Abstract
OBJECTIVES
To assess associations among maternal childhood experiences and subsequent parenting attitudes and use of infant spanking (IS), and determine if attitudes mediate the association between physical abuse exposure and IS.
METHODS
We performed a prospective study of women who received prenatal care at community health centers in Philadelphia, Pennsylvania. Sociodemographic characteristics, adverse childhood experiences (ACEs), attitudes toward corporal punishment (CP), and IS use were assessed via face-to-face interviews, conducted at the first prenatal care visit, 3 months postpartum, and 11 months postpartum. Bivariate and multiple logistic regression analyses were conducted.
RESULTS
The sample consisted of 1265 mostly black, low-income women. Nineteen percent of the participants valued CP as a means of discipline, and 14% reported IS use. Mothers exposed to childhood physical abuse and verbal hostility were more likely to report IS use than those not exposed (16% vs 10%, P = .002; 17% vs 12%, P = .02, respectively). In the adjusted analyses, maternal exposure to physical abuse, other ACEs, and valuing CP were independently associated with IS use. Attitudes that value CP did not mediate these associations.
CONCLUSIONS
Mothers who had childhood experiences of violence were more likely to use IS than mothers without such experiences. Intergenerational transmission of CP was evident. Mothers who had experienced physical abuse as a child, when compared to those who had not, were 1.5 times more likely to use IS. Child discipline attitudes and maternal childhood experiences should be discussed early in parenting in order to prevent IS use, particularly among at-risk mothers.
Keywords: physical punishment, adverse childhood experiences, positive influences in childhood, Adult-Adolescent Parenting Inventory
Corporal punishment (CP) in infancy is common in the United States, with prevalence rates between 14% and 35%.1–3 According to Straus,4 CP is the “use of physical force with the intention of causing a child to experience pain, but not injury, for the purpose of correction or control of the child's behavior.” As of 2008, many countries, including Sweden, Spain, Croatia, and Romania, have laws prohibiting CP use in children.5 Continuing debate among experts as to whether any form of CP is acceptable precludes the institution of such laws in the United States. Therefore, it is difficult to restrict CP use unless resulting physical evidence is brought to medical attention. Experts agree, however, that any form of physical punishment, including spanking, during infancy is inappropriate, ineffective in modifying behavior, and potentially harmful.6
Use of CP, including infant spanking (IS), crosses socioeconomic boundaries, although research shows higher prevalence rates among disadvantaged populations. Maternal young age, single marital status, black race/ethnicity, low education and socioeconomic status, large family size, living in the South, parental frustration, maternal depression, and a history of physical or sexual abuse, or family violence, are independent risk factors for CP use.1,2,7–10
Evidence showing that maternal experience of physical and sexual abuse and domestic violence are risks for subsequent CP use raises questions about whether other adverse childhood experiences predispose women to use CP on their offspring. The Adverse Childhood Experiences (ACE) study of the Centers for Disease Control and Prevention showed that ACEs individually and in a dose-response manner were associated with adverse health outcomes including depressive disorders, obesity, and ischemic heart disease.11–13 The ACE study, however, did not assess the relationship between ACEs and later IS use.
Negative consequences of CP in children include an increased risk for behavioral problems, delinquent behaviors, low self-esteem, depression, substance abuse, and physical abuse of their own children.14–18 Others found that parents experiencing CP as children were more likely to have attitudes that value CP,19 and such attitudes were associated with later CP use.3,20 Whether attitudes mediate the relationship between CP exposure and subsequent CP use is unclear.
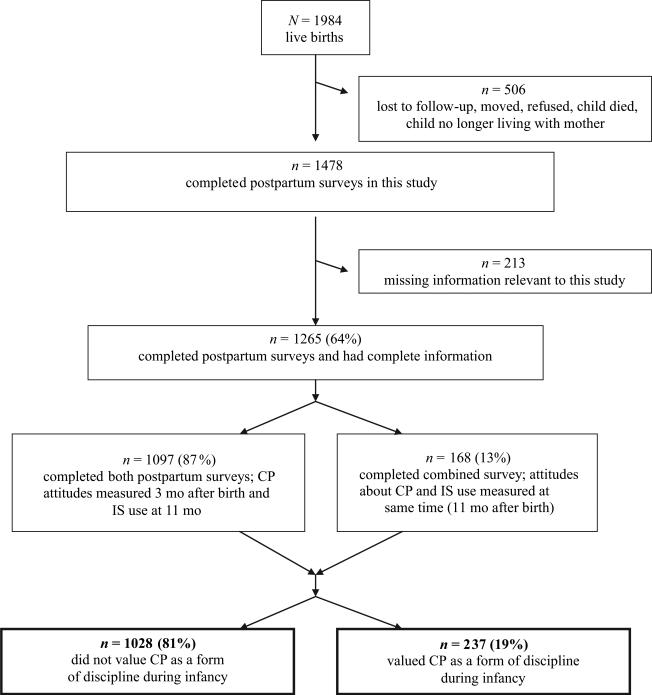
This study's objectives are to assess associations among maternal childhood experiences and subsequent parenting attitudes and IS, and to determine if parenting attitudes mediate the association between ACEs and IS. Our theoretical framework is depicted in Fig 1. The overarching hypothesis is that childhood physical abuse and other ACEs are associated with IS. A secondary hypothesis is that attitudes that value CP mediate the association between maternal physical abuse exposure and IS.
FIGURE 1.
Theoretical framework shows 2 possible pathways of how childhood experiences may influence later IS use. In the first pathway, depicted by the solid arrows, attitudes mediate the effect of childhood experiences on later use of IS. In the second pathway, depicted by the dashed arrow, childhood experiences influence later use of IS independent of attitudes.
METHODS
Sample Population
This research is part of a prospective study of pregnant women recruited from Philadelphia community health centers, consisting of Federally Qualified Health Centers and Federally Qualified Health Center look-alikes, from February 2000 to November 2002, as described previously.21–23 Inclusion criteria included having a singleton, intrauterine pregnancy, ability to speak English or Spanish, and living in Philadelphia. Face-to-face surveys were conducted at the first prenatal care visit, and at 3 ± 1 and 11 ± 1 months (mean ± SD) postpartum in participants’ homes. Institutional review boards at Thomas Jefferson University, Drexel University, and the University of Pennsylvania approved this research.
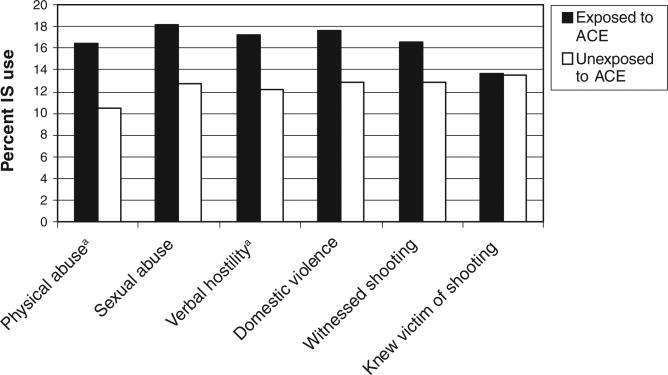
Of 2374 eligible women, 1984 women had a live birth and completed the prenatal interview. Postpartum surveys were completed by 1478 (74%) women. Of the remaining 506 women, 236 were lost to follow-up, 111 moved, 116 refused to participate, 34 were unable to participate, lacked data on key variables, or no longer lived with their child, and 9 had children who died. Because of missing information, 213 were dropped for a final sample of 1265 women. For 168 women, postpartum surveys were conducted as a combined survey at 11 ± 1 months (Fig 2). When compared with the final 1265 women, the 506 not completing the postpartum surveys did not differ with respect to age, income, marital status, parity, or education; however, they were more likely to be uninsured (71% vs 59%; P < .001) and Latina or white (20% vs 17% and 14% vs 10%, respectively; P = .002).
FIGURE 2.
Flow diagram of study participants.
Interviews were conducted by trained female interviewers by using standardized English and Spanish questionnaires. In the prenatal survey, maternal sociodemographic characteristics were obtained. In the second survey (3 ± 1 months postpartum), parenting attitudes toward CP were assessed by the 11-item CP subscale of the widely used Adult-Adolescent Parenting Inventory.24 This subscale is reliable, internally consistent, and valid.25 In the third survey (11 ± 1 months postpartum), women were asked about their experiences before age 16, which were categorized into ACEs associated with violence and positive influences in childhood (PICs). Participants were also asked about IS use with their own infants.
Study Variables
Maternal sociodemographic characteristics included maternal age, mean annual personal income, race/ethnicity, marital status, parity, and education. In the Adult-Adolescent Parenting Inventory CP subscale, parents responded to statements, using a 5-point Likert scale with “strongly agree” rated as 1, “neutral” as 3, and “strongly disagree” as 5. The following statements are among those in the subscale: “Spanking children when they misbehave teaches them how to behave” and “Children who bite others need to be bitten to teach them what it feels like.” Summary scores, based on a predeveloped tool, ranged from 11 to 55,26 and scores ≤33 were considered indicative of valuing CP.
Maternal experiences overlapping with the ACE study included assessments of physical and sexual abuse, verbal hostility, and household violence. Our study differed in that the 6 ACEs were assessed before age 16, whereas in the ACE study, 10 ACEs were assessed before age 18.
Maternal ACE variables included: (1) physical abuse, strictly defined by “rarely, sometimes, or often” as opposed to “never” in response to: “How often did you experience slapping you in the face, punching, pushing, kicking, or beating you with fists, hitting you with an object such as a belt or spoon, or burning you with an object such as a cigarette or iron by the person or people who raised you when you did something wrong?” This definition excluded “spanking.” (2) Sexual abuse, based on an affirmative answer to: “Were you ever sexually abused?” (3) verbal hostility, defined by “often” to: “How often did you experience yelling by the person or people who raised you when you did something wrong?” (4) domestic violence, based on an affirmative answer to: “Was anyone in your house being hit or beaten up?” (5) witnessing a shooting, based on an affirmative response to: “Did you ever see someone get shot?” and (6) knowing a victim of a shooting, based on an affirmative answer to: “Did you ever know someone who got shot?”
PICs included (1) positive maternal relationship, based on responses of “excellent, very good, or good” as opposed to “fair, poor, or nonexistent” to: “Growing up, would you say your relationship with your biological mother was . . .” (2) positive paternal relationship, identical to positive maternal relationship with “father” used instead of “mother.” (3) often given a hug, based on a response of “often” as opposed to “sometimes, rarely, or never” to: “How often did someone give you a hug when you did something well or when you were very good?” and (4) often told you were great, similar to “hug,” in response to: “How often were you told how great you were when you did something well or when you were very good?”
IS, the main outcome, was based on the mother's parenting practices and not her own childhood experiences. We defined mother's IS use as any response of >0 to the question “How many times, if any, have you had to spank your child in the past week?” This is similar to the question used in previous studies assessing “spanking” of children.7,17 Many would argue that spanking is a commonly used form of discipline; nevertheless, the American Academy of Pediatrics defines spanking as a form of CP.6
Statistical Analysis
χ2 tests were used for comparisons of categorical variables. For maternal age, we used the Student's t test. First, bivariate analyses were performed to determine the association between each ACE and PIC and parenting attitudes toward CP and IS use. Second, bivariate analyses were performed to determine the association between total ACEs and IS. A plateau effect was seen beyond 2 ACEs; therefore, total ACEs were categorized as 0 and 1 vs ≥2.
Logistic regression was employed to analyze IS, adjusting for potential confounding variables. Risk factors and confounders for inclusion in our final model were identified a priori on the basis of the above literature review and theoretical considerations. Sociodemographic characteristics were maternal age, annual personal income, race/ethnicity, marital status, parity, and education. Model A examined adjusted odds ratios including sociodemographic variables only. In model B, exposure to childhood physical abuse was added to model A. In model C, total ACEs other than physical abuse and PICs were added to model B. In model D, attitudes toward CP were included primarily to test whether attitudes mediated the association between physical abuse and IS. The Hosmer-Lemeshow goodness-of-fit χ2 statistic was calculated for the final model to assess model fit.27 The α value was set at .05 (2-sided), and Stata 10.1 (Stata Corp, College Station, TX) was used for all analyses.22 The Sobel-Goodman tests with bootstrapped standard errors were performed to assess whether attitudes toward CP mediated the association between maternal childhood physical abuse and IS.28–30
RESULTS
The sample consisted of 1265 mostly young (mean ± SD: 24 ± 6 years of age; range: 14–44 years), black, single, low-income women with poor education. Mothers who value CP were similar to those who did not by most sociodemographic characteristics. The only exception was that black mothers were more likely to value CP than other mothers (Table 1).
TABLE 1.
Sociodemographic Characteristics for the Overall Study Population and According to Whether the Mother Valued CP
| Overall Population (N = 1265) | Valued CP (N = 237) | Did Not Value CP (N = 1028) | P-value | |
|---|---|---|---|---|
| Maternal age, mean ± SD, y | 24 ± 6 | 24 ± 6 | 24 ± 6 | NS |
| Annual personal income, % | ||||
| <$6450 | 50 | 47 | 51 | NS |
| $6451–$11 758 | 26 | 30 | 25 | |
| >$11 758 | 24 | 23 | 24 | |
| Race/ethnicity, % | ||||
| Black | 70 | 82 | 68 | P < .001 |
| Latina | 17 | 7 | 19 | |
| White | 10 | 9 | 10 | |
| Other | 3 | 2 | 3 | |
| Marital status: single, % | 78 | 78 | 78 | NS |
| Primiparous, % | 49 | 46 | 50 | NS |
| Education, % | ||||
| Less than high school | 40 | 37 | 40 | NS |
| High school/GED | 42 | 46 | 42 | |
| College or more | 18 | 17 | 18 |
GED indicates general educational development certificate.
Table 2 shows the overall prevalence of maternal childhood experiences, attitudes that value CP, and IS use. Nineteen percent of participants valued CP (subscale score ≤ 33) and 14% reported IS use. A noteworthy finding was that over half (52%) of participants reported a history of childhood physical abuse. Nearly half (45%) of the women knew a victim of shooting before they were 16 years of age. The large majority (76%) reported a positive maternal relationship, but only half (52%) reported a positive paternal relationship. About three quarters of women (76%) reported at least 1 ACE and about half (51%) reported at least 2. Nearly all women (91%) had at least 1 PIC and three fourths (75%) had ≥2.
TABLE 2.
Prevalence of ACEs and PICs, Attitudes That Value CP and IS Use for the Study Population (N = 1265)
| Variables | % (n) |
|---|---|
| Adverse Childhood Experiences | |
| Physical abuse | 51.5 (652) |
| Sexual abuse | 12.6 (159) |
| Verbal hostility | 26.2 (331) |
| Domestic violence | 13.4 (170) |
| Witnessed shooting | 18.1 (229) |
| Knew victim of shooting | 44.7 (565) |
| Positive Influences in Childhood | |
| Positive maternal relationship | 76.4 (966) |
| Positive paternal relationship | 51.9 (656) |
| Often given hug | 57.8 (731) |
| Often told great | 50.3 (636) |
| Attitudes value CP | 18.7 (237) |
| IS use | 13.5 (171) |
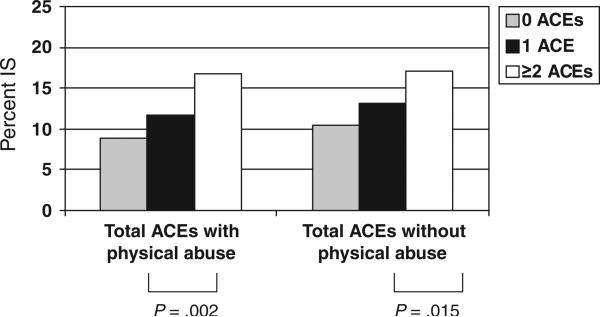
Figure 3 shows percentage of IS use by maternal exposure to each ACE. Mothers exposed to childhood physical abuse when compared with those not exposed were more likely to report IS use (16% vs 11%; P = .002). Similarly, those exposed to verbal hostility were more likely to use IS (17% vs 12%; P = .02). Knowing a victim of shooting was not associated with IS use. For the remaining ACEs, exposure was associated with IS use but these associations were not statistically significant, although the association between sexual abuse and IS use approached significance (P = .06). Parallel analyses were conducted for PICs, but no significant associations were found. We similarly explored associations between ACEs and PICs and attitudes toward CP use. Mothers exposed to physical or sexual abuse or verbal hostility were more likely to value CP (21% vs 16%, P = .016; 25% vs 18%, P = .046; 22% vs 17%, P = .050, respectively). Exposure to remaining ACEs and PICs was not associated with CP attitudes (data not shown).
FIGURE 3.
Percentage of IS use according to maternal exposure to ACEs (N = 1265). a P ≤ .05.
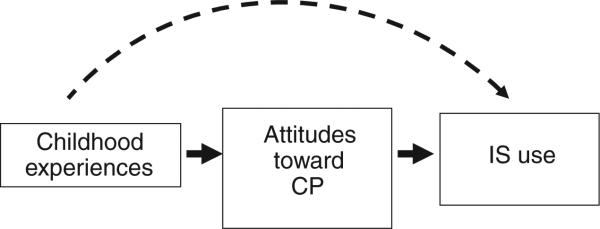
The relationships between total ACEs and IS use are shown in Fig 4. In a dose-response fashion, increasing numbers of ACEs were associated with higher rates of IS (graph on left). Removing physical abuse from total ACEs did not change our conclusions (graph on right). We also assessed the relationship between PICs and IS and found no association (not shown). Similar analyses were conducted to assess the relationship between total ACEs and PICs and CP attitudes. In a dose-response fashion, increasing numbers of ACEs were significantly associated with attitudes that value CP (not shown).
FIGURE 4.
Percentage of IS use according to total number of ACEs with and without physical abuse (N = 1265).
Table 3 presents the multivariate logistic regression models. In model A, marriage was protective and associated with a lower likelihood of IS. In model B, in addition to marital status, maternal history of physical abuse was a significant risk factor for IS (odds ratio [OR]: 1.70 [95% confidence interval (CI): 1.21–2.38]). Independent of physical abuse, a history of ≥2 ACEs predicted a greater likelihood of IS in model C (OR: 1.56 [95% CI: 1.01–2.41]). Finally, shown in model D, attitudes toward CP exhibited a significant association with IS such that those who valued CP were more likely to use IS (OR: 1.95 [95% CI: 1.32–2.87]). The addition of parenting attitudes to model C did not result in significant changes in the ORs corresponding to physical abuse or ACEs. The Hosmer-Lemeshow χ2 statistic was 6.13 (P = .63), showing a good fit of the adjusted model to the data.
TABLE 3.
Adjusted Odds Ratios From Models Predicting IS Use for the Study Population (N = 1265)
| Variable | Model A, aOR (95% CI)a | Model B, aOR (95% CI)b | Model C, aOR (95%CI)c | Model D, aOR (95% CI)d |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age | 0.98 (0.95–1.02) | 0.98 (0.95–1.02) | 0.99 (0.95–1.02) | 0.99 (0.95–1.03) |
| Race/ethnicity | ||||
| Black | 1.16 (0.65–2.08) | 1.14 (0.63–2.01) | 1.13 (0.63–2.04) | 1.08 (0.60–1.97) |
| Latina | 1.29 (0.65–2.56) | 1.30 (0.65–2.59) | 1.37 (0.69–2.74) | 1.49 (0.74–3.00) |
| Other | 1.48 (0.52–4.26) | 1.47 (0.51–4.26) | 1.55 (0.53–4.51) | 1.60 (0.55–4.67) |
| Marital status: married | 0.60 (0.36–0.97)e | 0.59 (0.36–0.97)e | 0.60 (0.36–0.98)e | 0.57 (0.35–0.94)e |
| Education | ||||
| High school/GED | 0.86 (0.52–1.40) | 0.85 (0.52–1.40) | 0.85 (0.52–1.41) | 0.83 (0.50–1.38) |
| Less than high school | 1.20 (0.72–1.99) | 1.17 (0.71–1.95) | 1.12 (0.67–1.89) | 1.12 (0.67–1.89) |
| Annual personal income | ||||
| $6450–$11 758 | 0.75 (0.47–1.15) | 0.73 (0.47–1.12) | 0.72 (0.47–1.11) | 0.69 (0.44–1.07) |
| >$11 758 | 0.97 (0.61–1.53) | 0.97 (0.62–1.54) | 0.93 (0.59–1.48) | 0.93 (0.59–1.48) |
| Parity: multiparous | 0.83 (0.56–1.23) | 0.81 (0.54–1.21) | 0.79 (0.53–1.18) | 0.77 (0.51–1.15) |
| Maternal history of physical abuse in childhood | — | 1.70 (1.21–2.38)e | 1.53 (1.07–2.20)e | 1.49 (1.04–2.14)e |
| ACEs | ||||
| 1 | — | — | 1.13 (0.72–1.78) | 1.14 (0.73–1.81) |
| ≥2 | — | — | 1.56 (1.01–2.41)e | 1.55 (1.01–2.39)e |
| PICs | ||||
| 1 | — | — | 1.16 (0.60–2.25) | 1.12 (.058–2.19) |
| 2 | — | — | 1.43 (0.77–2.64) | 1.37 (0.74–2.55) |
| 3 | — | — | 1.08 (0.57–2.03) | 1.03 (0.55–1.96) |
| 4 | — | — | 1.05 (0.54–2.04) | 1.01 (0.52–1.96) |
| Attitudes that value CP | — | — | — | 1.95 (1.32–2.87)e |
For each variable, the category not shown is the reference group (see Table 1 for all groups). aOR indicates adjusted odds ratio.
Model A: controlling for maternal age, race/ethnicity, education, annual personal income, and parity.
Model B: model A plus the childhood experience of physical abuse.
Model C: model B plus total ACEs other than physical abuse, and PICs.
Model D: model C plus attitudes that value CP.
Significant results.
DISCUSSION
Among a cohort of largely low-income, black mothers, 14% reported spanking their 11-month-old infants. Maternal physical abuse and other violent childhood experiences affected parenting attitudes and IS use. After adjusting for confounding variables, exposure to ≥2 ACEs was associated with a higher likelihood of IS. This study adds to the existing literature, which has not previously assessed the relationship between ACEs and parenting practices. Attitudes were associated with IS but did not mediate the association between ACEs and IS.
It was striking that the majority of respondents (76%) reported at least 1 ACE. The prevalence of physical abuse (52%) was higher than previous estimates of severe forms of physical abuse, measured nationally and in the ACE study.31,32 The prevalence of sexual abuse was lower than previous estimates of 20% to 40%.31,33 The prevalence of domestic violence was nearly identical to that found in the ACE study (13.4% vs 13.9%).31
Our results show a dose-response effect between ACEs and IS, adding to the adverse outcomes associated with cumulative ACEs.11,34 The finding that childhood physical abuse was associated with attitudes that value CP and with subsequent IS are consistent with previous reports. As hypothesized, exposure to ≥2 ACEs was associated with a higher (1.6 times) likelihood of IS. This suggests that, in addition to childhood physical abuse, cumulative violence exposure, including sexual abuse, verbal hostility, domestic violence, witnessing a shooting, or knowing a victim of shooting, predisposes mothers to IS use.
There are several limitations to our study. All mothers completing the prenatal survey did not complete postpartum surveys. The fact that these mothers were more likely to be uninsured suggests that they may have had more financial hardship. It is possible that they had more childhood adversity; therefore, our results may underestimate some exposure and outcome variables. Reports of childhood experiences were retrospective, with women being asked to report experiences before age 16 when they were, on average, 24 years of age. Reports are subject to recall bias, although empirical evidence suggests that this bias has been overestimated.35 Our study, building on the ACE study, may be subject to less recall bias because our sample was younger (average age of 24 vs 56 years).11 Survey questions may not capture the complexity, diversity, severity, or frequency of childhood experiences. The main outcome, IS, was based on spanking in the past week, which may have underestimated actual use. We did not assess motivations for spanking or predisposing characteristics related to the infant, such as temperament. Our assessment of sexual abuse was based on a question using the term “sexual abuse,” which may have underestimated exposure. A recent study showed that use of the word “abuse” in questions, when compared with the use of questions describing abusive experiences, resulted in lower reported abuse among community samples.36
Attitudes toward CP were associated with twice the likelihood of IS use toward 11-month-old infants in the adjusted analyses. This finding suggests that attitudes toward CP should be asked of mothers with infants. Parents may be unfamiliar with the harmful effects of IS. Health professionals should use the perinatal period as a “window of opportunity” to discuss parental experiences and attitudes. Recent evidence shows that maltreatment, including spanking, during infancy is associated with higher hormonal reactivity to stress, which in turn could impact future health outcomes.37 Additional research is needed to understand factors that link CP, ACEs, and adverse health outcomes. Early efforts to prevent CP are important because attitudes toward discipline are established early in parenting and disciplinary strategy is maintained throughout early childhood.3 Previous researchers note that negative parenting practices may occur at the expense of positive practices, showing that those who were more likely to spank also reported less reading, listening to music, playing, and hugging.9
The prevalence of IS (14%) in our study is similar to previous reports of CP in infancy.1–3 What is striking is that, even among those not exposed to physical abuse, 1 in 10 mothers reported spanking their infants, suggesting that discussions about child discipline should occur among all families, not just those with a history of violence. We found it hopeful that the majority (84%) of the participants who experienced childhood physical punishment did not report spanking their infants. This important point should be made by clinicians when counseling at-risk mothers exposed to ACEs about the harmful effects of CP. Although inter-generational transmission of CP has been described, the frequency with which this occurs is not well understood.38
CONCLUSIONS
Our findings call for greater efforts to prevent childhood adversity including physical and sexual abuse, verbal hostility, and domestic and gun violence. Although health care professionals must continue to assess personal risks, societal action is also recommended. In 2000, the American Academy of Pediatrics recommended that CP be abolished from schools,39 but 21 states have yet to implement laws banning this practice. National standards for out-of-home child care prohibit CP use by stating, “The following behaviors shall be prohibited in all child care settings and by all caregivers: CP, including beating, hitting, spanking, shaking, pinching, excessive exercise, exposure to extreme temperatures, and other measures producing physical pain.”40 In state-regulated child care centers, 48 states have laws prohibiting CP use.5 If policy makers recognize that CP should be abolished from child care centers and schools, it would seem logical that CP be prohibited altogether.
WHAT's KNOWN ON THIS SUBJECT: Corporal punishment (CP) in infancy is common in the United States, with prevalence rates between 14% and 35%. Maternal experiences of physical and sexual abuse, and domestic violence, are risks for subsequent CP use among their offspring.
WHAT THIS STUDY ADDS: This study assesses the relationship between adverse childhood experiences (ACEs) and infant spanking. Maternal physical abuse impacted attitudes and infant spanking (IS) use. Attitudes were associated with IS, but did not mediate the association between ACEs and IS.
ACKNOWLEDGMENTS
This research was funded in part by grant TS-286-14/14 from the Centers for Disease Control and Prevention (Dr Culhane), and grant 1-RO1-HD36462-01A1 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Drs Culhane and Elo).
We thank all of the women who participated in this study and all of the interviewers who collected the data.
ABBREVIATIONS
- ACE
adverse childhood experience
- CP
corporal punishment
- IS
infant spanking
- PIC
positive influence in childhood
- OR
odds ratio
- CI
confidence interval
Footnotes
This research was presented at the annual meeting of the Pediatric Academic Societies; May 4, 2008; Honolulu, HI.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Regalado M, Sareen H, Inkelas M, Wissow LS, Halfon N. Parents’ discipline of young children: results from the National Survey of Early Childhood Health. Pediatrics. 2004;113(suppl 6):1952–1958. [PubMed] [Google Scholar]
- 2.Straus MA, Stewart JH. Corporal punishment by American parents: national data on prevalence, chronicity, severity, and duration, in relation to child and family characteristics. Clin Child Fam Psychol Rev. 1999;2(2):55–70. doi: 10.1023/a:1021891529770. [DOI] [PubMed] [Google Scholar]
- 3.Vittrup B, Holden GW, Buck J. Attitudes predict the use of physical punishment: a prospective study of the emergence of disciplinary practices. Pediatrics. 2006;117(6):2055–2064. doi: 10.1542/peds.2005-2204. [DOI] [PubMed] [Google Scholar]
- 4.Straus MA. Beating the Devil Out of Them: Physical Punishment in American Families. 2nd ed. Transaction Publishers; New Brunswick, NJ: 2001. [Google Scholar]
- 5.The Center for Effective Discipline [June 13, 2009];Discipline and the law. Available at: www.stophitting.com/index.php?page=laws-main.
- 6.Stein MT, Perrin EL, American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health Guidance for effective discipline. Pediatrics. 1998;101(4 pt 1):723–728. [PubMed] [Google Scholar]
- 7.Combs-Orme T, Cain DS. Predictors of mothers’ use of spanking with their infants. Child Abuse Negl. 2008;32(6):649–657. doi: 10.1016/j.chiabu.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Dietz TL. Disciplining children: characteristics associated with the use of corporal punishment. Child Abuse Negl. 2000;24(12):1529–1542. doi: 10.1016/s0145-2134(00)00213-1. [DOI] [PubMed] [Google Scholar]
- 9.Wissow LS. Ethnicity, income, and parenting contexts of physical punishment in a national sample of families with young children. Child Maltreat. 2001;6(2):118–129. doi: 10.1177/1077559501006002004. [DOI] [PubMed] [Google Scholar]
- 10.Alyahri A, Goodman R. Harsh corporal punishment of Yemeni children: occurrence, type and associations. Child Abuse Negl. 2008;32(8):766–773. doi: 10.1016/j.chiabu.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 12.Anda RF, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- 13.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Straus MA, Sugarman DB, Giles-Sims J. Spanking by parents and subsequent antisocial behavior of children. Arch Pediatr Adolesc Med. 1997;151(8):761–767. doi: 10.1001/archpedi.1997.02170450011002. [DOI] [PubMed] [Google Scholar]
- 15.Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: a meta-analytic and theoretical review. Psychol Bull. 2002;128(4):539–579. doi: 10.1037/0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- 16.Straus MA, Kantor GK. Corporal punishment of adolescents by parents: a risk factor in the epidemiology of depression, suicide, alcohol abuse, child abuse, and wife beating. Adolescence. 1994;29(115):543–561. [PubMed] [Google Scholar]
- 17.Slade EP, Wissow LS. Spanking in early childhood and later behavior problems: a prospective study of infants and young toddlers. Pediatrics. 2004;113(5):1321–1330. doi: 10.1542/peds.113.5.1321. [DOI] [PubMed] [Google Scholar]
- 18.Weiss B, Dodge KA, Bates JE, Pettit GS. Some consequences of early harsh discipline: child aggression and a maladaptive social information processing style. Child Dev. 1992;63(6):1321–1335. doi: 10.1111/j.1467-8624.1992.tb01697.x. [DOI] [PubMed] [Google Scholar]
- 19.Deater-Deckard K, Lansford JE, Dodge KA, Pettit GS, Bates JE. The development of attitudes about physical punishment: an 8-year longitudinal study. J Fam Psychol. 2003;17(3):351–360. doi: 10.1037/0893-3200.17.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, Zelli A. Discipline responses: influences of parents’ socioeconomic status, ethnicity, beliefs about parenting, stress, and cognitive-emotional processes. J Fam Psychol. 2000;14(3):380–400. doi: 10.1037//0893-3200.14.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung EK, McCollum KF, Elo IT, Culhane JF. Does prenatal care at community-based health centers result in infant primary care at these sites? Ambul Pediatr. 2006;6(1):25–31. doi: 10.1016/j.ambp.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6) doi: 10.1542/peds.113.6.e523. Available at: www.pediatrics.org/cgi/content/full/113/6/e523. [DOI] [PubMed] [Google Scholar]
- 23.Culhane JF, Rauh V, McCollum KF, Hogan VK, Agnew K, Wadhwa PD. Maternal stress is associated with bacterial vaginosis in human pregnancy. Matern Child Health J. 2001;5(2):127–134. doi: 10.1023/a:1011305300690. [DOI] [PubMed] [Google Scholar]
- 24.Bavolek S, Keene RG. Adult-Adolescent Parenting Inventory (AAPI-2) Administration and Development Handbook. Family Development Resources, Inc; Asheville, NC: 1999. [Google Scholar]
- 25.Conners NA, Whiteside-Mansell L, Deere D, Ledet T, Edwards MC. Measuring the potential for child maltreatment: the reliability and validity of the Adult Adolescent Parenting Inventory-2. Child Abuse Negl. 2006;30(1):39–53. doi: 10.1016/j.chiabu.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Adult-Adolescent Parenting Inventory. [June 27, 2008];AAPI online. Available at: www.aapionline.com.
- 27.Lemeshow S, Hosmer DW., Jr A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982;115(1):92–106. doi: 10.1093/oxfordjournals.aje.a113284. [DOI] [PubMed] [Google Scholar]
- 28.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 29.MacKinnon D, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behav Res. 1995;30(1):41–62. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17(2):144–158. [Google Scholar]
- 31.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 32.Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl. 2003;27(10):1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 33.Roosa MW, Reinholtz C, Angelini PJ. The relation of child sexual abuse and depression in young women: comparisons across four ethnic groups. J Abnorm Child Psychol. 1999;27(1):65–76. [PubMed] [Google Scholar]
- 34.Schilling EA, Aseltine RH, Jr, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. 2007;7:30. doi: 10.1186/1471-2458-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Surtees PG, Wainwright NW. The shackles of misfortune: social adversity assessment and representation in a chronic-disease epidemiological setting. Soc Sci Med. 2007;64(1):95–111. doi: 10.1016/j.socscimed.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 36.Thombs BD, Bernstein DP, Ziegelstein RC, et al. An evaluation of screening questions for childhood abuse in 2 community samples: implications for clinical practice. Arch Intern Med. 2006;166(18):2020–2026. doi: 10.1001/archinte.166.18.2020. [DOI] [PubMed] [Google Scholar]
- 37.Bugental DB, Martorell GA, Barraza V. The hormonal costs of subtle forms of infant maltreatment. Horm Behav. 2003;43(1):237–244. doi: 10.1016/s0018-506x(02)00008-9. [DOI] [PubMed] [Google Scholar]
- 38.Ertem IO, Leventhal JM, Dobbs S. Intergenerational continuity of child physical abuse: how good is the evidence? Lancet. 2000;356(9232):814–819. doi: 10.1016/S0140-6736(00)02656-8. [DOI] [PubMed] [Google Scholar]
- 39.American Academy of Pediatrics. Committee on School Health Corporal punishment in schools. Pediatrics. 2000;106(2 pt 1):343. [PubMed] [Google Scholar]
- 40.American Academy of Pediatrics. American Public Health Association. National Resource Center for Health and Safety in Child Care and Early Education . Caring for Our Children: National Health and Safety Performance Standards: Guidelines for Out-of-Home Child Care Programs. 2nd ed. American Academy of Pediatrics and Washington, DC: American Public Health Association; Elk Grove Village, IL: 2002. p. 87. [Google Scholar]