Abstract
Objective
To determine age- and sex-specific incidence rates of inguinal hernia repairs (IHR) in a well defined USA population and examine trends over time.
Summary Background Data
IHR represent a substantial burden to the US healthcare system. An up to date appraisal will identify future healthcare needs.
Methods
A retrospective review of all IHR performed on adult residents of Olmsted County, MN from 1989 to 2008 was performed. Cases were ascertained through the Rochester Epidemiology Project, a record-linkage system with >97% population coverage. Incidence rates were calculated by using incident cases as the numerator and population counts from the census as the denominator. Trends over time were evaluated using Poisson regression.
Results
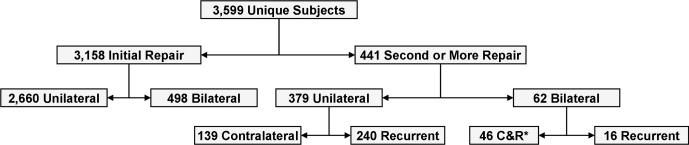
During the study period, a total of 4,026 IHR were performed on 3,599 unique adults. Incidence rates per 100,000 person-years were greater for men: 368 vs 44 for women, and increased with age: from 194 to 648 in men, and from 28 to 108 in women between 30 and 70 years of age. Initial, unilateral IHR comprised 74% of all IHR types. The life-long cumulative incidence of an initial, unilateral or bilateral IHR in adulthood was 42.5% in men and 5.8% in women. Over time (from 1989 to 2008), the incidence of initial, unilateral IHR in men decreased from 474 to 373 (relative reduction, RR=21%). Bilateral IHR increased from 42 to 71 (relative increase=70%), contralateral metachronous IHR decreased from 29 to 11 (RR=62%), and recurrent IHR decreased from 66 to 26 (RR=61%), all changes p<0.001.
Conclusions
IHR are common, their incidence varies greatly by age and sex, and has decreased substantially over time in Olmsted County, Minnesota.
Keywords: inguinal hernia, population-based study, incidence, repair, time trends, epidemiology
Introduction
Abdominal wall hernias collectively are the most common cause of major operations performed by general surgeons. Of these, inguinal hernias (IH) represent the vast majority. It is estimated that more than 800,000 IH are repaired each year in the USA and that 1 in every 4 men will require an inguinal hernia repair (IHR) in his lifetime.1,2 Nonetheless, there is limited epidemiological evidence emanating from well-defined populations, and most of the commonly quoted rates are either rough estimates or are outdated.1-3 Furthermore, little is known about whether the risk of developing an IH has increased or decreased over time, and whether the incidence of IHR is changing.
Several interconnected factors that can contribute to or protect from developing an IH have changed considerably over time. The American population is aging,4 and with an increase in life expectancy, a similar increase in the incidence of IHR is expected. On the contrary, the current obesity epidemic5 can decrease the expected incidence of IHR, as patients who are obese tend to have a lower incidence of IHR.1,6 The introduction of mesh-based repairs and minimally invasive techniques for the treatment of IH may modify the incidence of IHR, as changes in technique have been shown to influence the operation rate for recurrent hernias.7 In addition, a modern day acceptance of the watchful waiting approach to the treatment of IH can decrease the expected incidence of IHR.8 Furthermore, among particular types of hernia repair, changes over time could also be occurring. The increased adoption of laparoscopy for the treatment of IH with its inherent ability to treat an asymptomatic contralateral IH could increase the incidence of bilateral inguinal hernia repairs and decrease the rate of operations for contralateral metachronous inguinal hernias.9,10
Because projections of future healthcare burdens, resource allocation, policy making, and other important health related decisions are based on epidemiological indices, there is a need for accurate and up to date incidence rates. To address this problem we sought to measure age- and sex-specific incidence rates of IHR in a well-defined USA population. In addition, to better understand such a complex interplay of factors affecting the incidence of IHR over time, we sought to examine the trends in the incidence of IHR over the past two decades.
Methods
With prior Institutional Review Board approval, a retrospective review of all IHR performed on adult residents of Olmsted County, MN from January 1, 1989 to December 31, 2008 was performed.
Study Population
Olmsted County is located in southeastern Minnesota and has a population primarily of northern and central European descent. More than 70% of the population resides in Rochester, the centrally located county seat; the remainder of the county is rural. The local economy is based on farming, health care, and light industry. As of the 2000 US Census, the population of Olmsted County was 127,277: 51% being women, 11% above the age of 65 years, and 90% Caucasian.
Case Ascertainment
We ascertained cases through the Rochester Epidemiology Project (REP), a record-linkage system that provides the infrastructure for indexing and linking essentially all medical information of the county population.11,12 The REP covers and provides access to more than 97% of the population in Olmsted County. We ascertained potential cases of IHR (both primary and recurrent) by searching the REP electronic diagnostic indexes for H-ICDA13 (55001, 55003, 55004, 55011, 55021, 55101, 55201, 55301, 55211) and ICD-914 (550.01, 550.03, 550.11, 550.13, 550.91, 550.93) diagnostic codes, as well as Current Procedural Terminology (CPT)15 codes (17.11-17.24, 53.00-53.17) related to an IHR. The records of all patients with at least one of the aforementioned codes indexed during the study period were manually reviewed by the study team using a specifically designed form and following a manual of instructions. Study data were collected and managed using REDCap electronic data capture tools hosted at Mayo Clinic.16
Diagnostic Classification
We grouped IHR according to the order of occurrence in life (initial vs. second or more), laterality (unilateral vs. bilateral), and recurrence (recurrent vs. non-recurrent). We also sub-classified IH according to their location (left or right) and the type of hernia (direct, indirect, femoral, and pantaloon) as described in the operative note. In ambiguous cases we deferred the classification to the senior author (DRF), an experienced hernia surgeon.
Data Analysis
We determined as incident cases all subjects whose record revealed the presence of an IHR between January 1, 1989 and December 31, 2008 while they were county residents. Patients who moved to Olmsted County specifically for the treatment of their hernia were thus excluded. Incidence rates per 100,000 person-years were calculated using the incident cases of hernia repair as the numerator and age- and sex-specific estimates of the population of Olmsted County, Minnesota as the denominator. The population at risk was estimated using census data from 1980, 1990, and 2000 with simple linear interpolation for intercensal years separate within sex and 5-year age grouping. The counts for the years 2001-2009 were obtained from the US Intercensal Estimates.17 We did not correct the denominators by removing prevalent cases of IHR because all subjects were considered at risk for a repeat IHR. Incidence rates were directly age- and sex-adjusted to the structure of the 2000 USA white population. Trends over time were assessed by fitting Poisson regression models using the SAS procedure GENMOD (dist=poisson, link=log) and the natural logarithm of the population counts as the offset term. (SAS Institute Inc.; Cary, North Carolina). Incident cases were grouped into four calendar year intervals (1989-1993, 1994-1998, 1999-2003, 2004-2008). Age-specific incidence rates were used to derive cumulative incidence by age 70, 80, and 90 years, as well as for the entire lifetime (assuming no competing cause of death).18 All hypothesis testing was two-sided and p-values less than 0.05 were considered statistically significant.
Results
Age- and Sex-Specific Incidence Rates of IHR
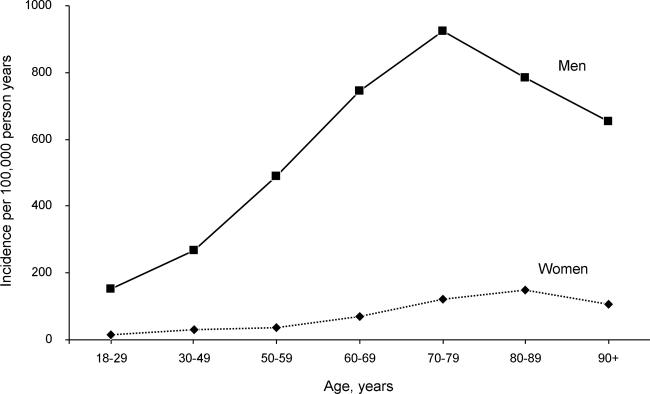
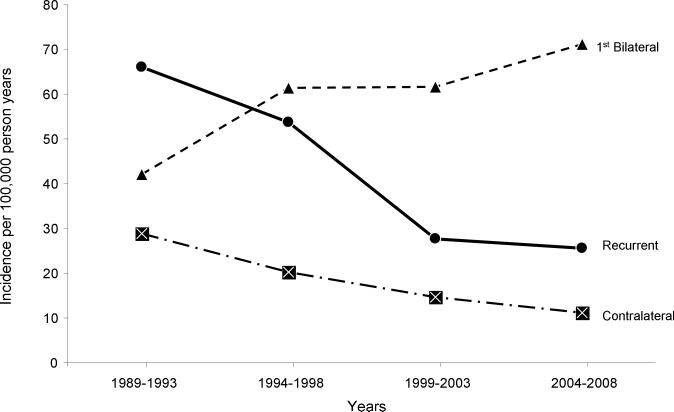
During the study period, a total of 4,026 IHR were performed on 3,599 unique adult residents of Olmsted County, MN, yielding an overall incidence of 200.1 per 100,000 person-years, or 217.1 per 100,000 person-years when age- and sex-adjusted to the structure of the 2000 USA white population (Figure 1 and Table 1). Incidence rates (per 100,000 person-years) varied greatly by sex, age, and clinical type of IHR. For IHR of any type, the incidence in men increased with age, reaching 922.6 for those aged 70-79 years old, and later decreasing to 654.3 for those 90 years of age or older. In women, the incidence of IHR of any type increased less noticeably with age, and reached its highest at 148.1 for women in the ninth decade of life (Figure 2). Similar age and sex patterns in incidence rates were also observed when examining different clinical types of IHR (Table 1).
Figure 1.
Clinical types of inguinal hernia repairs. *C&R= contralateral and recurrent
Table 1.
Age- and Sex-Specific Incidence Rates of Inguinal Hernia Repairs by Clinical Types of Inguinal Hernia Repairs in Olmsted County, MN, 1989-2008*
| Age (years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinical Type± | Sex | 18-29 | 30-49 | 50-59 | 60-69 | 70-79 | 80-89 | 90+ | Total |
| All | Women‡ | 15.1 (32) | 30.7 (118) | 37.8 (50) | 68.5 (59) | 122.1 (78) | 148.1 (61) | 106.9 (14) | 44.2 (412) |
| Men† | 153.4 (316) | 268.7 (1,023) | 488.3 (624) | 743.5 (588) | 922.6 (447) | 785.0 (165) | 654.3 (24) | 367.7 (3,187) | |
| Total | 83.4 (348) | 149.2 (1,141) | 259.1 (674) | 391.6 (647) | 467.3 (525) | 363.4 (226) | 226.6 (38) | 200.1 (3,599) | |
| 1 | Women‡ | 13.2 (28) | 28.1 (108) | 34.8 (46) | 59.2 (51) | 108.0 (69) | 131.1 (54) | 99.2 (13) | 39.6 (369) |
| Men† | 130.6 (269) | 194.3 (740) | 344.3 (440) | 505.8 (400) | 648.1 (314) | 528.1 (111) | 463.5 (17) | 264.3 (2,291) | |
| Total | 71.2 (297) | 110.9 (848) | 186.8 (486) | 272.9 (451) | 340.9 (383) | 265.3 (165) | 178.9 (30) | 147.9 (2,660) | |
| 2 | Women‡ | 0.9 (2) | 1.6 (6) | 3.0 (4) | 4.6 (4) | 6.3 (4) | 7.3 (3) | 7.6 (1) | 2.6 (24) |
| Men† | 11.6 (24) | 43.1 (164) | 81.4 (104) | 135.3 (107) | 128.0 (62) | 57.1 (12) | 27.3 (1) | 54.7 (474) | |
| Total | 6.2 (26) | 22.2 (170) | 41.5 (108) | 67.2 (111) | 58.7 (66) | 24.1 (15) | 11.9 (2) | 27.7 (498) | |
| 3 | Women‡ | 0.0 (0) | 0.5 (2) | 0.0 (0) | 1.2 (1) | 3.1 (2) | 4.9 (2) | 0.0 (0) | 0.8 (7) |
| Men† | 4.4 (9) | 10.5 (40) | 23.5 (30) | 30.3 (24) | 35.1 (17) | 52.3 (11) | 27.3 (1) | 15.2 (132) | |
| Total | 2.2 (9) | 5.5 (42) | 11.5 (30) | 15.1 (25) | 16.9 (19) | 20.9 (13) | 6.0 (1) | 7.7 (139) | |
| 4-6 | Women‡ | 0.9 (2) | 0.5 (2) | 0.0 (0) | 3.5 (3) | 4.7 (3) | 4.9 (2) | 0.0 (0) | 1.3 (12) |
| Men† | 6.8 (14) | 20.7 (79) | 39.1 (50) | 72.1 (57) | 111.5 (54) | 147.5 (31) | 136.3 (5) | 33.5 (290) | |
| Total | 3.8 (16) | 10.6 (81) | 19.2 (50) | 36.3 (60) | 50.7 (57) | 53.1 (33) | 29.8 (5) | 16.8 (302) | |
Data are presented as incidence rates per 100,000 person-years followed by the number of incident cases in parentheses.
Denominators (in person-years) for women are as follows: 18-29=211,405, 30-49=383,800, 50-59=132,316, 60-69=86,151, 70-79=63,902, 80-89=41,178, 90 and above=13,100.
Denominators (in person-years) for men are as follows: 18-29=206,015, 30-49=380,768, 50-59=127,803, 60-69=79,081, 70-79=48,449, 80-89=21,019, 90 and above=3,668.
± Clinical types of IHR are as follows: 1= Initial, unilateral IHR, 2= Initial, bilateral IHR, 3= Second or more, contralateral IHR, 4= Second or more, unilateral recurrent IHR, 5= Second or more, unilateral recurrent and contralateral metachronous IHR, 6= Second or more, bilateral recurrent IHR.
Figure 2.
Age- and sex-specific incidence of inguinal hernia repairs per 100,000 person-years for all types of inguinal hernia repairs.
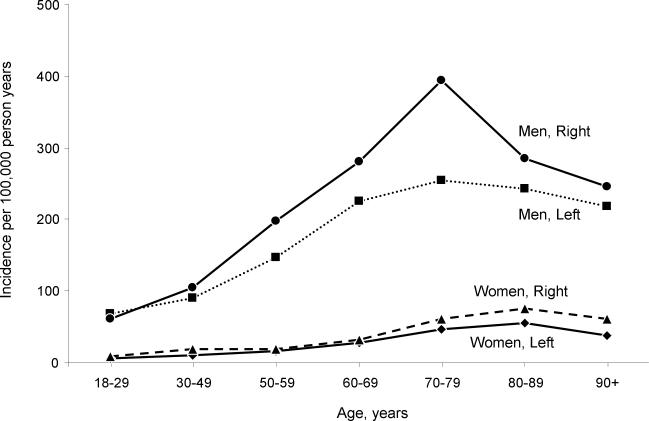
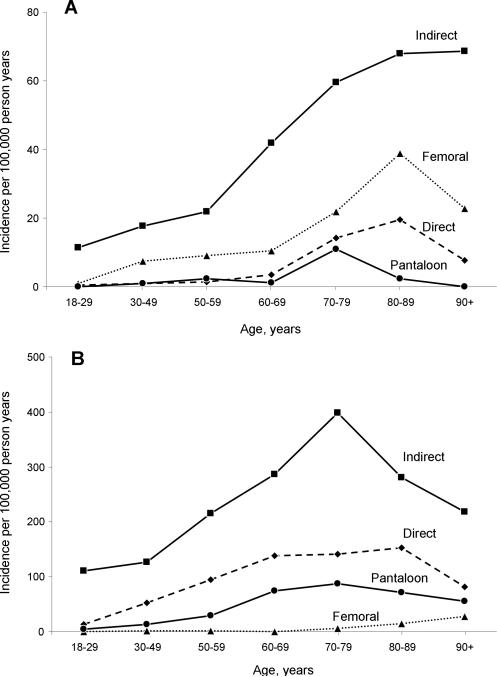
Incidence rates are presented by location and type of hernia for the cohort of patients with an initial, unilateral IHR event since this represented the largest group (Table 2). For men, the incidence of right sided IHR was greater than that of left sided IHR, both overall (ratio 1.2:1) and in each age group (except in the 18-29 age group). Right sided IHR were also more common than left sided IHR in women (ratio 1.4:1, Figure 3). The type of hernia also varied by age and sex. Indirect IH was the most common type of hernia in both men and women at any age; however, femoral hernias were the second most common type of hernia in women but the least common in men (Figure 4). Overall, the cumulative incidence of an initial, unilateral or bilateral, IHR in adulthood, assuming no competing cause of death, was 18.9% by age 70, 27.7% by age 80, 35.1% by age 90, and 42.5% for the entire lifetime for men. Likewise, the cumulative incidence for women, assuming no competing cause of death, was 1.9% by age 70, 3.1% by age 80, 4.5% by age 90, and 5.8% for the entire lifetime.
Table 2.
Age- and Sex-Specific Incidence Rates by Side and Type of Hernia for Initial Unilateral Inguinal Hernia Repairs in Olmsted County, MN, 1989-2008*
| Age (years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex | 18-29 | 30-49 | 50-59 | 60-69 | 70-79 | 80-89 | 90+ | Total | |
| Side | |||||||||
| Left | Women‡ | 5.2 (11) | 9.9 (38) | 15.9 (21) | 27.9 (24) | 46.9 (30) | 55.9 (23) | 38.2 (5) | 16.3 (152) |
| Men† | 68.9 (142) | 90.3 (344) | 146.3 (187) | 225.1 (178) | 253.9 (123) | 242.6 (51) | 218.1 (8) | 119.2 (1,033) | |
| Total | 36.7 (153) | 50.0 (382) | 80.0 (208) | 122.3 (202) | 136.2 (153) | 119.0 (74) | 77.5 (13) | 65.9 (1,185) | |
| Right | Women‡ | 8.0 (17) | 18.2 (70) | 18.9 (25) | 31.3 (27) | 61.0 (39) | 75.3 (31) | 61.1 (8) | 23.3 (217) |
| Men† | 61.6 (127) | 104.0 (396) | 198.0 (253) | 280.7 (222) | 394.2 (191) | 285.5 (60) | 245.4 (9) | 145.1 (1,258) | |
| Total | 34.5 (144) | 60.9 (466) | 106.9 (278) | 150.7 (249) | 204.7 (230) | 146.3 (91) | 101.4 (17) | 82.0 (1,475) | |
| Type | |||||||||
| Direct | Women‡ | 0.5 (1) | 1.0 (4) | 1.5 (2) | 3.5 (3) | 14.1 (9) | 19.4 (8) | 7.6 (1) | 3.0 (28) |
| Men† | 13.1 (27) | 52.3 (199) | 94.7 (121) | 137.8 (109) | 140.4 (68) | 152.2 (32) | 81.8 (3) | 64.5 (559) | |
| Total | 6.7 (28) | 26.6 (203) | 47.3 (123) | 67.8 (112) | 68.5 (77) | 64.3 (40) | 23.9 (4) | 32.6 (587) | |
| Femoral | Women‡ | 0.9 (2) | 7.6 (29) | 9.1 (12) | 10.4 (9) | 21.9 (14) | 38.9 (16) | 22.9 (3) | 9.1 (85) |
| Men† | 0.5 (1) | 0.8 (3) | 0.8 (1) | 0.0 (0) | 6.2 (3) | 14.3 (3) | 27.3 (1) | 1.4 (12) | |
| Total | 0.7 (3) | 4.2 (32) | 5.0 (13) | 5.4 (9) | 15.1 (17) | 30.5 (19) | 23.9 (4) | 5.4 (97) | |
| Indirect | Women‡ | 11.4 (24) | 17.7 (68) | 21.9 (29) | 41.8 (36) | 59.5 (38) | 68.0 (28) | 68.7 (9) | 24.9 (232) |
| Men† | 111.2 (229) | 125.8 (479) | 215.2 (275) | 285.8 (226) | 398.4 (193) | 280.7 (59) | 218.1 (8) | 169.5 (1,469) | |
| Total | 60.6 (253) | 71.5 (547) | 116.9 (304) | 158.6 (262) | 205.6 (231) | 139.9 (87) | 101.4 (17) | 94.6 (1,701) | |
| Pantaloon | Women‡ | 0.0 (0) | 1.0 (4) | 2.3 (3) | 1.2 (1) | 11.0 (7) | 2.4 (1) | 0.0 (0) | 1.7 (16) |
| Men† | 3.9 (8) | 13.1 (50) | 29.0 (37) | 74.6 (59) | 86.7 (42) | 71.4 (15) | 54.5 (2) | 24.6 (213) | |
| Total | 1.9 (8) | 7.1 (54) | 15.4 (40) | 36.3 (60) | 43.6 (49) | 25.7 (16) | 11.9 (2) | 12.7 (229) | |
Data are presented as incidence rates per 100,000 person-years followed by the number of incident cases in parentheses.
Denominators (in person-years) for women are as follows: 18-29=211,405, 30-49=383,800, 50-59=132,316, 60-69=86,151, 70-79=63,902, 80-89=41,178, 90 and above=13,100.
Denominators (in person-years) for men are as follows: 18-29=206,015, 30-49=380,768, 50-59=127,803, 60-69=79,081, 70-79=48,449, 80-89=21,019, 90 and above=3,668.
Figure 3.
Age- and sex-specific incidence of inguinal hernia repairs per 100,000 person-years by side of repair for subjects experiencing an initial, unilateral inguinal hernia repairs.
Figure 4.
Age-specific incidence of inguinal hernia repairs per 100,000 person-years by type of hernia in women (A), and men (B) who experienced an initial, unilateral inguinal hernia repairs.
Time Trends in the Incidence of IHR
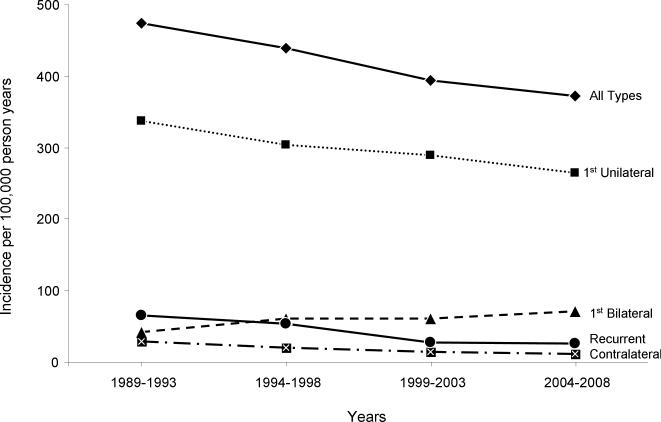
The incidence (rates per 100,000 person-years) of IHR of any type decreased over time. For men, it decreased almost linearly from 474.1 to 372.5 from the year 1989 to 2008 (p<0.001, Figure 5); the drop was roughly 1.1% per year or a relative reduction of 21.4% over the 20 year period. For women, the incidence of IHR remained relatively constant the first 15 years and then dropped from 49.1 to 42.1 in the last 5 years of the study (p<0.001, relative reduction 14.3%, Table 3).
Figure 5.
Age-adjusted incidence time trends of inguinal hernia repairs in men per 100,000 person-years, 1989-2008.
Table 3.
Age- and Sex-Adjusted Incidence Rate Time Trends of Inguinal Hernia Repairs in Olmsted County, MN, 1989-2008*
| Year of Repair | |||||
|---|---|---|---|---|---|
| Clinical Type± | Sex | 1989-1993 | 1994-1998 | 1999-2003 | 2004-2008 |
| All | Women‡ | 47.7 (93) | 47.0 (96) | 49.1 (116) | 42.1 (107) |
| Men† | 474.1 (727) | 438.4 (779) | 394.0 (802) | 372.5 (879) | |
| Total | 244.7 (820) | 227.7 (875) | 209.9 (918) | 198.7 (986) | |
| 1 | Women‡ | 42.6 (83) | 43.4 (89) | 45.4 (107) | 35.2 (90) |
| Men† | 337.4 (526) | 303.1 (545) | 290.0 (594) | 264.7 (626) | |
| Total | 179.2 (609) | 164.4 (634) | 159.5 (701) | 144.3 (716) | |
| 2 | Women‡ | 0.9 (2) | 1.9 (4) | 2.1 (5) | 5.3 (13) |
| Men† | 42.0 (65) | 61.4 (113) | 61.6 (125) | 71.2 (171) | |
| Total | 20.2 (67) | 30.0 (117) | 30.1 (130) | 36.9 (184) | |
| 3 | Women‡ | 0.9 (2) | 1.1 (2) | 0.4 (1) | 0.8 (2) |
| Men† | 28.8 (41) | 20.2 (35) | 14.7 (30) | 11.1 (26) | |
| Total | 13.5 (43) | 9.6 (37) | 7.1 (31) | 5.7 (28) | |
| 4-6 | Women‡ | 3.3 (6) | 0.6 (1) | 1.3 (3) | 0.8 (2) |
| Men† | 66.0 (95) | 53.7 (86) | 27.7 (53) | 25.5 (56) | |
| Total | 31.9 (101) | 23.6 (87) | 13.1 (56) | 11.8 (58) | |
Data are presented as age-adjusted (women, men) or age- and sex-adjusted (total) incidence rates per 100,000 person-years followed by the number of incident cases in parentheses. Rates are adjusted to the US white adult population in 2000, which included 83,579,000 women and 78,285,000 men.
Denominators (in person-years) for women are as follows: 1989-1993=205,217, 1994-1998=221,365, 1999-2003=240,848, 2004-2008=264,422.
Denominators (in person-years) for men are as follows: 1989-1993=186,589, 1994-1998=204,774, 1999-2003=225,760, 2004-2008=249,680.
±Clinical types of IHR are as follows: 1= Initial, unilateral IHR (n=2,660), 2= Initial, bilateral IHR (n=498), 3= Second or more, contralateral IHR (n=139), 4= Second or more, unilateral recurrent IHR (n=240), 5= Second or more, unilateral recurrent and contralateral metachronous IHR (n=46), 6= Second or more, bilateral recurrent IHR (n=16).
Initial, unilateral IHR followed similar incidence trends for both men and women, as those by IHR of any type (Figure 5 and Table 3). However, the incidence of bilateral IHR increased over time; particularly for men, increasing from 42.0 to 71.2 per 100,000 person-years (a relative increase of 70% over the last 20 years, p<0.001, Figure 6). For men, the rate of contralateral metachronous IHR decreased over time from 28.8 to 11.1 per 100,000 person-years (a relative reduction of 61.5% over the 20 year period, p<0.001). The rate of operations for recurrent hernias also decreased substantially over time, most notably for men, from 66 to 25.5 per 100,000 person-years (a relative reduction of 61.4% over the 20 year period, p<0.001).
Figure 6.
Age-adjusted incidence time trends of bilateral, contralateral and recurrent inguinal hernia repairs in men per 100,000 person-years, 1989-2008.
Discussion
This population-based study of all adults living in Olmsted County, Minnesota provides an up to date and rigorous measure of the incidence of IHR in a well-defined USA population. Our study shows that IHR varied greatly by age and sex. The incidence of IHR increased drastically with advancing age in men but increased only gradually in women. Both men and women were more likely to have a right sided than a left sided IHR. Though indirect inguinal hernias are the most common type of IH for both genders, femoral hernias represent the second most common type of IH in women but the least common in men. With an overall age- and sex-adjusted incidence rate of 217 per 100,000 person-years, IHR represent a substantial burden to the USA healthcare system. If these Olmsted County rates are extrapolated to the total USA population (307,006,550 residents as of July 2009),17 we expect that approximately 666,200 IHR are performed annually in the USA.
Based on 1996 statistics from the National Survey of Ambulatory Surgery (NSAS), Ruktow estimated that 770,000 IHR were performed in the United States in 2003.2 Non-sampling and sampling errors in the NSAS survey add to the uncertainty of such a quoted estimate. The NSAS survey did not sample Veterans Administration or other federal government hospitals which contribute substantially to the care of adult men at risk for hernia development, and it was estimated that the NSAS survey error rate was in the range of 10%.2 Additionally, data on hernias repaired on an emergent basis, for a recurrence or the type of hernia (i.e. direct or indirect), were not available to the NSAS survey. Despite such limitations, the NSAS survey has been the basis on which predictions and resource distribution decisions at the level of policy making have been made.2
Additional efforts to establish the magnitude of inguinal hernias include a community survey undertaken in Western Jerusalem from 1969-1973,3 the US First National Health and Nutrition Survey (1971-1975),1 and the Oxford Records Linkage Hernia Study (1976-1986).19 All three of these studies showed that the incidence of IHR increases with age, yielding a lifetime prevalence that ranges from 24% to 47% for men. With a lifetime cumulative incidence of 42.5% for men, our study results are consistent with previous reports.3,1,19 Of interest is the decrease in the incidence of IHR for both men and women after 80 years of age seen across all types of IHR. We believe this reflects that fewer individuals in this age group undergo an IHR because of comorbidities that take precedence over an IH. In such a case, a watchful waiting approach may seem a more attractive alternative than an IHR.8
This study shows a substantial decrease in IHR from 1989 to 2008. There are many potential explanations for these findings. First, the fact that the incidence of IHR decreased, despite an ever aging population,4 may reflect an increased adoption of the watchful waiting approach to the treatment of IHR;8 hence if less hernias are being repaired and potentially more hernias are being “watched”, the incidence would decrease. This seems unlikely given “watchful waiting” became a more publicized option in the year 20068 – nearing the end of this study.
Intuitively, obesity is thought of as a predisposing factor for developing an IH (i.e. increases intraabdominal pressure); however, recent evidence documents that obese people have a lower incidence of IHR.7, 8 Strikingly, the effect is reversed when dealing with recurrent hernias, as the risk of developing a recurrent IH appears to be increased with obesity.20 Whether the lower incidence rate of IHR in the obese population represents a true phenomenon or a reflection of: 1) obese patients not getting their hernias repaired because of comorbidities or 2) the diagnostic challenge of detecting an inguinal hernia in an obese patient, remains unknown and represents opportunity for further research. Regardless, during the last 2 decades, the prevalence of obesity in our community has increased5 and could explain, at least in part, the decrease in the incidence of IHR seen in this study.
Strenuous physical activity, because of occupation or type of work, has been also been thought of as a risk factor for developing an IH.21 Consequently, a shift in the workforce, from a more labor intensive environment (i.e. farming, construction) to an office-based-industrialized setting, could contribute to the decrease in the incidence of IHR seen in this study. However, studies that have evaluated such an association between strenuous work and the risk of developing an inguinal hernia are inconclusive, with some showing no difference,1 others an increase in risk,21 and others a protective effect.22
Changes in smoking patterns occurring over time could also be contributing to the findings of this study. Smoking, because of its deleterious effects on connective tissue and lung function, has been proposed as a risk factor for inguinal hernias by some,23 however, it is refuted by others.1,21 Regardless, community-wide smoking cessation programs in Olmsted County,24 the Minnesota Clean Indoor Air Act,25 and other cultural awareness programs could all be influencing the prevalence of smokers in Olmsted County, MN. Additionally, with increasing health care costs, lack of insurance, and ever-changing unemployment rates, access to medical care is not always a priority. Deferring or avoiding surgical repair of an IH because of the prohibitive costs or lack of insurance could be associated to our findings, although we have no tangible data to support this. How these potential changes in smoking patterns or economic intricacies interplay with the incidence of IHR represent opportunity for further research in the field.
The management of inguinal hernias has changed substantially over time.26 In fact, changes in technique have been shown to influence the operation rate for recurrent hernias.7 Hence an increased adoption of mesh-based techniques and/or laparoscopic repairs could explain the decrease in the rate for recurrent hernia repairs seen in this study; however, it would not explain the decrease seen in initial IHR. Of interest, the rate of bilateral IHR has increased over the past two decades. This phenomenon could be explained by an increased adoption of laparoscopic IHR,26 as such techniques allow for the detection and repair of asymptomatic contralateral inguinal hernias. Because such “occult” hernias can occur in up to 30% of patients who present clinically with a unilateral IH,27 it is not uncommon to convert a planned unilateral IHR to a bilateral IHR at the time of the operation during laparoscopic IHR. Thus, a downstream effect resulting from the increase in bilateral IHR appears to be the decrease in the rate of contralateral metachronous IHR seen over time, likely as a consequence of treating more of these “occult” contralateral IH. Such hernias if not detected and repaired at the time of an IHR, can become symptomatic in the subsequent years following the initial unilateral IHR and require a second operation (a contralateral metachronous IHR).10,28
This study has considerable strengths. A population-based sample avoids referral bias seen in hospital-based convenience samples. The REP covers the two locations where an IHR can be performed in the county (Olmsted Medical Center and Mayo Clinic), minimizing the possibility for coverage error; it includes both academic and community practice patterns and inpatient and outpatient surgery. We acknowledge that there may have been some Olmsted County residents who elected to undergo a hernia repair elsewhere, thus eluding the coverage of the REP. We believe this is unlikely and of minimal impact given the facilities and physicians available in the county and the nature of the disease. Another possible weakness is that epidemiological data generated in Olmsted County may not be generalizable to the USA population at large: Previous reports show that age, sex and ethnic characteristics of Olmsted County are similar to those of Minnesota and the Upper Midwest. However, Olmsted County is less ethnically diverse than the US population, more highly educated, and wealthier.29,12 Additionally, differences in health insurance coverage between Olmsted County and the US population could be influencing the rates of IHR seen in our county. Nonetheless, to our knowledge, this is the most up to date and rigorous appraisal of the incidence of IHR in a USA population. Our study is the first to provide separate incidence rates in both men and women for different clinical types of IHR, types of hernia, and laterality; such detail will enable better resource allocation and public health research. On the other hand, this appraisal of the incidence of IHR in adults is only half of the picture, and further research should explore the incidence of IHR in children, as their impact on adulthood can be substantial.30 In addition, we recognize that our study only captures one aspect of the IH spectrum (i.e. patients with an IH that had a surgical repair). To better understand the true impact of IH, we must characterize and quantify the population of patients who have an IH, either knowingly or not, and do not seek surgical repair.
In summary, the data from this study enable us to better understand and quantify the incidence of IHR in our society. This study also provides us with insight into the potential factors that interplay with the incidence of IHR over time. Because IH represent a substantial burden to the USA healthcare system, an accurate and up to date appraisal of the incidence of IHR and its changes over time may facilitate future healthcare needs planning and better study of interventions that aim to decrease the burden of IH.
Acknowledgments
The authors would like to thank Dr. Walter A. Rocca for his guidance and critical review of this manuscript, as well as all the personnel involved in the Rochester Epidemiology Project who made this study possible.
Support & Grants: This publication was made possible by the Rochester Epidemiology Project (Grant Number R01 AG034676 from the National Institute on Aging) and by Grant Number 1 UL1 RR024150 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Funding/Support: This study was supported by intramural funds.
Role of Sponsors: The funding sources for this study played no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation of the manuscript. The funding sources did not review the manuscript.
Footnotes
Author Contributions:
Dr. Zendejas had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Zendejas, Farley, Lohse
Acquisition of data: Zendejas, Ramirez, Kuchena, Jones, Ali, Hernandez-Irizarry
Analysis and Interpretation of Data: Lohse, Zendejas
Drafting of Manuscript: Zendejas, Lohse
Critical Revision of the Manuscript for Important Intellectual Content: Zendejas, Lohse, Hernandez-Irizarry, Farley
Statistical Analysis: Lohse
Obtained Funding: Zendejas, Farley
Administrative, Technical and Material Support: Zendejas
Study Supervision: Zendejas, Farley
Financial Disclosure: None relevant
Previous Presentation: None
References
- 1.Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol. 2007;165:1154–1161. doi: 10.1093/aje/kwm011. [DOI] [PubMed] [Google Scholar]
- 2.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83:1045–1051. v–vi. doi: 10.1016/S0039-6109(03)00132-4. [DOI] [PubMed] [Google Scholar]
- 3.Abramson JH, Gofin J, Hopp C, et al. The epidemiology of inguinal hernia. A survey in western Jerusalem. J Epidemiol Community Health. 1978;32:59–67. doi: 10.1136/jech.32.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Bank [August 20, 2011];World Development Indicators 2010. Available at: http://data.worldbank.org/data-catalog/world-development-indicators/wdi-2010.
- 5.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 6.Rosemar A, Angeras U, Rosengren A. Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg. 2008;247:1064–1068. doi: 10.1097/SLA.0b013e31816b4399. [DOI] [PubMed] [Google Scholar]
- 7.Aufenacker TJ, de Lange DH, Burg MD, et al. Hernia surgery changes in the Amsterdam region 1994-2001: decrease in operations for recurrent hernia. Hernia. 2005;9:46–50. doi: 10.1007/s10029-004-0279-5. [DOI] [PubMed] [Google Scholar]
- 8.Fitzgibbons RJ, Jr., Giobbie-Hurder A, Gibbs JO, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295:285–292. doi: 10.1001/jama.295.3.285. [DOI] [PubMed] [Google Scholar]
- 9.Bochkarev V, Ringley C, Vitamvas M, et al. Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc. 2007;21:734–736. doi: 10.1007/s00464-007-9196-x. [DOI] [PubMed] [Google Scholar]
- 10.Zendejas B, Onkendi EO, Brahmbhatt RD, et al. Contralateral metachronous inguinal hernias in adults: role for prophylaxis during the TEP repair. Hernia. 2011;15:403–408. doi: 10.1007/s10029-011-0784-2. [DOI] [PubMed] [Google Scholar]
- 11.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, et al. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. Ann Arbor: 1973. Commission on Professional and Hospital Activities: H-ICDA, hospital adaptation of ICDA. [Google Scholar]
- 14. [August 20, 2011];Classification of Diseases, Functioning, and Disability. Available at: http://www.cdc.gov/nchs/icd.htm.
- 15. [August 20, 2011];Current Procedural Terminology. Available at: http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/coding-billing-insurance/cpt.page.
- 16.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Census Bureau [August 20, 2011]; Available at: http://www.census.gov/.
- 18. [January 11, 2011];Mayo Clinic, Division of Biomedical Statistics and Informatics. Technical Reports #49, and 64, http://mayoresearch.mayo.edu/mayo/research/biostat/techreports.cfm.
- 19.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996;25:835–839. doi: 10.1093/ije/25.4.835. [DOI] [PubMed] [Google Scholar]
- 20.Rosemar A, Angeras U, Rosengren A, et al. Effect of body mass index on groin hernia surgery. Ann Surg. 2010;252:397–401. doi: 10.1097/SLA.0b013e3181e985a1. [DOI] [PubMed] [Google Scholar]
- 21.Carbonell JF, Sanchez JL, Peris RT, et al. Risk factors associated with inguinal hernias: a case control study. Eur J Surg. 1993;159:481–486. [PubMed] [Google Scholar]
- 22.Liem MS, van der Graaf Y, Zwart RC, et al. Risk factors for inguinal hernia in women: a case-control study. The Coala Trial Group. Am J Epidemiol. 1997;146:721–726. doi: 10.1093/oxfordjournals.aje.a009347. [DOI] [PubMed] [Google Scholar]
- 23.Cannon DJ, Read RC. Metastatic emphysema: a mechanism for acquiring inguinal herniation. Ann Surg. 1981;194:270–278. doi: 10.1097/00000658-198109000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Croghan IT, O'Hara MR, Schroeder DR, et al. A community-wide smoking cessation program: Quit and Win 1998 in Olmsted county. Prev Med. 2001;33:229–238. doi: 10.1006/pmed.2001.0883. [DOI] [PubMed] [Google Scholar]
- 25. [August 12, 2011];Minnesota Clean Indoor Air Act. Available at: http://www.health.state.mn.us/divs/eh/indoorair/mciaa/ftb/mciaa.pdf.
- 26.Zendejas B, Ramirez T, Jones T, et al. Trends in the utilization of inguinal hernia repair techniques: A population-based study. Am J Surg. 2012 doi: 10.1016/j.amjsurg.2011.10.005. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zendejas B, Onkendi EO, Brahmbhatt RD, et al. Long-term outcomes of laparoscopic totally extraperitoneal inguinal hernia repairs performed by supervised surgical trainees. Am J Surg. 2011;201:379–384. doi: 10.1016/j.amjsurg.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 28.Thumbe VK, Evans DS. To repair or not to repair incidental defects found on laparoscopic repair of groin hernia: early results of a randomized control trial. Surg Endosc. 2001;15:47–49. doi: 10.1007/s004640000254. [DOI] [PubMed] [Google Scholar]
- 29.St Stauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester epidemiology project. Mayo Clin Proc. 2012;87:151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zendejas B, Zarroug AE, Erben YM, et al. Impact of childhood inguinal hernia repair in adulthood: 50 years of follow-up. J Am Coll Surg. 2010;211:762–768. doi: 10.1016/j.jamcollsurg.2010.08.011. [DOI] [PubMed] [Google Scholar]