Introduction
Occurrence of all clinical manifestations of atherosclerosis increases with age. Aging is also associated with the acquisition of and increments in major modifiable risk factors that contribute to development of cardiovascular disease (CVD). This cluster of CVD risk factors accompanying advancing age could account for much of the rise in CVD incidence as we age. However, multivariable analysis, adjusting for the accompanying burden of risk factors, indicates an independent contribution of age to the development of atherosclerotic CVD. This suggests that the aging process per se promotes atherosclerosis. Nevertheless, it is possible that a considerable proportion of the effect of age on CVD risk may be a reflection of the intensity and duration of exposure to predisposing modifiable CVD risk factors that accompanies aging. If this latter hypothesis is valid, correction or avoidance of these CVD risk factors could allay some of the rise in incidence of CVD with age, as suggested by Sniderman and Furberg in a recent viewpoint in the Lancet.1 Herein we use prospective epidemiologic Framingham study data to investigate if, the age-associated escalation in CVD risk is in fact modifiable, despite the contention that age per se is a non-modifiable risk factor.
Age as an independent CVD risk factor
The Framingham Study has followed a cohort of the town’s population since 1950 gathering data on age-related trends in CVD incidence and life expectancy. Multivariable analysis of the prospective data clearly indicates an independent effect of age on CVD incidence taking all the major risk factors into account. The cardiovascular system is strongly affected by the “aging process”. However, in addition to intrinsic aging, the long-term burden of vascular risk factors also underlies the structural and functional changes in the heart and vessels (referred to as cardiovascular remodeling). Such remodeling of the vessels and the heart eventually leads to CVD morbidity and mortality in the general population. Examination of the risk of CVD in Framingham study participants who were designated as being at low risk by current risk factor guidelines suggests that there is clearly an independent contribution of age to occurrence of atherosclerotic CVD. However, this observation does not factor in the duration of exposure to and the time it takes to acquire established CVD risk factors.
Importance of concomitant burden of other risk factors
Although as noted, there is an independent influence of age on CVD risk, its influence is not uniform. Examination of atherosclerotic CVD incidence in relation to age in the Framingham cohort has revealed that at any age the risk of CVD events varies widely (4- to 5-fold) depending on the burden of accompanying risk factors. In other words, age per se does not pose an invariant risk of CVD at a given age.
Because the Framingham study cohort has been followed biennially for development of atherosclerotic CVD over more than 5 decades, it was possible to estimate the lifetime risk of developing coronary or stroke events.2,3 The lifetime risk of a coronary (47%-31%) or stroke (15%–18%) event in men and women of this cohort was alarmingly high. Examination of the lifetime risk of these CVD events at specified index ages revealed that the lifetime chance of acquiring them decreases with age (comparing lifetime risk in 40- or 50-year individuals with that in 60- or 70-year old people).2 Women had a higher lifetime risk of stroke than men, presumably because of their longer life expectancy.3 The observed decline rather than increase in probability of a CVD event with advancing age may reflect the shrinkage of the time left to acquire it, but it could also support the notion of an inherent resistance to cardiovascular risk factors in survivors to an old age. In other words, if age alone was an overwhelming risk factor for CVD, one would expect the lifetime risk of CVD to continue to escalate with increasing age.
Furthermore, examination of the lifetime risk of coronary disease in relation to multivariable cardiovascular risk tertiles in the Framingham Study has indicated a steep rise in lifetime CHD risk with an increasing burden of risk factors.4 However, the impact of the combined load of risk factors did not increase with age in either sex.4 The fact that the influence of multivariable CVD risk does not increase with age could be due to shorter possible follow-up time in the very old, a greater survival of persons with a lesser burden of cardiovascular risk factors throughout life, or an innate resistance to the effect of risk factors. These findings are consistent with the concept of age as a hazard reflecting the length of exposure to risk factors rather than a diminished capacity to cope with them with advancing age. Genetic influences are likely to play a role, but are currently non-modifiable and the impressive gains in life expectancy in 20th century are certainly not due to changes in genes.
It is important to note that the data cited above analyzed lifetime risk from middle age onwards because the Framingham Study recruited subjects ages 30–62 years at the time of the baseline examination in 1950. This should not be taken to mean that we advocate waiting until middle age before modifying CVD risk factors. Earlier intervention is likely to be even more efficacious in promoting a longer life free of CVD.
Importance of mid-life risk factors and their trajectory
An examination of whether midlife cardiovascular risk factors predict mortality and survival free of major comorbidities to the age of 85 years was undertaken using the Framingham Study cohort data in 2005.5 This prospective community-based cohort study involved 2,531 participants (1,422 women) who attended at least two examinations between the ages of 40 and 50 years. The comorbidities that were examined included myocardial infarction, coronary insufficiency, congestive heart failure, stroke, cancer, and dementia. Stepwise sex-adjusted logistic regression models were used to predict the outcomes of survival and survival free of morbidity to age 85 years stratified by the burden of the following risk factors: systolic and diastolic blood pressure, total serum cholesterol, glucose intolerance, cigarette smoking, education, body mass index, physical activity index, pulse pressure, antihypertensive medication, and electrocardiographic left ventricular hypertrophy.
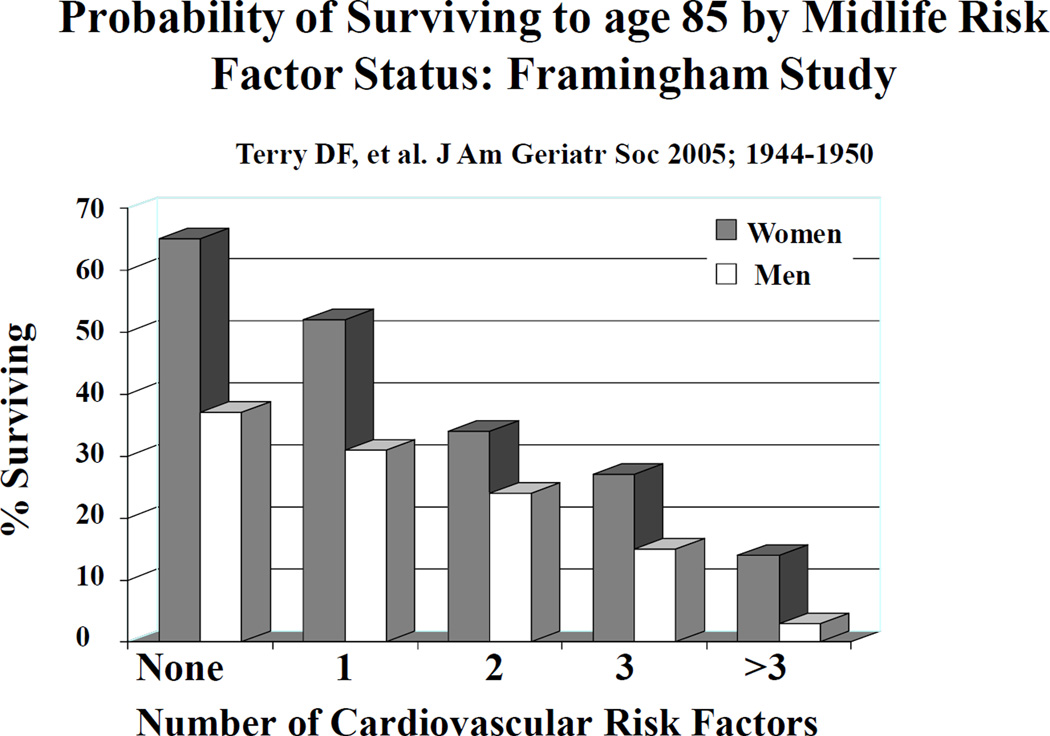
More than one-third of the cohort sample survived to age 85 years, and 22% of the original study sample survived free of morbidity. Lower midlife blood pressure and total cholesterol levels, absence of glucose intolerance, nonsmoking status, higher educational attainment, and female sex predicted favorable overall and morbidity-free survival. The predicted probability of survival to age 85 years fell markedly in the presence of accumulating risk factors: 37% for men with no risk factors to 2% with all five risk factors; 65% for women with no risk factors to 14% with all five risk factors (Figure 1).Clearly, recognizing and modifying CVD risk factors can be expected to delay or prevent age-associated morbidity and mortality.
Figure 1.
Probability of surviving to age 85 years according to number of CVD risk factors in mid-life.
Epidemiological studies have examined factors associated with overall and cause-specific morbidity and mortality but limited data exist about factors associated with longevity. The Framingham study previously examined factors associated with survival to 75 yrs of age in middle-aged men and women. After excluding persons with cancer, CVD, or diabetes, 747 men and 973 women 50 yrs of age at routine clinical examination who could potentially reach 75 yrs of age during follow-up were studied. Logistic regression modeling was used to examine factors associated with survival. Fewer cigarettes smoked per day, systolic blood pressure and higher forced vital capacity were associated with longevity in both sexes. Lower heart rate in men and parental survival to 75 yrs in women were also associated with survival to 75yrs. It was concluded that a number of lifestyles and one familial factor are associated with increased life expectancy and that the data further support the positive impact on life expectancy of health promotional efforts directed at smoking and control of hypertension in middle-aged men and women 6.
The powerful influence of CVD risk factors on longevity was also noted in another population-based study.7 The Honolulu Heart Program tested whether midlife biological, lifestyle, and socio-demographic risk factors are associated with overall survival and exceptional survival (free of a set of major diseases and impairments). A total of 5820 Japanese American middle-aged men (mean age, 54 years) free of morbidity and functional impairments were followed for up to 40 years (1965–2005) to assess overall and exceptional survival. Exceptional survival was defined as survival to a specified age (75, 80, 85, or 90 years) without incidence of 6 major chronic diseases and without physical and cognitive impairment. Of the original participants, 42% survived to age 85 years and 11% met the criteria for exceptional survival to age 85 years. High grip strength and avoidance of overweight, hyperglycemia, hypertension, smoking, and alcohol consumption were associated with both overall and exceptional survival. In addition, higher education and avoidance of hypertriglyceridemia were associated with exceptional survival, and lack of a marital partner was associated with mortality before age 85 years. Risk factor models based on cumulative risk factors (survival risk score) suggest that the probability of survival to oldest age is as high as 69% with no risk factors and as low as 22% with 6 or more risk factors. The probability of exceptional survival to age 85 years was 55% with no risk factors but decreased to 9% with 6 or more risk factors. It was concluded that avoidance of certain risk factors in midlife is associated with the probability of a long and healthy life among men.6
Yashin and coworkers extended these observations on midlife value of CVD risk factors to the age-related trajectories of physiological indices and underscore that such trajectories of CVD risk factors likely contain important information about aging-related changes in the humans and, therefore, may help our understanding of human longevity.8 The authors undertook a study to investigate whether shapes of such trajectories earlier in life affect the residual life span distribution using longitudinal data from the Framingham Study. Seven physiological indices were examined in relation to life spans of participants in the Framingham cohort. These included: diastolic blood pressure, pulse pressure, body mass index, serum cholesterol, blood glucose, hematocrit and heart rate. The investigators developed a method for assigning individuals to groups of potentially long-lived and potentially medium-lived groups using age trajectories of physiological indices at the age interval between 40 and 60 years. The analysis demonstrated that the longevity of individuals who survived to age of 65 years depends on the behavior of the physiological indices between 40 and 60 years of age.7
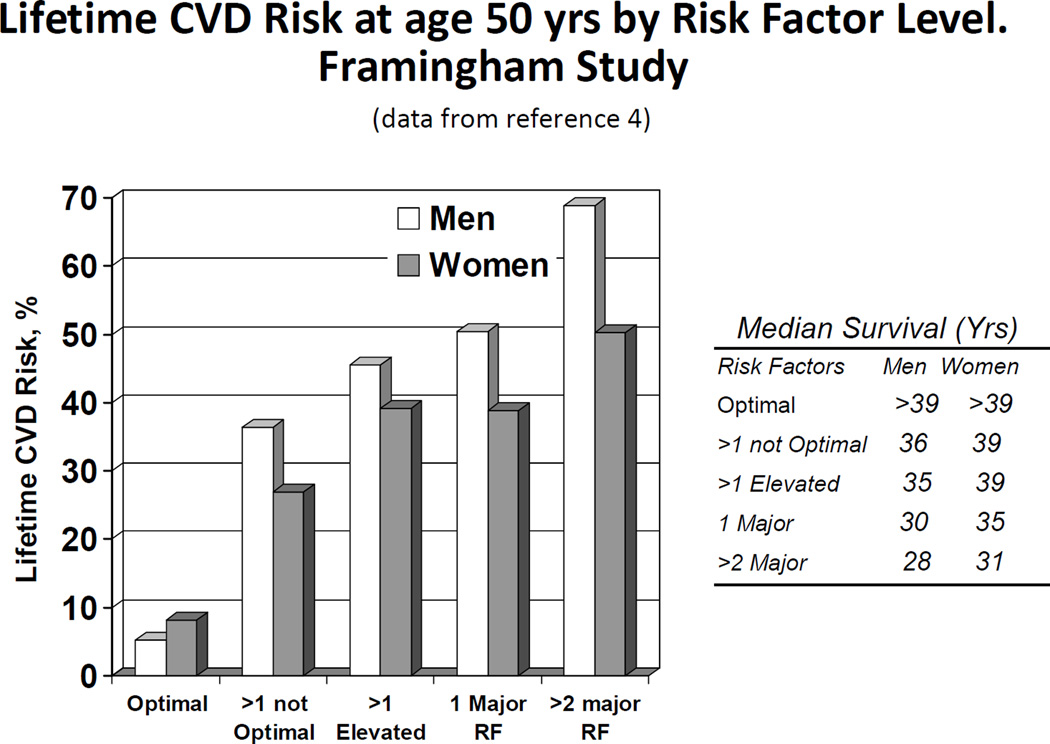
Lloyd-Jones et al in an analysis of Framingham data found that persons who attained age 50 yrs in the Framingham study with optimal risk factors (cholesterol <180 mg/dL, blood pressure <120/80 mm Hg, non-smoker, non-diabetic) were almost immune (5–8%) to development of CVD. Those with 2 or more risk factors had a 50–68% lifetime risk (Figure 2). Median survival for those with optimal risk factors after age 50 yrs was 39 years.4
figure 2.
Lifetime risk of CVD and median survival at age 50 years by risk factor status.
Quantitative estimate of the impact of concomitant risk factors on age effect
An analysis of the effect of age on CVD incidence with and without adjustment for risk factors in each sex in the Framingham cohort provides estimates of the influence of associated CVD risk factors on the age variable.9 Table 1 suggests that in men 11.9% of the influence of age is attributable to accompanying risk factors; in women the corresponding proportion is 40.3%. This is discernable from a comparison of the size of the age coefficients for CVD incidence unadjusted versus that adjusted for associated risk factors (systolic blood pressure, BMI, diabetes, smoking, total and HDL cholesterol). While the chances of achieving advanced age is clearly influenced by susceptibility to CVD promoted by modifiable risk factors, there is clearly a large residual risk imposed by age per se that is currently unexplained. Also the greater proportion of the age effect explained by the burden of risk factors in women than men is puzzling.
Table 1.
Effect of Age on risk of cardiovascular disease events: with and without adjustment for other cardiovascular risk factors
| No. of CVD events/ No. at risk |
Age coefficient unadjusted |
Age coefficient adjusted for other factors |
% of age effect not due to covariates |
|
|---|---|---|---|---|
| Men | 718/4969 | 0.067 | 0.059 | 11.9% |
| Women | 456/4522 | 0.072 | 0.043 | 40.3% |
CVD= cardiovascular disease.
Covariate risk factors: systolic blood pressure, total cholesterol, HDL-C, BMI, diabetes, and smoking. Data are based on follow-up of 8491 original cohort (examination 11) and Offspring cohort (examinations 1 and 3) participants for a 12-year period.9 The age coefficient indicates the regression coefficient (per 1 year increment) from Cox proportion hazards regression models. The ratio of the regression coefficients for age with and without adjustment for other risk factors indicates what proportion of the effect of age may be attributable to other risk factors.
Conclusions
Life expectancy is markedly influenced by atherosclerotic CVD and modifiable risk factors that predispose to it. Population research indicates that chances of surviving to age 85 years are heavily dependent on the burden of established risk factors carried from middle age on. Since the benefit of modifying these risk factors is well established in clinical trials, control or avoidance of the recognized major risk factors appears to be necessary to enhance chances of survival to an advanced age and may substantially reduce part of the aging-associated risk of CVD. An overview of epidemiological data presented in this report challenges the prevalent notion that age is a non-modifiable risk factor. It may well be that age is to a large extent a reflection of the length of exposure to the burden of risk factors.
Acknowledgments
Disclosures: This work was supported through National Institute of Health/ National Heart, Lung & Blood Institute Contract N01-HC-25195.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sniderman AD, Furberg CD. Age as a modifiable risk factor for cardiovascular disease. Lancet. 2008;371:1547–1549. doi: 10.1016/S0140-6736(08)60313-X. [DOI] [PubMed] [Google Scholar]
- 2.Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The Lifetime Risk of Stroke. Estimates from the Framingham Study. Stroke. 2006;37:345–350. doi: 10.1161/01.STR.0000199613.38911.b2. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones D, Larson M, Beiser A. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PWF, Wolf PA, Levy D. Prediction of Lifetime Risk for Cardiovascular Disease by Risk Factor Burden at 50 Years of Age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 5.Terry DF, Pencina MJ, Vasan RS, Murabito JM, Wolf PA, Hayes MK, Levy D, D'Agostino RB, Benjamin EJ. Cardiovascular risk factors predictive for survival and morbidity-free survival in the oldest-old Framingham Heart Study participants. J Am Geriatr Soc. 2005;53:1944–1950. doi: 10.1111/j.1532-5415.2005.00465.x. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Larson M, Levy D. Factors associated with survival to 75 years of age in middle-aged men and women. The Framingham Study. Arch Intern Med. 1996;156:505–509. [PubMed] [Google Scholar]
- 7.Willcox BJ, He Q, Chen R, Yano K, Masaki KH, Grove JS, Donlon TA, Willcox C, Curb JD. Midlife Risk Factors and Healthy Survival in Men. JAMA. 2006;296:2343–2350. doi: 10.1001/jama.296.19.2343. [DOI] [PubMed] [Google Scholar]
- 8.Yashin AI, Akushevich IV, Arbeev KG, Akushevich L, Ukraintseva SV, Kulminsk A. Insights on aging and exceptional longevity from longitudinal data: novel findings from the Framingham Heart Study. Age. 2006;28:363–367. doi: 10.1007/s11357-006-9023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D'Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]