Abstract
Background:
Few data are available concerning the impact of gender on temporal trends in patients with acute ST-segment elevation myocardial infarction (STEMI).
Methods:
All STEMI patients consecutively enrolled in the AMIS (Acute Myocardial Infarction in Switzerland) Plus project from 1997–2011 were included. Temporal trends in presentation, treatment and outcomes were analyzed using multiple logistic regressions with generalized estimations.
Results:
Of 21,620 STEMI patients, 5786 were women and 15,834 men from 78 Swiss hospitals. Women were 8.6 years older, presented 48 minutes later with less pain, but more dyspnea, and more frequently had atrial fibrillation (5.5 vs. 3.9%, p<0.001), heart failure (Killip class >2) (9.7 vs. 7.3%, p<0.001), and moderate or severe comorbidities (24.8 vs. 18.2%, p<0.001). Women were less likely to undergo primary reperfusion treatment after adjustment for baseline characteristics and admission year (OR 0.80, 95% CI 0.71–0.90, p<0.001) or receive early and discharge drugs, such as thienopyridines, angiotensin-converting-enzyme inhibitors, angiotensin II receptor antagonists, and statins. In 1997, thrombolysis was performed in 51% of male and 39% of female patients; its use rapidly decreased during the 1990s and has now become negligible. Primary percutaneous coronary intervention increased from under 10% in both genders in 1997 to over 70% in females and over 80% in males since 2006. Patients admitted in cardiogenic shock increased by 8% per year in both genders. The incidence of both reinfarction and cardiogenic shock developing during hospitalization decreased significantly over 15 years while in-hospital mortality decreased from 10 to 5% in men and from 18 to 7% in women. This corresponds to a relative reduction of 5% per year for males (OR 0.95, 95% CI 0.92–0.99, p=0.006) and 6% per year for female STEMI patients (OR 0.94, 95% CI 0.91–0.97, p<0.001). Despite higher crude in-hospital mortality, female gender per se was not an independent predictor of in-hospital mortality (OR 1.07, 95% CI 0.84–1.35, p=0.59).
Conclusion:
Substantial changes have occurred in presentation, treatment, and outcome of men and women with STEMI in Switzerland over the past 15 years. Although parallel trends were seen in both groups, ongoing disparities in certain treatments remain. However, these did not translate into worse risk-adjusted in-hospital mortality, suggesting that the gender gap in STEMI care may be closing.
Keywords: Acute myocardial infarction, evidence-based medicine, primary angioplasty, sex, trends
Introduction
Numerous advances in the treatment of acute ST-elevation myocardial infarction (STEMI) have occurred over the last few decades. In the early 1980s, acute reperfusion therapy with fibrinolytic agents was first introduced along with aspirin therapy and beta-blockers.1 Subsequent clinical trials in the 1990s first began to demonstrate the superiority of primary percutaneous coronary intervention (PCI) as an alternative method for acute reperfusion therapy when performed in a timely manner and by experienced operators.2,3 Thanks to the Stent for Life initiative of the European Association for Percutaneous Cardivascular Intervention (EAPCI) and the Working Group on Acute Cardiac Care (ESC), primary PCI has already become the dominant reperfusion therapy in the majority of European countries.4 The management of STEMI has advanced even further in recent years and now includes additional treatments as well, including dual antiplatelet therapy with thienopyridines, early statin use, and angiotensin-converting-enzyme (ACE) inhibitors and angiotensin-II receptor (AT) antagonists in selected patients.5–7
Despite these advances, STEMI remains an important cause of mortality and morbidity in the general population worldwide, and the application of evidence-based therapies for STEMI patients in real-world practice continues to be inconsistent.8 This last concern is particularly true for specific populations, such as women, where disparities in care have been shown in earlier studies.9–11 Whether such disparities between men and women are decreasing over time is uncertain but they are important for policymakers and providers to understand as the number of evidence-based therapies has grown. If disparities remain, then areas of focus could be identified for future quality improvement efforts within organized STEMI systems of care. A specific challenge to understanding this issue is finding comprehensive, national data sources that also include detailed clinical information. A recent Swedish study evaluated gender differences in treatment and outcome of STEMI patients in 1998–2000 vs. 2004–2006.12 A newer study from a nationwide STEMI network program in Belgium evaluated changes in reperfusion therapy and outcome between 2007–2008 and 2009–2010.13
Accordingly, we used the Acute Myocardial Infarction in Switzerland (AMIS) Plus registry to evaluate temporal trends in presentation, treatment, and outcome in men and women with STEMI in Switzerland between 1997 and 2011. The advantages of the AMIS Plus registry include its inclusiveness and rich data sources that allow for detailed assessments of processes of care and in-hospital outcomes. Further, use of the AMIS Plus registry provides insights into these trends in STEMI patients from central Europe, an area of the world that is relatively underrepresented in earlier studies.
Methods
The AMIS Plus project founded in 1997 is an ongoing nationwide prospective registry of patients admitted with ACS to hospitals in Switzerland with the goal to understand the transfer, use, and practicability of knowledge gained from randomized trials and to generate input for subsequent prospective and randomized studies. Details have been previously published.14–17 From 106 hospitals treating ACS in Switzerland, 78 hospitals temporarily or continuously enrolled patients in AMIS Plus. Participating centers, ranging from community institutions to large tertiary facilities, provided blinded data for each patient through standardized internet- or paper-based questionnaires using the most up-to-date information technology. Participating centers are strongly encouraged to enrol all patients fulfilling the inclusion criteria to avoid selection bias. Hospital data were provided and completed by the treating physician or a trained study nurse. All data were checked for completeness, plausibility, and consistency by the AMIS Plus Data Center in the Institute of Social and Preventive Medicine at the University of Zurich and treating physicians or study nurses were queried when necessary. The registry was approved by the Supra-Regional Ethics Committee for Clinical Studies, the Swiss Board for Data Security, and the Cantonal Ethics Commissions. The AMIS Plus project was officially supported by the Swiss Societies of Cardiology, Internal Medicine, and Intensive Care Medicine.
The questionnaire had 230 items that addressed medical history, comorbidities, known cardiovascular risk factors, clinical presentation, out-of-hospital management, early in-hospital management, reperfusion therapy, hospital course, used or planned diagnostic tests, length of stay, discharge medication, and discharge destination. Patients were enrolled in the registry on the basis of their final diagnosis.
In this study, the following therapies were studied: immediate drug (defined as therapy received within 24 hours after admission), reperfusion (thrombolysis or primary PCI), and discharge medication. Risk factors were documented in the patient’s medical history: dyslipidemia, arterial hypertension and diabetes were assigned if the patient had been previously treated and/or diagnosed by a physician. Documentation of the risk factors provided by the local physicians was accepted as stated. Patients were defined as obese if the body mass index was ≥30 kg/m2 and as smokers if the patient was a smoker at the time of the cardiovascular event. Comorbidities of the patients were assessed using the Charlson index.18 Reinfarction was defined as clinical signs or symptoms of ischemia with ECG changes indicative of new ischemia (new ST-changes or new left bundle branch block) and a re-rise of biomarkers following the initial infarction. A cerebrovascular event was defined as any event due to ischemic, thrombotic, or hemorrhagic disturbances confirmed by a neurologist or imaging modality.
The primary outcome measure was in-hospital mortality. Secondary outcome measures were the rates of in-hospital major adverse cardiac or cerebrovascular events, defined as a composite endpoint of mortality, reinfarction, and cerebrovascular events.
Patient selection
The present analysis included all patients enrolled in AMIS Plus between January 1997 and December 2011, with STEMI defined by characteristic symptoms and/or ECG changes and cardiac marker elevation (either total creatine kinase or creatine kinase MB fraction at least twice the upper limit of normal or troponin I or T above individual hospital cut-off levels for myocardial infarction) and ST-segment elevation and/or new left bundle branch block on the initial ECG.
Statistical analysis
The results are presented as percentages for categorical variables and analyzed using the non-parametric Pearson χ2 test or Fisher’s Exact test as appropriate. Continuous normally distributed variables are expressed as mean±1 standard deviation and compared using the Student’s two-tailed unpaired t-test. Continuous non-normally distributed variables are expressed as median and interquartile ranges and analyzed using the Mann–Whitney U test. To analyze temporal trends of continuous variables the Spearman rank correlation and linear regression were used. A probability value <0.05 was considered significant.
Temporal trends in treatment and outcomes were calculated using multiple logistic regression models. These models determined the use of immediate reperfusion and the early administration of evidence-based drugs according to gender, and included the following variables: age, Killip class >2, the risk factors smoking, dyslipidemia, hypertension, and diabetes, Charlson comorbidity weighted index >2, and admission year. To determine in-hospital mortality predictors, a multivariate logistic regression model included the following variables: age, sex, Killip class >2, the risk factors smoking, dyslipidemia, hypertension, and diabetes, Charlson comorbidity weighted index >2, and admission year. To address clustering of patients within hospitals, logistic regressions with robust standard error and hospital ID as cluster were performed to analyze the effect of gender treatment used and the effect of different covariables on in-hospital mortality using Stata 11.2 (StataCorp, College Station, TX, USA).19,20
SPSS software (version 19; SPSS, Chicago, IL, USA) was used for all other statistical analyses.
Results
Between 1997 and 2011, a total of 21,620 patients with STEMI were enrolled in the AMIS Plus registry. Of these, 5786 (27%) were females and 15,834 (73%) were males. Baseline characteristics are shown in Table 1. Compared with men, women were 8.6 years older (71.5±12.6 vs. 62.9±13.0 years) with increased comorbidities (Charlson Index ≥2 24.8 vs. 18.3%, p<0.001). Women had more frequently diabetes (22.4 vs. 17.3%, p<0.001) and hypertension (65.0 vs. 50.8%, p<0.001), but similar frequencies of coronary artery disease (30.1 vs. 31.5%, p=0.08). Women with STEMI presented 48 minutes later with less pain (85.2 vs. 88.4%, p<0.001) and more dyspnea (32.9 vs. 25.3%, p<0.001), had more frequently Killip class >2 (9.7 vs. 7.3%, p<0.001) and atrial fibrillation (5.5 vs. 3.9%, p<0.001). Men with STEMI had more frequently dyslipidemia (53.8 vs. 49.8%, p<0.001), were more often current smokers (46.3 vs. 29.9%, p<0.001), and were more likely to have resuscitation prior to admission (6.3 vs. 5.3%, p=0.004).
Table 1.
Baseline characteristics of patients admitted with ST-elevation myocardial infarction according to gender (n=21,620)
| Male | Female | p-value | |
|---|---|---|---|
| Patients | 15,834 (73) | 5786 (27) | |
| Age (years) | 62.9±13.0 | 71.5±12.6 | <0.001 |
| Delay (h:min) | 3:10 (1:40 to 8:00) | 3:58 (2:01 to 10:23) | <0.001 |
| Resuscitation prior admission | |||
| Cardiopulmonary resuscitation | 737/15,466 (4.8) | 218/5648 (3.9) | 0.005 |
| Cardioversion/defibrillation | 805/15,382 (5.2) | 216/5620 (3.8) | <0.001 |
| Symptoms at admission | |||
| Pain | 13,569/15,346 (88.4) | 4778/5608 (85.2) | <0.001 |
| Dyspnea | 3562/14,067 (25.3) | 1707/5190 (32.9) | <0.001 |
| Vital signs at admission | |||
| Systolic blood pressure (mmHg) | 133.5±27.5 | 134.4±30.0 | 0.06 |
| Heart rate (beats/min) | 78.2±20.1 | 80.8±21.9 | <0.001 |
| Systolic blood pressure ≤90 mmHg | 815/15,628 (5.2) | 400/5724 (7.0)) | <0.001 |
| Heart rate >100 beats | 1722/15,609 (11.0) | 843/5735 (14.7) | <0.001 |
| Heart rhythm | |||
| Sinus rhythm | 12,225/13,206 (92.6) | 4303/4757 (90.5) | <0.001 |
| Atrial fibrillation | 510/13,206 (3.9) | 264/4757 (5.5) | <0.001 |
| Killip class | n=15,643 | n=5709 | |
| I | 12,408 (79.3) | 4060 (71.1) | <0.001 |
| II | 2090 (13.4) | 1096 (19.2) | |
| III | 549 (3.5) | 329 (5.8) | |
| IV | 596 (3.8) | 224 (3.9) | |
| Risk factors | |||
| Smoking | 6805/14,691 (46.3) | 1553/5192 (29.9) | <0.001 |
| Dyslipidemia | 7593/14,112 (53.8) | 2453/4925 (49.8) | <0.001 |
| Hypertension | 7593/14,935 (50.8) | 3573/5499 (65.0) | <0.001 |
| Diabetes | 2623/15,149 (17.3) | 1230/5494 (22.4) | <0.001 |
| Obesity | 2407/12,830 (18.8) | 820/4361 (18.8) | 0.95 |
| Coronary artery disease | 4488/14,269 (31.5) | 1567/5201 (30.1) | 0.08 |
| Charlson weighted index | n=11,373 | n=4084 | |
| 0 (no comorbidities) | 6922 (60.9) | 2128 (52.1) | <0.001 |
| 1 | 2371 (20.8) | 944 (23.1) | |
| 2 | 983 (8.6) | 495 (12.1) | |
| ≥3 | 1097 (9.6) | 517 (12.7) | |
Values are mean±SD, median (interquartile range), n/total (%), or n (%).
The percentage of female STEMI patients remained relatively constant during the examined period of 15 years (OR 0.99, 95% CI 0.98–1.00, p=0.21). The mean age of male STEMI patients decreased slightly (regression coefficient B −0.06/year, 95% CI −0.14 to −0.02/year, p=0.16), but there was no change seen for female patients (B +0.02/year, 95% CI −0.11 to +0.14/year, p=0.79). The percentage of patients who presented with cardiogenic shock increased per year in both genders (male: OR 1.08, 95% CI 1.03–1.13, p=0.003; female: OR 1.08, 95% CI 1.03–1.12, p=0.001), whereas those with moderate to severe comorbidities (Charlson weighted index ≥2) slightly decreased in males (OR per year 0.98, 95% CI 0.96–1.00, p=0.09), but not in females (OR per year 1.00, 95% CI 0.97–1.04, p=0.97).
Delay between symptom onset and admission decreased between 1997 and 2011 in both gender significantly: in males from 218 min (IQR 120–640) to 169 min (IQR 100–375, p<0.001) and in females from 287 min (IQR 136–870) to 207 min (IQR 120–418min, p<0.001).
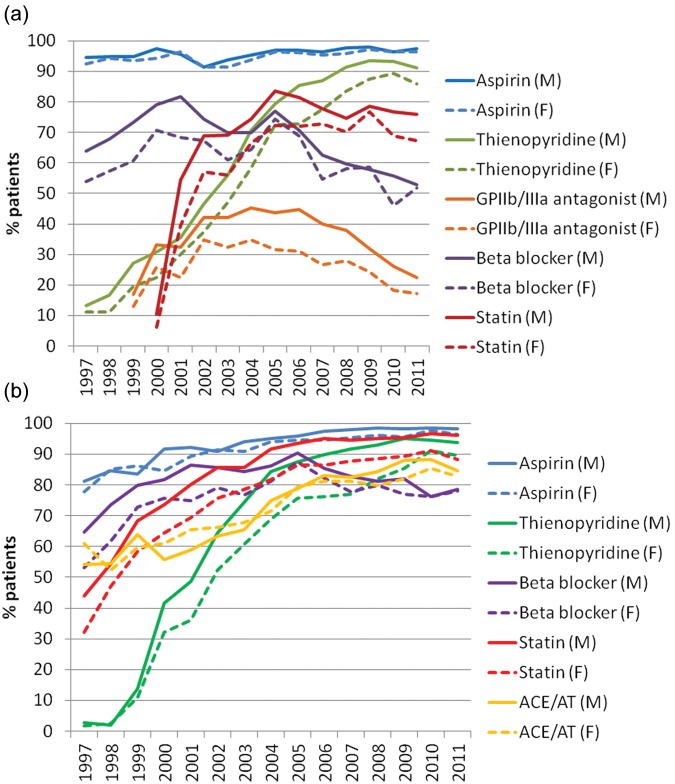
Trends in therapies
Female STEMI patients were less likely to undergo primary reperfusion (thrombolysis or PCI) than their male counterparts (62.2 vs. 75.9%, OR 0.52, 95% CI 0.49–0.56, p<0.001) even after adjustment for baseline characteristics and admission year (OR 0.80, 95% CI 0.71–0.90, p<0.001). After adjustment for all differences, female patients with STEMI were also less likely to receive most early and discharge drug therapies, such as thienopyridines, ACE inhibitors, and/or AT antagonists or statins (Figure 1).
Figure 1.
Adjusted OR for immediate therapies (A) and discharge drugs (B) received by female patients with acute ST-segment elevation myocardial infarction (reference group: male). Adjusted for age, Killip classes>2, risk factors (smoking, dyslipidemia, hypertension, diabetes) and comorbidities (Charlson weighted index ≥2) and admission year
Primary reperfusion, thrombolysis or primary percutaneous coronary intervention; ACE, angiotensin-converting enzyme; AT, angiotensin-II receptor; LMWH, low-molecular-weight heparin.
About 25–32% of patients needed to be transferred for intervention and this percentage did not change during the examined period.
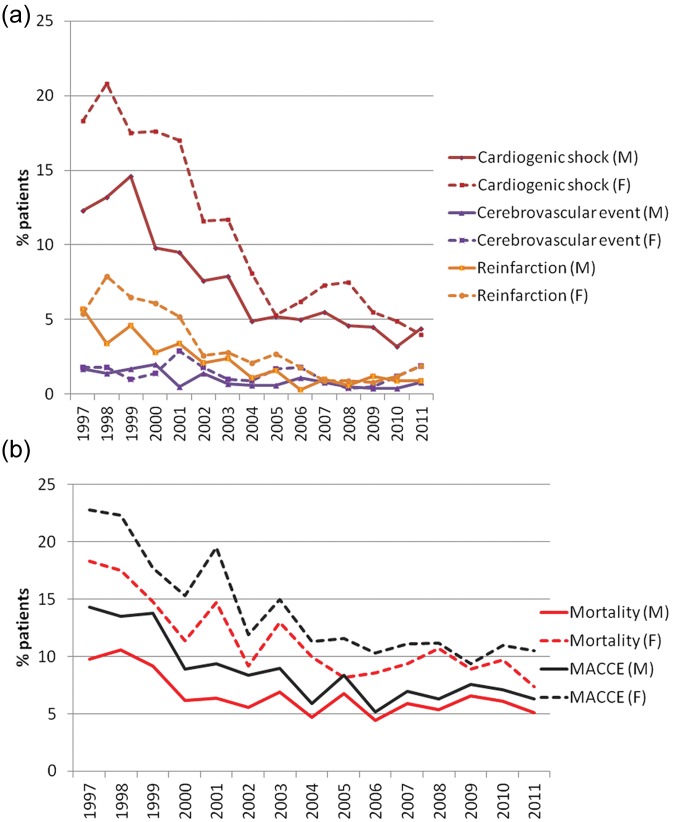
In 1997, thrombolysis was performed in 51% of male and 39% of female STEMI patients. This decreased continuously and was negligible in the last few years. In contrast, from 1997 to 2006, primary PCI was performed increasingly in both genders, from under 10% to over 70% in females and over 80% in males and since then has remained relatively constant (Figure 2).
Figure 2.
Trends in reperfusion therapies in male and female patients with acute ST-segment elevation myocardial infarction in Switzerland between 1997 and 2011
F, female; M, male; PCI, primary percutaneous coronary intervention.
Door-to-balloon time for primary PCI decreased between 2000 and 2011 for male STEMI patients from 51 min (IQR 29–135) to 43 min (IQR 16–90, p<0.001) and more prominently for females from 80 min (IQR 26–237) to 48 min (IQR 18–97, p<0.001). Therefore, the difference between men and women was no longer significant in 2011 (p=0.48).
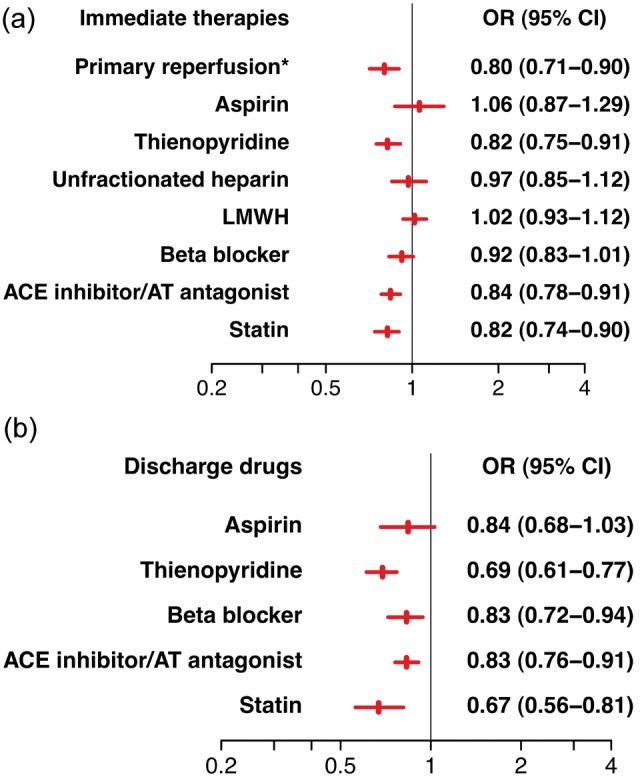
The trends in early drug therapy are depicted in Figure 3a. Thienopyridine use as early drug therapy consistently increased. Since 2008, it was administered to over 90% of males and over 80% in females. Early statin use increased rapidly up until 2002, with a peak use of 72% in females and 82% in males in 2005–2006. Afterwards there was a slight decrease in statin use within the first 24 hours.
Figure 3.
Trends in immediate (A) and discharge (B) drug therapies in male and female patients with acute ST-segment elevation myocardial infarction in Switzerland between 1997 and 2011
ACE, angiotensin-converting enzyme; AT, angiotensin-II receptor; F, female; GP, glycoprotein; M, male;
However, since 2008, the prescription of statins at discharge has continuously increased to over 95% in men and 89% in women. Thienopyridine use at discharge also increased and was prescribed to over 92% of all STEMI patients in 2011 (Figure 3b).
In-hospital outcome
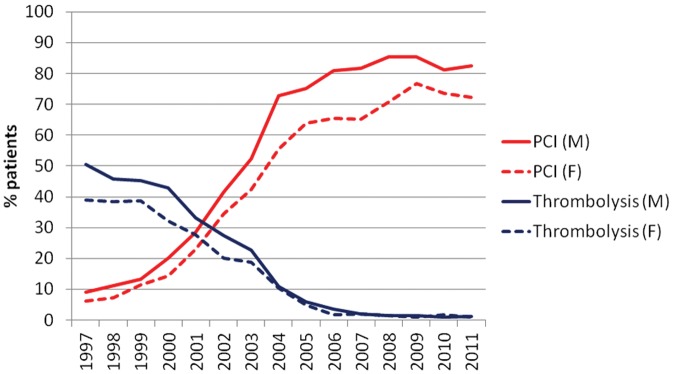
Overall, female STEMI patients had a higher rate of complications and higher crude in-hospital mortality. However, cardiogenic shock developing during hospitalization and reinfarction decreased significantly during these 15 years in both genders (all p<0.001; Figure 4a).
Figure 4.
Trends in complications during hospitalization (cardigenic shock, reinfarction, and cerebrovascular events; A) and in crude mortality and major adverse cardiac and cerebrovascular events (B) in male and female patients with acute ST-segment elevation myocardial infarction in Switzerland between 1997 and 2011
The duration of hospital stay decreased from 10 days for men and 12 days for women in 1997–1998 to 4 days and 6 days, respectively, in the last 3 years (both p<0.001).
Trends in crude in-hospital mortality in both genders are shown in Figure 4b. Over 15 years, crude in-hospital mortality decreased from 10 to 5% in men and from 18 to 7% in women. This corresponds to a relative reduction of 5% per year for males (OR 0.95, 95% CI 0.92–0.99, p=0.006) and 6% per year for female STEMI patients (OR 0.94, 95% CI 0.91–0.97, p<0.001). Female gender was not an independent predictor of in-hospital mortality (OR 1.07, 95% CI 0.84–1.35, p=0.59; Table 2).
Table 2.
Independent predictors for in-hospital mortality in patients with acute ST-segment elevation myocardial infarction
| OR | 95% CI | p-value | |
|---|---|---|---|
| Female gender | 1.07 | 0.84–1.35 | 0.59 |
| Age | 1.07 | 1.06–1.09 | <0.001 |
| Killip class >2 | 7.63 | 5.48–10.63 | <0.001 |
| Smoking | 1.30 | 1.03–1.64 | 0.028 |
| Dyslipidemia | 0.89 | 0.71–1.11 | 0.31 |
| Hypertension | 0.77 | 0.67–0.89 | <0.001 |
| Diabetes | 1.13 | 0.85–1.50 | 0.40 |
| Charlson weighted index ≥2 | 1.94 | 1.58–2.38 | <0.001 |
| Admission year | 0.97 | 0.92–1.01 | 0.052 |
Discussion
Our study has several key findings. First, in-hospital mortality has been halved among men and women with STEMI during the last 15 years in Switzerland. Furthermore, we identified important overall trends in the presentation and treatment in both gender. It is noteworthy, for example, that we found women presented at an older age, after greater delay, and in a sicker condition overall. These findings are consistent with work in other regions of the world.21
Second, the baseline characteristics of the STEMI patients changed in both genders during the observed period of 15 years. The mean age of women remained the same during this period, but male patients became slightly younger. In addition, a growing proportion of STEMI patients were admitted in cardiogenic shock, increasing between 1997 and 2011 in both genders to 8% per year. This could be related to better STEMI patient selection leading to a reduction in out-of-hospital deaths. Rates of cardiogenic shock at admission in ACS patients remained constant up until 2006.14
Finally, we found that important differences between men and women persisted when we examined treatment patterns. Women were significantly less likely to receive primary reperfusion and evidence-based therapies. Yet these differences in treatment did not translate into higher risk-adjusted mortality among women.
These findings complement and extend work by other groups. Between 1995 and 2006, for example, risk-standardized 30-day mortality rates among over 2.7 million elderly patients discharged with acute myocardial infarction in the USA showed a significant decrease.22 However, this study used administrative data and was unable to reliably distinguish between improvements in mortality related to STEMI as opposed to non-STEMI. In contrast, Yeh and colleagues reported that 30-day mortality improved in a large community-based population from Northern California over a similar time period for non-STEMI but not STEMI patients.23 A prospective observational cohort study from the SWEDEHEART registry evaluated gender differences in treatment and outcome between the two periods 1998–2000 and 2004–2006 and found reduced mortality but a persistent gender gap.12 In the latest Euro Heart Survey for acute coronary syndromes, improvements in in-hospital mortality were also seen between 2006 and 2008 among STEMI patients at 138 centers in 21 countries.24 These findings point toward general improvements in STEMI care and were accompanied by increases in the number of patients receiving reperfusion therapy, the proportion receiving primary PCI, and the timeliness of instituting treatments.
Our study showed a dramatic decrease in early mortality, in cardiogenic shock developing in hospital as well as in the reinfarction rates for both gender. Differences existed between the two groups at baseline, despite favourable changes for both men and women. For comparison, investigators from Denmark recently reported that trends in acute myocardial infarction over the last 25 years now suggest similar short- and long-term outcomes in men and women over the last several years25 – a finding that is consistent with our results – yet this study used administrative data and was unable to look at measures of processes of care, such as the use of evidence-based therapies. Thus, our findings still support the conclusions of the EuroHeart project in 2010 that highlighted ongoing disparities between men and women in cardiovascular care and also pushed for understanding reasons behind this complex phenomenon.26
A contemporary report from Canada, for example, suggested underutilization of evidence-based therapies among women were related to the patient (e.g. age), consequences of the disease (e.g. heart failure), and the physician’s assessment of patient risk.27 Finally, Canto and colleagues recently described findings from over 1 million patients in the National Registry for Myocardial Infarction (NRMI) in the USA from 1994 to 2006. In this study, a large proportion of women (~40%) presented without chest pain and had worse outcome than men – although these differences were attenuated in older age groups.28 Our study extends earlier work by systematically examining differences between these two groups as well as trends over a long period of time with more current data and in a single European healthcare system, as opposed to a series of ‘snapshots’.
What are the implications of our findings? We believe that it highlights both recent successes in diminishing disparities between men and women while also pointing out ongoing opportunities for further improvement. An important example of ongoing opportunities might be seen in the use of statin therapy, which was consistently lower in women than men. Future programs might target women specifically to understand barriers and to ensure that initiation of statin therapy occurs ideally within the hospital setting before discharge. However, a lack of differences in in-hospital mortality supports the notion that we have made substantial strides as well and that clinicians are making reasonable decisions in many circumstances. As future work progresses in this area, greater understanding of gender differences in psychosocial factors, cardiovascular risk factors, pathophysiological factors, and responses to both invasive and medical treatments will be needed.
Our study should be interpreted in the context of the following limitations. First, this study is an observational report with temporal and regional heterogeneity of the data. Although it included most of the hospitals in Switzerland, it was a voluntary program focused on a quality improvement initiative. It therefore may represent those facilities with a greater desire to benchmark their results in comparison with other hospitals. Second, the healthcare system in Switzerland differs from other European countries and the USA, making these findings difficult to generalize to other settings. Third, we tried to account for confounders that changed over time, including using total creatine kinase for the diagnosis of acute STEMI in the early period of our study. While our multivariable models included a number of factors, it is likely that some other important conditions that might explain differences between men and women may have been excluded. Furthermore, there was no long-term follow up. However, the large number of patients and continuity of the AMIS Plus data collection allowed a contemporary view of the development of STEMI treatment over a long time period in Switzerland.
In summary, we found that in-hospital mortality has been halved and that substantial changes have occurred in treatment of STEMI among both men and women in Switzerland over the last 15 years. For the most part, trends developed in parallel across the two groups, although ongoing disparities in treatments remain. These disparities in treatment, however, are not associated with worse risk-adjusted outcomes, suggesting that the gender gap may be closing.
Supplementary Material
Acknowledgments
We thank Jenny Piket for proofreading this manuscript. For full details of Centres participating in AMIS Plus 1997–2011 please see the supplementary material. ClinicalTrials.gov identifier: NCT01305785.
Footnotes
Funding: The AMIS Plus registry was supported by unrestricted grants from the Swiss Heart Foundation and from Abbot, Switzerland, Astra-Zeneca, Switzerland, Bayer Schering, Switzerland, Biotronik, Switzerland, Bristol-Myers Squibb, Switzerland, Daiichi-Sankyo/Lilly, Switzerland, Johnson & Johnson – Cordis Division, Switzerland, A Menarini, Switzerland, Merck Sharp & Dohme-Chibret, Switzerland, Medtronic, Switzerland, Pfizer, Switzerland, St Jude Medical, Switzerland, and Takeda Pharma, Switzerland.
Conflict of interest: The sponsors did not play any role in the design, data collection, analysis, or interpretation of the registry. The authors declare no conflict of interest.
References
- 1. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Lancet 1994; 343: 311–322 [PubMed] [Google Scholar]
- 2. Bates ER, Nallamothu BK. Commentary: the role of percutaneous coronary intervention in ST-segment-elevation myocardial infarction. Circulation 2008; 118: 567–573 [DOI] [PubMed] [Google Scholar]
- 3. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003; 361: 13–20 [DOI] [PubMed] [Google Scholar]
- 4. Widimsky P, Kristensen SD. Stent for Life Initiative: where are we standing and where are we going? EHJ ACC 2012; 1: 48–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, writing on behalf of the 2004 Writing Committee. Circulation 2008; 117: 296–329 [DOI] [PubMed] [Google Scholar]
- 6. Kushner FG, Hand M, Smith SC, Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009; 54: 2205–2241 [DOI] [PubMed] [Google Scholar]
- 7. Van de, Werf F, Bax J, Betriu A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology. Eur Heart J 2008; 29: 2909–2945 [DOI] [PubMed] [Google Scholar]
- 8. Mandelzweig L, Battler A, Boyko V, et al. The second Euro Heart Survey on acute coronary syndromes: Characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 2006; 27: 2285–2293 [DOI] [PubMed] [Google Scholar]
- 9. Nallamothu BK, Blaney ME, Morris SM, et al. Acute reperfusion therapy in ST-elevation myocardial infarction from 1994–2003. Am J Med 2007; 120: 693–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med 2005; 353: 671–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Radovanovic D, Erne P, Urban P, et al. Gender differences in management and outcomes in patients with acute coronary syndromes: results on 20,290 patients from the AMIS Plus Registry. Heart 2007; 93: 1369–1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lawesson SS, Alfredsson J, Fredrikson M, et al. Time trends in STEMI – improved treatment and outcome but still a gender gap: a prospective observational cohort study from the SWEDEHEART register. BMJ Open 2012; 2: e000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Claeys MJ, Sinnaeve PR, Convens C, et al. STEMI mortality in community hospitals versus PCI-capable hospitals: results from a nationwide STEMI network programme. EHJ ACC 2012; 1: 40–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jeger RV, Radovanovic D, Hunziker PR, et al. Ten-year trends in the incidence and treatment of cardiogenic shock. Ann Intern Med 2008; 149: 618–626 [DOI] [PubMed] [Google Scholar]
- 15. Radovanovic D, Erne P. AMIS Plus: Swiss registry of acute coronary syndrome. Heart 2010; 96: 917–921 [DOI] [PubMed] [Google Scholar]
- 16. Radovanovic D, Urban P, Simon R, et al. Outcome of patients with acute coronary syndrome in hospitals of different sizes. A report from the AMIS Plus Registry. Swiss Med Wkly 2010; 140: 314–322 [DOI] [PubMed] [Google Scholar]
- 17. Schoenenberger AW, Radovanovic D, Stauffer JC, et al. Age-related differences in the use of guideline-recommended medical and interventional therapies for acute coronary syndromes: a cohort study. J Am Geriatr Soc 2008; 56: 510–516 [DOI] [PubMed] [Google Scholar]
- 18. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383 [DOI] [PubMed] [Google Scholar]
- 19. Rogers WH. Regression standard errors in clustered samples. Stata Technical Bulletin 1993; 13: 19–23 [Google Scholar]
- 20. Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics 2000; 56: 645–646 [DOI] [PubMed] [Google Scholar]
- 21. Maas AH, van der Schouw YT, Regitz-Zagrosek V, et al. Red alert for women’s heart: the urgent need for more research and knowledge on cardiovascular disease in women: proceedings of the workshop held in Brussels on gender differences in cardiovascular disease, 29 September 2010. Eur Heart J 2011; 32: 1362–1368 [DOI] [PubMed] [Google Scholar]
- 22. Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA 2009; 302: 767–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362: 2155–2165 [DOI] [PubMed] [Google Scholar]
- 24. Schiele F, Hochadel M, Tubaro M, et al. Reperfusion strategy in Europe: temporal trends in performance measures for reperfusion therapy in ST-elevation myocardial infarction. Eur Heart J 2010; 31: 2614–2624 [DOI] [PubMed] [Google Scholar]
- 25. Schmidt M, Jacobsen JB, Lash TL, et al. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ 2012; 344: e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stramba-Badiale M. Women and research on cardiovascular diseases in Europe: a report from the European Heart Health Strategy (EuroHeart) project. Eur Heart J 2010; 31: 1677–1684 [Google Scholar]
- 27. Bugiardini R, Yan AT, Yan RT, et al. Factors influencing underutilization of evidence-based therapies in women. Eur Heart J 2011; 32: 1337–1344 [DOI] [PubMed] [Google Scholar]
- 28. Canto JG, Rogers WJ, Goldberg RJ, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012; 307: 813–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.