Abstract
Background:
Early restoration of blood flow of the infarct-related artery is associated with an improved outcome in patients with ST-elevation myocardial infarction (STEMI). Previous studies have shown a low mortality in patients with TIMI 3 flow before primary percutaneous coronary intervention (PCI). Most likely these patients had spontaneous recanalization of the infarct vessel and might constitute a low-risk subgroup. The purpose of the present analysis was to investigate whether TIMI 3 flow obtained with fibrinolysis before PCI is associated with a clinical outcome comparable to that in patients with spontaneous TIMI 3 flow.
Methods:
Patients with STEMI <6 hours enrolled in the ASSENT-4 PCI study were randomized to facilitated PCI with tenecteplase or primary PCI. For this analysis, patients were divided into three groups according to the TIMI flow of the infarct vessel before PCI: TIMI 0/1, TIMI 2, and TIMI 3.
Results:
From a total of 1617 patients, 861 had TIMI 0/1, 279 had TIMI 2, and 477 TIMI 3 flow. The rates of TIMI 3 flow after PCI were 84.6, 89.7, and 95.6%, respectively. Complete ST resolution was observed most often in the TIMI 3 flow group (47.5, 53.6, and 58.6%). The incidence of cardiogenic shock (6.2, 5.5, and 3.6%) and 90-day mortality (6.1, 4.7, and 4.0%) were lowest in the group with TIMI 3 patency before PCI, respectively. The rate of TIMI 3 flow before PCI was higher in the facilitated PCI group than in the primary PCI group (43.9 vs. 15.2%). The 90-day mortality in patients with TIMI 3 before PCI was identical in the facilitated and the primary PCI groups (14/353, 4.0% vs. 5/124, 4.0%).
Conclusion:
In this post-hoc analysis of ASSENT-4 PCI, TIMI grade 3 flow in the infarct-related artery before PCI, occurring either spontaneously or obtained by fibrinolysis, is associated with a higher TIMI patency after PCI, better improved ST resolution and a trend towards a favourable clinical outcome after 90 days.
Keywords: Facilitated PCI, patency, primary percutaneous coronary intervention, ST-elevation myocardial infarction
Introduction
In patients with acute ST-segment elevation myocardial infarction rapid restoration of blood flow in the infarct-related coronary artery is associated with an improved prognosis.1 One major component of the success of reperfusion therapy is the total ischaemic time.2–4 Primary percutaneous coronary intervention (PCI) is the preferred treatment in patients with acute ST-elevation myocardial infarction (STEMI), provided it can be undertaken with minimal delay by an experienced team following presentation.5 This strategy is limited, however, by time delays including those imposed by transferring patients to PCI-capable facilities.6 Establishing early pharmacological reperfusion prior to mechanical intervention has the potential to overcome these time-dependent limitations of primary PCI and thereby improve both procedural success and clinical outcomes.7 Previous studies report an improved outcome in patients with primary PCI with TIMI 3 patency prior to the intervention.8,9 These patients might constitute a special subgroup without persistent occlusion. The aim of this analysis was to compare the fate of patients with TIMI 3 patency before primary PCI occurring either spontaneous or associated with fibrinolysis.
Methods
The details of the ASSENT-4 PCI study have been published previously.10 In brief, 1667 patients with ST-segment elevation acute myocardial infarction of less than 6 hours, scheduled to undergo primary PCI were randomized to a standard PCI procedure or one preceded by full-dose tenecteplase administration (facilitated PCI). The investigators had initially planned to enrol 4000 patients; however, the data and safety monitoring board recommended early cessation of enrolment because of higher in-hospital mortality in the facilitated PCI group. ECG criteria for entry required total ST-segment elevations of ≥0.6 mV across multiple leads or, for inferior infarction, ≥0.6 mV ST-segment deviation with at least 0.4 mV of ST-elevation in leads II, III, aVF, or new left bundle branch block with concordant ST-segment elevation ≥0.1 mV.
For this analysis, we created subgroups of patients according to the TIMI flow11 in the infarct-related coronary artery as assessed by the investigators.
Electrocardiographic analysis
The amount of ST-segment elevation was measured at the J point with magnified callipers from leads I, aVL, and V1–V6 for anterior myocardial infarction and leads II, III, aVF, V5, and V6 for inferior MI. For the total ST-segment deviation, the sum of the ST-segment depression in leads II, III, and aVF for anterior and that in V1–V4 for inferior myocardial infarction were added. The resolution of ST-segment elevation (or total deviation if present) at 60 min and 180 min was classified according to the Schroder’s method:12 complete (i.e. resolution of the initial sum of ST-segment elevation ≥70%), partial (i.e. ST-segment resolution <70% to 30%), and none (i.e., ST-segment resolution <30%). Electrocardiographic spontaneous reperfusion was defined as those patients who achieved complete (≥70%) ST-segment resolution.
Statistical analysis
Descriptive statistics were summarized as medians with 25th and 75th percentiles for continuous variables and the Mann–Whitney U-test or Kruskal–Wallis test was used for group comparisons, where appropriate. The groups were compared with the Chi-squared test for categorical variables (%). A multivariate logistic regression, using backward stepwise variable selection procedures, was used to assess the independent prognostic value of TIMI 3 patency for 90-day mortality adjusted for key risk factors including age, sex, diabetes, systolic blood pressure, heart rate, location of infarction, Killip class, and time from onset of symptoms to treatment. All tests were two-sided, with a 5% level of significance. All analyses were performed using SPSS (version 16).
Results
A total of 1667 patients were included in ASSENT-4 PCI. Angiographic data were available from 1617 patients, of whom 861 (53.2%) had TIMI 0/1, 279 (17.3%) had TIMI 2, and 477 (29.5%) TIMI 3 flow at the initial angiography. The baseline variables of the groups according to the TIMI flow prior to PCI are shown in Table 1. There were no clinical relevant differences between the three groups, except for the incidence of Killip class, showing a higher rate of Killip class I in the group with TIMI 3 flow prior to PCI.
Table 1.
Baseline characteristics of patients according to TIMI flow before percutaneous coronary intervention
| TIMI 0/1 (n=861) | TIMI 2 (n=279) | TIMI 3 (n=477) | p-value | |
|---|---|---|---|---|
| Age (years) | 59 (52–69) | 62 (53–72) | 60 (51–70) | 0.226 |
| Women | 22.0 | 21.5 | 25.2 | 0.346 |
| Weight (kg) | 78 (69–87) | 77 (70–85) | 77 (68–85) | 0.049 |
| Previous CHF | 1.3 | 0.7 | 1.3 | 0.739 |
| Previous MI | 11.2 | 9.0 | 12.8 | 0.278 |
| Previous PCI | 8.0 | 8.4 | 8.7 | 0.902 |
| Previous CABG | 1.8 | 1.4 | 2.3 | 0.651 |
| Hypertension | 47.0 | 44.1 | 47.2 | 0.658 |
| Diabetes | 15.9 | 14.0 | 18.5 | 0.241 |
| Current smoker | 48.4 | 48.7 | 43.9 | 0.261 |
| Heart rate (bpm) | 75 (64–86) | 72 (62–84) | 73 (62–86) | 0.353 |
| Systolic blood pressure (mmHg) | 130 (119–150) | 135 (120–150) | 136 (120–150) | 0.175 |
| Symptom onset to initial treatment (min) | 151 (105–220) | 140.5 (100–210) | 145 (97–220) | 0.284 |
| Symptom onset to angiography (min) | 248 (158–305) | 246 (151–291) | 245 (184–337) | |
| Killip class >I | 8.6 | 10.4 | 5.7 | 0.027 |
| Anterior MI location | 46.7 | 55.6 | 47.8 | 0.034 |
Values are % or median (interquartile range). Chi-squared test for categorical variables and Kruskal–Wallis test for continuous variables. CABG, coronary artery bypass graft; CHF, congestive heart failure; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction.
We observed a higher rate of TIMI 3 flow after PCI in the group with TIMI 3 flow before PCI. In addition, the incidence of complete ST resolution was higher in these patients both before and after PCI (Table 2). The mortality (Figure 1) and combined clinical event rates after 30 and 90 days (Table 2) tended to be lower in the group with TIMI 3 flow before PCI, but the differences were not statistically significant. In the multivariate analysis, TIMI 3 flow before PCI was not an independent predictor of 90-day survival. At 30 days the clinical endpoints tended to better outcomes in patients with TIMI 2 or 3 flow, and at 90 days (the principal time point for the trial endpoint analysis in ASSENT 4 PCI) the lowest mortality, incidence of shock, heart failure, and the combined endpoints were observed in patients with pre-PCI TIMI 3, but the differences did not achieve statistical significance. At 90 days, Patients with a patent vessel (TIMI 2/3, n=756) before angiography had a lower mortality (4.2 vs. 6.1%, p=0.1) and combined primary endpoint (mortality, shock, and congestive heart failure) of 14.0 vs. 16.2% (p=0.2) compared to patients with an occluded artery (TIMI 0/1) before PCI. Again the differences were statistically not significant. The incidence of TIMI 3 flow was higher in the group with facilitated PCI (43.9 vs. 15.2%).
Table 2.
Outcomes of the patients according to the TIMI flow before percutaneous coronary intervention
| TIMI 0/1 (n=861) | TIMI 2 (n=279) | TIMI 3 (n=477) | p-value | |
|---|---|---|---|---|
| Complete ST-segment resolution (≥70%) at 60 min (prior to PCI) | 10.5 | 19.5 | 38.6 | <0.001 |
| TIMI 3 patency after PCI | 84.6 | 89.7 | 95.6 | <0.001 |
| Complete ST-segment resolution (≥70%) at 180 min (post PCI) | 47.5 | 53.6 | 58.6 | 0.002 |
| 30-day outcome | ||||
| Death | 5.2 | 3.6 | 3.6 | 0.274 |
| Cardiogenic shock | 6.0 | 5.5 | 3.2 | 0.082 |
| CHF | 10.3 | 9.1 | 9.2 | 0.760 |
| Reinfarction | 3.3 | 5.1 | 5.1 | 0.197 |
| Composite (death/shock/CHF) | 14.8 | 13.6 | 12.6 | 0.548 |
| Stroke | ||||
| ICH | 0.3 | 0.4 | 0.8 | 0.444 |
| Ischaemic | 0.6 | 0.0 | 0.8 | 0.324 |
| Unknown cause | 0.3 | 0.0 | 0.2 | 0.584 |
| Major bleeding | 5.2 | 6.1 | 4.0 | 0.401 |
| 90-day outcome | ||||
| Death | 6.1 | 4.7 | 4.0 | 0.241 |
| Cardiogenic shock | 6.2 | 5.5 | 3.6 | 0.147 |
| CHF | 11.2 | 10.2 | 9.7 | 0.688 |
| Reinfarction | 3.8 | 5.9 | 6.0 | 0.139 |
| Composite (death/shock/CHF) | 16.2 | 15.4 | 13.3 | 0.365 |
| Stroke | ||||
| ICH | 0.3 | 0.7 | 0.8 | 0.233 |
| Ischaemic | 0.6 | 0 | 0.8 | 0.665 |
| Unknown cause | 0.3 | 0 | 0.2 | 0.584 |
Values are %. CHF, congestive heart failure; ICH, intracerebral haemorrhage; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction.
Figure 1.
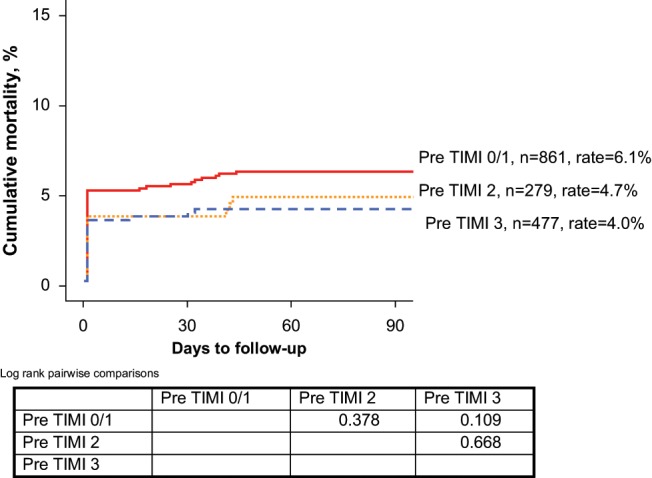
Kaplan–Meier curves for all-cause mortality according to thrombolysis in myocardial infarction (TIMI) flow of the infarct-related artery before percutaneous coronary intervention (n=1617)
Patients then were divided into four groups according to their treatment and TIMI flow before PCI. The baseline variables of the four groups are listed in Table 3 and the clinical outcomes and events are listed in Table 4. We observed no difference in outcome in patients with TIMI 3 flow prior PCI between the facilitated PCI and primary PCI group (Table 4, Figure 2). In contrast, the mortality and combined endpoint rates at 30 days were higher in patients with TIMI <3 flow before PCI treated with tenecteplase compared to patients with primary PCI (Table 4, Figure 2). The lowest event rate was observed in patients with a time interval of <3 hours between symptom onset and randomization and TIMI 3 flow before PCI (Table 5).
Table 3.
Baseline characteristics according to pre-percutaneous coronary intervention TIMI 3 or <3 flow in the two treatment groups
| Pre-PCI TIMI 3 |
Pre-PCI TIMI <3 |
|||||
|---|---|---|---|---|---|---|
| Primary PCI (n=124) | TNK+PCI (n=353) | p-value | Primary PCI (n=689) | TNK+PCI (n=451) | p-value | |
| Age (years) | 60 (51–70) | 60 (51–70) | 0.939 | 59 (51–69) | 61 (53–70) | 0.153 |
| Women | 33.1 | 22.4 | 0.018 | 20.5 | 23.9 | 0.164 |
| Weight (kg) | 74 (65–84) | 77 (68–85) | 0.126 | 78 (70–86) | 77 (67–87) | 0.814 |
| Previous CHF | 2.4 | 0.9 | 0.180 | 1.3 | 0.9 | 0.517 |
| Previous MI | 12.9 | 12.8 | 0.981 | 9.9 | 11.9 | 0.300 |
| Previous PCI | 6.5 | 9.4 | 0.321 | 8.5 | 7.4 | 0.519 |
| Previous CABG | 3.2 | 2.0 | 0.433 | 1.5 | 2.0 | 0.485 |
| Hypertension | 46.8 | 47.3 | 0.918 | 46 | 46.8 | 0.797 |
| Diabetes | 24.2 | 16.5 | 0.057 | 13.5 | 18.4 | 0.026 |
| Current smoker | 47.1 | 42.8 | 0.414 | 49.2 | 47.3 | 0.541 |
| Heart rate (bpm) | 75 (65–90) | 72 (60–84) | 0.031 | 75 (64–85) | 74 (62–85) | 0.359 |
| Systolic blood pressure (mmHg) | 130 (115–150) | 138 (120–154) | 0.072 | 135 (120–150) | 130 (117–148) | 0.062 |
| Symptom onset to initial treatment (min) | 139 (95–215) | 149 (100–225) | 0.312 | 145 (100–215) | 155 (110–221) | 0.143 |
| Killip class >I | 3.3 | 6.5 | 0.490 | 7.7 | 11.1 | 0.183 |
| Anterior MI location | 52.9 | 46.1 | 0.196 | 46.9 | 51.9 | 0.100 |
Values are% or median (interquartile range). CABG, coronary artery bypass graft; CHF, congestive heart failure; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction; TNK, tenecteplase.
Table 4.
Outcome according to TIMI 3 flow before percutaneous coronary intervention in two treatment groups
| Pre-PCI TIMI 3 |
Pre-PCI TIMI <3 |
|||||
|---|---|---|---|---|---|---|
| Primary PCI (n=124) | TNK+PCI (n=353) | p-value | Primary PCI (n=689) | TNK+PCI (n=451) | p-value | |
| Complete 60 min ST-segment resolution (post PCI) (n=with 60 min ECG) | 39.3 (n=89) | 38.4 (n=258) | 0.873 | 11.1 (n=505) | 14.9 (n=329) | 0.106 |
| TIMI 3 patency after PCI | 95.1 | 95.7 | 0.786 | 87.8 | 82.9 | 0.025 |
| Complete 180 min ST-segment resolution (post PCI) (n=with 180 min ECG) | 61.9 (n=97) | 57.5 (n=287) | 0.451 | 51.0 (n=561) | 45.9 (n=362) | 0.128 |
| 30-day outcome | ||||||
| Death | 3.2 | 3.7 | 1.000 | 3.6 | 6.7 | 0.020 |
| Cardiogenic shock | 2.5 | 3.4 | 0.769 | 4.5 | 7.9 | 0.020 |
| CHF | 9.1 | 9.3 | 0.952 | 8.7 | 12.0 | 0.068 |
| Reinfarction | 2.4 | 6.0 | 0.119 | 2.9 | 4.9 | 0.079 |
| Major bleeding | 4.0 | 4.0 | 0.974 | 4.6 | 6.7 | 0.144 |
| Composite (death/shock/CHF) | 12.1 | 12.8 | 0.843 | 11.6 | 18.8 | 0.001 |
| 90-day outcome | ||||||
| Death | 4.0 | 4.0 | 0.992 | 4.5 | 7.6 | 0.032 |
| Cardiogenic shock | 2.5 | 4.1 | 0.425 | 4.6 | 8.2 | 0.013 |
| CHF | 9.1 | 9.9 | 0.807 | 9.0 | 13.9 | 0.011 |
| Reinfarction | 3.2 | 7.0 | 0.133 | 3.4 | 5.7 | 0.066 |
| Composite (death/shock/CHF) | 12.1 | 13.8 | 0.641 | 12.7 | 21.2 | <0.001 |
| Stroke | ||||||
| ICH | 0 | 1.1 | 0.234 | 0.1 | 0.9 | 0.064 |
| Ischaemic | 0 | 1.1 | 0.234 | 0 | 1.1 | 0.006 |
| Unknown cause | 0 | 0.3 | 0.553 | 0 | 0.7 | 0.032 |
Values are%. CHF, congestive heart failure; ICH, intracerebral haemorrhage; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction; TNK, tenecteplase.
Figure 2.
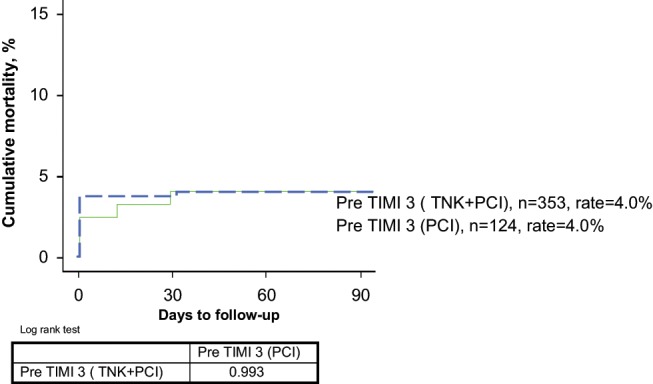
Kaplan–Meier curves for all-cause-mortality in patients with thrombolysis in myocardial infarction (TIMI) flow 3 or 0–2 according to their assignment to the facilitated or primary percutaneous coronary intervention group
Table 5.
Ninety-day event rates in patients with time to randomization ≤3 hours in the two treatment groups
| Pre-PCI TIMI 3 |
Pre-PCI TIMI <3 |
|||||
|---|---|---|---|---|---|---|
| Primary PCI (n=87) | TNK+PCI (n=240) | p-value | Primary PCI (n=460) | TNK+PCI (n=308) | p-value | |
| Death | 2.3 | 2.9 | 0.755 | 3.7 | 5.9 | 0.166 |
| Cardiogenic shock | 0 | 3.0 | 0.108 | 4.9 | 8.6 | 0.004 |
| CHF | 5.9 | 6.4 | 0.877 | 8.2 | 11.6 | 0.123 |
| Reinfarction | 1.1 | 8.1 | 0.022 | 4.2 | 5.7 | 0.354 |
| 90-day composite (death/shock/CHF) | 6.9 | 9.7 | 0.438 | 11.2 | 17.6 | 0.011 |
Values are%. CHF, congestive heart failure; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction; TNK, tenecteplase.
Discussion
Primary PCI is the preferred reperfusion therapy in patients with STEMI, if it can be provided by an experienced team within 2 hours after first medical contact.13 Previous reports have shown a higher success rate of primary PCI and a lower mortality in patients with TIMI 3 flow before PCI.8,9 Our analysis is the first to investigate the influence of TIMI 3 flow mediated by fibrinolysis on outcome of patients with PCI for acute ST-elevation myocardial infarction. In previous studies, the rate of TIMI 3 flow before primary PCI occurring spontaneously or mediated by heparin, aspirin, and clopidogrel has been found to be around 15–20%.14 In a meta-analysis of the PAMI trials, TIMI 3 flow before primary PCI was observed in 15.7% of the patients.8 These patients had a higher rate of TIMI 3 flow after PCI, which was 98.1 vs. 91.4% in patients with TIMI 0–2 flow before PCI. This was associated with a very low mortality of 0.5% after 6 months while the 4.4% mortality in patients with an occluded infarct vessel before PCI was significantly higher. However, in ASSENT-4 PCI, the 90-day mortality in patients with TIMI 3 flow before PCI was 4.0, which is higher than the mortality in those patients in the PAMI trials. This may reflect the design of ASSENT-4 PCI which purposefully recruited higher risk patients. However, in a retrospective analysis the benefit of facilitated PCI in the FINESSE trial has been observed only in patients with higher baseline risk.15 As in the PAMI meta-analysis in our study, patients with TIMI 3 flow before PCI had the lowest mortality. There was no difference in mortality between patients with TIMI 3 flow occurring spontaneously or mediated by fibrinolysis. In addition we observed comparable rates of TMI 3 flow after PCI and successful myocardial reperfusion rates assessed by complete ST resolution in patients with TIMI 3 flow before PCI in the primary PCI and facilitated PCI groups. Pre-PCI TIMI 3 flow was strongly associated with complete resolution of ST-segment elevation before intervention. After PCI, complete ST-segment resolution was again commonest in the pre-PCI TIMI 3 group. Complete resolution is generally accepted as evidence for myocardial salvage and therefore might predict improved clinical outcome.12 In a separate analysis of ASSENT-4 PCI spontaneous reperfusion assessed in a subgroup of 585 patients, spontaneous reperfusion determined by ST resolution was a stronger predictor of an improved outcome compared to TIMI 3 flow.16 In our analysis, mortality, shock, heart failure, and the combined endpoint were all lower with pre-PCI TIMI 3 but the differences did not reach statistical significance. However, in contrast to previous reports, TIMI 3 flow before PCI was not an independent predictor of survival. The reason might be related to the limited number of patients in our analysis, but is most likely due to the unexpected high mortality in the patients with TIMI 3 flow. In disagreement with earlier reports, the 90-day mortality in patients with TIMI 3 flow before PCI in the primary PCI group was found to be almost similar to that of patients with TIMI 2 flow (4.0 vs. 4.5%).
One interesting finding was that patients with TIMI 0–2 flow in the facilitated PCI group had a higher mortality than patients with TIMI 0–2 flow in the primary PCI group (7.6% vs. 4.5%). These patients had the lowest TIMI 3 flow rate after PCI (82.9%) and the highest 90-day composite endpoint rate of 21.2%. These results imply a negative impact of failed fibrinolysis on outcome of facilitated PCI. Therefore the positive effect of an increased rate of patent infarct vessels before PCI might be counterbalanced by the negative impact of failed fibrinolysis on PCI.
Other approaches than fibrinolysis to improve patency of the infarct vessel before primary PCI include glycoprotein IIb/IIIa inhibitors and ADP-receptor blockers. In the EGYPT meta-analysis, early initiation of glycoprotein IIb/IIIa inhibitors before primary PCI significantly increased TIMI 3 patency.14 In the randomized On-TIME 2 study, especially patients with longer transportation times had benefit from pre-hospital administration of tirofiban.17 The only randomized trial investigating the value of pre-hospital administration of clopidogrel before primary PCI showed only a modest increase of TIMI 3 patency compared to standard therapy.18 However the time between the clopidogrel loading dose and angiography was only 47 min, so clopidogrel had little chance to be metabolized and effectively inhibit platelet aggregation. It might be speculated that the new ADP-receptor antagonists parasugrel and ticagrelor will be more effective in this setting.
In summary, in this post-hoc analysis of ASSENT-4 PCI, TIMI grade 3 flow in the infarct-related artery before PCI, occurring either spontaneously or obtained by fibrinolysis, is associated with a higher TIMI patency after PCI, better improved ST resolution, and a trend towards a favourable clinical outcome after 90 days. Therefore effective and safe approaches to increase pre-PCI TIMI 3 flow should be investigated.
Footnotes
Funding: The ASSENT-4 PCI trial was funded by Boehringer Ingelheim.
References
- 1. Simes RJ, Topol EJ, Holmes DR, Jr., et al. Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion. Importance of early and complete infarct artery reperfusion. GUSTO-I Investigators. Circulation 1995; 91: 1923–1928 [DOI] [PubMed] [Google Scholar]
- 2. De Luca G, Suryapranata H, Ottervanger JP, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004; 109: 1223–1225 [DOI] [PubMed] [Google Scholar]
- 3. Reimer KA, Vander Heide RS, Richard VJ. Reperfusion in acute myocardial infarction: effects of timing and modulating factors in experimental models. Am J Cardiol 1993; 72: 13G–21G [DOI] [PubMed] [Google Scholar]
- 4. Tarantini G, Cacciavillani L, Corbetti F, et al. Duration of ischemia is a major determinant of transmurality and severe microvascular obstruction after primary angioplasty: a study performed with contrast-enhanced magnetic resonance. J Am Coll Cardiol 2005; 46: 1229–1235 [DOI] [PubMed] [Google Scholar]
- 5. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet 2003; 361: 13–20 [DOI] [PubMed] [Google Scholar]
- 6. Miedema MD, Newell MC, Duval C, et al. Causes of delay and associated mortality in patients with ST-segment myocardial infarction. Circulation 2011; 124: 1636–1644 [DOI] [PubMed] [Google Scholar]
- 7. Gersh BJ, Stone GW, White HD, et al. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA 2005; 293: 979–998 [DOI] [PubMed] [Google Scholar]
- 8. Stone GW, Cox D, Garcia E, et al. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation 2001; 104: 636–641 [DOI] [PubMed] [Google Scholar]
- 9. Brodie BR, Stuckey TD, Hansen C, et al. Benefit of coronary reperfusion before intervention on outcomes after primary angioplasty for acute myocardial infarction. Am J Cardiol 2000; 85: 13–18 [DOI] [PubMed] [Google Scholar]
- 10. The ASSENT-4 PCI Investigators Primary versus tenecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction (ASSENT-4 PCI). Lancet 2006: 367: 569–578 [DOI] [PubMed] [Google Scholar]
- 11. TIMI Study Group The thrombolysis in myocardial infarction (TIMI) trial: phase I findings. N Engl J Med 1985; 312: 932–936 [DOI] [PubMed] [Google Scholar]
- 12. Schröder R, Zeymer U, Wegscheider K, et al. ; for the HIT-4 trial group. Comparison of the predictive value of ST segment elevation resolution 90 and 180 minutes after start of streptokinase in acute myocardial infarction. A substudy of the Hirudin for Improvement of Thrombolysis (HIT)-4 Study. Eur Heart J 1999; 20: 1563–1571 [DOI] [PubMed] [Google Scholar]
- 13. Van de, Werf F, Bax J, Betriu A, et al. Management of acute myocardial infarction in patients presenting with pesistent ST-segment elevation. Eur Heart J 2008; 29: 2909–2945 [DOI] [PubMed] [Google Scholar]
- 14. De Luca G, Gibson CM, Bellandi F, et al. Early glycoprotein IIb-IIIa inhibitors in primary angioplasty (EGYPT) cooperation. An individual patients’ data meta-analysis. Heart 2008; 94: 1548–1558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Herrmann HC, Lu J, Brodie BR, et al. FINESSE Investigators. Benefit of facilitated percutaneous coronary intervention in high-risk ST-segment elevation myocardial infarction patients presenting to nonpercutaneous coronary intervention hospitals. JACC Cardiovasc Interv 2009; 2: 917–924 [DOI] [PubMed] [Google Scholar]
- 16. Bainey KR, Fu Y, Wagner GS, et al. Spontaneous reperfusion in ST-elevation myocardial infarction: comparison of angiographic and electrocardiographic assessments. Am Heart J 2008; 156; 156: 248–255 [DOI] [PubMed] [Google Scholar]
- 17. Heestermans T, de Boer MJ, van Werkum JVV, et al. Higher efficacy of pre-hospital tirofiban with longer pre-treatment time to primary PCI. Protection for the negative impact of time delay. EuroIntervention 2011; 7: 442–448 [DOI] [PubMed] [Google Scholar]
- 18. Zeymer U, Arntz H-R, Mark B, et al. Efficacy and safety of a high loading dose of clopidogrel administered prehospitally to improve primary percutaneous coronary intervention inacute myocardial infarction: the randomized CIPAMI trial. Clin Res Cardiol 2012; 101: 305–312 [DOI] [PubMed] [Google Scholar]


