Abstract
This study investigated whether loneliness and cognitive processing explain the influence of negative (social constraints) and positive (emotional support) relationship qualities on cancer survivors’ distress. Participants were 195 cancer survivors who had undergone hematopoietic stem cell transplantation. Path analysis supported the hypothesis that loneliness and cognitive processing would mediate the association between social constraints and distress. Only loneliness mediated the association between emotional support and distress—an indirect effect significant only when support came from family and friends rather than a partner. Findings suggest that addressing social constraints may enhance cancer survivors’ adjustment.
Keywords: hematopoietic stem cell transplantation, cancer survivorship, loneliness, psychological distress, social support, social constraints
Hematopoietic stem cell transplantation (HSCT) is a psychologically and medically taxing treatment for hematological cancers and other diseases (Copelan, 2006). In addition to facing demands of a life-threatening diagnosis and treatment, survivors cope with serious treatment side-effects, enduring medical risks (Copelan, 2006; Syrjala, Kurland, Abrams, Sanders, & Heiman, 2008), and practical stressors such as financial strain and difficulty resuming work and social roles (Andrykowski et al., 1999; Lee et al., 2001; Mosher et al., 2011). Together, these demands help explain the persistent elevated distress reported by up to 40% of transplant survivors (Hjermstad et al., 1999; Mosher, Redd, Rini, Burkhalter, & DuHamel, 2009). Identifying psychological and social factors related to long-term distress in cancer survivors, as well as the mechanisms linking these variables, will inform theory and clinical practice.
Research suggests the importance of cancer survivors’ social relationships in psychological adjustment to the disease (Pinquart, Frohlich, & Silbereisen, 2007), but provides little information regarding how these relationships have their beneficial effect. For instance, HSCT survivors with greater pre-transplant social support are less likely to experience post-transplant distress than others (Jenks Kettmann & Altmaier, 2008; Syrjala et al., 2004). Although relatively few studies have examined correlates of post-transplant support, several studies show that survivors who receive social support that meets their expectations after transplant have better psychological adjustment (Rini et al., 2011; Wingard et al., 2010). The goal of the present study was to investigate factors that may account for the influence of relationship qualities on distress among transplant survivors.
According to social-cognitive processing theory (Lepore, 2001; Lepore & Revenson, 2007), disclosure of stress-related thoughts and feelings to close others may partially explain the psychological benefits of a supportive social environment (Cordova, Walser, Neff, & Ruzek, 2005; Lepore & Helgeson, 1998; Manne, Ostroff, Winkel, Grana, & Fox, 2005). The effects of disclosure on psychological well-being may be partially mediated by emotional habituation and enhanced cognitive processing, the psychological process through which people make sense of their experience and integrate it into their self-concept and worldview (Lepore, 2001). Cognitive processing involves thinking about the stressor and discussing it with others, alternating with efforts to manage distress by avoiding reminders of it (Horowitz, 1986). Close others can promote successful cognitive processing in various ways, including suggesting new, more positive perspectives from which to understand it and encouraging acceptance (Lepore & Revenson, 2007). When successful, a meaningful narrative of the stressful experience is formed that reduces the need for further cognitive processing (i.e., stressor-related intrusions and avoidance) (Horowitz, 1986; Lepore, 2001).
However, some transplant survivors experience social constraints on disclosure that may increase intrusive thoughts and avoidance, contributing to post-transplant distress (Lepore, 2001; Lepore & Revenson, 2007). For instance, some survivors avoid or modify disclosures, either because their close others are unreceptive (e.g., they withdraw, criticize, or deny disclosures) or because they expect unreceptive responses (Lepore, 2001; Lepore & Revenson, 2007). Positive associations among social constraints, intrusions and avoidance, and distress have been replicated among cancer patients (Cordova, Cunningham, Carlson, & Andrykowski, 2001; Manne et al., 2005; Zakowski, Ramati, Morton, Johnson, & Flanigan, 2004).
Emotional support, which includes having close others who listen to and understand emotional disclosures (House & Kahn, 1985; Thoits, 1985), is related to reduced social constraints and may operate through the same pathways (i.e., reduced transplant-related intrusions and avoidance), assuming it is enacted effectively (Rini & Dunkel Schetter, 2010). In addition, emotional support involves demonstrations of caring and concern that are unrelated to disclosure and cognitive processing. For instance, close others enact emotionally supportive behaviors (e.g., being physically present throughout treatment and recovery) that help survivors feel less lonely (Cohen, Ley, & Tarzian, 2001). Lower loneliness (emotional isolation associated with perceived inadequacy of the quantity and quality of one's relationships; Hawkley & Cacioppo, 2010) has in turn been associated with less distress in cancer survivors (Boer, Elving, & Seydel, 1998) and healthy samples (Cacioppo, Hawkley, & Thisted, 2010; Wei, Russell, & Zakalik, 2005). These effects are notable because loneliness is a common problem among transplant survivors (Cohen et al., 2001; Rusiewicz et al., 2008).
The present study examined loneliness and cognitive processing (in the form of distressing, intrusive thoughts about the illness and attempts to avoid them) as key pathways linking transplant survivors’ social environment (their social constraints and emotional support) and distress. We investigated these psychosocial processes of adaptation among survivors beyond the initial months following transplantation, a time during which many face challenges related to the resumption of pre-transplant activities. We hypothesized that survivors with either lower emotional support or higher social constraints would report greater intrusive thoughts and avoidance (markers of incomplete cognitive processing) and, in turn, greater distress. We also hypothesized that lower emotional support would be associated with greater loneliness and, in turn, greater distress. Because social constraints may also contribute to greater loneliness (e.g., because people restrict their disclosures in response to social constraints, potentially increasing emotional isolation), we explored loneliness as a pathway linking social constraints and distress. Finally, we investigated effects of the source of support and constraints—a partner versus family and friends. Differential effects of social support from these sources have been observed in research on mothers of pediatric HSCT patients (Rini et al., 2008).
Method
Participants and Procedures
Data for this study come from a randomized controlled trial of a psychosocial intervention for HSCT survivors. Participants were recruited between May 2008 and June 2010 using two methods. First, potentially eligible participants were identified by clinical database staff at two medical centers in the northeastern United States and mailed introductory materials describing the study, followed by a recruitment call from a trained staff member. Second, the study was announced on cancer-related websites and in newsletters and mailings coordinated with cancer advocacy organizations. Interested individuals contacted the study team for more information. Potentially eligible transplant survivors completed a telephone screening interview to verify they met the following eligibility criteria: (1) 9-months to 3-years post-transplant during the intervention phase of the trial; (2) >18 years of age; (3) English fluency; and (4) at least some distress, quality of life, or survivorship difficulties according to scores on validated screening measures. Eighty-five percent of screened survivors qualified for the study. Thus, all had some distress, but its extent and nature varied broadly. Exclusion criteria included disease relapse, forthcoming additional transplant, severe cognitive impairment, active psychosis, suicidal ideation, or current substance dependence.1 After screening, eligible participants completed study measures as part of a baseline telephone interview for the intervention trial. Measures were completed before randomization. Procedures were approved by the institutional review boards of the study sites. Participants were compensated.
Measures
Distress was measured with the 53-item Brief Symptom Inventory (BSI) (Derogatis, 1993), which assesses symptoms of somatization, obsessive-compulsive behaviors, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. We used the Global Severity Index (GSI), a composite score of these symptoms. Participants rated how much discomfort each symptom had caused in the past month on a scale from 0 (not at all) to 4 (extremely). The BSI-GSI has adequate reliability and validity in cancer populations (Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001).
Intrusive thoughts and avoidance related to a specific stressor (in this study, participants’ illness and transplant) were measured with the 15-item Impact of Event Scale (IES) (Horowitz, Wilner, & Alvarez, 1979). Responses are provided on a 4-point scale (not at all=0, rarely=1, sometimes=3, and often=5) and summed. Higher scores indicate greater intrusions and avoidance. The measure has shown good reliability and validity in research on cancer populations (Salsman, Segerstrom, Brechting, Carlson, & Andrykowski, 2009) and has been used as a marker of incomplete cognitive processing (Lepore, 2001).
Loneliness was measured with the reliable and valid UCLA Loneliness Scale–Version 3 (Russell, 1996). Respondents rated each of 20 items (e.g., “How often do you feel alone?”) on a scale from 1 (never) to 4 (always).
Social constraints were measured with the 15-item Social Constraints Scale (SCS) (Lepore & Ituarte, 1999; Lepore & Revenson, 2007), which assesses perceived barriers to disclosing thoughts and feelings related to a stressor (in this study, the illness and transplant) experienced in the past month. Responses are provided on a scale from 1 (never) to 4 (often). Constraints from the partner and constraints from other family and friends were assessed separately. The scale has been validated with cancer populations (Lepore & Ituarte, 1999).
Emotional support was measured with the 3-item emotional support subscale of the positive and negative social exchanges scale (Newsom, Rook, Nishishiba, Sorkin, & Mahan, 2005), which assesses doing or saying considerate things, cheering the respondent up, and allowing discussion of concerns. The measure was administered twice to assess support from the partner and, separately, from other people. Respondents rated how often each behavior occurred in the prior month on a scale from 1 (never) to 5 (very often).
Medical factors were self-reported and included current disability status, time since HSCT, history of relapse and prior HSCT, type of transplant, and history of graft versus host disease (GvHD). Participants also completed checklists of major medical comorbidities and HSCT complications.
Analysis Plan
First, bivariate analyses were used to examine associations between medical and sociodemographic variables and distress; significant associations identified potential control variables. Next we tested study hypotheses with path analysis using EQS version 6.1. The Satorra-Bentler scaled chi-square statistic (Satorra & Bentler, 1988), the root-mean-square error of approximation (RMSEA), and the comparative fit index (CFI) were used to evaluate model fit. Good fit is indicated by a non-significant chi-square CFI ≥.95, and RMSEA ≤.06 (Hu & Bentler, 1999). Following conventional procedures (Bentler, 1992), a hypothesized model was specified, its parameters estimated (using Maximum Likelihood estimation), and its fit tested.
Modification indices (Chou & Bentler, 1990) were used to improve model fit. Finally, bootstrapping procedures (Preacher & Hayes, 2008) were used to test the significance of indirect effects (Shrout & Bolger, 2002).
Results
Sample Characteristics
Of the 432 transplant survivors recruited through the study sites or responding to advertisements, 353 (82%) completed screening, 54 were not eligible, 13 relapsed, 34 could not be contacted, and 18 declined (usually due to time constraints). Of the 234 survivors who were eligible for the study, 6 declined to continue, 12 relapsed, and 14 could not be contacted, resulting in 202 people (86%) who completed study measures, 195 (97%) of whom were eligible for the current analysis because they were married or had a main romantic partner. (Same sex couples were eligible, but none joined the study.) Screening rates were similar for participants recruited through the study sites and through advertisements, and participants recruited through these two channels did not differ on any study variables.
Sample characteristics are shown in Table 1. Most participants were non-Hispanic White, married, and had a college degree. There were equal numbers of men and women. The median household income was over $80,000. The most common diagnoses were myeloma, leukemia, or lymphoma.
Table 1.
Sample Characteristics (N = 195)
| Variable | n (%) | M (SD) | Range |
|---|---|---|---|
| Sex—Female | 97 (50%) | ||
| Marital status—Married | 187 (96%) | ||
| Race/ethnicity | |||
| Non-Hispanic White | 169 (87%) | ||
| Hispanic/Latino | 8 (4%) | ||
| African American/Black | 10 (5%) | ||
| Other | 8 (4%) | ||
| Age (years) | 54 (12) | 22 to 77 | |
| Annual household income (median) | > $80,000 | < $20,000 to > $110,000 | |
| Education | |||
| High school or less | 18 (9%) | ||
| Partial college | 40 (21%) | ||
| Four-year college degree | 70 (36%) | ||
| Graduate degree | 65 (33%) | ||
| Missing | 2 (1%) | ||
| Working full or part time | 75 (39%) | ||
| Unemployed due to disability | 47 (24%) | ||
| Retired | 46 (24%) | ||
| Other employment status | 27 (14%) | ||
| Diagnosis | |||
| Multiple myeloma | 60 (31%) | ||
| Lymphoma | 63 (32%) | ||
| Leukemia | 47 (24%) | ||
| Other | 25 (13%) | ||
| History of disease relapse since initial diagnosis | 75 (39%) | ||
| Type of transplant | |||
| Autologous | 116 (60%) | ||
| Allogeneic (matched) | 53 (27%) | ||
| Allogeneic (unmatched) | 18 (9%) | ||
| Missing | 8 (4%) | ||
| Months since transplant | 19 (8) | 7 to 37 | |
| History of prior transplant(s) | 41 (21%) | ||
| Graft versus host disease (GVHD) | |||
| Acute | 48 (25%) | ||
| Chronic | 42 (22%) | ||
| Number of serious transplant complications other than GVHD | |||
| None | 15 (8%) | ||
| One | 46 (24%) | ||
| Two | 48 (25%) | ||
| Three | 37 (19%) | ||
| Four or more | 49 (25%) | ||
| Number of major medical comorbidities | 1.14 (1.18) | ||
| None | 71 (36%) | ||
| One | 59 (30%) | ||
| Two | 42 (22%) | ||
| Three or more | 23 (12%) | ||
Intercorrelations among primary study variables, descriptive statistics, and reliabilities are shown in Table 2. Higher partner and family/friend social constraints were associated with greater loneliness (rs=.43), intrusive thoughts and avoidance (rs=.40, .37), and distress (rs=.52, .42). Lower partner and family/friend emotional support was associated with greater loneliness (rs=−.39, −.42) but not with intrusive thoughts and avoidance, and only lower partner emotional support was associated with distress (r=−.19). Moderate, negative associations were found between social constraints and emotional support from the same source (partner, r=−.34, or family/friends, r=−.23). Comparison using the Simple Interactive Statistical Analysis program (Uitenbroek, 1999) revealed that distress was more strongly correlated with partner social constraints (r=.52) than with partner emotional support (r=−.19), t(192)=6.87, p<.001. Similarly, distress was more strongly correlated with family/friend social constraints (r=.42) than with family/friend emotional support (r=−.10), t(192)=4.99, p<.001.
Table 2.
Descriptive Statistics and Correlations among Primary Study Variables (N = 195)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Mean | SD | Range | α |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Loneliness | — | 34.29 | 8.68 | 20.00–59.00 | .92 | ||||||
| 2. Cognitive processing | .34*** | — | 15.25 | 12.18 | 0–47.00 | .87 | |||||
| 3. Partner social constraints | .43*** | .40*** | — | 1.59 | .46 | 1.00–3.20 | .85 | ||||
| 4. Family/friend social constraints | .43*** | .37*** | .49*** | — | 1.70 | .52 | 1.00–3.33 | .90 | |||
| 5. Partner emotional support | −.39*** | −.04 | −.34*** | −.11 | — | 12.49 | 2.26 | 5.00–15.00 | .78 | ||
| 6. Family/friend emotional support | −.42*** | .03 | .00 | −.23** | .43*** | — | 10.60 | 2.29 | 3.00–15.00 | .78 | |
| 7. Distress | .61*** | .45*** | .52*** | .42*** | −.19** | −.10 | — | .56 | .41 | .01–1.87 | .95 |
p < .01.
p < .001.
Preliminary Analyses
Bivariate analyses of demographic and medical factors revealed five potential control variables: Greater distress was associated with lower income (r=−.17, p=.02), being on disability (t=−2.89, p=.004), history of GvHD (t=−3.35, p=.001), having more HSCT complications (r=.29, p<.001), and having more major medical comorbidities (r=.33, p<.001).
Model Testing
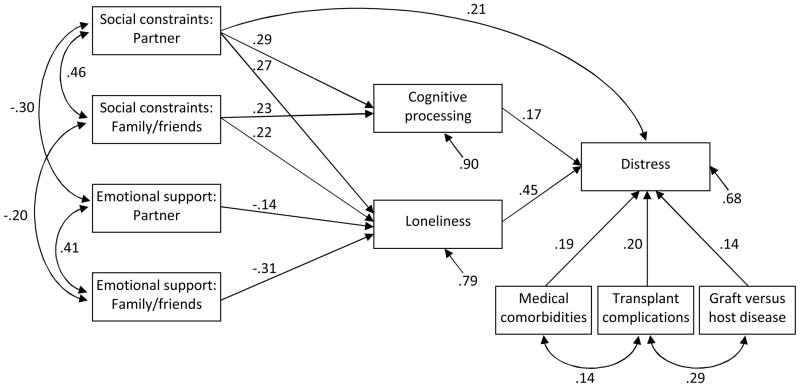
First we estimated the hypothesized model in which intrusive thoughts and avoidance and loneliness mediated effects of partner and family/friend social constraints and emotional support on distress. Control variables included history of GvHD, number of HSCT complications, and number of major medical comorbidities. (Income and disability were not significant independent predictors of distress and were dropped from the model). This model did not meet criteria for good fit (χ2=51.46, p=.002; CFI=.95; RMSEA=.07). Modification indices revealed non-significant paths from partner emotional support and family/friend emotional support to intrusive thoughts and avoidance and suggested a direct path from partner social constraints to distress (a theoretically plausible association). Making these changes resulted in a well-fitting final model (Figure 1) (χ2=40.29, p=.05; CFI=.97; RMSEA=.05) that supported most of the hypothesized pathways. For indirect pathways involving intrusive thoughts and avoidance, bootstrapped 95% confidence intervals (CIs) revealed significant indirect effects of partner social constraints (B=.04, 95% CI .01 to .08) and family/friend social constraints (B=.03, 95% CI .003 to .06) on distress. For pathways involving loneliness, bootstrapped 95% CIs revealed significant indirect effects of partner social constraints (B=.10, 95% CI .05 to .16), family/friend social constraints (B=.07, 95% CI .03 to .13), and family/friend emotional support (B=−.02, 95% CI −.04 to −.01) on distress. The indirect effect of partner emotional support on distress through loneliness was not significant (B=−.01, 95% CI −.02 to .002), despite significant paths linking partner emotional support and loneliness, and loneliness and distress. Additionally, there was a significant direct association between partner social constraints and distress.
Figure 1.
Final model. Parameter estimates are standardized. All paths are significant at p < .05.
Discussion
This study investigated relations between two features of HSCT survivors’ social environment—social constraints and emotional support—and their associations with survivors’ distress. Findings suggest that elevated loneliness and incomplete cognitive processing (i.e., intrusive thoughts about the illness and attempts to avoid them) may partially account for the relationship between social constraints and distress. In contrast, emotional support from others—especially family and friends—may influence distress by reducing loneliness, but not by reducing cognitive processing of the transplant experience.
Results replicate hypothesized links between social constraints and distress through cognitive processing (Lepore & Helgeson, 1998; Manne et al., 2005) and extend these findings by showing that these effects hold regardless of the source (partner or family/friends). According to social-cognitive processing theory, these effects likely stem from a social environment that encourages discussion and acceptance of cancer-related concerns, thereby reducing the need for further processing (Lepore, 2001; Lepore & Revenson, 2007). Results also extend our understanding of social constraints by highlighting loneliness as an additional pathway through which they may influence distress. For instance, survivors’ attempts to restrict or modify their illness-related disclosures in response to social constraints may increase their loneliness and distress. Alternatively, social constraints may amplify loneliness by undermining survivors’ sense of belongingness and security in relationships (Lepore & Revenson, 2007).
Loneliness and incomplete cognitive processing partially accounted for effects of partner constraints on distress, but fully accounted for effects of family/friend constraints on distress. Thus, partner constraints may influence distress through more diverse mechanisms. This finding is consistent with a study of prostate cancer patients, in which avoidance fully mediated the relation between family/friend constraints and distress but only partially mediated the relation between partner constraints and distress (Lepore & Helgeson, 1998). Constraints from a partner may be particularly distressing due to the centrality of this relationship (Fife, Monahan, Abonour, Wood, & Stump, 2009).
Unlike findings involving social constraints, effects of emotional support on distress were related to loneliness but not cognitive processing. Thus, results only supported one of the hypothesized pathways linking emotional support and distress. Moreover, effects involving emotional support were generally weaker than those involving social constraints. These findings indicate the relative importance of communicative aspects of the social environment after transplant compared to those involving affiliation, consistent with cognitive processing theories’ emphasis on making sense of traumatic experiences such as cancer (Lepore, 2001). Yet, they also suggest that emotional support may help protect survivors from loneliness—a provision of support that is consistent with theory and research (Newsom et al., 2005; Rook, 1987).
Furthermore, results from the path analysis suggest that emotional support from family and friends may be more important than partner emotional support for mitigating loneliness and reducing distress. Findings warrant replication, especially in light of bivariate correlations suggesting the opposite pattern of results. However, results are consistent with research identifying family and friend support as a key predictor of adjustment among mothers of pediatric HSCT patients (Rini et al., 2008) and suggest that partner support may be rendered less effective than it would normally be as partners cope with the stress of the loved one’s transplant.
These findings have implications for psychosocial interventions with cancer survivors, which often focus on increasing social support without attending to social constraints. Social support and constraints are largely independent (Lepore & Revenson, 2007). Thus, interventions that increase social support will not necessarily decrease social constraints, which may partially explain the generally disappointing effects of social support interventions for cancer survivors (Helgeson & Cohen, 1996; Lepore & Coyne, 2006). Survivors who perceive social constraints from their partner may benefit from intervention to enhance communication (Manne et al., 2007; Porter et al., 2009). If communication with the partner cannot be improved, alternative opportunities for safe disclosure (e.g., psychotherapy, support groups), may be helpful. Finally, individuals experiencing loneliness may benefit from interventions targeting maladaptive social cognitions, as suggested by a meta-analysis (Masi, Chen, Hawkley, & Cacioppo, in press).
Limitations of the current research should be noted. First, the cross-sectional study design precluded assessment of causal relations among variables. Future longitudinal analyses may reveal bi-directional relationships between social factors and distress. Second, consistent with HSCT survivor demographics (Joshua et al., 2010), participants were primarily married, Caucasian, and middle to upper class. Third, participants consented to participate in an intervention trial and therefore they may differ in important ways (e.g., distress level) from survivors who would refuse participation. However, most survivors met the trial’s eligibility criteria, and the average level of distress was comparable to that found in prior descriptive research with this population (Rusiewicz et al., 2008). Finally, data from multiple individuals (e.g., family, healthcare professionals) should be gathered in future research to enhance understanding of relational processes following transplantation.
Strengths of the present study include the novel focus on loneliness as a mechanism underlying the relations between social factors and distress following HSCT, comparison of relative effects of positive (social support) versus negative (social constraints) social factors, and the identification of unique pathways through which these factors may influence distress. Findings suggest that interventions may be strengthened by addressing social constraints on disclosure and emotional support.
Acknowledgments
This study was supported by grant RSGPB-07-285-01-CPPB from the American Cancer Society, awarded to Christine Rini.
We would like to thank Katie Basmajian and Anna Marie Vu for assistance with recruitment and data collection for this study.
Footnotes
Details of screening measures are available from the last author.
References
- Andrykowski MA, Cordova MJ, Hann DM, Jacobsen PB, Fields KK, Phillips G. Patients' psychosocial concerns following stem cell transplantation. Bone Marrow Transplantation. 1999;24:1121–1129. doi: 10.1038/sj.bmt.1702022. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS Structural Equations Program Manual. Los Angeles: BMDP Statistical Software; 1992. [Google Scholar]
- Boer H, Elving WJL, Seydel ER. Psychosocial factors and mental health in cancer patients: Opportunities for health promotion. Psychology, Health, and Medicine. 1998;3:71–79. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou CP, Bentler PM. Model modification in covariance structure modeling: A comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behavioral Research. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Cohen MZ, Ley C, Tarzian AJ. Isolation in blood and marrow transplantation. Western Journal of Nursing Research. 2001;23:592–609. doi: 10.1177/019394590102300605. [DOI] [PubMed] [Google Scholar]
- Copelan EA. Hematopoietic stem-cell transplantation. New England Journal of Medicine. 2006;354:1813–1826. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- Cordova MJ, Cunningham LL, Carlson CR, Andrykowski MA. Social constraints, cognitive processing, and adjustment to breast cancer. Journal of Consulting and Clinical Psychology. 2001;69:706–711. [PubMed] [Google Scholar]
- Cordova MJ, Walser R, Neff J, Ruzek JI. Predictors of emotional adjustment following traumatic injury: personal, social, and material resources. Prehospital and Disaster Medicine. 2005;20:7–13. doi: 10.1017/s1049023x00002089. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. 3. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation. 2009;43:959–966. doi: 10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychology. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- Hjermstad MJ, Loge JH, Evensen SA, Kvaloy SO, Fayers PM, Kaasa S. The course of anxiety and depression during the first year after allogeneic or autologous stem cell transplantation. Bone Marrow Transplantation. 1999;24:1219–1228. doi: 10.1038/sj.bmt.1702046. [DOI] [PubMed] [Google Scholar]
- Horowitz M. Stress-response syndromes: A review of posttraumatic and adjustment disorders. Hospital and Community Psychiatry. 1986;37:241–249. doi: 10.1176/ps.37.3.241. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- House JS, Kahn RL. Measures and concepts of social support. In: Cohen S, Syme L, editors. Social Support and Health. Orlando, FL: Academic Press; 1985. pp. 83–108. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jenks Kettmann JD, Altmaier EM. Social support and depression among bone marrow transplant patients. Journal of Health Psychology. 2008;13:39–46. doi: 10.1177/1359105307084310. [DOI] [PubMed] [Google Scholar]
- Joshua TV, Rizzo JD, Zhang MJ, et al. Access to hematopoietic stem cell transplantation: effect of race and sex. Cancer. 2010;116:3469–3476. doi: 10.1002/cncr.25297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Fairclough D, Parsons SK, et al. Recovery after stem-cell transplantation for hematologic diseases. Journal of Clinical Oncology. 2001;19:242–252. doi: 10.1200/JCO.2001.19.1.242. [DOI] [PubMed] [Google Scholar]
- Lepore SJ. A social-cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen BL, editors. Psychosocial Interventions for Cancer. Washington, DC: American Psychological Association; 2001. pp. 99–118. [Google Scholar]
- Lepore SJ, Coyne JC. Psychological interventions for distress in cancer patients: a review of reviews. Annals of Behavioral Medicine. 2006;32:85–92. doi: 10.1207/s15324796abm3202_2. [DOI] [PubMed] [Google Scholar]
- Lepore SJ, Helgeson VS. Social constraints, intrusive thoughts, and mental health after prostate cancer. Journal of Social and Clinical Psychology. 1998;17:89–106. [Google Scholar]
- Lepore SJ, Ituarte PHG. Optimism about cancer enhances mood by reducing negative social interactions. Cancer Research, Therapy, and Control. 1999;8:165–174. [Google Scholar]
- Lepore SJ, Revenson TA. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007;1:313–333. [Google Scholar]
- Manne SL, Ostroff J, Winkel G, Grana G, Fox K. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: patient and partner perspectives. Health Psychology. 2005;24:635–641. doi: 10.1037/0278-6133.24.6.635. [DOI] [PubMed] [Google Scholar]
- Manne SL, Rubin S, Edelson M, et al. Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2007;75:615–628. doi: 10.1037/0022-006X.75.4.615. [DOI] [PubMed] [Google Scholar]
- Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. doi: 10.1177/1088868310377394. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher CE, Duhamel KN, Rini C, Corner G, Lam J, Redd WH. Quality of life concerns and depression among hematopoietic stem cell transplant survivors. Supportive Care in Cancer. 2011;19:1357–1365. doi: 10.1007/s00520-010-0958-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psycho-Oncology. 2009;18:113–127. doi: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsom JT, Rook KS, Nishishiba M, Sorkin DH, Mahan TL. Understanding the relative importance of positive and negative social exchanges: examining specific domains and appraisals. Journals of Gerontology: Psychological Sciences. 2005;60:P304–P312. doi: 10.1093/geronb/60.6.p304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Frohlich C, Silbereisen RK. Cancer patients' perceptions of positive and negative illness-related changes. Journal of Health Psychology. 2007;12:907–921. doi: 10.1177/1359105307082454. [DOI] [PubMed] [Google Scholar]
- Porter LS, Keefe FJ, Baucom DH, et al. Partner-assisted emotional disclosure for patients with gastrointestinal cancer: results from a randomized controlled trial. Cancer. 2009;115(18 Suppl):4326–4338. doi: 10.1002/cncr.24578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rini C, Dunkel Schetter C. The effectiveness of social support transactions in intimate relationships. In: Davila J, Sullivan K, editors. Support Processes in Intimate Relationships. New York: Oxford; 2010. pp. 26–67. [Google Scholar]
- Rini C, Manne S, DuHamel K, et al. Social support from family and friends as a buffer of low spousal support among mothers of critically ill children: A multilevel modeling approach. Health Psychology. 2008;27:593–603. doi: 10.1037/0278-6133.27.5.593. [DOI] [PubMed] [Google Scholar]
- Rini C, Redd WH, Austin J, et al. Effectiveness of partner social support predicts enduring psychological distress after hematopoietic stem cell transplantation. Journal of Consulting and Clinical Psychology. 2011;79:64–74. doi: 10.1037/a0022199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rook KS. Social support versus companionship: effects on life stress, loneliness, and evaluations by others. Journal of Personality and Social Psychology. 1987;52:1132–1147. doi: 10.1037//0022-3514.52.6.1132. [DOI] [PubMed] [Google Scholar]
- Rusiewicz A, DuHamel KN, Burkhalter J, et al. Psychological distress in long-term survivors of hematopoietic stem cell transplantation. Psycho-Oncology. 2008;17:329–337. doi: 10.1002/pon.1221. [DOI] [PubMed] [Google Scholar]
- Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Salsman JM, Segerstrom SC, Brechting EH, Carlson CR, Andrykowski MA. Posttraumatic growth and PTSD symptomatology among colorectal cancer survivors: a 3-month longitudinal examination of cognitive processing. Psycho-Oncology. 2009;18:30–41. doi: 10.1002/pon.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. Scaling corrections for chi-square statistics in covariance structure analysis. Journal of the American Statistical Association. 1988;1:308–313. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111:989–996. doi: 10.1182/blood-2007-06-096594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syrjala KL, Langer SL, Abrams JR, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. Journal of the American Medical Association. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Social support and psychological well-being: Theoretical possibilities. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research, and Applications. Dordrecht, The Netherlands: Martinus Nijhoff; 1985. pp. 51–72. [Google Scholar]
- Uitenbroek, DG. SISA Correlations. Southampton: D.G. Uitenbroek; 1999. Available at: http://www.quantitativeskills.com/sisa/ [Google Scholar]
- Wei M, Russell DW, Zakalik RA. Adult attachment, social self-efficacy, self-disclosure, loneliness, and subsequent depression for freshman college students: A longitudinal study. Journal of Counseling Psychology. 2005;52:602–614. [Google Scholar]
- Wingard JR, Huang IC, Sobocinski KA, et al. Factors associated with self-reported physical and mental health after hematopoietic cell transplantation. Biology of Blood and Marrow Transplantation. 2010;16:1682–1692. doi: 10.1016/j.bbmt.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Zakowski SG, Ramati A, Morton C, Johnson P, Flanigan R. Written emotional disclosure buffers the effects of social constraints on distress among cancer patients. Health Psychology. 2004;23:555–563. doi: 10.1037/0278-6133.23.6.555. [DOI] [PubMed] [Google Scholar]