolization of atherosclerotic debris after PCI is responsible for a substantial part of clinically observed MVO. Several techniques (coronary angiography, myocardial contrast echocardiography, cardiovascular magnetic resonance imaging, electrocardiography) measuring slightly different biological and functional parameters are used clinically and experimentally. Currently there is no consensus as to how and when MVO should be evaluated after acute MI and PCI, respectively.71
Non-invasive diagnostic tools for the evaluation of coronary stenosis such as multi-slice coronary computed tomography (MSCCT) and MRI have also been validated.72 Some limitations remain with respect to accurate definition of in-stent restenosis and costs.73 Metal induced artefacts (blooming effect) may significantly compromise the diagnosis of a flow-limiting in-stent hyperplasia, while a total occlusion is usually well identified and defined. MRI could possibly be useful in combined evaluation of both coronary anatomy and flow.74 Contrast echocardiography is a cheap, non-invasive, low-cost tool for the evaluation of myocardial perfusion, although it provides operator-dependent results not easy to standardize.75 PET could be the benchmark for functional and perfusional assessment of myocardium, but costs are not negligible.76
Taken together, coronary angiography still represents the gold-standard for the diagnosis of in-stent restenosis. Functional assessment of coronary vasomotion can provide important information on cardiac mechanisms for RA especially in patients without flow-limiting epicardial stenosis.48
Recurrent angina: treatment (Figure 1)
Treatment of RA after PCI should be based on a careful evaluation of the underlying mechanism.
Current guidelines do not distinguish between CSA and RA. Therefore, theoretically, the treatment should be the same.48 In the case of coronary atherosclerosis, it should be noted that PCI is not the final solution to the problem but the beginning of a new way of life for the patients, characterized by a life-long treatment and radical changes in life-style. Independent of the revascularization procedure, cardio-vascular risk factors (hypertension, dyslipidaemia, diabetes, obesity) should be thoroughly managed in order to slow the progression of coronary atherosclerosis.77
In the case of non-ischaemic causes of chest pain (gastro-intestinal, lung, osteo-articular, herpes zoster, anxiety) it is necessary to get to a correct diagnosis. Gastro-intestinal pain may be relieved by anti-proton pump administration, osteo-articular by non steroidal anti-inflammatory drugs, anxiety by benzodiazepines.
Structural causes of RA (restenosis, in-stent thrombosis, incomplete revascularization, progression of coronary atherosclerosis) usually need to be managed with repeat angiography; repeat PCI may be further required when indications for revascularization occur.
‘Stretch pain’ early after PCI may be managed with the administration of analgesic or opioids.
Functional causes of RA (microvascular dysfunction, epicardial coronary spasm) usually need an upgrade in pharmacological treatment. Medical treatment of RA (Table 2) is currently based on the same drugs prescribed for CSA: beta-blockers, calcium-channel blockers, long lasting nitrates. In a study enrolling 4840 patients after PCI, repeat revascularization amounted to 12% at six months.78 Lower rates of the end-point were, however, detectable in the case of beta-blocker administration (10% vs. 13.5%, p<0.01, relative risk 0.76). Some patients need treatment with drugs at high doses,79 others a combination with calcium-channel blockers, especially when coronary spasm is suspected.80
Table 2.
Recurrent angina: pharmacological treatment options.
| Recurrent angina: pharmacological treatment options |
|---|
Established
|
New
|
ACE-inhibitors and statins should be part of pharmacological treatment in all patients with CAD to improve endothelial dysfunction and improve vascular remodelling. Statin therapy benefit has been shown by several trials,81 with possible reduction in coronary plaque volumes.82 Intensive treatment with aspirin, clopidogrel, statins, ACE-inhibitors, angiotensin receptor blockers, beta-blockers, calcium-channel blockers and nitrates may yield ‘encouraging’ results, but very high compliance levels obtained in the COURAGE trial (90–96% at five years) are not easy to obtain in everyday clinical practice5. Medical treatment, however, should not be discontinued even after successful revascularization with PCI.
Moreover, several new anti-ischaemic drugs are nowadays available for the treatment of RA added to conventional therapy when it is ineffective in controlling symptoms or used in isolation when beta-blockers and/or calcium-channel blockers are contraindicated or not tolerated.
High heart rate is a cardiovascular risk factor in any population of patients studied (general population, hypertensive, diabetics, in acute coronary syndrome, male and female). Heart rate is known as one of the main determinants in oxygen consumption83 and is involved in coronary plaque instabilization.84 Promising results were obtained with ivabradine, a selective inhibitor of channel (If) highly expressed in the sino-atrial node, on which it has a dampening effect. Pure heart rate reduction with ivabradine was able to reduce ischaemic burden, episodes of angina and cardiac events without any haemodynamic effect and negative inotropism, as shown in the BEAUTIFUL and ASSOCIATE trials.85,86
Within four months of treatment with ivabradine, heart rate was reduced by an average 12 beats/min, angina attacks from 2.4 to 0.4 per week, consumption of short-acting nitrates from 3.3 to 0.6 units per week.87 Ivabradine produces dose-dependent improvements in exercise tolerance and time to development of ischaemia during exercise.88 In the INITIATIVE trial, ivabradine was as effective as atenolol in patients with stable angina.89 In patients with stable angina, ivabradine has comparable efficacy to amlodipine in improving exercise tolerance, a superior effect on the reduction of rate-pressure product (a surrogate marker of myocardial oxygen consumption) and similar safety.90
Trimetazidine, an inhibitor of the fatty acid oxidation enzyme, 3-ketoacyl coenzyme A thiolase, reduces the symptoms of demand-induced ischaemia, shifting oxidation of free fatty acids, which is energy-consuming compared with glucose oxidation, towards glucose oxidation and better use of the energy supply (TRIMPOL II study).91
Ranolazine, an inhibitor of late INa current, reduces calcium uptake indirectly via the sodium/calcium exchanger, preserves ionic homeostasis and reverses ischaemia-induced left ventricular dysfunction.92 Ranolazine was shown to increase the ischaemic threshold and to reduce occurrence of angina and the use of nitrates (CARISA, ERICA trials93,94), lowering by 22% episodes of recurrent ischaemia in the sub-group of patients with CSA (MERLIN-TIMI 36 trial95). Ranolazine therapy prolonged exercise duration and decreased exercise-induced ischaemia and angina with quantitative effects equal to or greater than those obtained with atenolol.96 Unlike atenolol, the anti-ischaemic and anti-anginal effects of ranolazine occurred without decreases in blood pressure, heart rate or rate-pressure product. Among patients with a history of angina before their ACS event (54% of the study MERLIN-TIMI 36 trial cohort), there was a significant and sustained beneficial effect of ranolazine relative to placebo across the QOL and disease-specific health status measures – including angina frequency, perceived burden of disease, dyspnoea and overall treatment satisfaction.97
Other anti-ischaemic effects were shown with nicorandil, which induces ischaemic pre-conditioning acting on ATP-sensitive potassium channels98 (IONA trial99).
Physical training should also be encouraged since it may be useful in improving exercise tolerance and prognosis and in reducing hospitalization for RA and costs, even when compared with PCI in subjects with mild coronary stenosis and CSA.100
However, there is no standardized protocol for diagnosis and treatment of RA. Clinical trial results are often biased by heterogeneity of inclusion criteria. Patients with mild residual coronary stenosis and effort angina are sometimes enrolled with patients with RA; the former are often characterized by microvascular dysfunction (cardiac syndrome X),101 while the latter have a poorer prognosis and a worse quality of life.102 Repeat revascularization in RA should, however, be based on a careful examination of coronary anatomy, even in comparison with prior coronary angiography results, in order to identify a possible ‘culprit lesion’ susceptible of interventional treatment. When angiographic coronary anatomy is not sufficient to support repeat revascularization, quantitative coronary analysis, intra-coronary ultra-sound (IVUS) or FFR may be required.48
When repeat PCI is indicated, DES stenting should be the treatment of choice;103 POBA, bare metal stenting104 and brachy-therapy105 yielded sub-optimal results. PCI in CABG patients with RA is even more challenging, because of more severe and diffuse coronary atherosclerosis, older age of the patients and degenerative characteristics of venous graft disease.106 PCI on native coronary vessels could be a feasible strategy; when graft PCI is required, stenting with distal filter protection devices (filter-wire) may be helpful in reducing the rate of occurrence of distal embolization.107,108 The use of DESs reduces the rates of target lesion revascularization,109 but most adverse events at one year are related to progression of coronary plaques not subcritical (<50%) at the previous PCI.110
Treatment of refractory angina should aim at improving the patient’s symptoms. When maximum pharmacological treatment is in place but symptoms are still not controlled, several non-pharmacological interventions (external counter-pulsation, trans-myocardial laser revascularization, spinal cord stimulation, gene therapy) are available,12,111 most of them in specialized centres only.
Prognosis
Prognosis of RA after PCI substantially depends on underlying causes.
‘Stretch pain’ after PCI was not associated with the incidence of significant adverse events during short-term follow up.18
Angiographic in-stent restenosis accounts for a 20–30% target vessel revascularization at one year, and is associated with increased morbidity and mortality.112 In a retrospective study on patients with in-stent restenosis who did not undergo PCI and/or bypass surgery and were maintained on medical treatment alone, at mean 33-month follow-up, only 3% of patients died, none developed MI, while 9% had target lesion revascularization only.113
Ten to 30% of patients presenting with in-stent thrombosis die in hospital, although in-stent thrombosis can also lead to unexplained sudden deaths; non-fatal acute MI, however, is the most frequent clinical presentation of stent thrombosis (70–80% of cases).26,114,115 Subjects with in-stent thrombosis present an increased risk of recurrent stent thrombosis.116
In a cohort of more than 500 patients who underwent repeat coronary angiography for recurrence of chest pain after successful coronary angioplasty, 44% were classified as having restenosis, 13% incomplete revascularization, 20% new significant coronary artery lesions due to coronary disease progression and 23% no significant disease.117 When chest pain recurred within four weeks of angioplasty, 70% of patients had either incomplete revascularization or no significant coronary artery stenosis; when it recurred between four and 24 weeks of angioplasty, restenosis was the most common finding (71%), and when it recurred more than 24 weeks after angioplasty, new disease was the most common finding, occurring in 53% of patients. At repeat angiography, 61% of vessels that had had angioplasty and 49% that had not had angioplasty had new lesions. The incidence of new lesion development is higher in the vessels that have instrumented angioplasty.
Evidence from the Bypass Angioplasty Revascularization Investigation (BARI) trial shows myocardial jeopardy falls following initial revascularization with PCI from 60% to 17%, rebounding at five years to 25%.118 However, myocardial jeopardy at five years is independently associated with late angina. Increased myocardial jeopardy from entry to five-year angiogram occurs in 42% of patients. Among the increases in myocardial jeopardy, two-thirds occurred in previously untreated arteries. The authors conclude that native coronary disease progression occurs more often than failed revascularization in both PCI- and CABG-treated patients as a cause of jeopardized myocardium and angina recurrence.
In-hospital complications are insignificantly greater in incompletely revascularized patients compared with completely vascularized patients (mortality 3% vs. 1%, MI 11% vs. 4%, and emergency surgery 5% vs. 0%).119 After one year of follow-up, incompletely revascularized patients had similar outcomes (mortality 6% vs. 3%, MI 13% vs. 7%, CABG 18% vs. 15%, and repeat PCI 19% vs. 31%). Significantly fewer adverse events (death, MI or CABG) occur in the functionally adequate group than in the functionally inadequate group (27% vs. 6%). Incompletely revascularized patients have a favourable one-year outcome and patients with incomplete but functionally adequate revascularization have long-term results comparable with those of patients with complete revascularization.
Over a mean follow-up period of 26 months, the probability of event-free survival was significantly lower for incompletely revascularized patients only with respect to the need for coronary artery surgery and occurrence of angina.120 There were no significant differences in either the incidence of death, MI or the need for repeat angioplasty.
On the other hand, other studies reveal that there are fewer event-free patients in the cohort of incompletely revascularized multivessel disease patients (55%) when compared with the cohort of those who were completely revascularized (84%).121 This difference was caused by more infarctions and bypass operations in the multivessel disease, incomplete revascularization group. These results suggest that completeness of revascularization in multivessel disease patients is an important prognostic variable.
Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome;122 microvascular dysfunction predicts left ventricular remodelling and long-term clinical outcome after primary coronary angioplasty.123
In patients with inappropriate constriction of small coronary vessels after successful coronary angioplasty, no angina, ischaemic ST segment changes, occlusive or subocclusive spasm occurred.34 However, in a study on subjects with ST-elevation MI who had undergone a stent implantation and a provocation test for coronary spasm by intracoronary injection of acetylcholine two to five weeks after the attack, coronary spasm was provoked with a high frequency in both the infarct related arteries and non-infarct related arteries after stent.124 Calcium-channel blockers may be useful to improve the prognosis in patients with acute MI after stent implantation by suppressing coronary spasm. In patients with normal coronary angiogram, however, abnormal vasoreactivity of epicardial coronary arteries in response to sympathetic stimulation is associated with the risk of developing cardiovascular events.125
Conclusions
RA in patients after PCI is a challenging task for the clinical cardiologist. Careful assessment should aim at identifying the underlying mechanism. When repeat PCI is not indicated, a variety of drugs are currently available for targeted treatment and symptom control.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: None declared.
References
- 1. Ko DT, Tu JV, Samadashvili Z, et al. Temporal trends in the use of percutaneous coronary intervention and coronary artery bypass surgery in New York State and Ontario. Circulation 2010; 121: 2635–2644 [DOI] [PubMed] [Google Scholar]
- 2. Abrams J. Chronic stable angina. N Engl J Med 2005; 352: 2524–2552 [DOI] [PubMed] [Google Scholar]
- 3. Pocock SJ, Henderson RA, Seed P, et al. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation 1996; 94: 135–142 [DOI] [PubMed] [Google Scholar]
- 4. Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2010; 31: 2501–2555 [DOI] [PubMed] [Google Scholar]
- 5. Boden WE, O’rourke RA, Teo KK, et al. ; COURAGE trial coprincipal investigators and study coordinators. Design and rationale of the Clinical Outcomes Utilizing Revascularization and Aggressive DruG Evaluation (COURAGE trial). Am Heart J 2006; 151: 1173–1179 [DOI] [PubMed] [Google Scholar]
- 6. Ramsdale DR, Rao A, Asghar O, et al. Late outcomes after drug-eluting stent implantation in ‘real-world’ clinical practice. J Invasive Cardiol 2008; 20: 493–500 [PubMed] [Google Scholar]
- 7. Kirwan BA, Lubsen J, Poole-Wilson PA; ACTION investigators Treatment of angina pectoris: Associations with symptom severity. Int J Cardiol 2005; 98: 299–306 [DOI] [PubMed] [Google Scholar]
- 8. Weintraub WS, Spertus JA, Kolm P, et al. ; Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008; 359: 677–687 [DOI] [PubMed] [Google Scholar]
- 9. Pepine CJ, Abrams J, Marks RG, et al. ; TIDES investigators. Characteristics of a contemporary population with angina pectoris. Am J Cardiol 1994; 74: 226–231 [DOI] [PubMed] [Google Scholar]
- 10. RITA-2 trial participants Coronary angioplasty versus medical therapy for angina: The second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet 1997; 350: 461–468 [PubMed] [Google Scholar]
- 11. Henderson RA, Pocock SJ, Clayton TC, et al. ; for the Second Randomised Intervention Treatment of Angina (RITA-2) trial participants. Seven-year outcome in the RITA-2 trial: Coronary angioplasty versus medical therapy. J Am Coll Cardiol 2003; 42: 1161–1170 [DOI] [PubMed] [Google Scholar]
- 12. Kim MC, Kini A, Sharma SK. Refractory angina pectoris: Mechanisms and therapeutic options. J Am Coll Cardiol 2002; 39: 923–934 [DOI] [PubMed] [Google Scholar]
- 13. Lemos PA, Hoye A, Serruys PW. Recurrent angina after revascularization: an emerging problem for the clinician. Coron Artery Dis 2004; 15(Suppl. 1): S11–S15 [PubMed] [Google Scholar]
- 14. Shah BR, Cowper PA, O’Brien SM, et al. Patterns of cardiac stress testing after revascularization in community practice. J Am Coll Cardiol 2010; 56: 1328–1334 [DOI] [PubMed] [Google Scholar]
- 15. Holubkov R, Laskey WK, Haviland A, et al. ; NHLBI Dynamic Registry. Registry Investigators. Angina one year after percutaneous coronary intervention: A report from the NHLBI Dynamic Registry. Am Heart J 2002; 144: 826–833 [DOI] [PubMed] [Google Scholar]
- 16. Serruys PW, Unger F, Sousa JE, et al. ; Arterial Revascularization Therapies Study Group. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med 2001; 344: 1117–1124 [DOI] [PubMed] [Google Scholar]
- 17. Eisenberg MJ, Okrainec K, Lefkovits J, et al. ; for the ROSETTA Investigators. Medical therapy in patients undergoing percutaneous coronary intervention: Results from the ROSETTA registry. Can J Cardiol 2003; 19: 1009–1015 [PubMed] [Google Scholar]
- 18. Jeremias A, Kutscher S, Haude M, et al. Nonischemic chest pain induced by coronary interventions: A prospective study comparing coronary angioplasty and stent implantation. Circulation 1998; 98: 2656–2658 [DOI] [PubMed] [Google Scholar]
- 19. Joelson JM, Most AS, Williams DO. Angiographic findings when chest pain recurs after successful percutaneous transluminal coronary angioplasty. Am J Cardiol 1987; 60: 792–795 [DOI] [PubMed] [Google Scholar]
- 20. Al Suwaidi J, Holmes DR, Salam AM, et al. Impact of coronary artery stents on mortality and non-fatal myocardial infarction: Meta-analysis of randomized trial comparing a strategy of routine stenting with that of balloon angioplasty. Am Heart J 2004; 147: 815–822 [DOI] [PubMed] [Google Scholar]
- 21. Indolfi C, Pavia M, Angelillo IF. Drug-eluting stents versus bare metal stents in percutaneous coronary interventions (a meta-analysis). Am J Cardiol 2005; 95: 1146–1152 [DOI] [PubMed] [Google Scholar]
- 22. Holmes DR., Jr. In-stent restenosis. Rev Cardiovasc Med 2001; 2: 115-119 [PubMed] [Google Scholar]
- 23. Corbett SJ, Cosgrave J, Melzi G, et al. Pattern of restenosis after drug-eluting stent implantation: Insights from a contemporary and comparative analysis of sirolimus and paclitaxel-eluting. Eur Heart J 2006; 27: 2330–2337 [DOI] [PubMed] [Google Scholar]
- 24. Cosgrave J, Melzi G, Biondi-Zoccai GGL, et al. Drug-eluting stent restenosis: The pattern predicts the outcome. J Am Coll Cardiol 2006; 47: 2399–2407 [DOI] [PubMed] [Google Scholar]
- 25. Ong ATL, McFadden EP, Regar E, et al. Late angiographic stent thrombosis (LAST events with drug eluting stents). J Am Coll Cardiol 2005; 45: 2088–2093 [DOI] [PubMed] [Google Scholar]
- 26. Ong ATL, Hoye A, Aoki J, et al. Thirty-day incidence and six-month clinical outcome of thrombotic stent occlusion after bare-metal, sirolimus, or paclitaxel stent implantation. J Am Coll Cardiol 2005; 45: 947–953 [DOI] [PubMed] [Google Scholar]
- 27. Lemesle G, Delhaye C, Bonello L, et al. Stent thrombosis in 2008: Definition, predictors, prognosis and treatment. Arch Cardiovasc Dis 2008; 101: 769–767 [DOI] [PubMed] [Google Scholar]
- 28. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stent. JAMA 2005; 293: 2126–2130 [DOI] [PubMed] [Google Scholar]
- 29. Joner M, Finn AW, Farb A, et al. Pathology of drug-eluting stents in humans. Delayed healing and late thrombotic risk. J Am Coll Cardiol 2006; 48: 193–202 [DOI] [PubMed] [Google Scholar]
- 30. Serruys PW, Morice MC, Kappetein AP, et al. ; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360: 961–972 [DOI] [PubMed] [Google Scholar]
- 31. Van den Brand MJ, Rensing BJ, Morel MA, et al. ; on behalf of the ARTS Investigators. The effect of the completeness of revascularization on event-free survival at one year in the ARTS trial. J Am Coll Cardiol 2002; 39: 559–564 [DOI] [PubMed] [Google Scholar]
- 32. Loutfi M, Mulvihill NT, Boccalatte M, et al. Impact of restenosis and disease progression on clinical outcome after multivessel stenting in diabetic patients. Catheter Cardiovasc Interv 2003; 58: 451–454 [DOI] [PubMed] [Google Scholar]
- 33. The BARI Investigators Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med 1996; 335: 217–225 [DOI] [PubMed] [Google Scholar]
- 34. el-Tamimi H, Davies GJ, Sritara P, et al. Inappropriate constriction of small coronary vessels as a possible cause of a positive exercise test early after successful coronary angioplasty. Circulation 1991; 84: 2307–2312 [DOI] [PubMed] [Google Scholar]
- 35. Ito S, Nakasuka K, Morimoto K, et al. Angiographic and clinical characteristics of patients with acetylcholine-induced coronary vasospasm on follow-up coronary angiography following drug-eluting stent implantation. J Invasive Cardiol 2011; 23: 57–64 [PubMed] [Google Scholar]
- 36. Monnink SH, Tio RA, Veeger NJ, et al. Exercise-induced ischemia after successful percutaneous coronary intervention is related to distal coronary endothelial dysfunction. J Invest Med 2003; 51: 221–226 [DOI] [PubMed] [Google Scholar]
- 37. Pijls NH, Van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007; 49: 2105–2111 [DOI] [PubMed] [Google Scholar]
- 38. Tonino PA, De Bruyne B, Pijls NH, et al. , for the FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224 [DOI] [PubMed] [Google Scholar]
- 39. Eisenberg MJ, Wou K, Nguyen H, et al. Lack of benefit for routine functional testing early after coronary artery bypass graft surgery: results from the ROSETTA-CABG Registry. J Invasive Cardiol. 2006; 18:147–52 [PubMed] [Google Scholar]
- 40. Mak KH, Einsenberg MJ, Tsang J, et al. ; for ROSETTA Investigators. Clinical impact of functional testing strategy among stented and non-stented patients: Insights from the ROSETTA registry. Int J Cardiol 2004; 95: 321–327 [DOI] [PubMed] [Google Scholar]
- 41. Eisenberg MJ, Blankenship JC, Huynh T, et al. ; for the ADORE Investigators. Evaluation of routine functional testing after percutaneous coronary intervention. Am J Cardiol 2004; 93: 744–747 [DOI] [PubMed] [Google Scholar]
- 42. Levine GN, Chodos AP, Loscalzo J. Restenosis following coronary angioplasty: Clinical presentations and therapeutic options. Clin Cardiol 1995; 18: 693–703 [DOI] [PubMed] [Google Scholar]
- 43. Daimon M, Watanabe H, Yamagishi H, et al. Physiologic assessment of coronary artery stenosis by coronary flow reserve measurements with transthoracic Doppler echocardiography: Comparison with exercise thallium-201 single photon emission computer tomography. J Am Coll Cardiol 2001; 37: 1310–1315 [DOI] [PubMed] [Google Scholar]
- 44. Rathore S, Terashima M, Katoh O, et al. Predictors of angiographic restenosis after drug eluting stents in the coronary arteries: Contemporary practice in real world patients. EuroIntervention 2009; 5: 349–354 [DOI] [PubMed] [Google Scholar]
- 45. Cutlip DE, Chauhan MS, Baim DS, et al. Clinical restenosis after coronary stenting: Perspectives from multicenter clinical trials. J Am Coll Cardiol 2002; 40: 2082–2089 [DOI] [PubMed] [Google Scholar]
- 46. Uren NG, Marraccini P, Gistri R, et al. Altered coronary vasodilator reserve and metabolism in myocardium subtended by normal arteries in patients with coronary artery disease. J Am Coll Cardiol 1993; 22: 650–658 [DOI] [PubMed] [Google Scholar]
- 47. Gibbons RJ, Abrams J, Chatterjee K, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina – summary article: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol 2003; 41: 159–168 [DOI] [PubMed] [Google Scholar]
- 48. Fox K, Garcia MA, Ardissino D, et al. ; Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology; ESC Committee for Practice Guidelines (CPG). Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur Heart J 2006; 27: 1341–1381 [DOI] [PubMed] [Google Scholar]
- 49. Théroux P, Marpole DG, Bourassa MG. Exercise stress testing in the post-myocardial infarction patient. Am J Cardiol 1983; 52: 664–667 [DOI] [PubMed] [Google Scholar]
- 50. Babapulle MN, Diodati JG, Blankenship JC, et al. Utility of routine exercise treadmill testing early after percutaneous coronary intervention. BMC Cardiovasc Disord 2007; 7: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dori G, Denekamp Y, Fishman S, et al. Exercise stress testing, myocardial perfusion imaging and stress echocardiography for detecting restenosis after successful percutaneous transluminal coronary angioplasty: A review of performance. J Intern Med 2003; 253: 253–262 [DOI] [PubMed] [Google Scholar]
- 52. Wong DT, Leung MC, Das R, et al. Diagnostic accuracy of adenosine stress cardiovascular magnetic resonance following acute ST-segment elevation myocardial infarction post primary angioplasty. J Cardiovasc Magn Reson 2011; 13: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bernhardt P, Spiess J, Levenson B, et al. Combined assessment of myocardial perfusion and late gadolinium enhancement in patients after percutaneous coronary intervention or bypass grafts: A multicenter study of an integrated cardiovascular magnetic resonance protocol. JACC Cardiovasc Imaging 2009; 2: 1292–1300 [DOI] [PubMed] [Google Scholar]
- 54. Kern MJ, Lerman A, Bech J-W, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory. Circulation 2006; 114: 1321–1341 [DOI] [PubMed] [Google Scholar]
- 55. Ong P, Athanasiadis A, Borgulya G, et al. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol 2012; 59: 655–662 [DOI] [PubMed] [Google Scholar]
- 56. Petretta M, Costanzo P, Cuocolo A. Imaging techniques for the assessment of coronary flow reserve. Eur Cardiol 2008; 4: 37–40 [Google Scholar]
- 57. L’Abbate A, Sambuceti G, Haunso S, et al. Methods for evaluating coronary microvasculature in humans. Eur Heart J 1999; 20: 1300–1313 [DOI] [PubMed] [Google Scholar]
- 58. Meimoun P, Tribouilloy C. Non-invasive assessment of coronary flow and coronary flow reserve by transthoracic Doppler echocardiography: a magic tool for the real world. Eur J Echocardiogr 2008; 9: 449–457 [DOI] [PubMed] [Google Scholar]
- 59. Gould KL, Kirkeeide RL, Buchi M. Coronary flow reserve as a physiologic measure of stenosis severity. J Am Coll Cardiol 1990; 15: 459–474 [DOI] [PubMed] [Google Scholar]
- 60. Miller DD, Donohue TJ, Younis LT, et al. Correlation of pharmacological 99mTc-sestamibi myocardial perfusion imaging with poststenotic coronary flow reserve in patients with angiographically intermediate coronary artery stenoses. Circulation 1994; 89: 2150–2160 [DOI] [PubMed] [Google Scholar]
- 61. Hozumi T, Yoshida K, Ogata Y, et al. Noninvasive assessment of significant left anterior descending coronary artery stenosis by coronary flow velocity reserve with transthoracic color Doppler echocardiography. Circulation 1998; 97: 1557–1562 [DOI] [PubMed] [Google Scholar]
- 62. Caiati C, Montaldo C, Zedda N, et al. New non-invasive method for coronary flow reserve assessment: Contrast-enhanced transthoracic second harmonic echo Doppler. Circulation 1999; 99: 771–778 [DOI] [PubMed] [Google Scholar]
- 63. Pepine CJ, Anderson RD, Sharaf BL, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol 2010; 55: 2825–2832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Petretta M, Soricelli A, Storto G, et al. Assessment of coronary flow reserve using single photon emission computed tomography with technetium 99m-labeled tracers. J Nucl Cardiol 2008; 15: 456–465 [DOI] [PubMed] [Google Scholar]
- 65. Storto G, Cirillo P, Vicario ML, et al. Estimation of coronary flow reserve by Tc-99m sestamibi imaging in patients with coronary artery disease: Comparison with the results of intracoronary Doppler technique. J Nucl Cardiol 2004; 11: 682–688 [DOI] [PubMed] [Google Scholar]
- 66. Bergmann SR, Herrero P, Markham J, et al. Non-invasive quantitation of myocardial blood flow in human subjects with oxygen-15-labeled water and positron emission tomography. J Am Coll Cardiol 1989; 14: 639–652 [DOI] [PubMed] [Google Scholar]
- 67. Masuda D, Nohara R, Tamaki N, et al. Evaluation of coronary blood flow reserve by 13N-NH3 positron emission computed tomography (PET) with dipyridamole in the treatment of hypertension with the ACE inhibitor (Cilazapril). Ann Nucl Med 2000; 14: 353–360 [DOI] [PubMed] [Google Scholar]
- 68. Rieber J, Huber A, Erhard I, et al. Cardiac magnetic resonance perfusion imaging for the functional assessment of coronary artery disease: a comparison with coronary angiography and fractional flow reserve. Eur Heart J 2006; 27: 1465–1471 [DOI] [PubMed] [Google Scholar]
- 69. Jaffe R, Dick A, Strauss BH. Prevention and treatment of microvascular obstruction-related myocardial injury and coronary no-reflow following percutaneous coronary intervention: A systematic approach. JACC Cardiovasc Interv 2010; 3: 695–704 [DOI] [PubMed] [Google Scholar]
- 70. Cutrn JC, Perrelli MG, Cavalieri B, et al. Microvascular dysfunction induced by reperfusion injury and protective effect of ischemic preconditioning. Free Radic Biol Med 2002; 33: 1200–1208 [DOI] [PubMed] [Google Scholar]
- 71. Bekkers SC, Yazdani SK, Virmani R, et al. Microvascular obstruction: Underlying pathophysiology and clinical diagnosis. J Am Coll Cardiol 2010; 55: 1649–1660 [DOI] [PubMed] [Google Scholar]
- 72. Fayad ZA, Fuster V, Nikolaou K, et al. Computed tomography and magnetic resonance imaging for noninvasive coronary angiography and plaque imaging: Current and potential future concepts. Circulation 2002; 106: 2026–2034 [DOI] [PubMed] [Google Scholar]
- 73. Gaspar T, Halon DA, Lewis BS, et al. Diagnosis of coronary in-stent restenosis with multidetector row spiral computed tomography. J Am Coll Cardiol 2005; 46: 1573–1579 [DOI] [PubMed] [Google Scholar]
- 74. Wilke N, Jerosch-Herold M, Wang Y, et al. Myocardial perfusion reserve: assessment with multisection, quantitative, first-pass MR imaging. Radiology 1997; 204: 373–384 [DOI] [PubMed] [Google Scholar]
- 75. Elhendy A, Porter TR. Assessment of myocardial perfusion with real-time myocardial contrast echocardiography: Methodology and clinical applications. J Nucl Cardiol 2005; 12: 582–590 [DOI] [PubMed] [Google Scholar]
- 76. Machac J. Cardiac positron emission tomography imaging. Semin Nucl Med 2005; 35: 17–36 [DOI] [PubMed] [Google Scholar]
- 77. Fraker TD, Fihn SD. 2007 Chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina. Circulation 2007; 116: 20762-20772 [DOI] [PubMed] [Google Scholar]
- 78. Jackson JD, Muhlestein JB, Bunch TJ, et al. ; Intermountain Heart Collaborative Study Group. Beta-blockers reduce the incidence of clinical restenosis: Prospective study of 4840 patients undergoing percutaneous coronary revascularization. Am Heart J 2003; 145: 875-881 [DOI] [PubMed] [Google Scholar]
- 79. Versaci F, Gaspardone A, Tomai F, et al. Chest pain after coronary artery stent placement. Am J Cardiol 2002; 89: 500–504 [DOI] [PubMed] [Google Scholar]
- 80. Kaku B, Honin IK, Horita Y, et al. The incidence of stent-edge spasm after stent implantation in patient with or without vasospastic angina pectoris. Int Heart J 2005; 46: 23–33 [DOI] [PubMed] [Google Scholar]
- 81. Corti R, Fuster V. Should standard medical therapy for angina include a statin? Clin Cardiol 2004; 27: 547–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Nissen SE, Nicholls SJ, Sipahi I, et al. ; for the ASTEROID Investigators. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. The ASTEROID trial. JAMA 2006; 295: 1556–1565 [DOI] [PubMed] [Google Scholar]
- 83. Colin P, Ghaleh B, Monnet X, et al. Contributions of heart rate and contractility to myocardial oxygen balance during exercise. Am J Physiol Heart Circ Physiol 2003; 284: H676–H682 [DOI] [PubMed] [Google Scholar]
- 84. Grønholdt ML, Dalager-Pedersen S, Falk E. Coronary atherosclerosis: Determinants of plaque rupture. Eur Heart J 1998; 19(Suppl. C): C24–C29 [PubMed] [Google Scholar]
- 85. Fox K, Ford I, Steg PG, et al. ; on behalf of the BEAUTIFUL investigators. Relationship between ivabradine treatment and cardiovascular outcomes in patients with stable coronary artery disease and left ventricular systolic dysfunction with limiting angina: A subgroup analysis of the randomized, controlled BEAUTIFUL trial. Eur Heart J 2009; 30: 2337–2345 [DOI] [PubMed] [Google Scholar]
- 86. Tardif JC, Ponikowski P, Kahan T; ASSOCIATE study investigators Efficacy of the If current inhibitor ivabradine in patients with chronic stable angina receiving beta blocker therapy: A 4 month, randomized, placebo-controlled trial. Eur Heart J 2009; 30: 540–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Köster R, Kaehler J, Meinertz T; REDUCTION Study Group Treatment of stable angina pectoris by ivabradine in every day practice: The REDUCTION study. Am Heart J 2009; 158: e51–e57 [DOI] [PubMed] [Google Scholar]
- 88. Borer JS, Fox K, Jaillon P, et al. ; Ivabradine Investigators Group. Antianginal and antiischemic effects of ivabradine, an I(f) inhibitor, in stable angina: a randomized, double-blind, multicentered, placebo-controlled trial. Circulation 2003; 107: 817–823 [DOI] [PubMed] [Google Scholar]
- 89. Tardif JC, Ford I, Tendera M, et al. ; INITIATIVE Investigators. Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable angina. Eur Heart J 2005; 26: 2529–2536 [DOI] [PubMed] [Google Scholar]
- 90. Ruzyllo W, Tendera M, Ford I, et al. Antianginal efficacy and safety of ivabradine compared with amlodipine in patients with stable effort angina pectoris: A 3-month randomised, double-blind, multicentre, noninferiority trial. Drugs 2007; 67: 393–405 [DOI] [PubMed] [Google Scholar]
- 91. Ruzyllo W, Swed H, Sadowski Z, et al. Efficacy of trimetazidine in patients with recurrent angina: A subgroup analysis of the TRIMPOL II study. Curr Med Res Opin 2004; 20: 1447–1454 [DOI] [PubMed] [Google Scholar]
- 92. Haigney MC, Lakatta EG, Stern MD, et al. Sodium channel blockade reduces hypoxic sodium loading and sodium-dependent calcium loading. Circulation 1994; 90: 391–399 [DOI] [PubMed] [Google Scholar]
- 93. Chaitman BR, Pepine CJ, Parker JO, et al. ; Combination Assessment of Ranolazine In Stable Angina (CARISA) Investigators: Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: A randomized controlled trial. JAMA 2004; 291: 309–316 [DOI] [PubMed] [Google Scholar]
- 94. Stone PH, Gratsiansky NA, Blokhin A, et al. ; ERICA Investigators. Antianginal efficacy of ranolazine when added to treatment with amlodipine: The ERICA (Efficacy of Ranolazine in Chronic Angina) trial. J Am Coll Cardiol 2006; 48: 566–575 [DOI] [PubMed] [Google Scholar]
- 95. Wilson SR, Scirica BM, Braunwald E, et al. Efficacy of ranolazine in patients with chronic angina observations from the randomized, double blind, placebo controlled MERLIN-TIMI (Metabolic efficiency with Ranolazine for less ischemia in non ST-segment Elevation acute Coronary Syndrome) 36 TRIAL. J Am Coll Cardiol 2009; 53: 1510–1516 [DOI] [PubMed] [Google Scholar]
- 96. Rousseau MF, Pouleur H, Cocco G, et al. Comparative efficacy of ranolazine versus atenolol for chronic angina pectoris. Am J Cardiol 2005; 95: 311–316 [DOI] [PubMed] [Google Scholar]
- 97. Arnold SV, Morrow DA, Wang K, et al. ; MERLIN-TIMI 36 Investigators. Effects of ranolazine on disease-specific health status and quality of life among patients with acute coronary syndromes: Results from the MERLIN-TIMI 36 randomized trial. Circ Cardiovasc Qual Outcomes 2008; 1: 107–115 [DOI] [PubMed] [Google Scholar]
- 98. Matsuo H, Watanabe S, Segawa T, et al. Evidence of pharmacologic preconditioning during PTCA by intravenous pretreatment with ATP-sensitive K+ channel opener nicorandil. Eur Heart J 2003; 24: 1296–1130 [DOI] [PubMed] [Google Scholar]
- 99. IONA study group Effect of Nicorandil on coronary events in patients with stable angina. The Impact Of Nicorandil in Angina (IONA) randomized trial. Lancet 2002; 359: 1269–1275 [DOI] [PubMed] [Google Scholar]
- 100. Hambrecht R, Walther C, Mobius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease. Circulation 2004; 109: 1371–1378 [DOI] [PubMed] [Google Scholar]
- 101. Crea F, Lanza GA. Angina pectoris and normal coronary arteries: Cardiac syndrome X. Heart 2004; 90: 457–463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Dougenis D, Kelly PJ, Brown AH. Late survival and predictors of recurrent angina after coronary artery reoperation. Thorac Cardiovasc Surg 1997; 45: 114–118 [DOI] [PubMed] [Google Scholar]
- 103. Kastrati A, Mehilli J, von Bekerath N, et al. ; for ISAR-DESIRE Study Investigators Sirolimus-eluting stent or paclitaxel-eluting stent vs. balloon angioplasty for prevention of recurrences in patients with coronary in-stent restenosis: A randomized controlled trial. JAMA 2005; 293: 165–171 [DOI] [PubMed] [Google Scholar]
- 104. Singh IM, Filby SJ, El Sakr F, et al. Drug-eluting stents versus bare-metal stents for treatment of bare-metal in-stent restenosis. Catheter Cardiovasc Interv 2010; 76: 257–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Iofina E, Radke PW, Skurzewski P, et al. Superiority of sirolimus eluting stent compared with intracoronary beta radiation for treatment of in-stent restenosis: A matched comparison. Heart 2005; 91: 1584-1589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Fitzgibbon GM, Kafka HP, Leach AJ, et al. Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5065 grafts related to survival and reoperation in 1388 patients during 25 years. J Am Coll Cardiol 1996; 28: 616–626 [DOI] [PubMed] [Google Scholar]
- 107. Savage M, Douglas J, Fischman D, et al. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. N Engl J Med 1997; 337: 740–747 [DOI] [PubMed] [Google Scholar]
- 108. Stone GW, Rogers C, Hermiller J, et al. ; on behalf of the FilterWire EX Randomized Evaluation Investigators. Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts. Circulation 2003; 108: 548–553 [DOI] [PubMed] [Google Scholar]
- 109. Vermeersch P, Agostoni P. Should degenerated saphenous vein grafts routinely be sealed with drug-eluting stents? J Interv Cardiol 2005; 18: 467–473 [DOI] [PubMed] [Google Scholar]
- 110. Ellis SG, Brener SJ, Deluca S, et al. Late myocardial ischaemic events after saphenous vein graft intervention–importance of initially ‘nonsignificant’ vein graft lesions. Am J Cardiol 1997; 79: 1460–1464 [DOI] [PubMed] [Google Scholar]
- 111. Gowda RM, Khan IA, Punukollu G, et al. Treatment of refractory angina pectoris. Int J Cardiol 2005; 101: 1–7 [DOI] [PubMed] [Google Scholar]
- 112. Moussavian M, Casterella PJ, Teirstein PS. Restenosis after angioplasty. Curr Treat Options Cardiovasc Med 2001; 3: 103–113 [DOI] [PubMed] [Google Scholar]
- 113. Eltchaninoff H, Carlot R, Tron C, et al. Analysis of nonintervention strategy for in-stent restenosis in Pauci- or asymptomatic patients. Am J Cardiol 2004; 93: 1038–1040 [DOI] [PubMed] [Google Scholar]
- 114. Kuchulakanti PK, Chu WW, Torguson R, et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation 2006; 113: 1108-1113 [DOI] [PubMed] [Google Scholar]
- 115. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: A pooled analysis of multicenter coronary stent clinical trials. Circulation 2001; 103: 1967–1971 [DOI] [PubMed] [Google Scholar]
- 116. Lemesle G, Sudre A, Modine T, et al. High incidence of recurrent in stent thrombosis after successful treatment of a first in stent thrombosis. Catheter Cardiovasc Interv 2008; 72: 470–478 [DOI] [PubMed] [Google Scholar]
- 117. Tan KH, Sulke N, Taub N, et al. Predictors of angiographic findings when chest pain recurs after successful coronary angioplasty. Eur Heart J 1995; 16: 1593–1602 [DOI] [PubMed] [Google Scholar]
- 118. Alderman EL, Kip KE, Whitlow PL, et al. ; Bypass Angioplasty Revascularization Investigation. Native coronary disease progression exceeds failed revascularization as cause of angina after five years in the Bypass Angioplasty Revascularization Investigation (BARI). J Am Coll Cardiol 2004; 44: 766–774 [DOI] [PubMed] [Google Scholar]
- 119. Faxon DP, Ghalilli K, Jacobs AK, et al. The degree of revascularization and outcome after multivessel coronary angioplasty. Am Heart J 1992; 123: 854–859 [DOI] [PubMed] [Google Scholar]
- 120. Bell MR, Bailey KR, Reeder GS, et al. Percutaneous transluminal angioplasty in patients with multivessel coronary disease: How important is complete revascularization for cardiac event-free survival? J Am Coll Cardiol 1990; 16: 553–562 [DOI] [PubMed] [Google Scholar]
- 121. Samson M, Meester HJ, De Feyter PJ, et al. Successful multiple segment coronary angioplasty: Effect of completeness of revascularization in single-vessel multilesions and multivessels. Am Heart J 1990; 120: 1–12 [DOI] [PubMed] [Google Scholar]
- 122. Britten MB, Zeiher AM, Schächinger V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron Artery Dis 2004; 15: 259–264 [DOI] [PubMed] [Google Scholar]
- 123. Bolognese L, Carrabba N, Parodi G, et al. Impact of microvascular dysfunction on left ventricular remodeling and long-term clinical outcome after primary coronary angioplasty for acute myocardial infarction. Circulation 2004; 109: 1121–1126 [DOI] [PubMed] [Google Scholar]
- 124. Katoh D, Mizuno Y, Harada E, et al. High incidence of provoked coronary spasm in the presence of a stent after myocardial infarction: Therapeutic and prognostic implications. Coron Artery Dis 2012; 23: 141–145 [DOI] [PubMed] [Google Scholar]
- 125. Schindler TH, Hornig B, Buser PT, et al. Prognostic value of abnormal vasoreactivity of epicardial coronary arteries to sympathetic stimulation in patients with normal coronary angiograms. Arterioscler Thromb Vasc Biol 2003; 23: 495–501 [DOI] [PubMed] [Google Scholar]