Abstract
OBJECTIVE
South Africa has the highest rate of fetal alcohol syndrome (FAS) in the world. While efforts have been made to curb the high rate of FAS, little is known about situational factors that may contribute to alcohol use during pregnancy. In the current paper, we focus on the role of food insecurity and its relationship to alcohol use among pregnant women.
DESIGN
Women completed computed assisted interviews. Generalized linear modeling was used in all analyses.
SETTING
Women attending alcohol serving establishments in a township in Cape Town, South Africa were recruited for the study.
PARTICIPANTS
Five hundred sixty women were sampled and 95 women reported being pregnant.
RESULTS
High levels of alcohol use were reported among pregnant women: 65% of women consumed alcohol at least every month and 29% consumed alcohol as often as two to three times per week. Thirty four percent of the women reported having 6 or more drinks per occasion on at least a weekly basis. The majority (87%) of pregnant women reported experiencing some form of food insecurity (e.g. food unavailable, eating less) in the past month. Alcohol use was significantly associated with food insecurity, even when controlling for relevant demographic variables.
CONCLUSIONS
Intervention with pregnant women who consume alcohol is urgently needed. Future research should focus on understanding the intersection of food insecurity and alcohol, and how the experience of food insecurity may contribute to greater rates of alcohol use and abuse among pregnant women.
Keywords: Food insecurity, alcohol use, pregnant women
INTRODUCTION
Alcohol use among pregnant women residing within South African townships is prevalent and alarming (Eaton et al., 2012; May et al., 2007; Morojele et al., 2010; Rosenthal, Christianson, & Cordero, 2005). Rates of fetal alcohol syndrome (FAS) in South Africa are the highest in the world (“Fetal alcohol syndrome--South Africa, 2001,” 2003). The Western Cape Province of South Africa in particular has the highest rates of FAS ranging from 43.8–89.2 per 1,000 children; by comparison, the United States and Canada have rates generally observed at 1 per 1,000 children (May et al., 2000; May et al., 2009; May et al., 2007; Viljoen et al., 2005). FAS is directly linked to a multitude of negative health outcomes including deficiencies in the growth and development of cognitive and physical capabilities, particularly damage to the central nervous system. The effects of FAS are life-long with only limited treatment available (Adnams et al., 2001; Kodituwakku et al., 2006; Peltzer, Seoka, Babor, & Obot, 2006). Furthermore, FAS has had a devastating impact on the Western Cape economy and health care system (Crede, Sinanovic, Adnams, & London, 2010).
Heavy alcohol use occurs in informal drinking establishments or shebeens and taverns within many townships in South Africa (Kalichman, Simbayi, Jooste, Vermaak, & Cain, 2008; Kalichman, Simbayi, Cain, & Jooste, 2007; Kalichman, Simbayi, Jooste, & Cain, 2007; Kalichman, Simbayi, Vermaak, Cain, et al., 2008; Kalichman, Simbayi, Vermaak, Jooste, & Cain, 2008; Schneider, Norman, Parry, Bradshaw, & Pluddemann, 2007; Suliman, Seedat, Williams, & Stein, 2010). As such, South Africa has high rates of hazardous drinking. Although the proportion of South Africans who drink alcohol is fairly low (in a national household survey just 39% of men and 16% of women reported alcohol use in the past year), South Africa has one of the highest per-capita rates of alcohol consumption in the world among those who do consume alcohol (Parry, 2010; Rehm, Rehn, et al., 2003). Likewise, patterns of detrimental alcohol use tend to be more severe in South Africa (Gruenewald et al., 2002; Rehm, Room, et al., 2003; Rehm, Sempos, & Trevisan, 2003), compared to other parts of the world (Rehm, Rehn, et al., 2003).
Given the devastating health outcomes associated with FAS, the alarmingly high rates of FAS in South Africa, and the recognition that proper pre-natal health care can entirely prevent FAS, concerted efforts must be made to prevent the syndrome (Morojele et al., 2010; Parry, 2010; Peltzer, 2006; Peltzer et al., 2006). However, to date, limited data exists to inform our understanding of the contextual factors related to alcohol intake during pregnancy in South Africa. This lack of research, in turn, has stymied efforts to intervene and provide prevention options (Rosenthal et al., 2005).
Studies outside of South Africa have identified multiple negative psycho-social factors as contributing to an increased likelihood of alcohol use during pregnancy (Skagerstrom, Chang, & Nilsen, 2011). One area that has been overlooked, yet has been linked to alcohol use in non-pregnant individuals, is that of food insecurity (Sirotin et al., 2012). Food insecurity -a vital component of nutrition- concerns the availability, access, and nutritional content of one’s food. Food insecurity within South African households is under-studied; however there is agreement that it affects a substantial number of South Africans. In 2008, as many as one in four individuals in a national South Africa survey reported food insecurity (Labadarios et al., 2011). This percentage is down from 52% reported in both 1999 and 2005 suggesting that government policies relating to food supplementation, food fortification and school food programs have improved food insecurity. However, large numbers of individuals continue to report food insecurity, and women are disproportionately, negatively affected by food insecurity (Altman, Hart, & Jacobs, 2009).
Although multiple studies have investigated the use of alcohol among pregnant women in South Africa e.g.,(Desmond et al., 2012; Eaton et al., 2012; May et al., 2000; O’Connor et al., 2011), less is known about its relationship to food insecurity among pregnant women. Studies examining the physiological relationship between alcohol and nutrition have demonstrated that alcohol inhibits the absorption of nutrients by decreasing the functioning of digestive enzymes (Korsten, 1989). More recently, research has emerged suggesting that poor nutrition is, in fact, a critical factor in the development of FAS as it amplifies the teratogenic effects of alcohol (Carter, Jacobson, Molteno, & Jacobson, 2007; Faden, Hanna, & Graubard, 1997; Keen et al., 2010; K. Shankar, Ronis, & Badger, 2007; Xu et al., 2006). Poor nutrition compromises the body’s ability to effectively metabolize and clear ethanol, thus leading to greater ethanol toxicity. Likewise, it is believed that nutritionally rich diets can act as a buffer to protect fetal development among alcohol using pregnant women (Eaton et al., 2012; May et al., 2007; Morojele et al., 2010; Rosenthal et al., 2005). Therefore, food insecurity is a vital component to account for when assessing factors that contribute to the development of FAS. And finally, guidance is needed on how to frame the role of food insecurity in understanding high rates of FAS among alcohol using pregnant women.
For the current study, we used data collected from a cohort study to assess alcohol use, food security and the relationship between these two constructs among pregnant women attending alcohol serving establishments (shebeens and taverns) in Cape Town, South Africa. This paper is an exploratory study of the associations between alcohol use and food security. However, we use these findings to generate a conceptual model to explicate the relationships between food insecurity and alcohol use, and to generate hypotheses around contextual- and individual-level factors important in understanding FAS. Given the documented high rates of FAS in Cape Town, we predicted that alcohol use among pregnant women would be commonly reported. Furthermore, we expected that alcohol consumption, frequency, and problematic alcohol use will be associated with experiencing food insecurity among pregnant women.
METHODS
Participants were women attending alcohol serving establishments in a peri-urban township in Cape Town, South Africa. The township is located within 20 kilometers of Cape Town’s central business district and consists of both people of mixed ethnicity (i.e., Coloureds) and Black Africans. A relatively new township, the community was established in 1990 and is one of the first townships in South Africa to racially integrate. Large numbers of indigenous Black Africans started settling in and around the township during the 1990’s after government policies of racial segregation during Apartheid ended. The township sampled for this study, therefore, offers the opportunity to survey women of varying cultures residing within one South African community.
Venue Selection
Using an adaptation of the Priorities for Local AIDS Control Efforts (PLACE) community mapping methodology (Weir, Morroni, Coetzee, Spencer, & Boerma, 2002), we located and defined alcohol serving establishments in the township for the current study. Alcohol serving venues were systematically identified by approaching a total of 509 members of the community at public places such as bus stands and markets, and asking them to identify places where people go to drink alcohol. Venues were eligible if they had space for patrons to sit and drink, reported >50 unique patrons per week, had >10% female patrons, and were willing to have the research team visit periodically over the course of a year.
Participant Recruitment
Women from a total of twelve alcohol-serving venues were recruited for this study. Field staff invited female shebeen patrons to be part of a cohort study examining alcohol use among women over the course of one year. Women were eligible to participate if they were (a) at least 18 years of age; (b) drank alcohol in the venue and (c) lived in the township. A total of 604 women were approached to participate and given an appointment card to come to the study office to provide informed consent and complete a baseline assessment. Almost all (560, 92.7%) came for the initial appointment and enrolled in the study. Seventeen percent (N=95) of women recruited from alcohol serving establishments reported being pregnant. Study recruitment occurred over June 2009–May 2011.
Study Design
Women in the prospective cohort were assessed at three time points, each being four months apart. We used data from the time point in which the participant first reported being pregnant. Assessment measures were administered at a community-based research site located within a community center in the township using audio computer-assisted self-interviews (ACASI) delivered in English, Xhosa and Afrikaans, the three dominant languages spoken by persons in the township. Research has shown that ACASI procedures yield reliable responses in behavioral interviews (Gribble, HG, Rogers, & Turner, 1999; Turner, Ku, Sonenstein, & Pleck, 1996). Participants were given a grocery store voucher (150ZAR, or approximately 20USD) at each time point in exchange for their participation.
Measures
Measures were adapted from previous research conducted in South Africa (Eaton et al., 2012; Kalichman, Cain, Eaton, Jooste, & Simbayi, 2011; Scott-Sheldon et al., 2012; Sikkema et al., 2011). All of the measures were translated and back-translated to produce parallel forms in the three languages of administration.
Demographics
Participants were asked to report age, education, ethnicity, employment, marital status, having children, having electricity, having indoor tap water, and having a refrigerator.
Food Insecurity
We assessed food insecurity using items adapted from the USDA Food Security Scale (Bickel, Nord, Price, Hamilton, & Cook, 2000). We used eight items that focused on different aspects of food insecurity that a participant may have experienced in the previous month. Example items included, “In the past month, I could not feed my family;” and “In the past month, I or other adults in the household cut the size of our meals because there wasn’t enough money for food.” Responses were given on a 4 point scale with 0 = never, 1 = once or twice, 2 = every week, 3 = every day (α = .90). We provide descriptive information for each of the responses and then for analytic purposes we dichotomized food insecurity as either not experiencing it (responding “never”) or as having experienced it (responding “once or twice”, “every week”, or “every day”).
Alcohol Use
To assess alcohol use, we used the Alcohol Use Disorder Identification Test (AUDIT (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993)). This measure is a 10-item self-report instrument that includes quantity and frequency of alcohol use and is designed to identify individuals for whom the use of alcohol places them at risk for developing alcohol problems or who are currently experiencing alcohol problems (Catalan, Day, & Gallwey, 1988; Conigrave, Hall, & Saunders, 1995). Items were summed according to Saunders et al (Saunders et al., 1993). Scores ≥8 are considered an indicator of problematic alcohol use (Saunders et al., 1993).
Data analysis
We conducted descriptive analyses of sample demographic characteristics, alcohol use and food insecurity. We compared food insecurity and alcohol use among pregnant and non-pregnant women using t-tests. Generalized linear modeling (GZLM) with a Poisson distribution was used to model the relationship between alcohol use and food insecurity among pregnant women. Furthermore, GZLM with a binary logistic distribution was used to test for differences in AUDIT scores between pregnant women who did and did not report food insecurity. All analyses controlled for age, ethnicity, education, and marital status. There were less than 5% missing data for any given variable. For all analyses, we used p < .05 to define statistical significance. PASW Statistics version 18.0 (SPSS Inc., Chicago, IL) was used for all analyses.
RESULTS
Seventeen percent of women recruited from alcohol serving establishments reported being pregnant (95 out of 560). We compared alcohol use and food insecurity between pregnant and non-pregnant women. We found no differences between groups on these items (AUDIT scores-pregnant M=12.56, SD=8.08; non-pregnant M=12.76, SD=7.76 [t=.23(558) p=.82]; food insecurity sum-pregnant M=7.59, SD=5.74; non-pregnant M=8.58, SD=5.85 [t=1.51(558) p=.13]). Given our focus on alcohol use and food insufficiency among pregnant women and similar findings on these items between groups, we limited all further analyses to women reporting being pregnant (n=95). For women reporting being pregnant at more than one time point, we limited data analyses to the first time point they reported their pregnancy.
Women reported an average age of 29 years old and an average education of Grade 9. About one out of five women were married (21%) and a quarter of women were employed (25%). Almost all women were either of Black (38%) or Coloured (59%) ethnicity. Most women reported residing in a house with electricity (94%), indoor water (86%) and a refrigerator (85%). One in four women reported having children (Table 1).
Table 1.
Demographic characteristics of pregnant women attending alcohol serving establishments in Cape Town, South Africa (N=95).
| Pregnant Women | |||
|---|---|---|---|
| M | SD | ||
| Age | 29.85 | 9.73 | |
| Education | 5.34 | 2.22 | |
| n | % | ||
|
|
|||
| Married | 20 | 21 | |
| Employed | 24 | 25 | |
| Ethnicity | |||
| Black | 36 | 38 | |
| Coloured | 56 | 59 | |
| Other | 3 | 3 | |
| House has electricity? | 89 | 94 | |
| House has indoor water? | 82 | 86 | |
| Do you have a refrigerator? | 81 | 85 | |
| Do you have any children? | 24 | 25 | |
Note: Mean for education corresponds to grade 9.
Overall, pregnant women reported substantial alcohol use (Table 2). AUDIT scores averaged 12.56 (SD = 8.07). Sixty-nine percent of the sample had audit scores above the threshold of eight, suggesting behaviors and experiences indicative of problematic alcohol use. Sixty-five percent of women stated that they consumed alcohol at least every month, with 29% of women reporting consuming alcohol as often as two to three times per week. Sixty-nine percent of women reported consuming at least 3–4 drinks during a typical drinking session; 14% responded having at least 10 alcohol drinks during a typical session. Thirty-four percent of women reported binge drinking alcohol (6 or more drinks) at least weekly. Forty-one percent of women stated they were not able to stop drinking once they started on at least a monthly basis. A substantial number of women also reported guilt or shame in regards to their drinking, needing a drink first thing in the morning, and failing to do what was expected of them due to alcohol use. Finally, 27% of women reported, at least on a monthly basis, that they were unable to remember what happened the night before when consuming alcohol.
Table 2.
Alcohol use (AUDIT items) among pregnant women attending alcohol serving establishments in Cape Town, South Africa (N=95).
| Pregnant Women | ||
|---|---|---|
| n | % | |
| How often do you have a drink containing alcohol? | ||
| Never | 7 | 7 |
| Monthly or less | 27 | 28 |
| 2–4 times a month | 33 | 35 |
| 2–3 times a week | 20 | 21 |
| More than 4 times a week | 8 | 8 |
| How many drinks containing alcohol do you have on a typical day when you are drinking? | ||
| I don’t drink | 7 | 7 |
| 1–2 | 22 | 23 |
| 3–4 | 26 | 27 |
| 5–6 | 20 | 21 |
| 7–9 | 7 | 7 |
| 10 or more | 13 | 14 |
| How often do you have 6 or more drinks on one occasion? | ||
| Never | 19 | 20 |
| Less than monthly | 28 | 30 |
| Monthly | 16 | 17 |
| Weekly | 29 | 31 |
| Daily or almost daily | 3 | 3 |
| How often during the last year have you not been able to stop drinking once you started? | ||
| Never | 35 | 37 |
| Less than monthly | 21 | 22 |
| Monthly | 12 | 13 |
| Weekly | 23 | 24 |
| Daily or almost daily | 4 | 4 |
| How often during the last year have you failed to do what you are normally expected to do because you were drinking? | ||
| Never | 41 | 43 |
| Less than monthly | 24 | 25 |
| Monthly | 13 | 14 |
| Weekly | 13 | 14 |
| Daily or almost daily | 4 | 4 |
| How often during the last year have you needed a first thing drink in the morning to get yourself going? | ||
| Never | 50 | 53 |
| Less than monthly | 19 | 20 |
| Monthly | 10 | 11 |
| Weekly | 12 | 13 |
| Daily or almost daily | 3 | 3 |
| How often during the last year have you had a feeling of guilt or shame after drinking? | ||
| Never | 38 | 40 |
| Less than monthly | 22 | 23 |
| Monthly | 10 | 11 |
| Weekly | 11 | 12 |
| Daily or almost daily | 14 | 15 |
| How often during the last year have you been unable to remember what happened the night before because you had been drinking? | ||
| Never | 50 | 53 |
| Less than monthly | 20 | 21 |
| Monthly | 9 | 10 |
| Weekly | 9 | 10 |
| Daily or almost daily | 7 | 7 |
| Have you or someone else been injured as a result of your drinking? | ||
| No | 72 | 76 |
| Yes, in the past year | 14 | 15 |
| Yes, not in the past year | 9 | 10 |
| Has a relative or friend or health worker been concerned about your drinking and suggested that you cut down? | ||
| No | 52 | 55 |
| Yes, in the past year | 36 | 38 |
| Yes, not in the past year | 7 | 7 |
Eighty-seven percent of women reported experiencing at least one event in the past month consistent with food insecurity (Table 3). For each of the food insecurity items, more than half the women sampled reported experiencing it in the past month. Of particular concern for maternal health and fetal development: 76% of women reported being hungry, but couldn’t afford food, and 63% of women stated being unable to afford to buy a balanced meal.
Table 3.
Food insecurity among pregnant women attending alcohol serving establishments in Cape Town, South Africa (N=95).
| How often experienced in past month: | Pregnant Women | |||
|---|---|---|---|---|
| Never % | Once or twice % | Every week % | Every Day % | |
| I could not feed my family | 46 | 32 | 13 | 10 |
| The food I bought just didn’t last and I didn’t have money to get more | 32 | 45 | 16 | 7 |
| I ate less than I felt I needed to because there wasn’t enough money for food | 27 | 48 | 18 | 6 |
| I was hungry, but didn’t eat because I couldn’t afford enough food | 34 | 43 | 16 | 7 |
| I worried whether my food would run out before I got money to buy more | 31 | 43 | 19 | 7 |
| I couldn’t afford to eat balanced meals | 38 | 38 | 15 | 10 |
| I or other adults in my household did not eat for a whole day because there wasn’t enough money for food | 46 | 39 | 8 | 6 |
| I or other adults in the household cut the size of our meals because there wasn’t enough money for food | 34 | 41 | 13 | 12 |
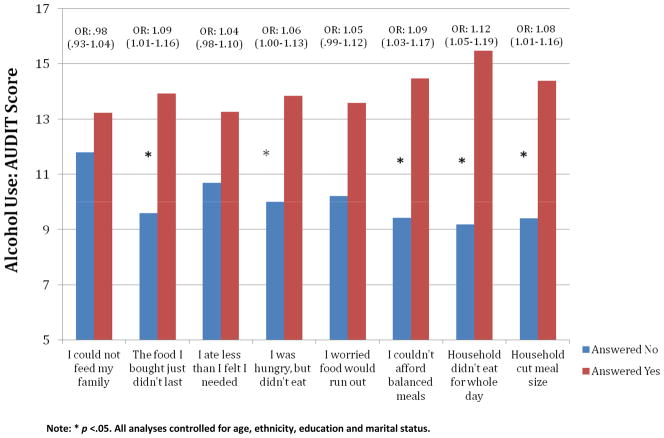
In examining the relationship between alcohol use and food security, we found a significant positive relationship between increased AUDIT scores and greater likelihood of experiencing food insecurity (AOR: 1.03, 95%CI: 1.02–1.04, controlling for demographic variables). To further understand this relationship, we compared the average AUDIT score for each food insecurity item (Figure 1). For five of the eight items, AUDIT scores were greater among women who reported experiencing the event in the past month. For the remaining three items, no significant differences emerged.
Figure 1.
The relationship between alcohol use and food insecurity among pregnant women attending alcohol serving establishments in Cape Town, South Africa (N=95).
Note: * p <.05. All analyses controlled for age, ethnicity, education and marital status.
DISCUSSION
This study explored the relationship between alcohol use and food insecurity among pregnant women attending alcohol serving venues in South Africa. Consistent with national data on FAS, data from the current study demonstrate alarmingly high rates of alcohol use among pregnant women attending alcohol serving establishments in a Cape Town, South African township. A majority of pregnant women reported that they regularly consumed moderate to heavy amounts of alcohol. Furthermore, a majority of the sample lacked access to a stable supply of food.
There exists an urgent need to intervene with pregnant women representative of those sampled in the current study. Efforts must be concentrated on all women of childbearing age in order to mitigate the negative effects of alcohol use during pregnancy while concurrently addressing food insecurity. South Africa has demonstrated some success in alleviating food insecurity among many of its residents; however, given the persistent rates of FAS more needs to be done to create an environment wherein pregnant women who use alcohol are provided with reliable access to food.
Although the exact causal factors driving the relationship between food insecurity and alcohol use are unknown, for the purpose of guiding future studies we used data from the current paper and available literature to form a hypothesized conceptual model that more fully explicates important pathways affecting alcohol use and food insecurity (Figure 2). To begin, it is known that resources and accessibility of food and alcohol (Blankenship, Friedman, Dworkin, & Mantell, 2006) are two critical determinants of their use. Alcohol serving establishments are plentiful in townships and large volumes of alcoholic drinks can be purchased with little monetary currency. In contrast, local food vendors are small in numbers. It’s possible that women are more likely to be spending money on alcohol than food as alcohol is, by and large, more easily accessible and requires fewer resources to secure. We hypothesize that employment, marriage, governmental support, transactional sex, and exchange of goods are the most commonly used means to gain resources to access food and alcohol; and that proximity to food/alcohol stores, available transportation, and available food/alcohol options drive accessibility (see Figure 2 for pathways). Once resources and accessibility have been determined, decision making around securing food and alcohol likely becomes critical. These decisions may be affected by social context (such as social norms and expectations), education around self-care during pregnancy, and addiction (patterns of alcohol use suggest that addiction is a central factor). Ultimately, we hypothesize that the larger contextual setting (resources/accessibility) and critical individual-level factors are ultimately driving resultant alcohol use and food insecurity, and their relationship to one another.
Figure 2.
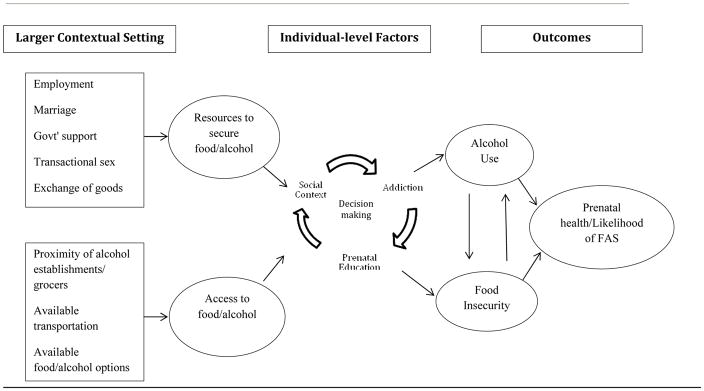
Conceptual/hypothetical model of pathways influencing alcohol use and food insecurity.
Research on the health, in particular in the area of nutrition, of pregnant women has focused on multiple interventions including: supplementation of iron folate, iodine, calcium, vitamin A and multiple micronutrients; nutritional based counseling; and less direct interventions to improve nutrition: mental health interventions, family planning; cash transfers; and food-for-work programs (Bhutta et al., 2008; Haider, Yakoob, & Bhutta, 2011). Programs focused on supplementation of multiple micronutrients have largely received the greatest attention and have demonstrated positive results (Haider & Bhutta, 2006; Haider et al., 2011; Huybregts et al., 2009; A. H. Shankar et al., 2008; Sunawang, Utomo, Hidayat, Kusharisupeni, & Subarkah, 2009). However, the World Health Organization states, “Although maternal nutrition and low birth weight are recognized as crucially important, WHO does not have a comprehensive strategy to address this issue” (WHO, Accessed June 26, 2012). This sentiment is consistent with the lack of available interventions for pregnant women experiencing multiple co-morbidities. Efforts to combat maternal malnutrition are mainly focused on developing strategies that would fit within the infrastructure of resource limited countries. To that end, there is urgent need for community leaders, medical professionals and other key stake-holders to develop and promote effective methods for mitigating maternal food insecurity.
In addition to researching and developing nutritional programs, more research is needed that specifically focuses on intervening with alcohol using, malnourished pregnant women. Existing data has documented the possibility of multiple micronutrient supplements protecting against the negative effects of fetal alcohol exposure. Research in this area is preliminary, yet the data are compelling and demonstrate the possibility of micronutrient supplementation as having a critical role in preventing FAS (Ammon Avalos, Kaskutas, Block, & Li, 2009; Avalos, Kaskutas, Block, Abrams, & Li, 2011; Ballard, Sun, & Ko, 2012). It is possible that the administration of fortified foods and micronutrient capsules during prenatal care could prevent FAS. Of course, these programs should be coupled with intensive alcohol treatment counseling including social-cognitive counseling strategies.
Findings from the current study should be viewed in light of their limitations. Results are limited to women attending alcohol serving establishments and can’t be generalized to the larger population. Findings related to alcohol use and food security are likely to vary between people who do and do not attend alcohol serving establishments. Data were cross-sectional, which precludes reporting on causal findings. We also relied on self-report of potentially stigmatizing behaviors, which could potentially bias responses. This work would benefit from incorporating a measure of nutrition. The current study measured food insecurity which doesn’t address the nutritional value of the foods that are being consumed. Pregnancy was based on self-report and we did not collect information on stage of pregnancy.
An area of important future research is that of the prenatal care habits among pregnant women consuming alcohol. Engagement in care is likely a critical factor in understanding the relationship between alcohol and food security; however, we were unable to present on this information. Given the considerable number of pregnant women attending alcohol serving establishments, these venues may serve an important function in engaging women into care. This information is necessary for determining effective strategies for intervening with women at risk for fetal alcohol exposure. Due to the consequences of alcohol misuse and abuse, it is likely that alcohol using pregnant women do not seek out regular prenatal care and likely delay initial contact with obstetric health care providers.
There is an urgent need to better and more fully address alcohol use behaviors among pregnant women residing in South African townships. The high rates of FAS demand considerable action to raise awareness about the negative effects of alcohol use during pregnancy. Focusing on the environment wherein alcohol use occurs will likely be a critical objective in curbing alcohol use among pregnant women. A combination of structural-level interventions to highlight the harms associated with alcohol use during pregnancy and individual-level treatment should be prioritized. Interventions aimed at reducing alcohol use among pregnant women should also focus on the broader context of these women’s lives that may be contributing to high levels of alcohol intake, in particular, food security. Without concentrated efforts to address alcohol use during pregnancy, rates of FAS in South Africa will likely continue to be among the highest in the world.
Acknowledgments
This project was supported by National Institute of Alcohol Abuse and Alcoholism grant R01 AA018074.
References
- Adnams CM, Kodituwakku PW, Hay A, Molteno CD, Viljoen D, May PA. Patterns of cognitive-motor development in children with fetal alcohol syndrome from a community in South Africa. Alcoholism: Clinical and Experimental Research. 2001;25:557–562. [PubMed] [Google Scholar]
- Ammon Avalos L, Kaskutas LA, Block G, Li DK. Do multivitamin supplements modify the relationship between prenatal alcohol intake and miscarriage? American Journal of Obstetrics & Gynecology. 2009;201:563, e561–569. doi: 10.1016/j.ajog.2009.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avalos LA, Kaskutas L, Block G, Abrams B, Li DK. Does lack of multinutrient supplementation during early pregnancy increase vulnerability to alcohol-related preterm or small-for-gestational-age births? Maternal and Child Health Journal. 2011;15:1324–1332. doi: 10.1007/s10995-010-0690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard MS, Sun M, Ko J. Vitamin A, folate, and choline as a possible preventive intervention to fetal alcohol syndrome. Medical Hypotheses. 2012;78:489–493. doi: 10.1016/j.mehy.2012.01.014. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Sekar M. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–440. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. [Accessed September 1, 2012];United States Depertment of Agriculture, Office of Analysis Nutrition, and Evaluation. 2000 http://www.fns.usda.gov/fsec/files/fsguide.pdf.
- Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: concepts, challenges and opportunities for research. Journal of Urban Health. 2006;83:59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RC, Jacobson SW, Molteno CD, Jacobson JL. Fetal alcohol exposure, iron-deficiency anemia, and infant growth. Pediatrics. 2007;120:559–567. doi: 10.1542/peds.2007-0151. [DOI] [PubMed] [Google Scholar]
- Catalan J, Day A, Gallwey J. Alcohol misuse in patients attending a genitourinary clinic. Alcohol and Alcoholism. 1988;23:421–428. doi: 10.1093/oxfordjournals.alcalc.a044838. [DOI] [PubMed] [Google Scholar]
- Center for Poverty Employment and Growth. Food Secruity in South Africa. Cape Town, South Africa: Altman, M., Hart, T., & Jacobs, P; 2009. [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: choosing a cut-off score. Alcohol Use Disorder Identification Test. Addiction. 1995;90:1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. [DOI] [PubMed] [Google Scholar]
- Crede S, Sinanovic E, Adnams C, London L. The utilization of health care services by children with Foetal Alcohol Syndrome in the Western Cape, South Africa. Drug and Alcohol Dependency. 2010;115:175–182. doi: 10.1016/j.drugalcdep.2010.10.019. [DOI] [PubMed] [Google Scholar]
- Desmond K, Milburn N, Richter L, Tomlinson M, Greco E, van Heerden A, Rotheram-Borus MJ. Alcohol consumption among HIV-positive pregnant women in KwaZulu-Natal, South Africa: prevalence and correlates. Drug and Alcohol Dependency. 2012;120:113–118. doi: 10.1016/j.drugalcdep.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Kalichman SC, Sikkema KJ, Skinner D, Watt MH, Pieterse D, Pitpitan EV. Pregnancy, alcohol intake, and intimate partner violence among men and women attending drinking establishments in a Cape Town, South Africa township. Journal of Community Health. 2012;37:208–216. doi: 10.1007/s10900-011-9438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faden VB, Hanna E, Graubard BI. The effect of positive and negative health behavior during gestation on pregnancy outcome. Journal of Substance Abuse. 1997;9:63–76. doi: 10.1016/s0899-3289(97)90006-7. [DOI] [PubMed] [Google Scholar]
- Gribble J, HGM, Rogers S, Turner C. Interview mode and measurement of sexual behaviors: Methodological issues. The Journal of Sex Research. 1999:16–24. doi: 10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Russell M, Light J, Lipton R, Searles J, Johnson F, Nochajski TH. One drink to a lifetime of drinking: temporal structures of drinking patterns. Alcohol: Clinical and Experimental Research. 2002;26:916–925. [PubMed] [Google Scholar]
- Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2006;(4):CD004905. doi: 10.1002/14651858.CD004905.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider BA, Yakoob MY, Bhutta ZA. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public Health. 2011;11:S19. doi: 10.1186/1471-2458-11-S3-S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huybregts L, Roberfroid D, Lanou H, Menten J, Meda N, Van Camp J, Kolsteren P. Prenatal food supplementation fortified with multiple micronutrients increases birth length: a randomized controlled trial in rural Burkina Faso. American Journal of Clinical Nutrition. 2009;90:1593–1600. doi: 10.3945/ajcn.2009.28253. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Cain D, Eaton L, Jooste S, Simbayi LC. Randomized clinical trial of brief risk reduction counseling for sexually transmitted infection clinic patients in Cape Town, South Africa. American Journal of Public Health. 2011;101:e9–e17. doi: 10.2105/AJPH.2011.300236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi L, Jooste S, Vermaak R, Cain D. Sensation seeking and alcohol use predict HIV transmission risks: prospective study of sexually transmitted infection clinic patients, Cape Town, South Africa. Addictive Behavior. 2008;33:1630–1633. doi: 10.1016/j.addbeh.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cain D, Jooste S. Alcohol expectancies and risky drinking among men and women at high-risk for HIV infection in Cape Town South Africa. Addictive Behavior. 2007;32:2304–2310. doi: 10.1016/j.addbeh.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in Cape Town, South Africa. American Journal of Drug and Alcohol Abuse. 2007;33:687–698. doi: 10.1080/00952990701522716. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, Jooste S. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Annals of Behavioral Medicine. 2008;36:270–279. doi: 10.1007/s12160-008-9067-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prevention Science. 2008;9:55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- Keen CL, Uriu-Adams JY, Skalny A, Grabeklis A, Grabeklis S, Green K, Chanbers CD. The plausibility of maternal nutritional status being a contributing factor to the risk for fetal alcohol spectrum disorders: the potential influence of zinc status as an example. Biofactors. 2010;36:125–135. doi: 10.1002/biof.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodituwakku PW, Adnams CM, Hay A, Kitching AE, Burger E, Kalberg WO, May PA. Letter and category fluency in children with fetal alcohol syndrome from a community in South Africa. Journal of Studies of Alcohol and Drugs. 2006;67:502–509. doi: 10.15288/jsa.2006.67.502. [DOI] [PubMed] [Google Scholar]
- Korsten M. Alcoholism and pancreatitis: Does nutrition play a role? Alcohol Health and Research World. 1989;13:232–237. [Google Scholar]
- Labadarios D, McHiza ZJ, Steyn NP, Gericke G, Maunder EM, Davids YD, Parker WA. Food security in South Africa: a review of national surveys. Bulletin of the World Health Organization. 2011;89:891–899. doi: 10.2471/BLT.11.089243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Brooke L, Gossage JP, Croxford J, Adnams C, Jones KL, Viljoen D. Epidemiology of fetal alcohol syndrome in a South African community in the Western Cape Province. American Journal of Public Health. 2000;90:1905–1912. doi: 10.2105/ajph.90.12.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Gossage JP, Kalberg WO, Robinson LK, Buckley D, Manning M, Hoyme HE. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Developmental and Disability Research Review. 2009;15:176–192. doi: 10.1002/ddrr.68. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP, Marais AS, Adnams CM, Hoyme HE, Jones KL, Viljoen DL. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug and Alcohol Dependency. 2007;88:259–271. doi: 10.1016/j.drugalcdep.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morojele NK, London L, Olorunju SA, Matjila MJ, Davids AS, Rendall-Mkosi KM. Predictors of risk of alcohol-exposed pregnancies among women in an urban and a rural area of South Africa. Social Science and Medicine. 2010;70:534–542. doi: 10.1016/j.socscimed.2009.10.040. [DOI] [PubMed] [Google Scholar]
- O’Connor MJ, Tomlinson M, Leroux IM, Stewart J, Greco E, Rotheram-Borus MJ. Predictors of alcohol use prior to pregnancy recognition among township women in Cape Town, South Africa. Social Science and Medicine. 2011;72:83–90. doi: 10.1016/j.socscimed.2010.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry CD. Alcohol policy in South Africa: a review of policy development processes between 1994 and 2009. Addiction. 2010;105:1340–1345. doi: 10.1111/j.1360-0443.2010.03003.x. [DOI] [PubMed] [Google Scholar]
- Peltzer K. Prevalence of alcohol use by rural primary care outpatients in South Africa. Psychological Reports. 2006;99:176–178. doi: 10.2466/pr0.99.1.176-178. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Seoka P, Babor T, Obot I. Training primary care nurses to conduct alcohol screening and brief interventions in South Africa. Curationis. 2006;29:16–21. doi: 10.4102/curationis.v29i2.1067. [DOI] [PubMed] [Google Scholar]
- Rehm J, Rehn N, Room R, Monteiro M, Gmel G, Jernigan D, Frick U. The global distribution of average volume of alcohol consumption and patterns of drinking. European Addiction Research. 2003;9:147–156. doi: 10.1159/000072221. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Sempos CT, Trevisan M. Alcohol and cardiovascular disease--more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease--a review. Journal of Cardiovascular Risk. 2003;10:15–20. doi: 10.1097/01.hjr.0000051961.68260.30. [DOI] [PubMed] [Google Scholar]
- Rosenthal J, Christianson A, Cordero J. Fetal alcohol syndrome prevention in South Africa and other low-resource countries. American Journal of Public Health. 2005;95:1099–1101. doi: 10.2105/AJPH.2004.057372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schneider M, Norman R, Parry C, Bradshaw D, Pluddemann A. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. South African Medical Journal. 2007;97:664–672. [PubMed] [Google Scholar]
- Scott-Sheldon LA, Carey MP, Carey KB, Cain D, Harel O, Mehlomakulu V, Kalichman SC. Patterns of alcohol use and sexual behaviors among current drinkers in Cape Town, South Africa. Addictive Behaviors. 2012;37:492–497. doi: 10.1016/j.addbeh.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar AH, Jahari AB, Sebayang SK, Aditiawarman, Apriatni M, Harefa B, Sofia G. Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: a double-blind cluster-randomised trial. Lancet. 2008;371:215–227. doi: 10.1016/S0140-6736(08)60133-6. [DOI] [PubMed] [Google Scholar]
- Shankar K, Ronis MJ, Badger TM. Effects of pregnancy and nutritional status on alcohol metabolism. Alcohol Research & Health. 2007;30:55–59. [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Meade CS, Ranby KW, Kalichman SC, Skinner D, Pieterse D. Mental health and HIV sexual risk behavior among patrons of alcohol serving venues in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndrome. 2011;57:230–237. doi: 10.1097/QAI.0b013e3182167e7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirotin N, Hoover D, Segal-Isaacson CJ, Shi Q, Adedimeji A, Mutimura E, Anastos K. Structural determinants of food insufficiency, low dietary diversity and BMI: a cross-sectional study of HIV-infected and HIV-negative Rwandan women. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skagerstrom J, Chang G, Nilsen P. Predictors of drinking during pregnancy: a systematic review. Journal of Womens Health. 2011;20:901–913. doi: 10.1089/jwh.2010.2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suliman S, Seedat S, Williams DR, Stein DJ. Predictors of transitions across stages of alcohol use and alcohol-use disorders in South Africa. Journal of Studies on Alcohol and Drugs. 2010;71:695–703. doi: 10.15288/jsad.2010.71.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunawang, Utomo B, Hidayat A, Kusharisupeni, Subarkah Preventing low birthweight through maternal multiple micronutrient supplementation: a cluster-randomized, controlled trial in Indramayu, West Java. Food and Nutrition Bulletin. 2009;30:S488–495. doi: 10.1177/15648265090304S403. [DOI] [PubMed] [Google Scholar]
- Turner C, Ku L, Sonenstein F, Pleck J. Impact of ACASI on reporting of male-male sexual contacts: Preliminary results from the 1995 National Survey of Adolescent Males. Library of Congress. 1996;178 [Google Scholar]
- Viljoen DL, Gossage JP, Brooke L, Adnams CM, Jones KL, Robinson LK, Viljoen DL. Fetal alcohol syndrome epidemiology in a South African community: a second study of a very high prevalence area. Journal of Studies on Alcohol. 2005;66:593–604. doi: 10.15288/jsa.2005.66.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viljoen D, Craig P, Kymbaugh K, Boyle C, Blout S. Fetal alcohol syndrome--South Africa, 2001. MMWR Morbidity and Mortality Weekly Report. 2003;52:660–662. [PubMed] [Google Scholar]
- Weir SS, Morroni C, Coetzee N, Spencer J, Boerma JT. A pilot study of a rapid assessment method to identify places for AIDS prevention in Cape Town, South Africa. Sexually Transmitted Infections. 2002;78:106–113. doi: 10.1136/sti.78.suppl_1.i106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. [Accessed June 26, 2012];Development of a strategy towards promoting optimal fetal growth. http://www.who.int/nutrition/topics/lbw_strategy_background.pdf.
- Xu Y, Li Y, Tang Y, Wang J, Shen X, Long Z, Zheng X. The maternal combined supplementation of folic acid and Vitamin B(12) suppresses ethanol-induced developmental toxicity in mouse fetuses. Reproductive Toxicology. 2006;22:56–61. doi: 10.1016/j.reprotox.2005.12.004. [DOI] [PubMed] [Google Scholar]