Introduction
More people than ever before are looking to their physicians to help them restore and maintain a youthful appearance. As our understanding of the intrinsic and extrinsic causes of aging expands, numerous minimally and noninvasive procedures have been developed. The use of these procedures extends to the correction of defects caused by disease or scarring.
Last year, the 4,000 members of the American Society for Dermatologic Surgery (ASDS) performed more than eight million procedures. According to ASDS, injectable soft tissue fillers and neuromodulators are two of the five most common procedures (http://www.asds.net/2011-procedures). The American Society for Aesthetic Plastic Surgery reported these as the top two nonsurgical procedures performed in 2011, totaling nearly four million (http://www.surgery.org/sites/default/files/ASAPS-2011-Stats.pdf). The most common adverse events are local injection site reactions1—primarily bruising. One study on injectable fillers reports bruising to occur in 19 to 24 percent of patients2 while others report it as high as 68 percent.3 Here, the authors address the common causes of and techniques to avoid bruising.
Avoiding Bruising
Medications. Prior to any procedure, proper patient selection and preparation can help to reduce the risk of bruising. Many medications can cause increased bleeding and bruising, such as aspirin, clopidogrel, and warfarin, which are some of the more common cardiovascular medications. Other medications that can cause bruising include dabigatran, enoxaparin, ticlopidine, and dipyridamole. Since anticoagulation is often necessary to prevent the occurrence of embolic and thrombotic phenomenon in patients with atrial fibrillation, coagulopathies, and other conditions, it is not recommend to discontinue these medications, but be aware and inform the patient of the increased risk of bruising. Due to the medical necessity of these medications, most dermatological surgeons do not discontinue them, but may ensure that patients on warfarin are not supratherapeutic (international normalized ratio [INR] is not greater than 3.0).4,5 If aspirin is not medically necessary, it should be held for one week prior to any injectable procedure. The patient should also avoid the use of nonsteroidal anti-inflammatory medications for five days prior to any procedures.
The use of herbal supplements and vitamins is becoming more and more common. Many of these have the potential to increase the risk of bruising. In particular, high-dose vitamin E, ginkgo biloba, and garlic have case reports and studies demonstrating increased bleeding and/or bruising. Many physicians recommend that patients stop taking these two weeks prior to any procedures.6
Patient positioning and surroundings. Patients undergoing a cosmetic injection procedure should be positioned properly. They should sit in a chair that is reclined 30° with the head firmly rested against a solid headrest. The hands of the physician should be braced against the patient, thus preventing any unnecessary trauma if the patient were to unexpectedly move. Blood vessels should be avoided by careful inspection of the injection site. The skin of the patient should be clean so makeup or other material does not cover or camouflage the vessels. The room and patient should be well lit and some providers recommend a sidelight on the patient to highlight blue vessels. The use of magnifying loops is helpful in looking for small vessels within the injection site. In addition, a new infrared device (VeinVeiwer® Flex, Christie Digital Systems USA, Inc.), which enhances vessels within 2 to 3mm of the skin surface, may also be useful (Figure 1).
TABLE 1.
Supplements and medications known to increase bruising and techniques to reduce bruising
| SUPPLEMENTS KNOWN TO INCREASE BRUISING | MEDICATIONS KNOWN TO INCREASE BRUISING | TECHNIQUES TO REDUCE BRUISING |
|---|---|---|
| Vitamin E | Aspirin(other salicylates) | Proper preparation of the patient |
| Garlic | Clopidogrel | Careful avoidance of blood vessels |
| Ginko biloba | Warfarin | Use small gauge needles when possible |
| Ibuprofen (other NSAIDS) | Avoid rapid large injections when possible | |
| Dabigatran | Avoid “fanning” injections when possible | |
| Enoxaparin | Compression and ice after the procedure | |
| Dipyridamole | ||
| Ticlopidine | ||
| Some selective serotonin reuptake inhibitors |
Figure 1.
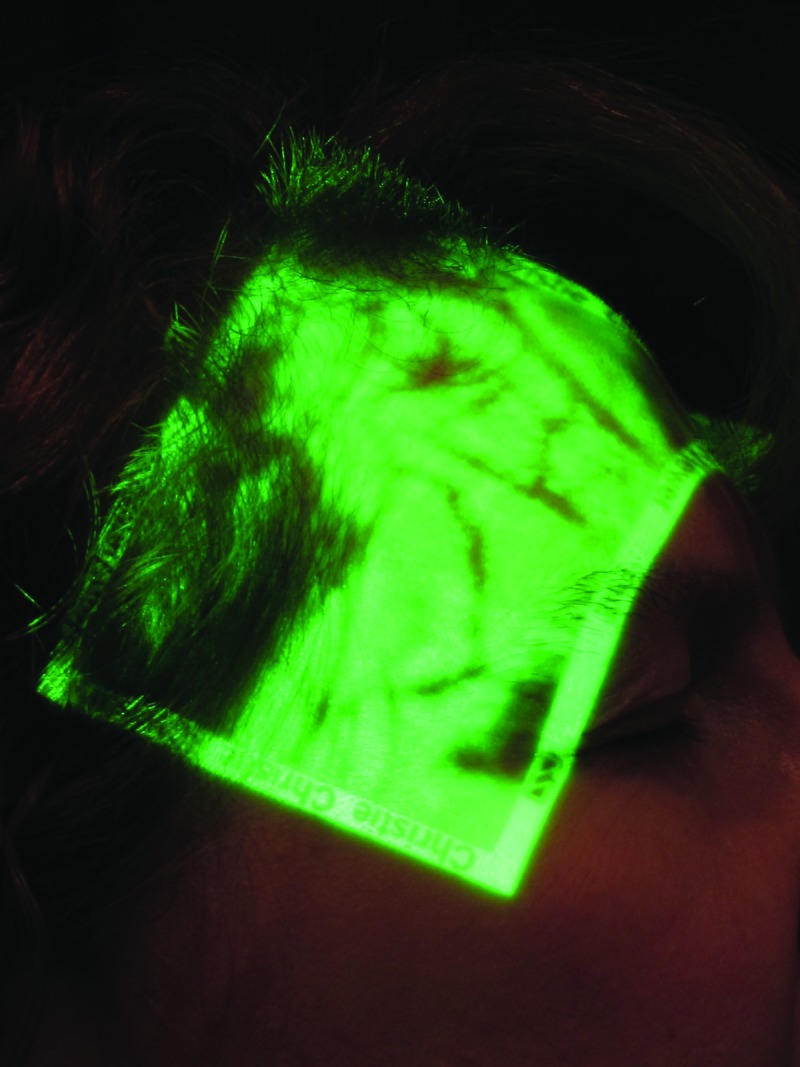

Photo of the right temple with (A) and without (B) VeinVeiwer.
Instrumentation. Using the right instrument can improve outcomes and reduce bruising. Larger cannula needles are more likely to transect blood vessels and cause bruising. Due to particle size, some fillers require the use of larger caliber syringes. When possible, as in the administration of neuromodulating agents, smaller gauge needles (30 gauge) should be used. Smaller needles are not necessary. A comparison study between 30- and 32-gauge needles used to administer botulinum toxin type A did not show a statistically significant difference in the rate of bruising.7 The use of blunt-tipped microcannulas is recommended by some practitioners. Many authors describe their experience of decreased bruising, especially when using a fanning injection technique in the dermis.8-10 Theoretically a blunt tip would be less likely to cut a blood vessel as it is being advanced, and the use of a longer blunt tipped microcannula can result in less entry points into the skin. However, there is not yet a published direct comparison study demonstrating less bruising, and we have found no difference in bruising or efficacy between cannulas and needles.
Injection technique can also be an independent risk factor when delivering fillers. Using a fanning technique increases the risk of bruising when compared to single puncture threading technique or multiple puncture technique.2 Bruising was also more commonly seen in patients who received larger volumes of filler and those whose injections were delivered in less time indicating that both rate of injection and volume are independent risk factors for bruising.
Aftercare. The outcomes of even a perfectly performed procedure can be improved with good aftercare. Immediately after the injection, pressure should be applied to the injection site. Cold compresses can also be applied to encourage vasoconstriction and reduce bruising. There are some data to indicate that topical application of arnica, bromelain, and/or high-dose vitamin K can reduce the formation of ecchymosis and increase the rate of resorbtion.11,12 However, it is not the authors’ practice to routinely use these topical therapies. Finally, a nice “trick” used by one author is to ask the patient food-related questions during and immediately after the procedure. When patients think about food, a relative vasoconstriction of the skin vessels occurs as blood is shunted to the gastric system in anticipation of eating. This relative cutaneous vasoconstriction may minimize slight bruising and bleeding.
Performing cosmetic enhancement procedures through injections of neuromodulators and/or fillers and biostimulatory products plays a large role in the cosmetic practice. Patients who present for these procedures, which are not reimbursable by insurance, do not wish to leave the office with bruising. The authors have found that the primary reason patients choose their physician and/or change physicians to perform injections is based on the degree of bruising by the physician. Carefully performed injections can minimize bruising making for happier patients and physicians.
Footnotes
Disclosures:The authors report no relevant conflicts of interest.
References
- 1.Duffy DM. Complications of fillers: overview. Dermatol Surg. 2005;31(11 Pt 2):1626–1633. doi: 10.2310/6350.2005.31251. [DOI] [PubMed] [Google Scholar]
- 2.Glogau RG, Kane MAC. Effect of injection techniques on the rate of local adverse events in patients implanted with nonanimal hyaluronic acid gel dermal fillers. Dermatol Surg. 2008;34(s1):S105–S109. doi: 10.1111/j.1524-4725.2008.34251.x. [DOI] [PubMed] [Google Scholar]
- 3.Tzikas TL. Evaluation of the radiance FN soft tissue filler for facial soft tissue augmentation. Arch Facial Plast Surg. 2004;6(4):234–239. doi: 10.1001/archfaci.6.4.234. [DOI] [PubMed] [Google Scholar]
- 4.Kirkorian AY, Moore BL, Siskind J, Marmur ES. Perioperative management of anticoagulant therapy during cutaneous surgery: 2005 Survey of Mohs Surgeons. Dermatol Surg. 2007;33(10):1189–1197. doi: 10.1111/j.1524-4725.2007.33253.x. [DOI] [PubMed] [Google Scholar]
- 5.Callahan S, Goldsberry A, Kim G, Yoo S. The management of antithrombotic medication in skin surgery. Dermatol Surg. doi: 10.1111/j.1524-4725.2012.02490.x. 2012:n/a-n/a. [DOI] [PubMed] [Google Scholar]
- 6.Broughton G, II, Crosby MA, Coleman J, Rohrich RJ. Use of herbal supplements and vitamins in plastic aurgery: a practical review. Plast Reconstr Surg. 2007;119(3):48e–66e. doi: 10.1097/01.prs.0000252661.72071.8d. [DOI] [PubMed] [Google Scholar]
- 7.Price KM, Williams ZY, Woodward JA. Needle preference in patients receiving cosmetic botulinum toxin type A. Dermatol Surg. 2010;36(1):109–112. doi: 10.1111/j.1524-4725.2009.01391.x. [DOI] [PubMed] [Google Scholar]
- 8.Fulton J, Caperton C, Weinkle S, Dewandre L. Filler injections with the blunt-tip microcannula. J Drugs Dermatol. 2012;11(9):1098–1103. [PubMed] [Google Scholar]
- 9.Zeichner JA, Cohen JL. Use of blunt tipped cannulas for soft tissue fillers. J Drugs Dermatol. 2012;11(1):70–72. [PubMed] [Google Scholar]
- 10.Niamtu J., III Filler injection with micro-cannula instead of needles. Dermatol Surg. 2009;35(12):2005–2008. doi: 10.1111/j.1524-4725.2009.01323.x. [DOI] [PubMed] [Google Scholar]
- 11.MacKay D, Miller AL. Nutritional support for wound healing. Altern Med Rev. 2003;8(4):359–377. [PubMed] [Google Scholar]
- 12.Leu S, Havey J, White LE, et al. Accelerated resolution of laser-induced bruising with topical 20% arnica: a rater-blinded randomized controlled trial. Br J Dermatol. 2010;163(3):557–563. doi: 10.1111/j.1365-2133.2010.09813.x. [DOI] [PubMed] [Google Scholar]


